
Continuing Education in
the Health Professions
Proceedings of a Conference
Chaired by Suzanne W. Fletcher, M.D., M.Sc.
Edited by Mary Hager, Sue Russell,
and Suzanne W. Fletcher
, M.D., M.Sc.
Continui ng Educ ation in the Health Profess ions
Fl etcher
The Josiah Macy, Jr. Foundation is a private philanthropy dedicated to improving
the health of individuals and the public. Since its establishment in 1930, the
Foundation has focused its support principally on projects and conferences
designed to enhance the education of health professionals, especially physicians.
ISBN 0-914362-49-6
This monograph is in the public domain and may be reproduced or copied without
permission. Citation, however, is appreciated: Hager M, Russell S, Fletcher SW, editors.
Continuing Education in the Health Professions: Improving Healthcare Through
Lifelong Learning, Proceedings of a Conference Sponsored by the Josiah Macy, Jr.
Foundation; 2007 Nov 28 - Dec 1; Bermuda. New York: Josiah Macy, Jr. Foundation;
2008. Accessible at www.josiahmacyfoundation.org

A Conference Sponsored by the
Josiah Macy, Jr. Foundation
Chaired by Suzanne W. Fletcher, M.D., M.Sc.
Bermuda
November 2007
Edited by Mary Hager, Sue Russell,
and Suzanne W. Fletcher, M.D., M.Sc.
Published by the
Josiah Macy, Jr. Foundation
44 East 64th Street
New York, NY 10065
www.josiahmacyfoundation.org
2008
Continuing Education in
the Health Professions:
Improving Healthcare
Through Lifelong Learning
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 1

Preface …………………………………………………………………… 4
Introduction ……………………………………………………………… 7
Chairman’s Summary of the Conference ……………………………… 13
Conference Participants ………………………………………………… 24
Conference Images ……………………………………………………… 26
I. APPROACHES TO KNOWLEDGE DEVELOPMENT—
WHAT WORKS AND WHAT DOES NOT ………………………… 29
How Physicians Learn and How to Design Learning
Experiences for Them …………………………
—Donald E. Moore, Jr., Ph.D. …………………………………… 30
Transforming Continuing Medical Education Through
Maintainence of Certification ………………
—F. Daniel Duffy, M.D. ………………………………………… 63
Discussion Highlights ………………………………………… 77
Internet Continuing Education ………………
—Denise Basow, M.D.…………………………………………… 82
Informatics Skills Needed! ………………………
—Donald A.B. Lindberg, M.D. ………………………………… 92
Remarks ……………………………………………
—David C. Slawson, M.D. ……………………………………… 94
Discussion Highlights ………………………………………… 98
II. FINANCING CONTINUING EDUCATION: ………………………
WHO, HOW, A ND WHY……………………………………………… 103
Financial Support for Continuing Education in the
Health Professions ……………………………
—Robert Steinbrook, M.D. ……………………………………… 104
Remarks ……………………………………………
—Jordan J. Cohen, M.D. ………………………………………… 127
Discussion Highlights ………………………………………… 132
III. DESIGNING SYSTEMS FOR LIFELONG LEARNING ………………
TO IMPROVE HEALTH …………………………………………… 141
Continuing Health Professional Education Delivery
in the United States ……………………………
—David A. Davis, M.D., and Trina Loofbourrow, B.A. ……… 142
Remarks ……………………………………………
—Pamela Mitchell, Ph.D., M.S., B.S. …………………………… 177
Discussion Highlights ………………………………………… 179
Table of Contents
2
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 2

The Macy Conference format provides ample time for discussion and, after
reading commissioned background papers and hearing remarks prepared
by the authors and several participants, the 36 participants seated around
the table offered countless informed observations, comments, and opinions.
The Discussion Highlights sections at the end of each session group these
comments according to themes that emerged, though many comments might
have been placed in several categories. The papers, remarks, and comments
have been lightly edited for brevity and clarity. On the final day, partici-
pants developed the set of conclusions and recommendations found in the
Executive Summary and, again, beginning on page 219.
3
Learning to Work Together to Improve the
Quality of Healthcare …………………………
—Maryjoan D. Ladden, Ph.D., R.N. …………………………… 182
Remarks ……………………………………………
—Carol Havens, M.D. …………………………………………… 189
Discussion Highlights ………………………………………… 191
IV. REACTION FROM THE TRENCHES ……………………………… 195
Remarks ……………………………………………
—Grant S. Fletcher, M.D., M.P.H. ……………………………… 196
—James A. Clever, M.D. ………………………………………… 199
—Susan W. Wesmiller, M.S., R.N. ……………………………… 200
—Regina Benjamin, M.D., M.B.A. ……………………………… 203
Discussion Highlights ………………………………………… 206
V. MOVING TOWARDS THE FUTURE ………………………………… 209
Continuing Medical Education: Some Important ………
Odds and Ends …………………………………
—David C. Leach, M.D. ………………………………………… 210
Discussion Highlights ………………………………………… 216
Conference Conclusions and Recommendations …………………… 219
Additional References Suggested by Conference Participants ……… 225
Biographical Sketches and Statements of Potential Conflicts of ……
Interest of Conference Participants ……………………………… 230
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 3

Preface
June E. Osborn, M.D.
During my tenure as president of the Macy Foundation, we funded
efforts to improve undergraduate health professional and even
graduate medical education. However, it seemed difficult, if not
impossible, to find a useful entry point on continuing education,
even though it was a massive enterprise that was mandated very
broadly. What is more, I repeatedly bumped up against the fact that
much of the funding for continuing medical education (CME) was
being provided by pharmaceutical company sponsors. Decades
earlier that was true, of course, but not to anywhere near the extent
that had come to be the case. In fact, as I inquired of colleagues
closer to the issue than I was, I got estimates that 60-90 percent of
all CME was supported by industry. Indeed, so pervasive was that
mechanism of support that almost no alternative sources remained.
While there was nothing intrinsically wrong with that state of affairs,
it tended to be festooned by associated phenomena having little to
do with education per se, such as free lunches, gifting of other sorts,
or even more attractive subsidies such as opportunities to qualify for
CME credits by enrolling in courses offered in desirable spots.
4
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 4

5
Clearly there was room for considerable concern about the planning
of offerings for life-long learning, not to mention possible distortion
of objectivity of CME content design and delivery.
I became increasingly troubled as, over time, requirements by state
licensing bodies to accumulate arbitrary hours of CME credit became
virtually universal, and yet they could be satisfied rather randomly,
or at least without any consistency or quality control as to format
and content. The well-established PowerPoint presentation format
had become nearly universal, and there was little evident impetus
or support for other forms of learning, especially at points of care.
All those worrisome trends in CME content, quality, and relevance
to practice were evolving at a time when bench-to-bedside transla-
tional research was being promoted and when biomedical advances
made the need for pertinent life-long learning experiences ever
more urgent and important.
By happy chance, I got into a discussion of these concerns with
Dr. Suzanne Fletcher early in 2006, at a time when I was trying to
formulate plans for the final Macy Conference to be held prior to my
retirement at the end of 2007. When I asked if she — with her long
leadership of a large Harvard CME course — thought that would be
a timely and useful topic for a conference, she endorsed the idea
vigorously. Better yet when I began to plan, the first step — choosing
a chairperson — fell neatly into place. Suzanne’s enthusiasm was
matched by her energy, and she agreed to chair the planning,
convening, and subsequent monograph preparation.
This volume, then, is the product of the resultant Macy Conference,
held in Southhampton, Bermuda from November 28 to December 1,
Osborn
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 5

2007. In preparation for the conference, an excellent and hard-working
planning committee delineated areas of need for newly commissioned
papers, set an agenda for the conference over two-and-one-half
days, and worked diligently to be sure that the professional and
experiential range of the participants invited to contribute to the
deliberations would provide as many pertinent voices as possible
to assure a rich discussion. Given that all the health professions are
facing similar or analogous problems to those of medicine, efforts
were made to include nursing, in particular, and other professions’
experience where possible. The resulting conference was remark-
ably stimulating and led to a broad consensus, expressed in the
conclusions and recommendations presented in this monograph.
As Dr. Fletcher says eloquently in her Introduction, the resultant
exploration of the facts, deficiencies, needs, and challenges for
continuing education of health professionals is certainly timely. I
hope it serves to move the health professions forward in their pur-
suit of optimal ways to provide and require continuing education
throughout the professional lifetimes of their members.
President Emerita, Josiah Macy, Jr. Foundation
6
Preface
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/12/08 11:07 AM Page 6

7
Introduction
Suzanne Fletcher, M.D., M.Sc.
Harvard Medical School
Chair
In November, 1908 the Board of Trustees of the Carnegie Foundation
authorized what many consider the seminal study of medical
education in this country. Two years later Abraham Flexner published
his report on medical education in the United States and Canada.
1
The report was so influential that most physicians in the United
States continue to be educated according to Flexner’s precepts.
One hundred years later, the Josiah Macy, Jr. Foundation convened
a Conference on Continuing Education in the Health Professions.
Our mandate was to examine continuing education in multiple
health professions, not undergraduate medical education. So why
bring up Flexner, who wrote his report many years even before the
birth of the Macy Foundation? When I perused Flexner’s report in
preparation for our gathering, I was struck that, even now, many
aspects of that nearly 100-year-old document remain remarkably
relevant to our deliberations at this conference.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 7

First, why is education in the health professions so important anyway?
The Carnegie Foundation undertook their study with two major
interests in mind, or as President Pritchett put it, “first, the youths
who are to study medicine and to become the future practitioners,
and secondly, the general public, which is to live and die under
their ministrations.”
2
The planning committee for this conference
came to a remarkably similar conclusion. At our very first meeting,
Marc Nivet asked about the view from the trenches, and this question
led to an important session in our conference. Later, when we were
deep into thinking about the complicated educational approaches,
financing, and structures involved in continuing education, June
Osborn, who has stressed the public throughout her tenure as
President at Macy, and Jordan Cohen brought it all into focus by
reminding us that what makes these deliberations truly important
is the need to improve the quality of healthcare. This broader social
perspective separates education in the health professions from
many other worthy educational endeavors.
The second reason why Flexner’s report remains relevant is that he
addressed the type and mode of education. He visited every one
of the 150 medical schools in existence at that time to observe
precisely what subjects were taught and how they were taught. He
concluded that too often laboratory science and bedside teaching
were neglected in favor of didactic lectures. He summed up his
argument for the need for hands-on learning by quoting an earlier
article by Cabot and Locke:
Learning medicine is not fundamentally different from learning
anything else. If one had one hundred hours in which to learn
to ride a horse or to speak in public, one might profitably spend
perhaps an hour (in divided doses) in being told how to do it,
four hours in watching a teacher do it, and the remaining ninety-
five hours in practice, at first with close supervision, later under
general oversight.
3
Today, how best to conduct continuing education so as to positively
affect the health of patients and the public remains a challenge.
That we have a ways to go is clear from many studies demonstrating
large differences — a “chasm” according to the IOM report
4
—
between what should be done and what is done in practice. Don
Introduction
8
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 8

Fletcher
9
Moore presented a wonderful summary of what we know today
about how clinicians learn. He pointed out that most formal continuing
education programs continue to be made up of didactic lectures
and very few — Don estimates 5 percent — on assessing competence
and performance. What Flexner (and Cabot and Locke) said 100
years ago still applies.
Medical specialty boards are beginning to address this problem
with the requirement of maintenance of certification programs.
As Dan Duffy described in his presentation, these programs require
clinicians to review the care they actually deliver in their own prac-
tices, compare the results with standards of excellence, and create
a plan for improvement. This approach goes back to the 95-hour
rule Flexner advocated so long ago.
Perhaps the most important issue in continuing education today is
its financing. Robert Steinbrook pointed out that commercial support
for accredited continuing medical education in the United States
has quadrupled in less than a decade, and last year it reached a total
of $1.5 billion—accounting for about 60 percent of the income for
all of the accredited continuing medical education programs in the
United States. No wonder we see a rising concern that commercial
interests may be distorting the education of practicing clinicians. The
U.S. Senate Finance Committee summed it up this way: “It seems
unlikely that [a] sophisticated industry would spend such large sums
on an enterprise but for the expectation that the expenditures will
be recouped by increased sales.”
5
The Senate Committee called for
better oversight to ensure that continuing education programs are
independent of drug company interests.
Flexner wrote his report 100 years ago, when very few effective
drugs existed, when Osler advocated little more than morphine,
nitroglycerin, iron, and quinine. How could Flexner have any rele-
vance to this vexing modern problem? I think he does. Flexner often
used the word “commercial” when describing the problems of the
worst medical schools he visited. He pointed out that laboratory
and patient-based education was expensive while didactic lectures
were cheap, and so the schools that survived and profited only from
fees tended to emphasize the latter. He challenged the fundamental
assumption that medical education should be a business. He advo-
cated the need for standards that, if adopted, clearly would adversely
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 9

affect the financial interests of some.
Today, it is increasingly clear that commercial financing has infiltrated
the very fabric of continuing education. Last year JAMA published a
paper, coauthored by David Blumenthal and Jordan Cohen, calling
for academic medical centers to take the lead in eliminating conflicts
of interest between physicians and industry. The authors proposed
that manufacturers should not be permitted to provide support for
any ACCME-accredited continuing education program and, further,
that faculty should not serve on speakers’ bureaus sponsored by
drug companies.
6
Results from a recent survey of medical school department chairs,
published in JAMA, show just how difficult it will be to move this
call from proposal to policy; 60 percent of the department chairs had
some form of financial relationship with industry, as did two thirds
of their departments
.
7
Most chairs perceived no ill effects from these
relationships, and most viewed them as helpful to the educational
process. Our conference dealt squarely with this conundrum.
With regard to organizations that teach, Flexner recommended that
medical education be linked closely with universities. He was con-
vinced that such linkage would provide higher standards, better
teachers, and more resources for students. He also recommended that
teaching hospitals have close links to medical schools. Fundamentally,
he was suggesting that organizational aspects of education should
be set up to achieve the best possible education.
What about the situation today? Dave Davis has provided us with an
overview of the organizations involved in and accrediting continuing
education in medicine, pharmacy, and nursing; the landscape is
crowded, with many different types of organizations involved— far
more than for undergraduate and graduate education. Is this the best
way? We devoted a session of our conference to this topic.
One area barely mentioned by Flexner is interprofessional collabo-
ration, but today high-quality healthcare demands communication,
collaboration, and teamwork among heath professionals. Several IOM
reports on quality of healthcare in this country have stressed team-
work and systems changes. Maryjoan Ladden argued that continuing
education of various health professionals together promotes collabo-
10
Introduction
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 10

ration, decreases adverse health effects, and improves healthcare.
I found no comment about continuing education in Flexner’s report.
However, one of the giants of that age, William Osler, was acutely
aware of its importance. He thought physicians had an obligation to
keep learning about medicine from others, both through the literature
and through subjecting their practices to the scrutiny of colleagues.
He loved medical libraries and amassed a private library of approxi-
mately 8000 books. He summed up his feelings this way: “It is
astonishing with how little reading a doctor can practice medicine,
but it is not astonishing how badly he may do it
.
”
8
One hundred
years later, we still have a ways to go.
If Flexner had attended this conference, perhaps the most fascinat-
ing part for him would have been the discussion about the Internet
and its effect on the ability of doctors and nurses to keep up with
new information. Denise Basow and Don Lindberg both offered
presentations describing the ways in which this wonderful new
technology provides, really for the first time, just-in-time learning
for all of us in the health professions, and, as Don pointed out, for
our patients.
Flexner made major recommendations for change. This conference
also has led to major recommendations, although we spent two and
a half days together as opposed to Flexner’s two years’ effort. Also,
David Leach reminded us about the efforts of other groups. What
can one more report from a Macy Conference contribute?
I think there are at least two possibilities. First, our perspective cuts
across health professions. Second, the participants in this conference
were invited as leaders in the medical, nursing, and education
professions, not as representatives of organizations involved in
continuing education. As such, we had the opportunity to consider
continuing education of the healthcare professions as it contributes
to our professions and to society at large. By adopting this approach,
our goal was that the description of a profession written many years
ago in a legal opinion, and echoing Justice Brandeis’ famous quote,
continues to apply today:
A profession is not a business. It is distinguished by the require-
ments of extensive formal training and learning, admission to
11
Fletcher
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 11

12
Introduction
practice by qualifying licensure, a code of ethics imposing stan-
dards qualitatively and extensively beyond those that prevail or
are tolerated in the marketplace, a system for discipline of its
members for violation of the code of ethics, a duty to subordi-
nate financial reward to social responsibility, and notably, an
obligation on its members, even in non-professional matters, to
conduct themselves as members of a learned, disciplined, and
honorable occupation.
9
REFERENCES
1. Flexner A. Medical Education in the United States and Canada. A Report to the
Carnegie Foundation for the Advancement of Teaching. New York: The Carnegie
Foundation for the Advancement of Teaching; 1910.
2. Pritchett HS. Introduction. In Flexner A. Medical Education in the United States and
Canada. A Report to the Carnegie Foundation for the Advancement of Teaching. New
York: The Carnegie Foundation for the Advancement of Teaching; 1910. p. vi–xvii.
3. Cabot RC, Locke EA. The organization of a department of clinical medicine. Boston
Med Surg J. 1905;153:461–465.
4. Institute of Medicine Committee on Quality of Healthcare in America. Crossing the
Quality Chasm: A New Health System for the 21st Century. Washington DC: National
Academy Press; 2001.
5. Committee Staff Report to the Chairman and Ranking Member. Use of Educational
Grants by Pharmaceutical Manufacturers. Washington DC: United State Senate
Committee on Finance; April 2007.
6. Brennan TA, Rothman DJ, Blank L, et al. Health industry practices that create con-
flicts of interest: a policy proposal for academic medical centers. JAMA.
2006;295:429–433.
7. Campbell EG, Weissman JS, Ehringhaus S, et al. Institutional academic-industry rela-
tionships. JAMA. 2007;298:1779–1786.
8. Osler W. Books and men. In: Osler W. Aequanimatas and Other Addresses.
Philadelphia: P. Blakeson’s Sons and Co; 1905. p. 22.
9. New York Court of Appeals Statement on Matter of Freeman, 311 N. E. 2d 480(1974).
Accessible at www.wsba.org/atj/committees/jurisprudence/jurisethics.htm (Access
date: February 15, 2008).
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 12
Chairman’s Summary
of the Conference
Continuing education (CE) of health professionals is essential to
the health of all Americans. With accelerating advances in health
information and technology, physicians, nurses, and other health
professionals must maintain and improve their knowledge and skills
throughout their careers in order to provide safe, effective, and high
quality healthcare for their patients.
Yet continuing education in the health professions is in disarray.
Over the past decade, both professional and lay reports have
identified multiple problems. CE, as currently practiced, does not
focus adequately on improving clinician performance and patient
health. There is too much emphasis on lectures and too little empha-
sis on helping health professionals enhance their competence and
performance in their daily practice. With Internet technology, health
professionals can find answers to clinical questions even as they
care for patients, but CE does not encourage its use or emphasize
its importance. And, while studies show that inter-professional
collaboration, teamwork, and improved systems are key to high
quality care, accrediting organizations have not found ways to
promote teamwork or align CE with efforts to improve the quality
of health systems.
Another significant problem is the growing link between continuing
education and commercial interests. In 2006, the total income for
accredited CE activities in medicine was $2.4 billion. Commercial
support from pharmaceutical and medical device manufacturers
accounted for more than 60 percent, about $1.45 billion, of the total.
Over the past two years, the Senate Finance Committee has investi-
gated pharmaceutical company support for continuing education
13
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 13

in medicine. Despite efforts to control improper influences, the
committee concluded that the organizations providing continuing
education could still accommodate commercial interests of sponsors
and sponsors could still target their funding for educational
programs likely to support sales of their products.
To address concerns about CE, the Josiah Macy, Jr. Foundation
convened a conference on “Continuing Education in the Health
Professions.” Suzanne W. Fletcher, M.D., M.Sc., Professor of
Ambulatory Care and Prevention, Emeritus, at Harvard Medical
School, served as chair. The two-and-one-half-day conference,
which was held in Bermuda in November of 2007, included 36
leaders in medicine, nursing, and education. Commissioned back-
ground papers covered a range of CE-related topics, including a
review of how physicians and other health professionals learn, the
role of information technology, financing, and certification.
Although much of the conference discussion was relevant to the
continuing education of all health professionals, participants focused
on accredited CE for medicine and nursing. They acknowledged
that much professional learning takes place informally and outside
accredited formats.
Conference themes were inter-related, for the methods used for
continuing education are influenced both by the means of financial
support and by mechanisms for accreditation. Unfortunately,
participants found, current systems of CE do not meet the needs
of health professionals as well as they should:
— Too much CE relies on a lecture format and counts hours of
learning rather than improved knowledge, competence, and
performance.
— Too little attention is given to helping individual clinicians examine
and improve their own practices.
— Insufficient emphasis is placed on individual learning driven by
the need to answer the questions that arise during patient care.
— CE does not promote inter-professional collaboration, feedback
from colleagues and patients, teamwork, or efforts to improve
systems of care, activities that are key to improved performance
14
Chairman’s Summary
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 14

by health professionals.
— CE does not make adequate or creative use of Internet technology,
which can help clinicians examine their own practice patterns,
bring medical information to them during patient care, and aid
them in learning new skills.
— There is too little high-quality scientific study of CE.
Participants warned that the health professions, especially medicine,
threaten the ethical underpinnings of professionalism by participat-
ing in a multi-billion dollar CE enterprise so heavily financed by
commercial interests. This arrangement, which evolved over the
years, distorts continuing education. It places physicians and nurses
who teach CE activities in the untenable position of being paid,
directly or indirectly, by the manufacturers of healthcare products
about which they teach. At the same time, commercial support of
CE places learners in an obligatory position because they are often
given free meals and small gifts. Independent judgment of how
best to care for patients is compromised. Bias, either by appearance
or reality, has become woven into the very fabric of continuing
education. The professions, themselves, must right this wrong.
In a free-market system, commercial entities, such as drug and
device manufacturers, have a clear responsibility to shareholders to
gain market advantage and generate a profit, while health profes-
sionals have a moral responsibility to provide safe, high quality
care for their patients, based on valid scientific findings. The two
responsibilities are fundamentally incompatible. Even if bias could
be avoided, the potential, and the perception, are ever-present.
Companies with billions of dollars at stake cannot be expected to
be neutral or objective when assessing the benefits, harms, and
cost-effectiveness of their products, for they are in the legitimate
business of gaining market advantage and want clinicians to use
and prescribe their products.
Yet, an objective and neutral assessment of clinical management
options is precisely what is needed in continuing education.
Participants emphasized that, regardless of the financial impact on
for-profit companies, patient care must be based on scientific evidence
and commercial interests should not determine the topics or content
Fletcher
15
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 15

of CE. Because of these underlying ethical issues, participants
concluded that the commercial entities that manufacture and sell
healthcare products should not provide financial support for the
continuing education of health professionals.
Participants acknowledged that many major advances in health-
care, especially in the development of new drugs and devices,
have come from careful collaboration between medical and
commercial investigators. Too, corporations have made valuable
donations to academic health centers to support professorships,
scholarships, programs, and buildings, all of which contribute to
the public good.
Despite recent changes in CE accreditation to reduce commercial
influence, the problem persists and organizations with little profes-
sional expertise in healthcare, and supported almost entirely by
commercial interests, provide accredited continuing education. At
the same time, accrediting groups require all organizations providing
CE to go through laborious, bureaucratic procedures to document
that no inappropriate influence has occurred.
Participants pinpointed another serious failure with current accredi-
tation mechanisms. At a time when inter-professional collaboration,
teamwork, and improvement of systems are key to high quality
healthcare, accrediting organizations for the various health profes-
sions still work in silos. Rather than promoting inter-professional
collaboration and education, regulations and procedures for
accreditation make inter-professional collaboration difficult. And,
while systems of care have a major impact on the quality of health-
care delivered by clinicians, accrediting organizations have been
slow to align their CE activities with quality improvement efforts
by systems of care.
Participants identified a set of principles they believe should underlie
and guide continuing education of the health professions:
— Integrate continuing education into daily clinical practice.
— Base continuing education on the strongest available evidence
for practice.
16
Chairman’s Summary
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 16

— Minimize, to the greatest extent possible, both the reality and the
appearance of bias.
— Emphasize flexibility and easy accessibility for clinicians.
— Stress innovation and evaluation of new educational methods.
— Address needs of clinicians across a wide spectrum, from
specialists in academic health centers to rural solo practitioners.
— Support inter-professional collaboration.
— Align continuing education efforts with quality improvement
initiatives at the level of health systems.
After two and a half days of discussion, participants agreed to the
following conclusions and recommendations:
CONCLUSIONS
Continuing Education and the Public
The quality of patient care is profoundly affected by the performance
of individual health professionals.
The fundamental purposes of continuing health professional
education (CE) are:
— To improve the quality of patient care by promoting improved
clinical knowledge, skills and attitudes, and by enhancing
practitioner performance.
— To assure the continued competency of clinicians and the
effectiveness and safety of patient care.
— To provide accountability to the public.
CE fulfills a critically important, indeed essential, public purpose.
Given the accelerating pace of change in clinical information and
technology, CE has never been more important.
Fletcher
17
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 17

18
Responsibilities of Individual Professionals, Professional
Teams, and Health Systems
Maintaining professional competence is a core responsibility of
each health professional, regardless of discipline, specialty, or type
of practice.
The individual clinician has been the principal unit of accountability
for performance in the healthcare delivery system. Given that the
performance of health systems also profoundly affects patient care,
CE fails to take into account systems of care.
Effective patient care increasingly depends on well-functioning
teams of healthcare professionals. Therefore, CE must address the
special learning needs of collaborating teams.
Quality improvement efforts and CE activities overlap and ideally
are mutually reinforcing.
CE Methods
Traditional lecture-based CE has proven to be largely ineffective in
changing health professional performance and in improving patient
care. Lecture formats are employed excessively relative to their
demonstrated value.
Professional conferences play an important role in CE by promoting
socialization and collegiality among health professionals. Health
professionals have the responsibility to help one another practice
the best possible care. Meeting together provides opportunities for
cross-disciplinary and cross-generational learning and teaching.
Practice-based learning and improvement is a promising CE
approach for improving the quality of patient care. Maintenance
of certification programs (in which clinicians review the care they
actually deliver in their own practices, compare the results with
standards of excellence, and create a plan for improvement) and
maintenance of licensure programs are moving CE in this direction.
Currently, most CE faculty are insufficiently prepared to teach
practice-based learning.
Information technology is essential for practice-based learning by:
Chairman’s Summary
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 18

— Providing access to information and answers to questions at the
time and place of clinical decision-making (point-of-care learning).
— Providing a database of clinician performance at the individual
and/or group practice level, which can be compared to best
practices and used to make plans for improvement.
— Providing automated reminder systems.
Interactive scenarios and simulations are promising approaches to
CE, particularly for skills development, whether the skill is a highly
technical procedure, history taking, or a physical examination
technique.
Insufficient research is currently directed at improving and evaluating
CE. There is no national entity dedicated to advancing the science of
CE as there is for biomedical and clinical research.
Financing CE
The majority of financial support for accredited CME, and increas-
ingly for CNE, derives directly or indirectly from commercial entities.
Pharmaceutical and medical device companies and healthcare pro-
fessionals have inherently conflicting interests in CE. Commercial
entities have a legitimate obligation to enhance shareholder value
by promoting sales of their products, whereas healthcare profession-
als have a moral obligation to improve patient/public health without
concern for the sale of products.
Commercial support for CE:
— Risks distorting the educational content and invites bias.
— Raises concerns about the vows of health professionals to place
patient interest uppermost.
— Endangers professional commitment to evidence-based decision
making.
— Validates and reinforces an entitlement mindset among health
professionals that CE should be paid for by others.
Fletcher
19
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 19

20
— Impedes the adoption of more effective modes of learning.
No amount of strengthening of the “firewall” between commercial
entities and the content and processes of CE can eliminate the
potential for bias.
Academic health centers and other healthcare delivery systems are
not sufficiently attentive, either to their roles in planning, providing,
and assessing CE or to their responsibilities in managing their own
conflicts of interest and those of individual faculty and administrators
when paid by commercial interests for CE teaching.
Accrediting CE
Current accreditation mechanisms for CE are unnecessarily complex
yet insufficiently rigorous. Compared to earlier, formal stages of
health professions education, the CE enterprise is fragmented, poorly
regulated, and uncoordinated; as a result, CE is highly variable in
quality and poorly aligned with efforts to improve quality and
enhance health outcomes.
With the increasing need for inter-professional collaboration,
accrediting bodies of the various health professionals need closer
working relationships.
RECOMMENDATIONS
CE Methods
The CE enterprise should shift as rapidly as possible from excessive
reliance on presentation/lecture-based formats to an emphasis on
practice-based learning.
New metrics are needed:
— To assess the quality of CE. These metrics should be based
on assessment of process improvement and enhanced patient
outcomes.
— To identify high-performing healthcare organizations. The
possibility of awarding CE credit to individual health professionals
who practice in such organizations should be explored.
Chairman’s Summary
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 20

— To automate credit procedures for point-of-care learning.
Federal and state policymakers should provide financial support
for the further development of information technology tools that
facilitate practice-based learning and should strongly encourage all
clinicians to use these tools.
The responsibility for lifelong learning should be emphasized
throughout the early, formal stages of education in all health
professions. Students should be taught the attitudes and skills to
accomplish CE throughout their professional lifetimes.
A national inter-professional CE Institute should be created to
advance the science of CE. The Institute should:
— Promote the discovery and dissemination of more effective
methods of educating health professionals over their profession-
al lifetimes and foster the most effective and efficient ways to
improve knowledge, skills, attitudes, practice, and teamwork.
— Be independent and composed of individuals from the various
health professions.
— Develop and run a research enterprise that encourages increased
and improved scientific study of CE.
— Promote and fund evaluation of policies and standards for CE.
— Identify gaps in the content and processes of CE activities.
— Develop mechanisms needed to assess and fund research
applications from health professional groups and individuals.
— Stimulate development and evaluation of new approaches to
both intra- and inter-professional CE, and determine how best
to disseminate those found to be effective and efficient.
— Direct attention to the wide diversity and scope of practices
with special CE needs, ranging from highly technical specialties
on the one hand to solo and small group practices in remote
locations, on the other.
Fletcher
21
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 21

Chairman’s Summary
22
— Acquire financial resources to support its work and provide
funding for research. Possible funding sources include the
Federal government, foundations, professional groups, and
corporations.
A concerted effort is needed to make the concept of a Continuing
Education Institute a reality. To achieve this, The Institute of Medicine
should convene a group to bring together interested parties to propose
detailed steps for developing a Continuing Education Institute.
CE Financing
Accredited organizations that provide CE should not accept any
commercial support from pharmaceutical or medical device compa-
nies, whether such support is provided directly or indirectly through
subsidiary agencies. Because many professional organizations and
institutions have become heavily dependent on commercial support
for current operations, an abrupt cessation of all such support would
impose unacceptable hardship. A five-year “phase out” period
should be allowed to meet this recommendation.
The financial resources to support CE should derive entirely from
individual health professionals, their employers (including academic
health centers, healthcare organizations, and group practices), and/or
non-commercial sources.
Faculty of academic health centers should not serve on speakers’
bureaus or as paid spokespersons for pharmaceutical or device
manufacturers. They should be prohibited from publishing articles,
reviews, and editorials that have been ghostwritten by industry
employees.
CE Accreditation and Providers
Organizations authorized to provide CE should be limited to profes-
sional schools with programs accredited by national bodies, not-for-
profit professional societies, healthcare organizations accredited by
the Joint Commission, multi-disciplinary practice groups, point-of-care
resources, and print and electronic professional journals.
Existing accrediting organizations for continuing education for
medicine (the Accreditation Council for Continuing Medical
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 22

Fletcher
23
Education) and nursing (the American Nurses Credentialing Center)
should meet and within two years develop a vision and plan for a
single accreditation organization for both nursing and medicine.
The new organization should incorporate the guiding principles for
CE and the recommendations laid out in this report where relevant.
The American Academy of Nursing and the Association of American
Medical Colleges should convene the two accrediting bodies for
this purpose.
Academic health centers should examine their missions to determine
how to strengthen their commitment to CE. They should help their
faculty gain expertise in teaching practice-based learning and incor-
porate information technology, simulations, and interactive
scenarios into their CE activities.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 23

Suzanne W. Fletcher, M.D., M.Sc.*
Harvard Medical School
Chair
________________________________
Barbara F. Atkinson, M.D.
University of Kansas Medical Center
Denise Basow, M.D.*
UpToDate
Waltham, MA
Regina Benjamin, M.D., M.B.A.
Bayou Clinic, Inc.
Bayou La Batre, AL
David Blumenthal, M.D., M.P.P.
MGH/Partners Healthcare System
James A. Clever, M.D.
Marin County, CA
Jordan J. Cohen, M.D.*
Association of American Medical Colleges
Ellen M. Cosgrove, M.D.*
University of New Mexico School of
Medicine
Linda Cronenwett, Ph.D., R.N.
University of North Carolina at Chapel Hill
David A. Davis, M.D.
Association of American Medical Colleges
Catherine D. DeAngelis, M.D., M.P.H.
JAMA and Archives
John Hopkins University
Lyn DeSilets, Ed.D., R.N.-B.C.
Villanova University
F. Daniel Duffy, M.D.*
American Board of Internal Medicine
Harvey Fineberg, M.D., Ph.D.
Institute of Medicine
Grant S. Fletcher, M.D., M.P.H.
University of Washington School
of Medicine
Melvin I. Freeman, M.D.
Virginia Mason Medical Center
Seattle, WA
Michael Green, M.D., M.Sc.
Yale University School of Medicine
Carol Havens, M.D.
Kaiser Permanente Medical Center
Sacramento, CA
Paul C. Hébert, M.D., M.H.Sc.
Canadian Medical Association Journal
Maryjoan D. Ladden, Ph.D., R.N.*
Harvard Medical School
Participants
24
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 24

David Leach, M.D.*
Accreditation Council for Graduate
Medical Education
Donald A. B. Lindberg, M.D.*
National Library of Medicine
Phil Manning, M.D.
Keck School of Medicine of the
University of Southern California
Paul Mazmanian, Ph.D.
Virginia Commonwealth University
Pamela Mitchell, Ph.D., M.S., B.S.
University of Washington
Donald E. Moore Jr., Ph.D.
Vanderbilt School of Medicine
Ajit K. Sachdeva, M.D.
American College of Surgeons
Marla E. Salmon, Sc.D., R.N.
Emory University
David C. Slawson, M.D.
University of Virginia
Robert Steinbrook, M.D.
New England Journal of Medicine
William Tierney, M.D.
Indiana University School of Medicine
Thomas R. Viggiano, M.D., M.Ed.
Mayo Clinic
Susan Wesmiller, M.S., R.N.
University of Pittsburgh Medical Center
Michael Wilkes, M.D.
University of California, Davis
Patricia S. Yoder-Wise, R.N., Ed.D.
Texas Tech University Health Sciences Center
MACY FOUNDATION
June E. Osborn, M.D.*
Marc A. Nivet, Ed.D.
Nicholas R. Romano, M.A.
Mary Hager, M.A.
*
Planning Commitee
Macy Conference participants are invited for their individual perspectives
and do not necessarily represent the views of any organization.
25
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 25

26
Conference Images
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 26

27
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 27

28
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 28
I.
Approaches to
Knowledge Development
—
What Works and
What Does Not
29
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 29

30
How Physicians Learn and How to
Design Learning Experiences for Them:
An Approach Based on an Interpretive
Review of Evidence
Donald E. Moore, Jr., Ph.D.
Vanderbilt School of Medicine
Researchers from multiple studies over the past several years have
reported that there are distressing gaps between the healthcare services
that patients receive and those that they could be receiving.
1,2
These
studies show that many patients do not receive the best possible
care, receive suboptimal care, or are victims of errors, despite the
fact that approaches to care are improving and demonstrating
enhanced outcomes. A variety of approaches have been suggested
to address this gap.
3
Continuing medical education (CME) has been
a longstanding suggestion. For many years, however, people have
expressed concerns about the effectiveness of CME. As a result,
confidence in the ability of CME to address the identified gaps in
healthcare delivery was not high. But significant work over the past
20 years has demonstrated the effectiveness of CME, if it is planned
and implemented according to approaches that have been shown
to work.
4–6
This interpretive essay reviews the evidence that describes how
physicians learn and proposes six principles from that evidence and
research from other fields that can be used to plan formal educational
activities designed to facilitate physician learning. Next, the essay
proposes an instructional design approach for designing effective
formal CME activities. Finally, the essay briefly discusses assessment
of formal CME activities. See Appendix A for a brief review of the
evidence on how nurses and pharmacists learn.
How Do Physicians Learn?
At any given time, physicians are engaged simultaneously in several
different kinds of learning. Systematic reading, self-directed improve-
ment at work, participation in formal CME courses, and consultation
with colleagues are woven into the basic fiber of their professional
lives to create an approach to learning that is unique to each individual
physician. Studies on physician learning have revealed that the
learning process consists of several stages. In general, these stages
begin with a physician learner becoming aware of a problem or
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 30

R
ecognizing
a
n Opportunity
for Learning
S
earching for
R
esources
for Learning
E
ngaging
i
n Learning
T
rying Out
W
hat Was
Learned
I
ncorporating
W
hat Was
Learned
Priming
Reflecting-in-action
Reflecting-on-
action
Awareness
Priming
Pre-awareness
Awareness
Scanning
Awareness
Felt need
Felt need
Articulate a
problem
Awareness
Pre-contemplation
Contemplation
Experiencing
Reflecting
Focusing
Decision to pursue
information
Actively seeking
a solution
Decision-making
Preparing to
make a change
Follow-up
Agreement
Evaluating
Obtain
knowledge about
an innovation
Search for
solutions
Information
seeking
Interest
Preparation
Conceptualization
Planning
Focusing
Develop
learning project
Making the
change
Follow-up
Learning
Obtain
knowledge about
an innovation
Preparation
Planning
Follow-up
Solidifying the
change
Follow-up
confirmation
Adoption
Gaining
experience
Favorable opinion
about the
innovation
Decision to adopt
or reject
Choice
Evaluation
Trial test
Action
Problem
resolution
Solidifying the
change
Adherence
Gaining
experience
Implementation
Confirmation
Application
of solution
Adoption
Integration
Maintenance
G
eertsma
et al
1
982
1
5
Schon
1983
16
Means
1984
17
Putnam,
Campbell
1989
1
8
Garcia,
Newsom
1996
19
Pathman
et al
1996
20
Slotnick
1999
21, 22
Rogers
1962
23, 24
Havelock
et al
1969
25, 26
Havelock
et al
1973
25, 26
Prochaska
1983
27-29
Kolb
1984
30
Table 1. Stages of Learning
S
tudies on Physician Learning
Studies on How People Learn
Moore
31
challenge and end when all stages are completed, with that physician
learner comfortably and confidently applying newly learned knowl-
edge and/or skills (Table 1).
Stage theories are used commonly in the social and behavioral
sciences.
7
A stage theory describes a social or behavioral process
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 31

in terms of the collection of activities that an individual must pass
through in order to successfully complete that process. Descriptions
of learning as a process that includes several stages have been in
the educational literature at least since the early 1950s.
8
Tough,
9–11
Knowles,
12
and Knox
13
have reported stage learning projects of
adults who planned and directed the projects, consisting of multiple
stages, for themselves.
There is a danger of oversimplification when describing a complicated
process like learning as a straight line that “flows” from stage to stage.
In fact, the process of learning is extraordinarily complex, and it is
made even more complex because it is embedded in a social context.
It is more dynamic, with many interactions among the stages and
within the stages. The system dynamics model described by Hirsch
and his colleagues
14
is probably a more accurate way to depict the
process. For the purposes of this monograph, however, we use the
more static approach because the studies we are reviewing were
reported in that way, and while possibly oversimplified, this
approach helps us understand the process at a very macro level.
The findings of seven studies that examined physician learning and
five studies that examined how people learn are summarized in Table1.
These studies revealed that learning begins with an individual becoming
aware of a problem or challenge and ends when all stages are com-
pleted, with that learner comfortably and confidently applying newly
learned knowledge and/or skills. We propose a five-stage model
that synthesizes the stages identified in the studies reviewed here. The
five stages are reflected as the headings of Table 1: 1) recognizing
an opportunity for learning; 2) searching for resources for learning;
3) engaging in learning to address an opportunity for improvement;
4) trying out what was learned; and 5) incorporating what was learned.
It is a precarious endeavor to synthesize the results of studies con-
ducted by others in an attempt to create a working theory. There
are dangers of over-interpreting some studies and under-interpreting
others. There is also a danger of making assumptions that the original
researchers did not intend. In addition, each of the models presented
has its own characteristics and features, which may be overemphasized
or underemphasized in the synthesis. Furthermore, the stages proposed
may contain part of a stage from one study and two stages from
another study. The following paragraphs describe these stages in
more detail as they relate to physician learning.
32
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 32

Stage 1: Recognizing an opportunity for learning
This is the initial stage of the process of physician learning. In this
stage, a physician begins to sense that there may be something in
his or her practice that is “not right” and may begin to consider
learning as a way to address it. The term “scanning” describes the
sometimes conscious, sometimes subconscious examination of a
physician’s practice and his or her professional environment that
results in a state of dissatisfaction with some aspect of the practice
or practice performance. Scanning may be passive, when a physician
reacts to surprises in practice or “feels” that something may not be
right, or it may be more active, when the physician is actively engaged
in examining areas that he or she has identified as opportunities for
improvement. The terms “reflecting-in-action” and “reflecting-on-
action” describe what a physician does when he or she becomes
“aware” that something is not right with the management of a patient
or group of patients, or if there might be a better way to manage a
patient. The product of reflection is an ongoing “articulation” of a
problem that describes the feeling that something is not right as a
difference between “what should be” and “what is”— what psychol-
ogists call “cognitive dissonance.”
31
For physicians in practice, “what
is” and “what should be” can be described in terms of performance
in practice or patient outcomes. Dissonance is associated with
discomfort that causes action to search for a solution to reduce the
discomfort. In a physician, cognitive dissonance will create discomfort,
which, in turn, will lead the physician to search for knowledge that will
make it possible to reduce the discrepancy and the discomfort.
17,32,33
Another way to describe what happens during this stage is to say
that a “teachable moment” emerges. A teachable moment is defined
as the time when a learner’s psychological readiness for learning is
highest.
34
The strength and persistence of the teachable moment will
determine whether a physician will move to the second stage.
What causes a physician to move from recognizing that there is an
opportunity for learning to starting the process to pursue learning?
The strength and persistence of cognitive dissonance, or the teachable
moment, is important, but there are a variety of other issues and
considerations that affect the decision to pursue learning.
35
In the
general adult education literature, Cross
36
suggested that an indi-
vidual is more likely to participate in an educational activity if he or
she 1) possesses positive attitudes about education; 2) considers an
educational activity relevant to his or her educational need; 3) sees
33
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 33

more opportunities than barriers to participate; and 4) expects to be
successful in learning what he or she needs to learn to address the
educational need (cognitive dissonance) that initiated the search for
a learning opportunity. In the medical literature, Gorman suggests
that physicians will pursue learning if they believe that there is
something to be learned that might resolve the discrepancy at hand,
but they are not inclined to seek answers when they do not believe
that useful information exists.
37
Fox and his colleagues reported that
if a physician perceives learning and the results of learning to be
rational, relatively easy to achieve, and in the best interest of his or
her patients, the physician would be more likely to pursue learning.
If learning is coerced, however, by regulation or administrative
requirements, a physician’s participation would likely be minimal
and grudging. Moore and colleagues saw the decision to participate
in formal CME as part of information-seeking efforts and described
a complex transactional process in which the costs and benefits of
participation were compared at several levels.
38
During this stage, questions may emerge for physicians like “Am I
treating patients (in this disease area) correctly?” “How are my
patients (in this disease area) doing?” “What are the acceptable
standards of care (in this disease area)?” “Is there anything “new”
in this disease area?” And, “What’s important in all this information
that I am hearing about this disease area?”
39
Stage 2: Searching for resources for learning
Practicing physicians seek to address problems they identify for
themselves by starting a search for resources for learning, framed
by these problems stated as questions, articulated at varying levels
of clarity. A question could focus on any number of the components
of patient management: pre-diagnostic evaluation, diagnosis, treat-
ment, or follow-up. A physician seeking information in any of these
areas might be concerned about declarative information (knowledge
base) but is more likely concerned about procedural information
(knowledge about how to use the knowledge base). In addition, a
physician seeking information may be seeking that information as
new knowledge to update his or her current knowledge or to rein-
force current knowledge.
40
During this stage, a physician prepares to make a change to address
the problem he or she has articulated by trying to understand it
34
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 34

and estimating what would have to be learned to address it. The
physician becomes aware of alternative approaches to address the
identified problem, decides which approach to use, and selects
resources to learn about that approach.
A physician begins to develop an image of the change in behavior
that is necessary to address the problem identified during stage 1
and how learning will help accomplish that change.
41
Slotnick found
that during this stage, a physician evaluates the problem or question
to determine whether pursuing learning will be beneficial. Slotnick
suggests that a physician determines the benefits by asking the fol-
lowing questions:
— Does the problem likely have a solution?
— Are resources available to learn the solution to the problem?
— Will learning the solution change my practice in
desirable ways?
If a physician responds to these questions with positive answers, the
next step will be to determine whether she needs to learn something
to make a change. With the image of change in mind,
41
the physi-
cian will determine the extent to which he or she is able to make
the change without learning (her capabilities are adequate) or the
extent to which she will have to pursue learning (she feels that her
capabilities are not adequate). A physician at this stage will assess
her capabilities in a number of ways, including personal reflection,
feedback, and interaction with colleagues, as well as personal,
community, and professional expectations.
42
In addition, a physician
may assess her capabilities while engaged in CME activities, such
as reading journals, attending a formal CME activity, and partici-
pating in a Web-based CME activity. Slotnick suggests that the
physician would ask the following questions:
— What’s important in all this information that I am hearing,
reading, or viewing?
— What experiences have other physicians had doing what I am
hearing about?
— What is the best way to learn?
At the end of this stage, a physician has evaluated the problem or
question that precipitated the search for learning resources, deter-
35
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 35

mined whether pursuing learning would be beneficial, and decided
what type of learning to pursue.
Stage 3: Engaging in learning
During the entire five-stage process, a physician manages the pattern
of formal and informal resources that he or she finds most effective
to address the opportunity for learning that started the process.
43
Learning becomes more focused, intentional, and formal during this
stage. Physicians learn informally as well as in formal settings.
44
Informal learning consists of (but is not limited to) casual journal
reading, ad hoc conversations with colleagues, interactions with
industry representatives, and attendance at grand rounds and other
regularly scheduled conferences. Some informal CME focuses on
specific patient problems and is more structured, such as consultations
with colleagues and focused reading of journals or textbooks. Formal
CME is usually planned in some detail and consists of CME activities
planned by the physician learner or by someone else. Formal CME
activities planned by the physician learner would include preceptor-
ships in which educational activities are negotiated between the
learner and the preceptor and learning projects like the Maintenance
of Competence Program (MOCOMP) of the Royal College of Physi-
cians and Surgeons of Canada, in which a physician identifies an
opportunity for improvement, designs learning activities directed at
the improvement, and assesses accomplishments.
45–49
Other educa-
tional activities planned by the learner are those in the maintenance
of certification programs of specialty societies that are members of
the American Board of Medical Specialties (ABMS).
50
CME activities
planned by others include formal CME courses and enduring materials.
Questions that emerge during this stage include but are not limited
to the following: “Is this educational activity addressing what I need
to learn?”; Is the content based on evidence from research?”; “What
do other participants think about what is being presented?”; How
does what is being presented relate to my patients?”; “Is this all I
have to learn?”; “Does what is being presented actually work?”; and
“How will what is being presented change my practice?”
Stage 4: Trying out what was learned
In this stage a physician begins to use newly learned skills and
knowledge to address the problem that precipitated the learning
36
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 36

process. During this stage a physician develops a favorable
opinion about what she has learned and makes a decision to
accept it or reject it. She experiments with what she has learned
in her practice setting but not before confirming the benefits of
what she has learned with colleagues. The stage begins with a
physician being less than comfortable with her new skills and
knowledge. As she progresses through the stage, however, she
will become more skillful and confident with what she is doing.
The stage is over when the physician is sufficiently comfortable
with the newly learned skills and knowledge and they become
second nature.
During this stage a physician is likely to rely more on her own
reflections and conversations with colleagues than the other resources
she used during the learning process.
51,52
Questions she might ask
during this stage include the following:
— How does what I have learned apply to my practice?
— What do I have to do in my practice to use what I have
learned?
— Am I doing it right?
— Does it work?
An important part of this trial and evaluation stage for a physician is
determining not only how to use what she has learned but also
whether it works in her setting. If the physician’s practice uses an
electronic medical record or other digital databases for monitoring
performance and patient outcomes, she will be able to determine
the effectiveness of the new learning. But it is more likely that she
will “reflect-on-her-practice” after several “experiments,”
16
and if the
new learning appears to be effective, will move on to the next stage.
This stage raises interesting ethical issues. One might ask what the
responsibility of a CME program is to ensure that every participant
has the opportunity to practice until confident in an environment in
which patients are not endangered by physician experimentation
“until he or she gets it right.”
Stage 5: Incorporating what was learned
During this final stage, a physician integrates what he has learned
into his daily routines; it will become a part of what he does when
37
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 37

How Physicians Learn and How to Design Learning Experiences for Them
38
managing patients. Questions that emerge in this stage include but
are not limited to the following: What do I have to do differently
in my practice to use what I have learned? How do I make what I
have learned a part of my practice? What office routines have to
be changed? What new procedures have to be introduced? What
training does staff need? And, what do I have to do for my patients?
If the physician has not done so already in the previous stage, during
this stage, a physician will have to make sure that office routines
and procedures include not only what he has learned but also what
he will need to implement what he has learned. Most important, he
will need to train his staff in what he has learned.
Principles for Facilitating Physician Learning in Formal CME
As the research summarized here suggests, physician learning is
predominantly self-directed. Physicians engage in CME activities
because they want to learn something that will help them provide
the very best possible care to their patients, not because someone
has told them what to learn. In most cases, physicians proceed on
their own through the five stages of self-directed learning described
here, consulting a variety of resources, but essentially planning and
directing the learning project in which they are engaged on their
own. In many cases, physicians choose to enroll in a formal CME
activity that has been planned by someone else. The most effective
formal learning experience for physicians would take into account
where a physician is in his or her learning process (what stage) and
what will help him or her accomplish learning goals. The principles
summarized in the following paragraphs are drawn from the studies
reviewed in the previous section of this monograph as well as from
studies that have examined learning in general.
Principle 1: Planners of formal CME should consider physicians’
stages of learning.
Typically, CME planners asssume that all physicians who enroll in a
CME activity are at stage 3, engaging in learning, and need informa-
tion. In reality, a physician who enrolls in a formal CME activity
could be at any one of the five stages of learning and would have
questions related to his stage (Table 2). To make the learning expe-
riences of physicians more productive, CME planners should help
physicians recognize what stage they are in and plan activities to
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 38

Recognizing
an Opportunity
f
or Learning
Searching for
Resources
f
or Learning
Engaging
in Learning
Trying Out
What Was
L
earned
Incorporating
What Was
L
earned
Am I treating patients
(
in this disease area)
correctly?
H
ow are my patients
(in this disease area)
doing?
What are the
a
cceptable standards
o
f care (in this
disease area)?
Is there anything
“new” in this
disease area?
What’s important
in all this information
that I am hearing
about this disease
area?
Is this a problem
f
or me?
D
oes this problem
have a solution that
can be addressed
b
y learning?
Are there resources
a
vailable for learning
t
he solution?
Can I learn the
solution?
What’s important
in all this information
that I am hearing
about this disease
area?
What do I need to
learn?
What is the best way
to learn?
What experiences
have other
physicians had
with this problem?
How will learning the
solution change my
practice?
Is this educational
a
ctivity addressing
what I need to learn?
I
s the content based
on evidence?
What do the other
p
articipants think
a
bout what is being
presented?
How does what
is being presented
relate to my
patients?
Is this all I have
to learn?
Does what is being
presented work?
How will what is
being presented
change my practice?
How will what is
being presented
change my practice?
Am I doing what
I
am learning
correctly?
H
ow will I be able
to do what I am
learning in my
p
ractice?
Does what I am
l
earning to do work?
What do I have to
d
o differently to use
what I have learned
in my practice?
H
ow do I make what
I have learned a
part of my practice?
What office routines
h
ave to be changed;
w
hat new
procedures have
to be introduced?
What training does
staff need?
What do I have to
do for patients?
What do I have to
do for patients?
Table 2. Questions Physicians Have at Each Stage of Learning
Adapted from Slotnick
39
Moore
39
address the questions they have that are associated with that stage.
A physician would initiate the five-stage learning process for
problems related to specific patients and for more generalized
patient-related issues. The process that results for each is slightly
different. For problems related to specific patients (Why is Mrs.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 39

Jones not responding to her hypertension medication?), a physician
would likely use resources in his office (journals, textbooks, online
resources) and local consultants in almost all stages. The physician
would typically enroll in a formal CME activity for learning initiated
by a more general patient-related problem (Why are the hemoglobin
A1c levels of my diabetes patients consistently high?).
51
With respect to a general patient problem, some physicians might
be at stage 1, recognizing an opportunity for learning, or not yet
at stage 1. These physicians would benefit from information that
would help them recognize or create a teachable moment. Many
physicians who are at stage 2, searching for resources for learning,
may have difficulty articulating the opportunity for learning they
recognize into questions that can lead to a productive search for
information and an effective educational experience.
21,25,52–54
CME
planners should design experiences that allow physicians to translate
what they are feeling about their practice behavior into questions.
Some physicians may find answers for the questions they develop
as part of the CME activity, while for others the questions may
remain. For the latter group, it is important for the CME activity
to help with that search.
Other physicians may be at stage 3, engaging in learning. At this
stage, a physician already has formulated questions. The CME activity
should be designed to provide the conditions in which this physician
can create the knowledge necessary to answer those questions.
Physicians who are at stage 4, trying out what was learned, will
benefit from an opportunity to practice using what they have learned.
Practice in an educational setting will prepare them to transfer new
learning when they return to their practice setting. If physicians at
stage 5, incorporating what was learned, are enrolled in a CME
activity, it is important to provide them with information or resources
showing how to integrate new approaches into a practice.
Physicians may decide to discontinue activities within a stage or
stop the entire learning process itself when they feel they have
learned enough to pass on to the next stage or deal with the prob-
lem that precipitated the learning process, or they may decide that
the benefits from learning are not worth the efforts.
55
Maintaining
motivation is important if physicians are to persist in learning through
all five stages and change their behavior based on that learning.
40
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 40

The physician was motivated to initiate the learning process because
of cognitive dissonance. Frequent reminders are an important part
of the educational activity to show that progress is being made in
closing the gap between “what is” and “what should be” that created
the cognitive dissonance. Linking feedback and motivation is the
key to a successful educational experience.
Principle 2: Formal CME activities should focus on clinical
problems and should provide information that physicians can
use in practice.
Practicing physicians are in a more or less continuous search for
information that they want to use to solve problems or address
opportunities for improvement in practice.
56
They may be at any one
of the five stages described earlier. Regardless of what stage they are
in, physicians are interested in clinical issues, not necessarily a detailed
description of the basic science or clinical research that led to the
finding that has clinical implications.
When physicians select learning resources in their self-directed
learning projects, one of the features that is important to them is a
focus on clinical issues.
27,51,57–60
This is useful to consider when
planning formal CME activities where physicians may be in any one
of the five stages of learning.
Principle 3: Formal CME activities should be organized to provide
opportunities to obtain knowledge and develop skills in settings
and applications that would normally involve the use of that
knowledge and/or those skills.
The ultimate goal of an effective formal CME activity is for the
physician to apply what he or she has learned in the practice, and
not just retain the facts. Like other learners, physicians are more
likely to learn and change their behavior if the learning experience
closely resembles the setting in which the learning will be used.
Physicians learn in relation to what else they know, believe, and
have experienced — the settings and applications that would nor-
mally involve that knowledge. They will transfer what they have
learned in an educational setting to a work setting more readily
when the educational setting is designed as an “authentic” work
setting.
61
Physicians will learn more effectively in this setting by
deriving insights from clinical practice with the help of CME faculty
41
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 41

who demonstrate how to reflect on a problem, identify the most
feasible solution, use the solution in a real-world setting, and assess
the effectiveness of the chosen solution. CME planners should work
with faculty to create authentic settings that will engage the learner
in complex, realistic, “messy,” problem-centered activities and create
a setting that will be familiar and in which physician learners can
recognize what they need to learn and begin the process of transfer-
ring learning to their practice settings.
Principle 4: Formal CME activities should provide opportunities
for active learning.
Like other learners, physicians learn best by doing.
2
1
Actively involv-
ing learners is more effective than simply disseminating concepts
and principles. Teachers should function more as facilitators of
learning than as disseminators of facts.
62,63
CME planners should not
only provide an authentic setting in formal CME activities but should
also provide physicians with opportunities to interact within that
setting. Because the goal is for physicians to apply what they have
learned in a formal CME activity in a dynamic social environment —
the practice setting — a formal CME activity will be more effective in
accomplishing this goal if it is planned as a social process dependent
on transactions with others within a context that resembles as closely
as possible the practice environment. Indeed, CME course design
and materials should permit and encourage physicians to explore
the new content, their own experience, and the experiences of
other physician learners. The choice of a particular method is not
as important as providing the opportunity for learners to practice
what they have learned and to receive feedback on their efforts.
Active learning is more effective than passive learning for several
reasons. First, it draws on the experience and previous knowledge
of the learners. Second, it recreates the social environment within
which the new information will be used. Third, it provides an
opportunity for practice and feedback, two activities essential for
learning and transferring that learning to action. Fourth, it permits
the physician learners to engage at their own stage of learning.
Learning is more effective if the experience and previous knowledge
of the learners is taken into account. Active learning formats in
formal CME activities facilitate the incorporation of a learner’s previous
knowledge and experience into learning activities. Learning is a
42
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 42

social activity. Learning is intimately associated with an individual’s
connection with other human beings, including colleagues, teachers,
peers, and family, as well as casual acquaintances, and physicians
attend CME activities because doing so provides opportunities to
talk with others sharing their interests.
1
Learning requires both practice and feedback. Again, like other
learners, physicians are more likely to learn if they are given an
opportunity to practice and receive feedback. For effective learning
to occur, there must be opportunities for practice as well as positive
feedback when something is performed correctly, and negative
feedback given constructively when something is performed incor-
rectly. In addition, practice provides opportunities to reflect on the
task at hand as well as past experience — to understand not only
what happened, but also why it happened.
In an active learning environment, physicians can feel vulnerable
and resist participation because they fear being exposed for lack
of knowledge or posing an incorrect solution to a problem encoun-
tered as part of an educational exercise. An individual must feel
safe before effective learning can occur.
64
An important part of the
andragogical approach developed by Malcolm Knowles is creating
a climate comfortable for learning and the learners.
12
Permitting
each participant to maintain his or her level of self-esteem is crucial
to creating conditions for learning.
Principle 5: Effective CME activities are more likely to consist of
multiple educational activities that are organized according to
an instructional design plan.
The results of several systematic reviews suggest that physicians are
more likely to learn and use what they have learned in their practices
if they participate in multiple learning activities on a single topic.
65–67
A recent systematic review suggests, however, that this may not
always be true.
3
The issue may not be so much how many activities,
but rather how the activities are organized. Instructional design
provides suggestions not only for what educational methods and
techniques are most likely to result in desired learning outcomes
but also how to organize them.
4
Conventional approaches to planning CME, loosely based on the
approach described by Malcolm Knowles,
68,69
focus only on the
43
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 43

R
ecognizing
an Opportunity
for Learning
S
earching for
Resources
for Learning
E
ngaging
in Learning
T
rying Out
What Was
Learned
I
ncorporating
What Was
Learned
Table 3. CME Planning that is Responsive to Questions that
Physician Have at Each Stage of Learning
PREDISPOSING
1. How are my patients
(in this problem area) doing?
(Stage 1)
2. Am I treating patients
(in this problem area) correctly?
(Stage 1)
3. What are the acceptable
standards of care (in this
problem area)? (Stage 1)
4. Is there anything “new”
in this problem area?
(Stage 1)
5. Does this problem have a
solution that can be addressed
by learning? (Stage 2)
6. What experiences have
other physicians had with
this problem? (Stage 2)
7. Are there resources available
for learning the solution?
(Stage 2)
8. Can I learn the solution?
(Stage 2)
9. What is the best way to learn?
(Stage 2)
10. What’s important in all this infor-
mation that I am hearing about this
problem area?(Stages1 and2)
ENABLING
1. What do I need to learn?
(Stage 2)
2. How will what is being
presented change my
practice? (Stage 2)
3. Is this educational activity
addressing what I need to learn?
(Stage 3)
4. Does what is being presented
work? (Stage 3)
5. Is the content based on
evidence? (Stage 3)
6. What do the other participants
think about what is being pre-
sented? (Stage 3)
7. How does what is being present-
ed relate to my patients?
(Stage 3)
8. How will learning the solution
change my practice? (Stage 2)
9. Am I learning?
(Stage 3)
10. Is this all I have to learn?
(Stage 3)
11. Am I doing what I am learning
correctly? (Stage 4)
12. What do I have to do differently to
use what I have learned in my
practice? (Stage 4)
13. What’s important in all this infor-
mation that I am hearing about
this problem area? (Stages 2, 3,
and 4)
REINFORCING
1. Does what I am learning
to do work? (Stage 4)
2. How do I make what I have
learned a part of my practice?
(Stage 5)
3. What new procedures have
to be introduced?
(Stage 5)
4. What office routines have to
be changed? (Stage 5)
5. What training does staff need?
(Stage 5)
6. What do I have to do differently
for patients? (Stage 5)
7. How will I be able to do what
I am learning in my practice?
(Stage 5)
8. What’s important in all this
information that I am hearing
about this problem area?
(Stages 4 and 5)
C M E P L A N N I N G
How Physicians Learn and How to Design Learning Experiences for Them
44
stage of the learning process when a physician is “engaged in learn-
ing” (stage 3). See Table 3. Davis and colleagues
7
0,71
observed,
however, that in effective CME, multiple educational activities were
organized as predisposing, enabling, and reinforcing, following
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 44

Moore
45
the PRECEDE-PROCEED framework developed by Green and
colleagues.
7
2
This observation has been reinforced by positive
findings in studies reported by Mann and colleagues,
73
White,
74
and
Cantillon.
75
The predisposing-enabling-reinforcing paradigm appears
to match well with the stage learning theories described by researchers
investigating how physicians learn. Predisposing activities relate
to stage 1 and most of stage 2; enabling activities relate to some
of stage 2, all of stage three, and some of stage 4; and reinforcing
activities relate to most of stage 4 and all of stage 5. Before engaging
in learning, most physicians feel a need to learn (cognitive disso-
nance); they become predisposed to learn. While engaging in learning,
physicians strive to learn what to do and how to do it so they
become enabled to do what they did not know how to do before.
And most physicians will seek reinforcing comments from peers
or local opinion leaders after learning something new and trying it
in practice.
Principle 6: Learning is enhanced if content is organized
in small units.
Learning tasks should be organized in such a way that what is to be
learned is presented in small amounts, so that each unit will be mas-
tered before the next one is considered. Cognitive scientists have
called this “chunking” and suggest that it improves the efficiency of
working memory.
76
External information (sensory input) must first
be processed by short-term memory. When short-term memory is
overloaded, learning can be difficult. Overload can be eliminated by
reducing or pacing sensory input. Designing formal CME activities in
15-minute modules would modulate sensory input and contribute to
improved learning conditions.
Designing Effective CME:
A Proposed Instructional Design Approach
No single tested theory exists that CME planners and others could
use as a guide for planning educational activities.
77
Several studies
have contributed to an emerging theory of how physicians learn,
some of which were reviewed in the first section of this paper.
Other studies have suggested what contributes to effective CME,
and additional studies have reviewed the effectiveness of various
educational techniques in CME. However, the findings from these
studies do not appear to have been combined, synthesized, hypoth-
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 45

Presentation Techniques
• Lecture
• Panel
Interactive Techniques
• Teaching and learning from cases
Case presentation
Case discussion
• Small group discussion
Skill Development Techniques
• Presentation
• Demonstration
• Practice
• Feedback
Table 4. Educational Methods in Formal CME
How Physicians Learn and How to Design Learning Experiences for Them
46
esized, and tested in a way that would produce a theory on which
instructional design decisions in CME could be confidently based.
This section represents an attempt to combine and synthesize the
material presented in previous sections into a proposed approach
for CME instructional design.
Educational methods used in formal CME activities traditionally fall
into three broad categories: presentation methods, interactive methods,
and skill development methods (Table 4). Presentation methods
are used when learning objectives call for knowledge acquisition.
Interactive methods are used when the intent is to increase under-
standing of educational content and improve the chances that it
will be applied in the practice setting. The most common interactive
method in medical education is teaching and learning from cases.
Two formats are useful in CME: case presentation and case discussion.
In a case presentation, information about the experience of managing
a patient with a specific disorder is reported to the audience in a
presentation format. Case discussion engages members of the audi-
ence in decision making about a case. Skill development methods
are used to help learners develop and use a skill. These methods
can be used to help learners develop cognitive skills, for example
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 46

Moore
47
deciding to prescribe an ACE inhibitor for patients with congestive
heart failure; interpersonal skills, like obtaining a sexual history
from an adolescent; or psychomotor skills, like performing flexible
sigmoidoscopy or a new cardiac surgery technique. Merrill suggests
that there are four components of effective skill development, referred
to here as presentation, demonstration, practice, and feedback.
78
Although presentation methods, such as lectures, panels, and printed
materials, may not change physician behavior when used alone, they
continue to be the most prevalent method for CME. When presentation
methods are made more interactive through case presentations or
group discussion, moderately large changes in professional practice
can result. No systematic review of skill development methods has
been performed, but evidence from the literature suggests that multiple
CME activities focused on a single topic organized following the
predisposing-enabling-reinforcing model are effective in changing
physician behavior.
To make the learning experiences of physicians more effective,
CME planners should use the predisposing-enabling-reinforcing
framework to align learning activities with physician learning stages.
At each learning stage, physicians have specific questions, some
more conscious and articulated than others. In Table 3, the questions
listed in Table 2 under columns related to the stage of learning have
been resorted and placed under columns labeled “Predisposing,”
“Enabling,” and “Reinforcing.” The instructional design approach
described here involves identifying content to answer the questions
and determining the best way to help physicians learn that content,
drawing on what has been described about how physicians learn,
principles that describe how to facilitate physician learning, and
educational methods that have been effective in CME.
Planning predisposing CME activities
As mentioned earlier, predisposing activities appear to relate to all of
stage 1: recognizing an opportunity for learning, and part of stage 2,
searching for resources for learning. As a result, the questions that
need to be addressed to design predisposing learning activities are all
of the questions in stage one and some of the questions from stage
two. See Table 5 for a list of the questions, the content that could
address the questions, and suggested educational methods for each
question.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 47

Table 5. Planning Pre-disposing CME Activities
Q
UESTION
1
. How are my patients
(in this problem area) doing?
2. Am I treating patients
(
in this problem area) correctly?
3. What are the acceptable
standards of care (in this
problem area)?
4. Is there anything “new”
in this problem area?
5. Does this problem have a
solution that can be addressed
by learning?
6. What experiences have
other physicians had with
this problem?
7. Are there resources available
for learning the solution?
8. Can I learn the solution?
9. What is the best way to learn?
10. What’s important in all this
information that I am hearing
about this problem area?
CONTENT
R
esults of audit that focus on
p
atient health status and outcomes
in the problem area and information
about those results.
R
esults of audit that focus on
p
hysician performance in the
problem area and information
about those results.
Local or national clinical practice
guidelines (CPGs) in the problem
area.
Findings from studies recently
published in peer reviewed journals
and vetted for level of evidence.
Separation of educational from
non-educational components
of CPGs.
Stories of other physicians.
Information about enabling
activities that have been or will
be designed to address this problem
area. Enabling activities can be
part of a single activity that follows
predisposing activities or part of
a series of activities that occur
at another time.
Information about the enabling
activities that have been developed
that demonstrates that they are
convenient, accessible, and will not
be an unreasonable burden.
Information that shows that the
enabling activities that have been
or will be designed to facilitate
physician learning, and that there
will be activities to reinforce it.
Regular reference to the gap
between current and actual and
how what is being presented
relates to reducing the gap.
EDUCATIONAL METHOD
L
ecture and group discussion
A
cademic detailing
Lecture and group discussion
Academic detailing
Lecture and group discussion
Academic detailing
Lecture and group discussion
Academic detailing
Lecture and group discussion
Academic detailing
Panel
Group discussion
White space on schedule for
informal interactions among
participants.
Recruitment material
Handout
Lecture (testimonial)
Recruitment material
Handout
Lecture (testimonial)
Recruitment material
Handout
Lecture (testimonial)
All methods
How Physicians Learn and How to Design Learning Experiences for Them
48
Planning enabling CME activities
Enabling CME activities appear to relate to all of stage three, engaging
in learning; parts of stage 2, searching for resources for learning;
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 48

Table 6. Planning Enabling CME Activities
Q
UESTION
1
. What do I need to learn?
2. How will what is being
presented change my practice?
3. Is this educational activity
addressing what I need to learn?
4. Does what is being presented
work?
5. Is the content based on evidence?
6. What do the other participants
think about what is being
presented?
7. How does what is being presented
relate to my patients?
8. How will learning the solution
change my practice?
9. Am I learning?
10. Is this all I have to learn?
11. Am I doing what I am learning
correctly?
12. What do I have to do differently
to use what I have learned in my
practice?
13. What’s important in all this
information that I am hearing
about this problem area?
CONTENT
S
pecific behaviors that potential
participants would be expected
to perform after participating in
t
he enabling activity, e.g. learning
objectives.
D
escription (in general) of the
i
mplications of what will be learned
during the enabling activity for
practice organization and the people
that work within the practice.
Regular reference to the gap between
current and actual and how what is
being presented relates to reducing
the gap.
Summaries of CPGs or the findings of
studies that demonstrate the efficacy of
what is being presented, i.e., what is
being presented actually produces
desired results. In addition, summaries
should include the level of evidence.
Opinions of other participants.
Description of patients in the studies
reported. Comparison of study
patients with participant’s patients.
Description of the practice organization
in the studies and what the people in
those practices did as part of the study.
Summary of the criteria of
performance, highlighted during the
demonstration and coached during
practice. Information about how the
learner(s) performed the criterion
components of the skill and how to
improve to criterion.
Regular reference to the gap between
current and actual and how what is
being presented relates to reducing
the gap.
EDUCATIONAL METHOD
R
ecruitment materials
Handout
Lecture
Handout
Lecture
Group discussion
Teaching and learning from cases
All methods
Skill development (presentation)
Skill development (presentation)
• Panel
• Group discussion
White space on schedule for informal
interactions among participants.
Skill development (cases)
• Demonstration
• Practice
Skill development (cases)
• Demonstration
• Practice
• Action plan
Skill development (cases)
• Practice
• Feedback
• Action plan
All methods
Moore
49
and stage four, trying out what was learned. As a result, the questions
that need to be addressed to design enabling learning activities are
all of the questions in stage 3 and some of the questions from stages
2 and 4. (Table 6).
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 49
Table 7. Planning Reinforcing CME Activities
QUESTION
1. How will I be able to do what I
am learning in my practice?
2. Does what I am learning to
do work?
3. How do I make what I have
learned a part of my practice?
4. What new procedures have to
be introduced?
5. What office routines have to be
changed?
6. What training does staff need?
7. What do I have to do differently
for patients?
8. What’s important in all this infor-
mation that I am hearing about
this problem area?
CONTENT
Summaries of CPGs or the findings
of studies that demonstrate the
efficacy of what is being presented,
i.e., what is being presented actually
produces desired results. In addition,
summaries should include the level
of evidence.
Results of audit that focus on
physician performance in the
problem area and information about
those results.
• Summaries of CPGs or the
findings of studies that
demonstrate the efficacy of
what is being presented,
i.e., what is being presented
actually produces desired
results. In addition, summaries
should include the level of
evidence.
• Description of patients in the
studies reported. Comparison
of study patients with
participant’s patients.
• Description of the practice
organization in the studies
and what the people in
those practices did as part
of the study.
Regular reference to the gap between
current and actual and how what is
being presented relates to reducing
the gap.
EDUCATIONAL METHOD
Skill development
• Action plan
Reminders
Commitment to change
Lecture and group discussion
Academic detailing
Skill development (cases)
• Action plan
Group Discussion
Reminders
Commitment to change
All methods
How Physicians Learn and How to Design Learning Experiences for Them
50
Designing reinforcing CME activities
Reinforcing CME activities include part of stage 4, trying out what
was learned and all of stage 5, incorporating what was learned.
As a result, the questions that need to be addressed to design rein-
forcing learning activities are some of the questions in stage 4 and
all of the questions from stage 5 (Table 7).
Assessing CME Activities
At the beginning of this paper, the gap between the healthcare that
most Americans are receiving and the healthcare that they could be
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 50

Desired Results
Outcomes Impact
Competence Performance Patient
(Shows how) (Does)
health
status
Inputs
Current
Situation
Intervention
CME Activity
Outputs
• Learning
• Declarative
Knowledge
(knows)
• Procedural
Knowledge
(knows how)
Figure 1. Systems Overview of CME as an Intervention
Moore
51
receiving was identified as a significant problem. CME, designed
according to the model presented here, is one approach to address
the gap. This section offers suggestions on how to determine the
effectiveness of CME activities planned according to the suggested
approach.
“Effective” is a term used to describe an activity that has accom-
plished an intended or desired result or outcome. Something that is
effective is considered to have value. Assessment is the act of judging
something in terms of its worth or value. Assessment can be done at
three levels: the individual physician learner; a single educational
activity; or a program of educational activities that might represent
all of the offerings of an institutional CME provider. At each of these
levels, an educational activity represents an intervention in a situation
to improve it by producing something (outputs) that, when introduced
into the situation, will result in outcomes (competence and perform-
ance) that represent improvements (the desired results), and an
impact (enhanced health status of a group or population of patients).
See Figure 1 for an overview.
A CME activity can produce two potential types of output. The first
is declarative knowledge. An example of declarative knowledge
would be a physician knowing what to do, for example, to manage
the complications of type 2 diabetes. After a CME activity, the physi-
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 51

cian would also be able to state what to do, for example, to examine
the feet of all patients with diabetes (Figure 2). The second type
of output is procedural knowledge. An example of procedural
knowledge would be for the physician to know how to manage
the complications of type 2 diabetes. The physician could describe
how to do it. For example, after participating in a CME activity, the
physician should be able to describe how to examine the feet of
patients with diabetes. Furthermore, if a physician learns procedural
knowledge, four types of desired results are possible: two outcomes
(competence and performance) and two impacts (improved health
status of a group or population of patients). To demonstrate a com-
petence outcome, it would be necessary for a physician to show
how he or she would manage complications of type 2 diabetes, for
example, by examining the feet of a patient with diabetes in the
educational setting. To show a performance outcome, a physician
learner would then be expected to demonstrate what he or she has
learned to his or her associates in the job setting, for example by
examining the feet of all the patients with diabetes in the practice.
The impact of a CME activity or program can be ascertained by
measuring the health status of a group or population of patients, for
example decreased rates of amputations for patients with diabetes.
Figure 2. Levels of Physician Learning and Assessment
DOES
Performance
SHOWS HOW
Competence
KNOWS HOW
Procedural Knowledge
KNOWS
Declarative Knowledge
Adapted from Miller
7
9
How Physicians Learn and How to Design Learning Experiences for Them
52
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 52

Moore
53
When planning to assess a CME activity, it is important to remember
that measurement of competence outcomes should occur in the
educational setting, whereas performance outcomes should be
measured in the practice setting. Impact should be measured in the
practice or community setting. In many cases, it is difficult for a
CME planner to gain access to data or develop instrumentation to
collect objective data. In these cases, data can be obtained through
self report. Self-report data are usually the opinions or perceptions
of individuals and may reflect their biases or “socially acceptable”
responses. Observational methods produce more objective data
from systematic observation and recording of those observations.
Data from self-report methods are not scientifically rigorous, but
they are useful for making judgments about outcomes, especially
if the alternative is no data.
Currently most assessment in CME focuses on outputs: self-reports of
knowledge gained in declarative or perhaps procedural knowledge.
It is difficult to know precisely what percentage of CME assesses
outcomes at the level of competence or performance. The recently
released revised Accreditation Council for Continuing Medical
Education criteria will require assessment of competence, perform-
ance, and health status. Until then, a conservative guess would be less
than 5 percent. Many CME providers do not have access to practice
or community settings where the measurement of performance and
patient health status alluded to in the previous paragraph can be
accomplished. It may be, therefore, that the most realistic outcome
for most providers will be competence, where measurement can
occur in the educational setting.
In the approach described here, a CME activity that is designed to
be effective in accomplishing a competence outcome will provide
learners with an opportunity to practice the skill in which compe-
tence is desired and receive feedback on their level of competence.
While practice and feedback are considered “formative assessment”
for the purposes of planning opportunities for learning, they could
also be considered “summative assessment” for the purposes of
determining if desired results (outcomes) have been attained.
One approach that would create the most realistic setting for a
CME activity to accomplish competence outcomes would be to use
simulated and standardized patients. CME faculty could observe
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 53

physician learners practicing the skill (cognitive, interpersonal, or
psychomotor) with simulated patients and provide feedback to them
as formative assessment to help them understand the level of com-
petence they were functioning at and what they needed to do to
reach the target level. The faculty would then observe the learner
in a final exercise with a standardized patient to confirm that the
target level has been reached.
Not all CME programs have the resources for simulated and stan-
dardized patients. Planners associated with these programs could
consider observing physician learners in live CME activities working
through authentic case scenarios using an audience response system
(ARS) embedded at key decision or observation points in the case.
This would give CME planners a sense of a group’s level of compe-
tence. To determine an individual learner’s level of competence,
one-on-one sessions could be arranged with CME faculty after group
activities are completed. A similar approach could be used for
Webcasts and video or audio conferences. In a Web-based CME
activity, the interactivity and multimedia capability of the Web
provide an opportunity to develop truly authentic case scenarios.
Information technology associated with the Web can function in a
similar way to an ARS.
Many physicians participate in CME through print enduring materials,
like monographs or journal CME. It is challenging to design a CME
activity to achieve competence outcomes in the print enduring
material format. A blended approach might be one in which learn-
ers would read an article or monograph from which they would be
directed to access a site online, where there would be opportunities
for them to assess their competence level. A less desirable approach
would be to develop a paper-based scenario and multiple choice
test that learners could fax or mail to the CME provider.
The preceding paragraphs described how CME activities might be
designed to facilitate the development and assessment of competence.
If a CME activity designed to accomplish competence outcomes
is effective, two questions should be asked: 1) What should be
measured to determine if a physician is competent; and 2) How
should it be measured?
The example of foot care in diabetic patients will help us under-
stand what needs to be measured to demonstrate that physician
54
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 54

learners have accomplished the desired level of competence. The
competence outcome would be showing how to examine the feet
of patients with diabetes so that neuropathy and vasculopathy might
be detected and amputation prevented or delayed. According to the
American Diabetes Association, a “competent” provider would be
expected first to demonstrate the correct techniques for the physical
examination of the feet. The following would be among the impor-
tant items to be checked: pulse; skin temperature; skin appearance
(ulcerations and/or infections); sensation to vibration or slight pain;
proprioception (sense of body position); muscle strength; and
presence of abnormalities (eg, bunions). Second, the learners would
be expected to detect, based on observations, if neuropathy or
vasculopathy is present and show how they would confirm a diagnosis.
Finally, the learners would be expected to develop a management
plan that included follow-up.
80
An observation checklist, adapted
for each of the settings described here, might be the best way to
collect the data.
Concluding Thoughts
This paper has reviewed a wide range of literature on physician
learning, instructional design, and assessment. Physicians engage in
learning in response to problems and opportunities for improving
their practices. A five-stage learning process was developed to
describe the efforts of physicians to address problems encountered
in practice, understand what they need to learn to address those
problems, learn what they need to know and do, experiment with
it, and incorporate it into practice. An approach to instructional
design was proposed as a way to help physicians learn by determining
what content and which instructional methods are most appropriate
for the questions they have at each stage of their learning. The
predisposing-enabling-reinforcing model is one approach to organize
learning activities. An approach to assessment in educational activi-
ties designed to achieve competence outcomes was suggested in
which a summative assessment grew out of formative assessment
that was designed as part of the learning experience.
Recently published work recognizes that CME, no matter how well
planned, cannot produce changes in physician performance and
patient health status by itself.
81
Rather, as the research in CME and
other fields has matured, it has become clear that there are as many
approaches to deal with the many forces acting on physicians and
55
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 55

patients in and around the clinical encounter as there are forces,
and maybe more. The hope of many people in many fields is for
collaboration among the proponents and implementers of these
approaches. Richard Grol and his colleagues have made an important
start by developing a taxonomy in which they categorize these
approaches into two major groups: those that emphasize internal
processes and those that emphasize external influences, reflecting
assumptions about human behavior and how groups or organiza-
tions function.
3
Approaches that emphasize internal processes
include educational, epidemiological, and marketing approaches.
Approaches that emphasize the influence of external approaches
include external influences, social interaction, managerial approach,
and control and compulsion. In addition, theory-driven evaluation,
using the logic model,
82,83
and the newly emerging intervention
science may provide the tools to understand how the collaboration
will work (http://www.implementationscience.com/).
REFERENCES
1. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the
twenty-first Century. Washington, DC: The National Academy Press; 2001.
2. Institute of Medicine. Improving the Quality of Healthcare for Mental and
Substance-use Conditions. Washington, DC: The National Academy Press; 2006.
3. Grol R, Wensing M, Eccles M. Improving Patient Care: The Implementation of
Change in Clinical Practice. Edinburgh: Elsevier; 2005.
4. Mazmanian PE, Davis DA. Continuing medical education and the physician as a
learner: guide to the evidence. JAMA. 2002; 288:1057–1060.
5. Mansouri M, Lockyer J. A meta-analysis of CME effectiveness. J Contin Educ Health
Prof. 2007;27:6–15.
6. Marinopoulos SS, Dorman T, Ratanawongsa N, et al. Effectiveness of Continuing
Medical Education. Rockville MD: Agency for Healthcare Research and Quality; 2007.
7. Flavell JH. Stage related properties of cognitive development. Cognitive Psychology.
2007;2:421–453.
8. Lewin K. Field Theory in Social Science. New York: Harper and Row; 1951.
9. Tough A. The Adult’s Learning Projects. Toronto: Ontario Institute for the Study of
Education; 1971.
10. Tough A. Intentional Changes: A Fresh Approach to Helping People Change.
Chicago: Follett Publishing Company; 1982.
11. Tough A. Major learning efforts: recent research and future directions. Adult
Education Quarterly. 1978;28:250-63.
12. Knowles MS. The Adult Learner: A Neglected Species, 3rd ed. Houston: Gulf
Publishing; 1984.
13. Knox AB. How Adults Learn. San Francisco: Jossey-Bass; 1986.
56
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 56

14. Hirsch GB, Levine R, Miller RL. Using system dynamics modeling to understand the
impact of social change initiatives. Am J Community Psychol. 2007;39:239–253.
15. Geertsma RH, Parker RC, Whitbourne SK. How physicians view the process of
change in their practice behavior. J Med Educ. 1982;57:752–761.
16. Schon D. The Reflective Practitioner: How Professionals Think in Action. New York:
Basic Books; 1983.
17. Means RP. How family physicians use information sources. In Green JS, Grosswald
SJ, Suter E, Walthall DB, editors. Continuing Education for the Health Professions.
San Francisco: Jossey-Bass; 1984:72–86.
18. Putnam RW, Campbell D. Competence. In: Fox RD, Mazmanian PM, Putnam RW, edi-
tors. Changing and Learning in the Lives of Physicians.New York: Praeger;
1989:79–97.
19. Garcia R, Newsom R. Learning and change among emergency physicians. J Contin
Educ Health Prof. 1996;16:33–41.
20. Pathman DE, Konrad TR, Freed GL, Freeman VA, Koch GG. The awareness-to-adher-
ence model of the steps to clinical guideline compliance. The case of pediatric vac-
cine recommendations. Med Care. 1996;34:873–889.
21. Slotnick HB. How physicians learn: physicians’ self-directed learning episodes. Acad
Med. 1999;74:1106–1117.
22. Slotnick HB. Physicians’ learning strategies. Chest. 2000;118(2 Suppl):18S–23S.
23. Rogers EM. Diffusion of Innovations, 5th ed. New York: Free Press; 1995.
24. Lockyer J, Mazmanian PE, Moore DE Jr, Harrison A, Knox AB. The adoption of inno-
vation. In: Davis DA, editor, Physician as Learner: Linking Research to
Practice.Chicago: American Medical Association; 1994.
25. Havelock RG. Planning for Innovation through Dissemination and Utilization of
Knowledge, 6th ed. Ann Arbor: University of Michigan, Institute for Social Research;
1976.
26. Havelock RG. The Change Agent’s Guide to Innovation in Education. Englewood
Cliffs, NJ: Educational Technology Publications; 1973.
27. Prochaska JO, Velicer WF The transtheoretical model of health behavior change. Am
J Health Promot. 1997;12:38–48.
28. Parker K, Parikh SV. Applying Prochaska’s model of change to needs assessment,
programme planning and outcome measurement. J Eval Clin Pract. 2001; 7:365–371.
29. Cohen SJ, Halvorsen HW, Gosselink CA. Changing physician behavior to improve
disease prevention. Prev Med. 1994;23:284–291.
30. Kolb DA Experiential Learning: Experience as the Source of Learning and
Development. Englewood Cliffs, NJ: Prentice Hall; 1984.
31. Festinger L. A Theory of Cognitive Dissonance. Stanford CA: Stanford University
Press; 1957.
32. Knox AB. Proficiency theory of adult learning. Contemporary Educational
Psychology. 1980;5:378–404.
33. Fox RD. Discrepancy analysis in continuing medical education. Mobius.
1983;3:37–44.
34. Hunt D.E. Teachers’ adaptation: ‘Reading’ and ‘flexing’ to students. Journal of
Teacher Education. 1976;27:268–275.
35. Cordes DL. Relationship of motivation to learning. In: Green JS, Grosswald SJ, Suter E,
Walthall DB III, editors. Continuing Education for the Health Professions; 1984:52–71.
36. Cross KP. Adults as Learners. San Francisco: Jossey-Bass; 1981.
57
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 57

37. Gorman PN, Helfand M. Information seeking in primary care: how physicians
choose which clinical questions to pursue and which to leave unanswered. Med
Decis Making. 1995;15:113–119.
38. Moore DE Jr, Knox AB, Bennett NL, Kristofco RE. Factors affecting physician deci-
sion-making to participate in formal CME activities. In: Davis DA, editor. Physician
Learner: Linking Research to Practice. Chicago: American Medical Association;
1994:219–240.
39. Slotnick HB. How doctors learn: physicians’ self-directed learning episodes. Acad
Med. 1999;74:1106–1117.
40. Florance V. Medical knowledge for clinical problem solving: a structural analysis of
clinical questions. Bull Med Libr Assoc. 1992;80:142–149.
41. Fox RD, Mazmanian PE, Putnam RW. Changing and Learning in the Lives of
Physicians. New York: Praeger; 1989.
42. Mann KV, Ribble J. The role of motivation in self-directed learning. In: Davis DA, editor.
Physician as Learner: Linking Research to Practice. Chicago: American Medical
Association; 1994:69–88.
43. Fox RD. New research agendas for CME: organizing principles for the study of self-
directed curricula for change. J Contin Educ Health Prof. 1991;11:155–167.
44. Jennett P, Jones D, Mast T, Egan KL, Hotvedt M. The characteristics of self-directed
learning. In: Davis DA, editor. Physician as Learner: Linking Research to Practice.
Chicago: American Medical Association; 1994:47–66.
45. Campbell CM, Parboosingh JP, Gondocz ST, et al. Study of physicians’ use of a software
program to create a portfolio of their self-directed learning. Acad Med.
1996;71:S49–S51.
46. Parboosingh JP. The maintenance of competence (MOCOMP) program. Can J
Cardiol. 1993;9:695–697.
47. Parboosingh JP. The maintenance of competence (MOCOMP) program. Can J Surg.
1993;36:29–32.
48. Wilkinson TJ, Challis M, Hobma SO, et al. The use of portfolios for assessment of the
competence and performance of doctors in practice. Med Educ. 2002;36:918–924.
49. Dornan T, Carroll C, Parboosingh JP. An electronic learning portfolio for reflective-
continuing professional development. Med Educ. 2002;36:767–769.
50. Miller SH. American Board of Medical Specialties and repositioning for excellence in
lifelong learning: maintenance of certification. J Contin Educ Health Prof.
2005;25:151–156.
51. Slotnick HB, Harris TR, Antonenko DR. Changes in learning-resource use across
physicians’ learning episodes. Bull Med Libr Assoc. 2001;89:194–203.
52. Fox RD, Rankin R, Costie KA, Parboosingh JP, Smith E. Learning and the adoption of
innovations among Canadian radiologists. J Contin Educ Health Prof.
1997;17:173–187.
53. Slotnick HB. Physicians’ learning strategies. Chest. 2000;118(2 Suppl):18S–23S.
54. Slotnick HB. How doctors learn: education and learning across the medical-school-
to-practice trajectory. Acad Med. 2001;76:1013–1026.
55. Slotnick HB. How doctors know when to stop learning. Med Teach.
2000;22:189–196.
56. Slotnick HB, Razskowski RR, Lichtenauer D. Rethinking continuing medical educa-
tion. J Contin Educ Health Prof. 1995;15:8–22.
57. Gruppen LD. Physician information seeking: Improving relevance through research.
Bull Med Libr Assoc. 1990;78:165–172.
58
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 58

58. Haug JD. Physicians’ preferences for information sources: a meta-analytic study. Bull
Med Libr Assoc. 1997;85:223–232.
59. Verhoeven AA, Boerma EJ, Meyboom-de Jong B. Use of information sources by fami-
ly physicians: a literature survey. Bull Med Libr Assoc. 1995;83:85–90.
60. Thompson ML. Characteristics of information resources preferred by primary care
physicians. Bull Med Libr Assoc. 1997;85:187–192.
61. Brown JS, Collins A, Duguid P. Situated cognition and the culture of learning.
Educational Researcher. 1989;18:32–42.
62. Bransford JD, Brown AL, Cocking RR. How People Learn: Brain, Mind, Experience,
and School. Washington, DC: National Academy Press; 1999.
63. Haidet P, Morgan RO, O’Malley KO, Moran BJ, Richards BF. A controlled trial of
active versus passive learning strategies in a large group setting. Adv Health Sci
Educ. 2004;9:15–27.
64. Maslow AH. Toward a Psychology of Being, 3rd ed. New York: Wiley; 1998.
65. Davis DA, Thomson MA, Oxman AB, Haynes RB. Evidence for the effectiveness of
CME. A review of 50 randomized controlled trials. JAMA. 1992;268:1111–1117.
66. Davis D, Thomson M, Oxman A, Haynes R. Changing physician performance. a sys-
tematic review of the effect of continuing medical education strategies. JAMA. 1995;
274:700–705.
67. Thomson MA, Freemantle N, Wolf F, Davis DA, Oxman AB. Educational meetings,
workshops, preceptorships to improve the practice of health professionals and
healthcare outcomes. The Cochrane Library 2001;1.
68. Knowles MS. The Modern Practice of Adult Education: Andragogy versus Pedagogy.
New York: Association Press; 1970.
69. Knowles MS. The Modern Practice of Adult Education: From Pedagogy to
Andragogy. 2nd ed. New York: Cambridge Books; 1980.
70. Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance:
a systematic review of the effect of continuing medical education strategies. JAMA.
1995; 274:700–705.
71. Davis DA, Thomson MA, Oxman AD, Haynes RB. Evidence for the effectiveness of
CME. A review of 50 randomized controlled trials. JAMA. 1992;268:1111–1117.
72. Green LW, Kreuter MW. Health Promotion Planning: An Educational and
Environmental Approach. Mountain View, CA: Mayfield Publishing Company; 1991.
73. Mann KV, Lindsay EA, Putnam RW, Davis D.A. Increasing physician involvment in
cholesterol lowering practices: the role of knowledge, attitudes and perceptions.
Adv Health Sci Educ. 1997;2:237–253.
74. White MI. Toward an evidence-informed, theory-driven model for continuing med-
ical education. The University of British Columbia; 2003.
75. Cantillon P, Jones R. Does continuing medical education in general practice make a
difference? BMJ. 1999;318:1276–1279.
76. Gobet F, Lane PC, Croker S. Chunking mechanisms in human learning. Trends Cogn
Sci. 2001;5:236–243.
77. Mann KV. The role of educational theory in continuing medical education: Has it
helped us? J Contin Educ Health Prof. 2004;24:S22–S30.
78. Merrill DM. Instructional Design Theory. Englewood Cliffs, NJ: Educational
Technology Publishers; 1994.
79. Miller GE. The assessment of clinical skills/competence/performance. Acad Med.
1990; 65(9 Suppl):S63–S67.
59
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 59

80. Boike AM, Hall JO. A practical guide for examining and treating the diabetic foot.
Cleve Clin J Med. 2002;69:342–348.
81. Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interven-
tions to improve the management of depression in primary care: a systematic review.
JAMA. 2003;289:3145–3151.
82. Chen HT. Theory-drive Evaluations. Newbury Park. CA: Sage Publishers; 1990.
83. Chen HT. Practical Program Evaluation: Assessing and Improving Planning,
Implementation, and Effectiveness. Thousand Oaks, CA: Sage Publishing; 2005.
APPENDIX A:
How Nurses and Pharmacists Learn
At the time of this writing, I have not found an exact replica of the
model developed in this monograph for physicians in the nursing
or pharmacy literature. CME has the largest and most robust body
of evidence examining professional learning and effectiveness of
programming. However, I have found interesting and intriguing
parallels in the nursing literature.
Almost all the articles I reviewed mentioned that nurses function in
a complex healthcare environment where social, technological, and
medical changes present them with challenges and that self-directed
learning plays a vital role in ensuring that they respond to these
challenges in appropriate ways.
1
In a small qualitative study (n=24), Daley explored the different
ways that novice and expert nurses learn. The learning of expert
nurses was more “self-directed;” the learning of novice nurses was
more “other-directed.” Daley suggested that as nurses become more
“expert,” their meta-cognition skills become more developed, that
is, they begin to understand better how they learn.
2
While not stated
explicitly in the study that Daley reported, the need reduction and
integration into work approach described in this monograph is usually
associated with self-directed learning projects.
1
It may be that nurses
follow the same five stage process as physicians, but Daley’s study
provides an interesting perspective on the differences between
novice and expert practitioners.
Scanlon and Weir suggest that reflection and self-directed learning can
be facilitated by clinical supervisors who focus on the developmental
needs of nurses rather than disciplinary requirements established by
administration. This is necessary because, according to Scanlon and
60
How Physicians Learn and How to Design Learning Experiences for Them
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 60

Weir, the culture of nursing practice for the most part has become
routinized and automatic. A clinical supervisor, however, could develop
a more reflective nursing practice by helping nurses“reflect-on-practice,”
which they believe would lead eventually to “reflection-in-practice”
becoming part of how a nurse learns from work.
3
Johns suggested that clinical supervisors could help nurses frame
their learning through structured reflection using Carper’s “funda-
mental ways of knowing in nursing” as a heuristic device.
4
Carper’s
fundamental ways are empirical, personal, ethical, and aesthetic
knowing.
5
Empirical knowledge is systematically organized into
general laws and rules that describe, explain, and predict clinical
phenomena. Personal knowing is knowing oneself in the clinical
environment. Knowing of self involves three inter-related factors:
recognizing feelings and prejudices; managing feelings and prejudices
in order to respond properly; and managing anxiety and sustaining
the self. Ethical knowing is knowing what is right or wrong and
being committed to act on this basis. Aesthetic knowing involves
perceiving the nature of a clinical situation, interpreting this infor-
mation, envisioning desired outcomes, and subsequently determining
if the outcomes were effectively achieved. According to Carper, the
aesthetic way of knowing is the core way of knowing in practice,
informed by the empirical, personal, and ethical.
This framework resembles the first stage of the stage model described
in this monograph for physicians, recognizing the need to learn. Both
Scanlon and Weir and Johns state that the purpose of reflecting is
to identify, confront, and resolve contradictions between what practi-
tioners aim to achieve and actual results (cognitive dissonance), with
the intent to achieve more effective work and desirable outcomes. In
their review of literature on continuing nursing education, Furze and
Pearcey state that several studies have found that the primary reasons
for nursing participation in continuing nursing education are to
improve professional knowledge and skills and increase competence.
6
Because this reflecting occurs in the context of an interaction between
a clinical supervisor and a nurse, learning to reduce cognitive
dissonance can begin almost immediately.
In general, Daley found in her study that that novice nurses tend to
learn through more formal mechanisms, including review of policy
or procedures, attendance at continuing education programs, and
reading of journals. Experts seem to use more informal approaches,
61
Moore
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 61

such as consulting with peers and other healthcare professionals.
Novices appear to learn through concept formation while experts
seem to construct a knowledge base for themselves in the context
ßof their practice.
2
Studies in nursing education suggest that Kolb’s cycle of learning
(concrete experience, reflective observation, abstract conceptualiza-
tion, active experimentation) is a valid and useful model to
conceptualize learning in nurses.
7
I have not been able to locate articles at the time of this writing that
contain overwhelming evidence that nurses pursue learning in a
way that resembles the five-stage process described in this mono-
graph. I am convinced, however, by the information summarized
above, along with the information in the studies describing how
people in general learn (Table 1 in main text), that nurses generally
follow the same stages.
There is less explicit evidence in pharmacy. While there is a sense
that pharmacists follow a similar stage process, there are no studies
that specifically describe the steps.
8
62
Appendix A
REFERENCES
1. O’Shea E. Self-directed learning in nurse education: a review of the literature.
J Adv Nurs. 2003;42:62–70.
2. Daley BI. Novice to expert: an exploration of how professionals learn. Adult
Education Quarterly. 1999; 49:133–147.
3. Scanlon C, Weir WS. Learning from practice? Mental health nurses’ perceptions and
experiences of clinical supervision. J Adv Nurs. 1997;26:295–303.
4. Johns C. Framing lessons through reflection within Carper’s fundamental ways of
knowing in nursing. J Adv Nurs. 1995;22:226–234.
5. Carper P. Fundamental ways of knowing in nursing. Advances in Nurs Science.
1978;1:13–23.
6. Furze G, Pearcey P. Continuing education in nursing: a review of the literature.
J Adv Nurs. 1999;29:355–363.
7. Kolb DA, Boyatzis RE, Mainemelis C. Experiential learning theory: previous research
and new directions. In: Sternberg RJ, Zhang LF, editors. Perspectives on Cognitive,
Learning and Thinking Styles. NJ: Lawrence Erlbaum; 2000.
8. Fjortoft NF. Learning outcomes and behavioral changes with a pharmacy CPE
program. Am J Pharm Educ. 2006;70:1–6.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 62

63
Transforming Continuing Medical Education
Through Maintenance of Certification
F. Daniel Duffy, M.D.
American Board of Internal Medicine
Competency-based Education and Evaluation
Over the past 15 years, ideas about the qualities and competencies
of physicians have changed. The Association of American Medical
Colleges’ Medical School Objectives Project (MSOP), the CanMEDS
2005 Physician Competency Framework reports, the American
Medical Association Council on Ethical and Judicial Affairs reports,
and the UK General Medical Council’s Good Medical Practice reflect
the medical profession’s search to describe essential attributes of
physicians.
Building upon these initiatives, the Accreditation Council for Graduate
Medical Education (ACGME) revolutionized residency education
and evaluation through its Outcomes Project in Graduate Medical
Education. Their aims were to improve GME by encouraging programs
to measure their educational outcomes based on the competencies
of their graduates and to accredit programs based on their use of
these measures.
1
To establish a framework for physician competence,
ACGME solicited the help of the larger medical community. On the
basis of this feedback, they identified six core physician competen-
cies: medical knowledge, professionalism, communications and
interpersonal skills, patient care, systems-based practice, and practice-
based learning and improvement.
2
At the same time, the American Board of Medical Specialists (ABMS)
revised its policy for member boards’ certification and recertification
through a new program called Maintenance of Certification (MOC).
3
Adopting the ACGME framework, the ABMS boards issued time-
limited certification following residency and required physicians to
maintain certification through a four-part program. In MOC physi-
cians provide their boards with the following documentation: Part-1)
evidence of professional standing (unrestricted medical license and
appropriate staff credentials); Part-2) evidence of lifelong learning
and periodic self-assessment of knowledge and skills; Part-3) evi-
dence of cognitive expertise by passing a secure examination; and
Part-4) assessment of performance and improvement in practice.
ABMS initiated this program based on growing evidence that many
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 63

Transforming Continuing Medical Education Through Maintenance of Certification
64
physicians fail to remain current in their practices.
4
Likewise, patients
expect their physicians to keep up with new developments in the
field and would welcome more frequent evaluation by medical
boards and other peer groups to achieve this end.
5
The idea of demonstrating continuing competence has spread. The
Federation of State Medical Boards (FSMB) established the Physician
Accountability for Physician Competence Initiative to engage the
medical community in a dialogue about the future of healthcare in
the United States, with the ultimate goal of answering the following
question: How does the medical profession identify, measure, and
evaluate the ongoing competence of its members to assure the public
of its commitment to accountability?
6
One of the outcomes of this
initiative is the US version of Good Medical Practice, which is mod-
eled after a UK General Medical Council document and organized
according to the competencies framework. The FSMB, Osteopathic
Boards, National Board of Medical Examiners, American Medical
Association, Association of American Medical Colleges, ACGME,
ABMS, and other groups are contributing to this work in progress.
The Joint Commission issued hospital accreditation standards for
granting privileges and evaluating physician performance. This
evidence-based process goes beyond review of technical competence
and includes an ongoing evaluation of the six core competencies.
As with MOC, periodic evaluation of performance in practice is
incorporated into the process.
7
The adoption of a common framework for educating and evaluating
physician competencies evolved within a culture of intense public
scrutiny of the quality of medical care in the United States.
8,9
Many
authors have addressed problems with healthcare safety and
quality.
10,11
Others have proposed strategies for improvement in
these areas. Examples of the latter include the Six Sigma or Lean
Production methods adopted by other industries.
12
Improvement
science has been introduced into medical care and has begun to
transform the quality agenda from one of searching for and elimi-
nating poor performance into one for overall quality improvement.
13
MOC embraced this approach.
In the 1990s, the National League for Nursing established a competency
framework for education and evaluation that included outcome
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 64

Duffy
65
criteria.
14
A comprehensive nursing curriculum focused on Competency
Outcomes and Performance Assessment (COPA) was recommended
for development, implementation and assessment of initial and
continuing competence in nursing.
15
In addition, the American Board
of Nursing Specialties now certifies nurses based on their knowledge,
skills, and experience in over 25 specialties assessed by examination
along with documented evidence of specialized training.
16
Pharmacists
have a national certifying board that provides specialty certification
in nutrition support pharmacy, pharmacotherapy, psychiatric phar-
macy, nuclear pharmacy, and oncology pharmacy.
1
7
Most board-
certified pharmacists and pharmacies appreciate the value of this
specialty certification; unlike board-certified physicians, however,
board-certified pharmacists are not widely recognized outside or
even within the pharmacy profession.
18
As of 2007, nothing compa-
rable to MOC existed for either nursing or pharmacy, although most
states require continuing education for license maintenance in both
professions.
The Significance of MOC’s Requirement for Lifelong
Learning, Self-Assessment, and Practice Improvement
The Maintenance of Certification concept of lifelong learning and
practice improvement expands the definition of education from
passively learning new knowledge from experts to actively learning
from measurement and experimentation in one’s own practice.
We learn about new treatments and methods by reading, attending
lectures, participating in skills development workshops, and reflecting
on how they apply to us. Guided self-assessment helps physicians
determine their level of understanding of the new information or
skill in performing new techniques and protects us from the self
deception that convinces us we know more than we do.
19
These
elements are included in MOC Part-2: lifelong learning and periodic
self-assessment. But some of the most important learning occurs
when physicians examine the outcomes of their work and learn
how to change system processes to improve outcomes. This type
of learning is promoted in MOC Part-4: assessment of practice
performance and improvement.
Recognizing the role of active learning in the continuing develop-
ment of physicians, the American Medical Association modified its
AMA PRA Category 1 Credit
20
to permit accredited CME providers
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 65

Transforming Continuing Medical Education Through Maintenance of Certification
66
to grant credit for Internet searching and learning, test item writing,
manuscript review, and performance improvement activities, in
addition to live activities (including some committee work), enduring
materials, and journal-based continuing medical education. The
Accreditation Council for Continuing Medical Education (ACCME)
now permits accredited CME providers to provide learning activities
based on performance improvement projects. In structured and
long-term projects, a physician or group of physicians can 1) learn
about specific performance measures (ie, a mechanism that enables
the learner to quantify the quality of a selected aspect of care by
comparing it to a criterion); 2) retrospectively assess their practice;
3) apply these measures prospectively over a useful interval; 4)
enhance their knowledge or competence as necessary; 5) modify
practice as warranted; and 6) re-evaluate performance.
21
The Practice
Improvement Module used in the American Board of Internal
Medicine’s MOC program is an example of how these principles can
be applied to learning from practice.
As our concept of physician competencies expanded to include sys-
tems-based practice, our ideas about competence in professionalism
were updated. The American Board of Internal Medicine (ABIM)
Foundation, the American College of Physicians (APC) Foundation,
and the European Federation of Internal Medicine created the
Physician Charter: Medical Professionalism in the New Millennium.
22
This document reaffirms the principles of putting patient welfare
first and respecting patient autonomy; however, it adds a new
principle of social justice. The charter affirms traditional physician
commitments to update scientific knowledge and to maintain
trust by managing conflicts of interest, being honest with patients,
maintaining patient confidentiality, and maintaining appropriate
relationships with patients. It adds the physician commitments to
maintain professional competence, improve the quality of care,
improve access to care, and manage finite resources.
Accountability for continuing competence is a newly articulated
commitment of medical professionalism; however, consumer and
employer groups also are urging physicians to report quality meas-
ures to the public with the expectation that the quality of practice
will improve. This is what happened when public reporting led to
improved quality of hospital care for patients with cardiovascular
diseases.
23
Many insurers, health plans, the Center for Medicare and
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 66

Medicaid Services (CMS), and self-insured employer groups (eg,
Bridges to Excellence) are enticing physicians to engage in quality
measurement, reporting, and improvement activities through pay-
for-performance programs. For example, the Bridges to Excellence
program rewards physicians who have achieved recognition from
the National Committee on Quality Assessment (NCQA) in diabetes
care and heart stroke prevention care and who have established
high performing medical practice systems.
24
CMS has launched the
first phases of the Physician Quality Reporting Initiative, through
which physicians are encouraged to report additional codes on
claims forms from which performance measures can be calculated.
Physicians may receive additional payment if they report measures
on 80% of patients for whom the measures are applicable.
25
Integrated Model for Systems-based Practice,
Learning, and Improvement
How does all of this activity link MOC with CME and stimulate a
transformation in physician learning? Figure 1 shows a model for
understanding the interrelationship in the competencies of system-
based practice, practice-based learning and improvement, and
professionalism. It also shows how these qualities are measured and
how CME influences changes in practice.
Figure 1. Model of System-based Practice, Learning, & Improvement
Duffy
67
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 67

Transforming Continuing Medical Education Through Maintenance of Certification
68
The model incorporates three interrelated processes: 1) creating
and disseminating new medical knowledge, methods, or technology
(shown in white); 2) translating innovations into practice to produce
measurable improvements in the outcomes of care (gray); and 3)
demonstrating accountability for producing valued medical care to
patients and the healthcare marketplace (black). Through this third
process the medical licensing boards and specialty certifying boards
stimulate improvement and provide a conduit for public accounta-
bility of physician quality.
The process for developing new medical knowledge, products, and
services begins with formulating new hypotheses based on meas-
urement of care. These hypotheses reshape theories of medicine,
which can be tested in scientific research or in local practice-based
experimentation. Authors report research results in scientific journals
and publish consensus guidelines that distill these findings.
Professional societies, educational institutions, and medical staffs
convert the scientific research and guidelines into “how-to” courses
that help physicians and practice managers redesign systems to
incorporate new knowledge, products, and methods into actual
practice. Empiric evidence demonstrates that the CME most effective
in changing practice outcomes involves “how-to”learning experiences.
26
Pharmaceutical and device companies are another source of infor-
mation through the materials and activities they offer to physicians
describing new medications, processes, and technologies.
The items in the black boxes in the diagram have little direct influence
on CME; they represent the objectives for physician accountability,
which can be provided directly to patients through public reporting
and indirectly by reporting performance measures as a part of
maintaining certification or obtaining a medical license. Employers
demand that health plans provide evidence of the quality of the
healthcare they are purchasing. Through payment policies, health
plans influence the quality of care by providing capital needed for
implementing new technologies in practice. Some individual physi-
cians and medical groups actively manage the inner (gray) cycle of
practice-based learning and improvement to redesign systems in
order to eliminate waste, reduce variation, increase reliability, and
generally improve the quality of healthcare.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 68

Duffy
69
The gray cycle in the center of the model describes physician tasks
in practice-based learning and improvement. The first task, acquir-
ing and assessing new knowledge, involves point-of-care learning,
traditional CME, learning from product detailing, and practice-based
learning. Point-of-service learning involves skill in retrieving informa-
tion to solve problems in delivery of care. Traditional CME involves
reading scientific publications and participating in continuing medical
education courses. Information delivered by pharmaceutical or
device marketing and education divisions provides knowledge
applicable to improving care; however, marketing techniques
unconsciously distort physician judgment when information is
associated with gifts or favors. Therefore physicians must carefully
avoid conflicts of interests.
27
Acquiring and assessing new knowledge
is both the first step and the last step in the gray cycle of practice-
based learning.
Moving clockwise through the cycle, the second task is designing
practice processes to apply new knowledge. Physicians may know the
right thing to do but fail to reliably do what they intend. Learning
from practice changes that deficiency because it promotes frequent
experimentation and learning from mistakes. Industrial engineers such
as Demming and Juran have developed methods for translating new
knowledge and innovations into business, service, and manufacturing
operations.
28
The ACGME and ABMS competencies of systems-based
practice and practice-based learning and improvement adapted this
approach to medical care. The model shows the relationship among
medical societies, learning collaboratives, pharmaceutical and device
manufacturers, and local vendors in providing education and infor-
mation to help physicians re-design practice to incorporate new drugs,
products, and technologies. Examples of educational programs
are the ACP’s Closing the Gap project, the American Academy
of Family Practice TransforMed, and the Robert Wood Johnson
Foundation–funded Improving Performance in Practice project.
The third task in the gray cycle is executing/leading change in systems
for delivering care. This task requires the application of practice
management skills, negotiating with vendors, structuring personnel
policy, training staff, and implementing technology. This body of
knowledge and skills challenges traditional approaches to medical
education and evaluation, and it may seem more like business
school than medical education. For many physicians, the “system”
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 69

Transforming Continuing Medical Education Through Maintenance of Certification
70
is an Orwellian organizational monster that can neither be under-
stood nor managed. Traditional ideas about physician autonomy
place value on rugged individualists who work around the system
for the benefit of their patients. The new model of medical profes-
sionalism recognizes the disruption to systematic care of unbridled
physician autonomy and espouses physician competence in systems-
based practice, improvement of care, and just distribution of scarce
medical resources.
29
Today, physician competence includes capability
to manage or influence the management of clinical work processes;
develop teamwork habits, communication and interpersonal skills;
and understand the principles of human resources and business
management. Although not all physicians must achieve expertise in
system management, all must understand that system management
is essential for high-quality medical practice.
The fourth component of competence in systems-based learning and
practice improvement is measurement of practice performance.
Quantitative and qualitative measurement of the outcomes and
processes of care is the lynchpin that holds together systems-based
practice, practice-based learning and improvement, and the new
professionalism. Measurement is essential for improvement: “We
improve what we measure.” Through measurement we acquire
knowledge about how practice works and the outcomes it produces;
this knowledge informs re-design of work processes; and re-meas-
urement determines if the change improved care. Measurement leads
to creating new knowledge; by reflecting on the meaning of measured
results we generate new hypotheses about the theories of health,
medicine, and medical practice that can be tested in empiric
experiments to advance the theory and the evidence base for
improving patient care. Moreover, measurement is essential for
public accountability. Reporting performance measures to payers,
consumers, and purchasers gives them information they need to
purchase the highest-quality care. Measurement of practice perform-
ance is central to providing the evidence of continuing competence
for maintenance of board certification, and the act of reporting is a
powerful motivator to change.
How Is MOC Changing CME?
MOC creates an obvious demand for CME board review courses
and durable study materials to prepare for the secure examination.
Because most boards require passing an examination demonstrating
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 70

Duffy
71
cognitive expertise every 6 to 10 years, a steady demand exists for
“brush-up” education before the test.
The desire to align the MOC requirement for lifelong learning and
periodic self-assessment with periodic hospital staff re-credentialing
and re-licensure has prompted many boards to build 2-year or 3-
year milestones for self-assessment of knowledge or skills focused
on recent advances in the field. Commonly, these CME exercises
contain multiple choice questions appended to durable learning
materials on a particular topic. These modules have been developed
by boards and by medical societies, and they provide guided self-
assessment and focused learning on recent advances. Examples of
self-assessment programs are the ACP MKSAP (Medical Knowledge
Self-Assessment Program), ACCP-SAP, Nephrology-SAP, and American
Board of Family Medicine SAM (Self-Assessment Module).
The internal medicine CME community has developed group learning
sessions in which 10 to 200 physicians work with faculty on a self-
assessment module. Audience response technology makes it possible
to include a display of the participants’ answers to questions, and
the wide variation in answers permits the faculty to clarify the issues
contained in the question and answers. This type of course is fun,
challenging, and informative, and a popular addition to annual
meetings.
The MOC requirement for physicians to assess themselves and
make changes in their practice systems to improve their perform-
ance is arguably the most important innovation driving changes in
CME. As of 2004, few physicians had adopted formal learning and
improvement experiences in their practices.
30
For family physicians
and internists, completion of the MOC Part-4 (assessment of practice
performance and improvement) was the first personal experience
with systematically reviewing medical records to calculate perform-
ance measures, receiving feedback from patient surveys about their
experience of care, and reflecting on the practice processes and
systems that produce the care. This was the first objective of practice
performance measurement for most, and lower than expected
performance called for action to improve. Some physicians had
difficulty understanding how this activity could help them to learn
based on their more narrow view of learning and certification being
a test of their medical knowledge. They could not imagine that
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 71

Transforming Continuing Medical Education Through Maintenance of Certification
72
knowledge gained from examination and experimentation could
improve their practice. Others found the exercise tremendously
informative, were surprised by their performance, and felt motivated
to take remedial action but lacked the knowledge and skill to do so.
Others made simple changes in their practice, such as adding a flow
sheet or changing the tasks medical assistants performed, and they
re-measured to determine if the change led to improvement. Although
they did not necessarily fully understand the theory behind the
“plan, do, study, act cycle,” of quality improvement, these physicians
learned that measurement is necessary for knowing the quality of
practice, and that in measuring quality, they could begin to change
the practice. These physicians acquired deeper knowledge about
their own practice than could be achieved through more traditional
learning experiences.
The ABIM Part-4 MOC exercises are called Practice Improvement
Modules (PIM).
31
Each PIM focuses on an aspect of practice, such
as diabetes, asthma, preventive cardiology, or comprehensive care.
One PIM allows physicians to use measures provided by health plans
or medical groups. Three PIMs focus on physician and practice
communication skills, and another uses the hospital measures
reported to CMS. All of the PIMs include a self-assessment of the
practice systems, and all guide physicians through reflection on the
measures, design, and testing of an idea for improving at least one
measure. Each PIM also provides the opportunity for physicians to
reflect on the ways in which learning from a small experiment can
lead to improvements in practice.
After completing their assessment of practice, physicians report
a variety of learning and improvement outcomes. Nearly all are
surprised to find that their level of performance was lower than
expected. Many select a particular PIM to validate their anticipated
high performance and are surprised at the room for improvement.
Because the physicians themselves collect the data for calculating
the measures, they believe the results. Many connect the dots
between practice structure and processes and the outcomes of care;
they begin to develop a theory of systems-based practice. They see
the holes in their understanding and the skills they need to change
their systems of care. Some physicians learn the importance of team-
work and begin to understand that the roles and responsibilities of
practice staff can be changed to achieve more reliable care. Many
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 72

Duffy
73
begin to understand the value of information management, electron-
ic records, and prescribing and test tracking systems. Some commit
to adopting these technologies based on this exercise, and others
have been motivated to activate technologies they already possess
but have not used. For a minority of physicians, completing Part-4
MOC is a frustrating experience: Their conclusion after completing
it was that they must “learn more and work harder.” No response
could be further from the the mark. This type of self-assessment is
about the social learning that is essential for innovations and
improvement in medical practice.
Certifying boards now understand that their MOC programs’ Part-4
innovations are changing the learning experience of physicians.
The exercise engages physicians in measuring performance in patient
care, communications and interpersonal skills, systems-based practice,
and practice-based learning and improvement. But this is the barest
beginning. The next step is a robust CME program to meet the
urgent learning needs uncovered through the self-assessment of
practice performance. A theory of practice needs to grow, and new
learning activities that involve practice teams are needed. Some
early examples of learning collaboratives have been organized
by the Institute for Healthcare Improvement and projects like the
Robert Wood Johnson–funded AAFP, AAP, and ABMS Improving
Performance in Practice.
Although Part-4 MOC was developed to provide guided self-
assessment of practice performance and improvement, the data
obtained also enhance accountability for the quality of performance
to patients, payers, and purchasers of the care. ABMS boards have
developed agreements with multiple insurers and health plans to
use participation in MOC and completion of an assessment of practice
performance as measures of quality for pay-for-performance and
other recognition programs.
32
Boards who use the data in this way
must add an audit of a sample of physicians to assure the veracity
of the self-reported measures. In pursuit of the goal to reduce
redundancy in performance assessment, the ABMS boards are
working with the FSMB to align MOC with maintenance of licensure
and with the American Hospital Association to help hospitals use
MOC as evidence for meeting the joint requirements for evaluating
physician competencies in their credentialing processes.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 73

Conclusion
First, MOC provides physicians and the medical education community
with objectives and standardized measures of learning and practice
performance that can be used for guided self-assessment and sum-
mative evaluation of the effectiveness of learning outcomes. Moreover,
voluntary participation in MOC sets in motion self-imposed require-
ments for meeting 2-year to 3-year milestones for self-assessment of
knowledge about recent advances and assessment of the outcomes
and improvement of care delivered in the practice.
MOC is driving a new curriculum for physician education at all levels.
Systems-based practice calls for developing information and skills
in teamwork and people management, assuring consistent value
for patients through improving internal systems management, and
negotiating with purchasers and payers of medical care to assure
that we can meet the commitments of the new professionalism.
The self-assessment of practice provides a deeper understanding of
practice systems and the needs of the patients seeking care in the
system. This assessment will reveal the need for more training and
education in communication and interpersonal skills to help patients
from particular cultures and social groups. The performance assess-
ment will guide selection of education in how to change clinical
methods. Instead of focusing education on the curriculum devised
by experts, continuing education will be driven by patient demo-
graphics and patient care needs uncovered by the self-assessment
of individual practices.
Most importantly, MOC provides evidence of physician performance
that can be used to meet our social contract for accountability to the
public. Board certification and the MOC milestones provide one way
for physicians to reclaim their role in assuring and improving the
quality of medical care.
33
Transforming Continuing Medical Education Through Maintenance of Certification
74
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 74

REFERENCES
1. ACGME Outcome Project. Accessible at http://www.acgme.org/Outcome/ (Access
date: September 4, 2007).
2. Baltaden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and
accreditation in graduate medical education. Health Affairs 2002;21:103–111.
3. Wasserman SI, Kimball, HR, Duffy FD, for the Task Force on Recertification.
Recertification in internal medicine: a program of continuous professional development.
Ann Intern Med. 2000;133:202–208.
4. Choudhry N, Fletcher R, Soumerai S. Systematic review: The relationship between
clinical experience and quality of healthcare. Ann Intern Med. 2005;142:260–273.
5. Brennan TA, Horowitz RI, Duffy FD, Cassel CK, Goode L, Lipner RS. The role of
physician specialty board certification status in the quality movement. JAMA.
2004;292:1038–1043.
6. The Physician Accountability for Physician Competence Initiative Summits I-IV.
Accessible at http://www.innovationlabs.com/summit/. (Access date: September 4,
2007).
7. Joint Commission Requirements. Accessible at
http://www.jointcommission.org/NR/rdonlyres/8AB389E2-412D-49F0-BAC9-
996D7EF098B1/0/audio_conference_043007.pdf (Access date: September 4, 2007).
8. National Healthcare Quality Report 2005. Accessible at
http://www.ahrq.gov/qual/nhqr05/nhqr05.htm (Access date: September 4, 2007).
9. Blumenthal D. The role of physicians in the future of quality management. N Engl J
Med. 1996;335:1328–1331.
10. Institute of Medicine. To Err is Human: Building a Safer Healthcare System.
Washington, DC: The National Academy Press; 2000.
11. McGlynn EA, Asch SM, Adams J, et al. The quality of healthcare delivered to adults in
the United States. N Engl J Med. 2003;348:2635–2645.
12. Committee on Quality of Healthcare in America, Institute of Medicine. Crossing the
Quality Chasm: A New Health System for the 21st Century. Washington, DC:
National Academy Press; 2004.
13. Berwick DM, James B, Coye MJ. The connections between measurement and report-
ing. Med Care. 2002;41(suppl):I30–I38.
14. National League for Nursing (NLN). Criteria and guidelines for the evaluation of bac-
calaureate and higher degree programs in nursing. New York: NLN; 1992.
15. Lenburg CB. Redesigning expectations for initial and continuing competence for con-
temporary nursing practice. OJIN 1999 issues accessible at
http://www.nursingworld.org/ojin (Access date: February 19, 2007).
16. American Board of Nursing Specialties. Accessed at http://nursingcertification.org/.
(Access date: September 13, 2007).
17. Gourley DR, Fitzgerald WL Jr, Davis RL. Competency, board certification, credential-
ing, and specialization: who benefits? Am J Manag Care. 1997; 3:795–801.
18. Pradel FG, Palumbo FB, Flowers L, Mullins CD, Haines ST, Roffman DS. White paper:
value of specialty certification in pharmacy. J Am Pharm Assoc. 2004;44:612–620
19. Duffy FD, Holmboe ES. Self-assessment in lifelong learning and improving perform-
ance in practice: Physician know thyself. JAMA. 2006;296:1137–1139.
Duffy
75
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 75

20. AMA standards for the PRA. Accessible at
http://www.amaassn.org/ama1/pub/upload/mm/455/pra2006.pdf (Access date:
September 4, 2007).
21. ACCME standards for accredited CME providers. Accessible at
http://www.accme.org/ (Access date: September 4, 2007).
22. Project of the ABIM Foundation, ACP-ASIM Foundation, and European Federation of
Internal Medicine. Medical professionalism in the new millennium: a physician char-
ter. Ann Intern Med. 2002;136:243–246.
23. Steinbrook R. Public report cards—cardiac surgery and beyond. N Engl J Med.
2006;355:1847–1849.
24. Bridges to Excellence Physician Reward Programs. Accessible at
http://www.bridgestoexcellence.org/programs/ (Access date: September 4, 2007).
25. Center for Medicare and Medicaid Services Physician Quality Reporting Initiative.
Accessible at http://www.cms.hhs.gov/pqri/ (Access date: September 4, 2007).
26. Davis D, O’Brien MA, Freemantle N, et al. Impact of formal continuing medical edu-
cation: do conferences, workshops, rounds, and other traditional continuing educa-
tion activities change physician behavior or healthcare outcomes? JAMA.
1999;282:867–874.
27. Brennan TA, Rothman, DJ, Blank L, et al. Health industry practices that create con-
flicts of interest: a policy proposal for academic medical centers. JAMA.
2006;295:429–433.
28. Demming WE. The New Economics for Industry, Government, Education, 2nd ed.
Cambridge, MA: MIT Press; 1994.
29. Cohen JJ, Cruess S, Davidson C. Alliance between society and medicine: the public’s
stake in medical professionalism. JAMA. 2007;298:670–673.
30. Audet AJ, Doty MM, Shamasdin J, Schoenbaum SC. Measure, learn, and improve:
physicians’ involvement in quality improvement: evidence that quality improvement
still has not permeated the professional culture of medicine, although progress is evi-
dent. Health Affairs. 2005;24:843–853.
31. Holmboe ES, Meehan TP, Lynn L, Doyle P, Sherwin T, Duffy FD. The ABIM diabetes
practice improvement module: a new method for self assessment. J Contin Educ
Health Prof. 2006;26:109–119.
32. American Board of Internal Medicine. Health Plans Recognizing Maintenance of
Certification. Accessible at http://www.abim.org/moc/recognition_hp.shtm (Access
date: September 4, 2007).
33. Cassel CK, Holmboe ES. Credentialing and public accountability: a central role for
board certification. JAMA. 2006;295:939–940.
Transforming Continuing Medical Education Through Maintenance of Certification
76
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 76

DISCUSSION HIGHLIGHTS
Knowledge Development Approaches
CE must demonstrate effectiveness in terms of improving the per-
formance outcomes of health professionals. CE must help clinicians
accomplish practice-based learning and improvement. It should focus
on clinical problems and knowledge that can be used in practice,
using questions that clinicians have in practice to determine content.
If instruction really consists of presentation, example, practice, and
feedback, we do the presentation and example pretty well, but we
don’t give our attendees the opportunity to practice what we’ve told
them they should do, or offer expert consultation and feedback.
At the ABIM, almost 20,000 internists have completed self-assessment
of their practices and practice-based learning, and have begun to
demonstrate some improvement. The uniform comment that people
give back is “This was the best CME I ever took,” and they weren’t
in any CME environment doing it. But about 60 percent of them
also say, “Help. Help me. I don’t know how to improve my
performance.”
The ABMS Boards have provided as many options as possible for
recertification in allowing self-directed learning to take place, but they
do not allow the avoidance of self-directed learning to take place.
When the ABIM had voluntary recertification, it had a five percent
uptake. Regulation is important for keeping up. Continuing education
can and should be linked to recertification.
An important area of continuing education, especially in the surgical
specialties, is learning and maintaining skills. The American College
of Surgeons has begun accrediting education institutes, which are
simulation centers to provide support for skill acquisition, often in
collaboration with other professionals working in the ORs, ICUs,
and so forth.
The ACCME has injected the phrase, “practice-based learning and
improvement” into our vocabulary. We are talking about a gigantic
culture change among physicians and CME providers, and all health-
care providers as a group, to make CME actually relate to practice.
It would not be out of the question to end every sentence with “and
we are doing this because it’s about improving patient care.” It may
77
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 77

Discussion Highlights
78
be obvious, but many CME providers never have made a conscious
association between CME and improving patient care, and a lot of
physicians haven’t made the association, either.
One of the strongest motives for improving patient care through
continuous professional development is the inherent desire of
physicians, indeed of all health professionals, to do a better job,
if only they knew what they were doing and how it compared with
benchmarks. Measuring performance and feeding it back to physi-
cians, irrespective of whatever else we may add on as continuing
education around that, can be a powerful agent for change.
The motivation for continuing education, from the perspective of
the public, has been a deficit model — we must find out what our
deficits are and make sure they get plugged so we don’t harm patients.
But continuing education is also about professionalism and the
ability to grow in our professional development. We tend to lose
sight of that because of the pressing nature of clinical care problems.
The problem with our general concept of CME, which is conferences
and random reading, is that it depends on memory.
We need to get away from the idea that it is only about knowledge.
It really is about behavior and our ability to do complex tasks that
we refer to as competencies. These involve knowledge, skills,
attitudes, behaviors, and communication.
Medical practice has two components: doing what you know and
knowing what you do. Performance assessments shouldn’t be the
only thing; knowledge assessment also is essential. But too often,
performance is left out of CE.
Studies show doctors are more likely to change when learning is
initiated by a patient-based clinical question, not by a vague desire
to keep up. Continuing education ought to be learning from what
the patient brings.
The fundamental problem with CME is the total dominance of
courses. The use of hours is a misplaced metric. Also, there is an
over-reliance on numbers of attendees. People judge the effective-
ness of a CE offering by how many show up.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 78

Discussion Highlights
79
Continuing education is not only about expanding expertise, it’s also
about continuing to have your basic expertise intact.
We should not forget the importance of understanding in medicine.
Technical competence is not enough; plenty of technically competent
surgeons do the wrong operations on the wrong patients.
The current system has two flaws: first, lectures are ineffective,
except for passing on new information, and are opened to biased
information, or the perception that information could be biased;
and, second, their “entitlement mentality” signals to the public that
physicians are “for sale.”
The Need for Feedback and Evaluation
It is difficult for physicians to provide feedback to other physicians.
In one example, a physician caring for a patient with HIV made five
mistakes, yet the physician who identified the mistakes wondered
if the physician who made the mistakes should be notified. The
physician was reluctant to say that evidence-based practices had
not been followed. Physicians are not trained early either to give or
receive this kind of feedback. In other professions feedback is part
of the practice. Architects don’t just design and build; they submit
designs to colleagues first. How can physicians be trained to expect
this kind of feedback?
Lessons might be learned from other professions. For instance,
pilots are comfortable with the idea that someone will sit with them
on a regular basis to assess their performance. Pilots recognize this
lifelong learning as part of their professional responsibility while
physicians tend to think they are finished when they complete their
training.
The airlines, in addition to relying on another person for pilot
certification, also rely on computerized tests. Pilots sit in a simulator
with a real pilot and a third person dials in problems. Nothing in
medicine begins to compare. The only thing that even comes close
is simulation in surgery.
Perhaps there needs to be legal protection, an exemption from
“discovery” when mistakes are uncovered during evaluation and
feedback.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 79

Discussion Highlights
80
In the UK, general practitioners are encouraged to have a peer
mentor who meets with them every six months or so to review
charts. In Ontario, Canada, randomly selected physicians undergo
an audit by a peer physician every seven years. The peer reviewer
goes through 25 or 50 charts, and then writes a review that is shared
with the assessed physician. Based on that, some of the physicians
are then further assessed with low-tech simulations involving
standardized patients.
A group practice experimented with ways to give feedback so
physicians view it as an improvement opportunity, not as a punitive
exercise. With blinded data, everyone tended to migrate toward
the mean. When the data were unblinded, they tended to migrate
to people they respected, regardless of whether that had anything
to do with good quality of care. Now feedback is combined with
recommendations on what the evidence shows is the best practice,
followed with opportunities for the team to figure out how to do
better.
What group or party determines what outcomes are important?
The physician? The practice? Hospitals? Regulatory boards? There’s
not much opportunity for outside feedback. The ready reliance on
markers, or things that are easily measured, does not necessarily
relate to meaningful patient outcomes.
One way to measure or help competence is with a computer
and simulation, with a different problem each time. The process
depends on actually doing it, getting feedback, and reflective
thinking afterwards.
Sociability, companionship, and collegiality are pretty important in
education, and the opportunity to discuss actual practice data with
colleagues is quite valuable. Hospitals, group practices, specialty
and county societies should be able to offer these opportunities.
Two areas are involved: education and training, and certification
and verification of skills. The two are related but different. Skill
virtuosity requires thousands of hours of deliberative practice.
It is amazing that we give the practice, but little in the way of
feedback.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 80

Discussion Highlights
81
Lectures
While conferences and courses should not dominate, they still have
a place. Lectures play an important role in helping people keep up
with what’s new and what’s interesting.
Lectures can be made better, for example with interactivity, case
discussions, and small-group breakouts. Even groups of 5000 can
use these techniques.
Lectures may not be the best way to learn, but the reason so much
money is put into for-profit lectures is that they are marvelous
propaganda and advertisement. In some continuing medical education
courses you get a real expert, someone highly respected, to talk
about the use, maybe off label, of a drug. That’s powerful, but it
may it not be good education. It is, however, good advertisement.
CME providers are allowed to focus on educational objectives,
such as knowledge updates, that can be accomplished by lectures.
There is no specific requirement that, to be accredited, they spend
a certain percentage of time providing and promoting educational
activities that focus on competence and performance in practice,
as well.
Think of a learning portfolio as a bucket into which you put things
like self-assessment of learning needs, performance measures that
are required, and audits done by peer assessors, as well as compe-
tency exams, maintenance of certification and licensure. Where do
lectures fit in?
Academic detailing creates an environment that permits people to
identify, on their own, opportunities to improve without the sense
that change is being imposed.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 81

Internet Continuing Education
Denise Basow, M.D.
UpToDate, Waltham, MA
An increasing number of physicians now use the Internet to obtain
medical information. The number of physicians using the Internet
specifically for continuing education is also rising. Potential benefits of
continuing education delivered via the Internet include convenience,
flexibility, reduced travel time and expense, multimedia format, and
possibly adaptability to different learning styles.
This review begins with a description of the current landscape for
continuing medical education and the role of the Internet within that
larger context. What follows is a discussion of the ways in which
continuing education delivered via the Internet relates to our current
understanding of adult learning. An additional topic is the current
state of research on the effectiveness of online continuing education
in reaching its goals of increased knowledge and improved patient
outcomes.
Most of the literature that addresses the influence of the Internet on
continuing education limits its focus to physicians, but various groups
of healthcare professionals have established their own terminology.
For this review the term “continuing education” (abbreviated hence-
forth as CE) refers to the educational activities of all of these groups.
CE Requirements
American Medical Association (AMA) Physician Recognition Award
(PRA) Category 1 credit is awarded by accredited providers to
physicians who participate in educational activities that are certified
as meeting educational goals set forth by the AMA.
1
Every US state
requires physicians to earn AMA PRA Category 1 credit for medical
licensure, although the amounts vary by state.
Most medical societies also recognize AMA PRA Category 1 credit
as evidence of an ongoing commitment to learning, although some
specialties have variations. As an example, the American Academy
of Family Physicians (AAFP) requires that their members earn both
“prescribed” and “elective” credit, but members can only use AMA
PRA Category 1 to cover elective credits. Similarly, the American
College of Obstetrics and Gynecology (ACOG) requires that its
82
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 82

Basow
Fellows earn a number of credits designated as “ACOG Cognates,”
and the American Academy of Pediatrics (AAP) requires specific
CE activities for members who want to be recognized as Fellows
of the Academy. Most non-physician medical providers, including
nurses, nurse practitioners, physicians’ assistants, and doctors of
osteopathy, also recognize AMA PRA Category 1 credit but require
additional types of CE for maintenance of licensure, society mem-
bership, or recertification.
Outside the United States, with the exception of Canada, CE is gen-
erally less well structured, although that is changing. The European
Accreditation Council for Continuing Medical Education, for example,
only began operation in the year 2000. In some countries, CE is
essentially an ethical and moral obligation, while in others it is
required by the profession, insurance, or other bodies involved in
healthcare.
2
Italy has a well developed system regulated by a gov-
ernment body that encompasses all professions related to healthcare
and not physicians alone. The AMA recently established an agree-
ment with the European Union of Medical Specialties to mutually
recognize CE credit.
3
Internet Point-of-care CE
The AMA recognizes many activities as eligible for AMA PRA
Category 1 credit.
1
The newest activity to be recognized is Internet
point-of-care CE, defined as structured, self-directed online learning
on topics relevant to a physician’s practice. To earn Internet point-of-
care credits, physicians must complete a “learning cycle” that includes
reviewing the original clinical question, identifying the relevant
sources of information, and describing the application of these find-
ings to practice. The last component of the learning cycle, which has
also been termed “reflection,” is based on the idea that reflecting
upon one’s clinical practice is an essential component for the devel-
opment of expertise and therefore should be a component of the
educational process.
4
However, what constitutes reflection, and
whether this reflective process affects patient outcomes, is not clear.
5
Frequently, clinicians consult resources that award Internet point-of-
care CE to answer questions that arise during patient encounters.
This type of CE has the potential to be extremely vital, given results
from studies demonstrating that physicians often have important
questions (questions that could affect outcomes) during the patient
83
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 83

Internet Continuing Education
84
encounter that are left unanswered.
5–7
In one study, physicians only
pursued answers to 55 percent of questions that arose during the
patient encounter.
6
Internet point-of-care CE does not describe all CE done over the
Internet. “Live” Internet teleconferences, online case presentations
with questions and answers, and a variety of other online activities
might fall into different categories of CE. The wide variety of activi-
ties that fall under the umbrella of Internet CE makes it difficult to
know what activities investigators are considering when they study
the utility of the Internet to provide CE.
The distinction between Internet point-of-care CE and other types
of CE delivered via the Internet has several implications:
1. In an effort to address the lack of quality standardization of the
plethora of CE activities available over the Internet, the AMA
and AAFP have limited the number of providers of Internet
point-of-care CE; currently this list includes ACP PIER, DynaMed,
UpToDate, and InfoRetriever. However, this list continues to
evolve.
2. The AAFP limits the number of credits that physicians can earn
from Internet point-of-care CE to 20 prescribed credits per year.
3. Although activities that fall into the realm of Internet point-of-
care CE are usually understood to be those that are used during
patient encounters, the documentation process mandated by
the AMA (completion of the learning cycle) has made it difficult
to complete these activities during the course of a busy clini-
cian’s day. While a number of groups, including the AANP, the
AOA, and the AAP, offer credit for the same activities, only the
AMA and AAFP require the potentially limiting documentation
process.
It is too early to fully understand the implications of #3. Some
point-of-care providers have tried to simplify the documentation
process by “prefilling” a number of items on the required forms with
information that can be gleaned from the search itself. Although
physicians have not responded negatively to this process, it remains
unclear whether these activities fulfill the goals set out by the AMA
for the reflective component of the learning cycle.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 84

Basow
85
Availability and Usage of Internet CE
It is difficult to ascertain the number of websites that deliver Internet
CE. According to one estimate, 300 sites offered more than 16,000
courses and more than 26,000 credits as of December 2006,
8
but this
is likely an underestimate. Sources for Internet point-of-care CE are
more scarce.
The Physicians’ Preferences in CME Study is the longest running
longitudinal study of its kind, albeit with a small sample size.
9
For
the 2006 survey, data were collected between September 28 and
November 2. Surveys were mailed to 1200 US-based physicians; 148
usable surveys were returned, for a response rate of 12.5 percent.
These were the key findings:
— About 26 percent of respondents said they planned to use
Internet point-of-care CE during the next 12 months.
— Of those who used the Internet to obtain CE, Internet point-of-
care CE was most popular (62 percent used Internet point of
care, versus 21 percent using enduring Internet activities).
— Respondents earned the largest percentage of their CE credits
by attending out-of-town meetings, but that amount was only
32 percent, the lowest in the 14-year history of the survey (with
the exception of 1998, when it was also 32 percent). Men were
more likely to travel than women (34 versus 21 percent).
— Internet point-of-care activities were more popular with women
than men (39 versus 20 percent) and with physicians over the
age of 55.
These findings suggest that Internet CE activities have become more
popular than attendance at out-of-town meetings, and that physi-
cians tend to use Internet point-of-care activities.
These results mirror trends in physicians’ overall use of the Internet
and in the availability of CE on the Internet. In a 2001 AMA survey
of 997 physicians in the United States, 78 percent said they used
the Internet in their practices, compared with 20 percent in 1997.
10
About half of the physicians said that the Internet had a major
impact on the way they practiced medicine. In a 2003 survey of
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 85

Internet Continuing Education
86
3347 US physicians, more than half reported daily (23 percent) or
weekly (37 percent) use of the Internet for clinical information; 28
percent reported accessing online CE several times a year.
11
Similarly, data from the Accreditation Council for Continuing Medical
Eduation suggest substantial growth in physician use of the Internet
for CE between 1998 and 2005. In 1998, 37,879 physicians (0.5 percent
of those receiving CE) accumulated 3436 hours of credit (0.5 percent
of total credits awarded) from Internet CE.
1
2
By comparison, in 2005,
over 1.3 million physicians (18 percent) earned almost 37,000 credits
(5 percent) via the internet.
13
Outcomes of Self-directed Learning
In consideration of how physicians learn and how this learning can
affect change, “optimal” CE has been described as “highly self-
directed with content, learning methods, and learning resources
selected specifically for the purpose of improving the knowledge,
skill, and attitudes that physicians require in their daily professional
lives that lead to improved patient outcomes”.
14
Malcolm Knowles,
15,16
a professor of adult education with an interest in how adults learn,
developed a theory of “andragogy,”which emphasizes the following
four points:
— Adults need to be involved in the planning and evaluation of
their learning.
— Experience provides the basis for learning.
— Adults are most interested in learning when it has immediate
relevance to their job or personal life.
— Adult learning is problem centered rather than content oriented.
These observations are consistent with results from CE studies.
The data demonstrate that exclusively didactic types of CE, such
as lectures, do not improve physician performance or patient care,
while interactive and sequenced learning has been associated with
a positive impact.
17
Internet CE, particularly point-of-care CE, takes advantage of this
concept of self-directed learning. A physician with a question that
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 86

Basow
87
arises in clinical practice who searches for an answer and then
applies the information to patient care has satisfied all four points
cited in the previous text. The search for that answer may occur in a
number of ways, but easy accessibility to online resources makes
the Internet an ideal source for this type of learning.
Although only a few randomized controlled trials have compared
Internet-based CE interventions with traditional CE, a number of
controlled trials have compared online CE with no intervention and
reported changes in nonbehavioral measures, such as knowledge,
attitudes, confidence, and satisfaction, as summarized below:
18–23
— In one study, 643 practicing pathologists from around the world
took a pretutorial quiz on pathologic images of prostate carcinoma
specimens and then viewed an online tutorial with text describing
the Gleason grading system.
18
The tutorial significantly improved
Gleason grading in 15 of 20 specimens; on average there was a
12 percent increase in assigning the correct Gleason score.
— Researchers in a study involving 354 physicians evaluated an
online CE program focusing on identification of pigmented
lesions. They assessed the performance of the physicians using a
pretest, a tutorial, and an identical posttest.
19
Completing the CE
tutorial was associated with significant improvements in physi-
cian confidence, correct answers to a knowledge test (52 versus
85 percent correct), and correct answers to a clinical skills test
(81 versus 90 percent correct).
— A randomized crossover trial of physicians, pharmacists,
advanced practice nurses, and dietitians evaluated an Internet
case-based curriculum on herbs and dietary supplements.
21
Participants were randomly assigned to an immediate interven-
tion group or a waiting list and were surveyed about their
knowledge, confidence, and communication related to herbs
and dietary supplements on enrollment in the study and after
both groups completed the curriculum. Scores improved signifi-
cantly in all three areas for the immediate intervention group
compared with the waiting list group; after the latter group com-
pleted the program the scores in the two groups were similar
and significantly improved from baseline.
— A randomized trial of primary care physicians evaluated the
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 87

Internet Continuing Education
88
effect of four CE modules released at 3-month intervals on
screening for Chlamydia infection.
22
Physicians completed an
average of 2.4 modules, with each module requiring an average
of 12 minutes to complete. Both groups demonstrated declines in
Chlamydia screening rates during the study period. Nevertheless,
despite this modest intervention, the physicians in the interven-
tion group had significantly lower declines in screening
compared with the control group.
A number of studies have demonstrated that Internet-based CE
programs are at least as effective as traditional CE methods for
improving knowledge.
24
For example, a study of 358 physicians in
British Columbia compared four interventions to improve physicians’
knowledge about the management of workplace injuries.
25
Physicians
selected whether to receive intervention through an online learning
program, videoconferencing, traditional lectures, or face-to-face
small group outreach programs. The Internet and videoconferencing
programs were as effective as more traditional CE approaches in
terms of enhancing physician knowledge.
The literature examining whether Internet CE leads to behavioral
change or increased knowledge is limited. The only randomized
trial that looked at these outcomes compared an Internet-based CE
intervention that could be completed over multiple sessions over
2 weeks to a single “live,”small-group interactive CE workshop.
26
The results from the comparison group indicate that this type of
interactive CE affects performance, compared with purely didactic
CE.
17
The investigators made the following observations:
26
— Similar to other studies of Internet CE, both interventions
resulted in significant and similar knowledge gains.
— The Internet-based CE resulted in objectively measured changes
in behavior and improved adherence to treatment guidelines,
compared with “live” CE.
The authors hypothesized that the behavior change associated with
Internet-based CE could be attributed to several factors, including
completing the activity over multiple sessions rather than one work-
shop and the ability of the physicians to structure their own learning
by moving freely throughout the website.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 88

Basow
89
Other data on the effect of Internet CE on patient outcomes are lim-
ited to results from observational studies and self-reported physician
behavior. In one study that evaluated a variety of online CE programs
to enhance physician knowledge, a retrospective survey of physicians
participating in online CE found that physicians reported changes in
practice based on CE participation.
27
Similarly, UpToDate, an online
resource designed to answer clinical questions at the point of care
and a provider of Internet point-of-care CE, has done multiple
subscriber surveys, with results suggesting that physicians change
behavior when they consult UpToDate to answer questions.
2
8
These
behaviors range from changes in diagnostic testing and management
decisions to avoiding specialist referrals. In addition, investigators
in an observational study of hospitals that subscribe to UpToDate
found that, compared with nonsubscribing hospitals, hospitals that
used UpToDate had significantly fewer adverse events and shorter
duration of patient stays (personal communication). Although the
last report is limited by its observational nature, the results are
supported by the observation that these effects were greater with
increasing use of UpToDate at any given hospital; that is, there was
a “dose effect.”
Summary
Internet use, including use of Internet CE opportunities, is increas-
ing rapidly. Accreditation councils in the United States and
elsewhere and across all healthcare professions recognize this
method of CE as valid. Acquiring CE via the Internet makes sense
based on our understanding of the importance of self-directed learn-
ing. However, although a substantial amount of data suggest that
Internet CE activities enhance knowledge to an extent that is equiva-
lent to improvements with other types of CE, data on whether
Internet CE alters the behavior of clinicians and improves patient
outcomes are scarce. Thus, more studies are necessary to evaluate
the effect of Internet CE on patient outcomes.
Another question is whether Internet point-of care CE leads to
results that are equivalent to those from other types of Internet CE.
This question is particularly important given our knowledge that
physicians often do not answer questions during the patient
encounter despite the availability of point-of-care resources that can
provide the information they need. In addition, although the AMA
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 89

Internet Continuing Education
and such specialty societies as the AAFP have promoted point-of-
care CE opportunities over the past couple of years, potential
obstacles, including the documentation process, may actually limit
the routine use of these activities.
REFERENCES
1. The Physicians Recognition Award and credit system. Information for accredited
providers and physicians (2006 revision). Chicago: American Medical Association,
product number OP412806.
2. Braido F, Popov T, Ansotegui J, et al. Continuing medical education: an international
reality. Allergy. 2005;60:739–742.
3. AMA UEMS/EACCME Credit. Accessible at http://www.ama-
assn.org/ama/pub/category/14348.html (Access date: February 20, 2007).
4. Mamede S, Schmidt HG. The structure of reflective practice in medicine. Med Educ.
2004;38:1302–1308.
5. Bennett NL, Casebeer LL, Zheng S, Kristofco R. Information-seeking behaviors and
reflective practice. J Cont Med Educ. 2006;26:120–127.
6. Ely JW Osheroff JA, Chambliss ML, et al. Answering physicians’ clinical questions:
obstacles and potential solutions. J Am Med Inform Assoc. 2005;12:217–224.
7. Covell DG, Uman GC, Manning PR. Information needs in office practice: Are they
being met? Ann Intern Med. 1985;103:596–599.
8. Sklar, BM. Online continuing medical education. http://www.cmelist.com/list.htm#M
(Access date: March 6,2007).
9. Hosansky, T. CME changes course. Medical Meetings. January 2007, p. 16.
10. American Medical Association. 2002 AMA Study of Physicians’ Use of the World
Wide Web. Chicago: AMA Press; 2002.
11. Bennett NL, Casebeer LL, Kristofco RE, Strasser SM. Physicians’ Internet information-
seeking behaviors. J Cont Educ Health Prof. 2004;24:31–38.
12. Accreditation Council for Continuing Medical Education. ACCME annual report data
1998. Accessible at http://www.accme.org/dir_docs/doc_upload/dc316660-2a48-
46d4-916f-60334f7527ba_uploaddocument.pdf (Access date: March 6, 2007).
13. Accreditation Council for Continuing Medical Education. ACCME annual report data
2005. Accessible at http://www.accme.org/dir_docs/doc_upload/9c795f02-c470-
4ba3-a491-d288be965eff_uploaddocument.pdf (Access date: March 6, 2007).
14. Bennett NL, Davis DA, Easterling WE, et al. Continuing medical education: a new
vision of the professional development of physicians. Acad Med. 2000;75:1167–1172.
15. Knowles, M. The Adult Learner: A Neglected Species, 3rd ed. Houston, TX: Gulf
Publishing; 1984.
16. Andragogy (M. Knowles). Accesible at http://tip.psychology.org/knowles.html
(Access date: March 6, 2007).
17. Davis D, O’Brien MA, Freemantle N, et al. Impact of formal continuing medical
education. Do conferences, workshops, rounds, and other traditional continuing
education activities change physician behavior or healthcare outcomes? JAMA.
1999;282:867–874.
90
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 90

Basow
91
18. Kronz JD, Silberman MA, Allsbrook WC, Epstein JI. A web-based tutorial improves
practicing pathologists’ Gleason grading images of prostate carcinoma specimens
obtained by needle biopsy: validation of a new medical education paradigm.
Cancer. 2000;89:1818–1823.
19. Harris JM, Salasche SJ, Harris RB. Can internet-based continuing medical education
improve physicians’ skin cancer knowledge and skills? J Gen Intern Med.
2001;16:50–56.
20. Harris JM Jr, Kutob, RM, Surprenant ZJ, et al. Can internet-based education improve
physician confidence in dealing with domestic violence? Fam Med. 2002; 34:287–292.
21. Kemper KJ, Amata-Kynvi A, Sanghavi D, et al. Randomized trial of an internet cur-
riculum on herbs and other dietary supplements for healthcare professionals. Acad
Med. 2002;77:882–889.
22. Allison JJ, Kiefe CI, Wall T, et al. Multicomponent Internet continuing medical educa-
tion to promote Chlamydia screening. Am J Prev Med. 2005;28:285–290.
23. Casebeer L, Andolsek K, Abdolrasulnia M, et al. Evaluation of an online bioterrorism
continuing medical education course. J Contin Educ Health Prof. 2006;26:137–144.
24. Wutoh R, Boren SA, Balas EA, et al. eLearning: A review of internet-based continuing
medical education. J Contin Educ Health Prof. 2004; 24:20–30.
25. Karlinsky H, Dunn C, Clifford B, et al. Workplace injury management: using new
technology to deliver and evaluate physician continuing medical education. J Occup
Rehabil. 2006; 16:719–730.
26. Fordis M, King JE, Ballantyne CM, et al. Comparison of the instructional efficacy of
internet-based CME with live interactive CME workshops: a randomized controlled
trial. JAMA. 2005;294:1043–1051.
27. Curran V, Lockyer J, Sargeant J, Fleet L. Evaluation of learning outcomes in web-
based continuing medical education. Acad Med. 2006; 81:S30–S34.
28. UpToDate Caregroup physician survey, Massachusetts General Hospital (MGH)
and Brigham and Women’s Hospital physician survey, Harvard Vanguard physician
survey, and UpToDate subscriber survey. Accessible at
http://www.uptodate.com/research/index.asp (Access date: March 6, 2007).
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 91

Informatics Skills Needed!
Donald A. B. Lindberg, M.D.
National Library of Medicine
The information technology employed in continuing education
for health professionals cannot reasonably be less revolutionary than
the information technology that is quickly reshaping biomedical
research and clinical treatment. Information technology is also
revolutionizing the provision of scientific clinical guidance to
patients, families, and the public.
The best biomedical research increasingly shares scientific results in
publicly free electronic sources, publishes peer-reviewed analytical
results speedily and freely, and complies with governmental and
ethical obligations for voluntary clinical trials, including registration
of trials and public reporting of results. Physicians and healthcare
facilities are increasingly part of regional or national configurations.
Consequently, learning and continuing education, both for health
science students and for the best advanced practitioners, absolutely
demands understanding of and regular access to computer-based
systems that can provide the following four basic functions:
A. Fairly effortless access to traditional publications in the
peer-reviewed biomedical literature
B. Fairly effortless access to modern interactive biomedical
publications
C. Comprehension of elementary database structure of the
latest genome/phenome whole genome database systems,
along with understanding of the procedures to contribute
findings for one's patients, and understanding of the rules
for proper access to the accumulating combined wisdom
D. Technical capability for participation in medical informa-
tion systems for disaster management
This all may sound a bit like “overkill.” Please let me illustrate with
some examples of these existing systems:
1. Patients and the public access MedlinePlus.Gov about a million
times each day. They are urged to bring their questions to the
92
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 92

Lindberg
93
doctor, and they do! I have found practitioners to be full of praise,
especially for the tutorials that have been designed to increase
one’s understanding of medical diagnoses or procedures. About
25 percent of the use of MedlinePlus is now from physicians.
2. Over 2 percent of each year’s 900,000 new Medline articles are
interactive. That is, the message is contained in video attachments
and/or data tables with which the reader can interact to see “the
data behind the table,” or can learn online to do procedures —
even endoscopic surgical ones.
3. Db Gap is a new system from the National Institutes of Health for
storing and selectively providing genomic and phenomic data
from prospective population studies that include genome-wide
analyses (GWAS). These data will include (after appropriate
individual patient consent) populations such as the National
Heart Lung and Blood Institute Framingham studies and the
Genes and Environment study. Access to the summarized studies
and resulting data will be generally available. Individual patient
results will be available to research team participants and others
authenticated through Institutional Review Boards. These devel-
opments represent a new and powerfully important approach to
top quality medical practice — and to participation in new large
clinical research projects. These studies will supplement reports
from traditional clinical trials.
4. In interpreting both traditional clinical trials results—and espe-
cially the GWAS work — it is essential to have mastered the
rudiments of statistical, especially Bayesian, calculation of signif-
icance. Why? Because most traditional clinical trials are way too
small; that’s why authors present us with force-fit meta-analyses
that combine multiple too-small studies.
The GWAS studies are exciting new probes into the genomic
unknown, but they will demand much care in interpretation.
Otherwise, there is the danger of almost hopelessly underspeci-
fied statistical fishing expeditions: 500,000 SNP (snapshot) files,
for example, and 400 cases!
5. The details of healthcare professional participation in disaster
management are not yet in their final form, but it is already certain
that we must have a prominent role. The communication systems
of the past cry out for improvement, and local and regional
advanced planning, triaging, and team play are essential. So here,
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 93

Informatics Skills Needed
too, old fashioned continuing education aimed at individual
skills and test-passing abilities without care for the larger health-
care organizational framework will no longer be acceptable.
Remarks by David C. Slawson, M.D.
University of Virginia
We got involved in developing an “Information Mastery”
1-3
curriculum
for two reasons. The first is that, basically, primary care doctors guess
at answers for about 70 to 80 percent of the information questions
that they have.
The second is that only three factors influence about 95 percent
of their decision-making.
4
Number one is what a patient asks for.
Forty percent of the time that patients ask for something by name,
they get it from their doctor. Number two is what the pharmaceutical
reps recommend. And Number three, and this influences them most
of all, is their local, expert-based continuing medical education. All
three of these factors are almost completely paid for by the pharma-
ceutical industry. So, basically you have a system where doctors are
guessing and what they do is based on what they get from drug
reps and their continuing education, both paid for mostly by industry.
If Oprah Winfrey knew what it was like right now, the public would
be in an uproar.
The last 100 years of medicine have been based on the biomedical
approach, basically breaking the body down into its components
and figuring out how each works. Information Mastery is the exact
opposite. It is based on the probability approach to medicine: What
evidence out there has the highest probability of helping us do the
“right thing” for the patient? The “right thing” means doing more
good than harm, but knowing that you can’t always win. That is
probability. No matter how good you are, you can’t always win. Our
challenge is to find the best, most likely probability.
The goal of Information Mastery is to answer 90 percent of physicians’
questions in 30 seconds to 60 seconds. John Ely’s work has shown
that doctors in busy clinical practice won’t look up a question if
they think it will take more than a minute to find the answer.
5
That
means we’ve got to do it in less than a minute, and it must be the
94
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 94

Slawson
95
highest-quality information. Quality matters.
Unfortunately, the perception of quality matters more. Our job is to
teach physicians how to tell the difference between true quality and the
perception of quality. The way we do that is to use what’s called the
“Information Mastery Usefulness Equation.” That means the usefulness
of information depends upon three variables: How relevant is that
information, how valid is that information and, inversely, how much
work does it take to get that information. If the best answer takes
ten minutes, it’s too long. If I turn and ask someone who is practicing
right next to me what to do and what he gives me is neither relevant
nor valid, it is a useless answer because of the equation: zero times
anything is still zero and divided by anything is still zero.
We recognize four levels of information mastery proficiency. Level
zero is where most clinicians are today, where they do not base
their information decisions on the highest-quality information. Our
goal is to get every physician — and not just physicians, but dentists,
veterinarians, nurses, chiropractors, everyone — to Level 1, which is
where they make decisions based on the highest-quality information
that exists at that point in time. The way to do that, we believe, is
using what we call “specialty-specific comprehensive coordinated
hunting and forging tools.” A forging tool is basically a team of people
at Level 2, which involves less than one percent of those in each
specialty in each discipline. These people survey all of the journals
and find the 10 to 20 important articles each month for their disci-
pline or specialty. We call these important articles POEMs, or
Patient Oriented Evidence that Matters, and we make sure that
everybody gets the POEMs each month. They say, “Hey, this is new
information that’s important. This is the kind of information that has
the potential to change what I do every day.”
The hunting tool basically takes all of that and puts it together in a
database where it’s accessible in less than one minute. Then, for
instance, I can say to somebody, “There’s a new study that says
Riboflavin 400 milligrams once a day works better than just about
everything else for migraine headaches at one-tenth the cost.” Five
months from now, a doctor may remember there is a vitamin but
won’t remember Riboflavin 400 milligrams. But with the hunting
tool and “MIG-go”— even if the doctor can’t remember whether the
i comes before the a or the a before the i with migraine — at least
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 95

the MIG finds that article for them. That’s the coordinated tool that
makes it work.
We’ve done work in the U.K., where doctors have been taught to
read the literature critically since the late 1980s. Their data show, for
example, that if there is an article about a particular drug, as time
goes on, use of that drug gets higher and higher. If, at a later time, a
major article in JAMA says that drug should NOT be used, their data
show that the use keeps going up and the article has no effect at all.
The bottom line is that practicing doctors do not have time to read
the literature. The approach must be to find another way to be sure
that they get the information and they know it is important.
Figure 1. Inter-relationship Between Relevance of Medical Outcomes
and Validity of Medical Evidence
Everything that we use is based on what we call the X and Y-axis
(Figure 1). The X-axis is how valid the information is, starting with
expert opinion and ending with homogeneous systematic review of
well done randomized controlled trials. The Y-axis is how relevant
is this information. The lowest relevance is what effect does it have
on my blood sugar. The highest relevance is will this information,
or these outcomes, make me live longer or better. The only thing
patients care about, in the end, is am I going to live longer or better,
so the most useful medical information is both valid and relevant.
Remarks
Effect on Patient-
Oriented Outcomes
•
Symptom (drivers license)
•
Functioning (visual loss)
•
Quality of Life (Leg Ulcers,
Amputation)
•
Life Span
Effect on Disease Markers
•
Diabetes (GFR,
Photocoagulation rates)
•
Arthritis (Sed rates, X-rays)
•
Peptic Ulcer (endoscopic
ulcers, etc.)
Effect on Risk Factors
for Disease
•
Improvement in markers
(blood pressure cholesterol,
HBAIC, microalbuminuria)
Highly Controlled Research
•
Randomized Controlled Trials
•
Systematic Reviews
LOE 1b, 1a
Psysiological Research
•
Case reports
•
Observational Studies
LOE 2,3
Uncontrolled
Observations &
Conjecture LOE 4,5
Relevance of Outcome
Validity of Evidence
(LOE)
Disease Oriented Evidence
Valid Patient-
Oriented
Evidence
96
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 96

We need clinicians to make their decisions based on the highest rel-
evances that exist and use the lowest the least, but realize that over
time those positions may change. And over time we have to keep
them up to date with any changes. We want to get everybody at Level
1. We have training teams and we’re starting with cardiology and
with gastroenterology so that those specialties will have a team to
Level 2 to survey the literature, find those important valid “POEMs”
for that specialty, and make sure that they are available to everyone.
As for point of care learning, Michigan State has developed a tool to
provide CME credit. Based on where the doctor looks for an answer
to a question, the prompt will ask, “Do you want CME for this,” and
if the answer is “yes,” then the prompt will ask, “Is this your clinical
question?” Based on whether the doctor looked in the diagnosis
section or the treatment section, the program can actually create the
question and ask, “Is this your question?” If the answer is “yes,” then
the next prompt asks, “What are you going to do now as a result of
this information?” The doctor may answer, “I’m going to change my
diagnosis,” or whatever. At the end it asks, “Do you want to send
CME?” If so, in less than ten seconds, it sends to their accrediting
agency something that says, “This was the question and this was the
reference that was used and this was the impact on practice,” and
they send that report automatically. The AMA has been very excited
about that work as this is the type of point of care CME that can
actually improve practice and patient outcomes.
REFERENCES
1. Shaughnessy AF, Slawson DC, Bennett JH. Becoming an information master: A
guidebook to the medical information jungle. J Fam Pract. 1994;39(5):489–499.
2. Slawson DC, Shaughnessy AF. Teaching evidence based medicine: Should we be
teaching information management instead? Acad Med. 2005;80:685–689.
3. Shaughnessy AF, Slawson DC. Are we providing doctors with the training
and tools for lifelong learning? BMJ. 1999: 319:1280. Accessible at
http://bmj.com/content/full//319/7220/1280 (Access date: February 25, 2008)
4. Prosser H, Almond S, Walley T. Influences on GPs’ decision to prescribe new
drugs — the importance of who says what. Fam Pract. 2003;20: 61-68.
5. Ely JE. Analysis of questions asked by family doctors regarding patient care. BMJ.
1999;319:358–361.
Slawson
97
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 97

98
DISCUSSION HIGHLIGHTS
Three of four components that should be included in practice-linked
CE involve IT: a practice database, so physicians can know what
they are doing; access to information at the time and place of
patient care (point of care); and a reminder system to help avoid
errors of omission. The fourth component of practice-linked CE is
the opportunity to discuss what has been done and why.
We should think in terms of the entire management of the patient,
not just the decision-making of the physician. We should develop a
database that includes every member of the team and that answers
the needs of every professional that is involved with the care of the
patients.
Technical competence is probably the core attribute of a profession.
One of the core capabilities that defines technical competence in
today’s world is the ability to search and use all resources at your
disposal. You can’t be a competent provider of care unless you use
electronic technologies in real time to manage your patients. You
can’t be a truly competent clinician unless you are fully interactive.
It is part of the practice and part of the delivery system, and the
delivery system owes patients a workforce that can use technology.
Why is it then, that in the U.S. only 10 to 20 percent of primary care
physicians has electronic records where in most of Western Europe
virtually 100 percent of physicians do?
There’s a clear link between the efficiency of our educational agenda
and our ability to take advantage of electronic technology. The
electronic revolution will happen in good time, but now about 40
percent of large medical groups and only six percent of solo practi-
tioners have an electronic record. The numbers are going up faster
among groups than individuals, but physicians working in areas like
the Mississippi delta need help to become part of a wired healthcare
system. Many states are doing better in supporting the electronic
infrastructure for continuing education than is the federal government.
The electronic health record is fundamental and whatever the
barriers have been are starting to erode, but too slowly.
Generational differences and cultural variance in learning and rela-
tionships to technology should be considered. I’m not sure people
in the age group 18 to 22 think about the Internet the way older
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 98

Discussion Highlights
99
people do. I just watch our faculty working with PDAs, as contrasted
with the ways our students work with PDAs night and day. Some
healthcare professionals are going to need more training in informa-
tion and other hands-on activities so it doesn’t seem like a big
project and they can see it can be done in real time.
Doctors should be excited about point of care learning because they
would be getting credit for what they are already doing, with a little
bureaucratic requirement. One payback would be a self-directed
learning report in which they could see all their questions, the topic
areas, the resources they used, what was helpful and what changed
their practice.
Healthcare providers also need to become informed consumers of
their resources. Clinicians must be able to appraise information
resources since they are predigested summaries.
Since physicians tend to consult multiple resources for their ques-
tions, maybe the on-line resources could be centralized for quicker
access. Clinicians don’t have the time or capacity to read multiple
studies and put all the information together. Centralization is going
to be critical because physicians practicing medicine don’t like using
lots of resources. They don’t have the time, so there’s got to be what
amounts to one-stop shopping. The question of which resources
physicians should be using is still up in the air. Also, more study is
needed to determine if the learning during point of care is surface
or deep.
Some physicians have said being able to find answers to clinical
questions on the Internet has “put the fun back into medicine.” It is
fun to learn new things and the Internet and point-of-care resources
give them the answers that help them provide better medical care.
Studies show doctors are more likely to change when learning is
initiated by a patient-based clinical question, not by a vague desire
to keep up. Even though AMA now gives credit for that type of
learning, many doctors find the documentation requirements too
burdensome. That is something that needs to be worked on.
One reason physicians won’t take the extra step to do point of care
documentation is they don’t need to. They can get credit a million
different ways and do no work at all.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 99

Discussion Highlights
100
It is good to improve the ways people use the Internet to obtain
information, regardless of whether credit is associated with it, but
the credit part could be less bureaucratic.
If you want to get information to people quickly, format is an issue.
Doctors have more access than they realize, and they are not aware
that many resources are free or relatively inexpensive. Look at what
the National Library of Medicine gives for free and there’s also the
possibility of partnering with academic centers.
IT offers a huge opportunity to do lifelong learning and continuing
education, as well as early education, across the professions. We all
have the opportunity to get the same information but we use it in a
different way. Physicians are primarily in private offices, nurses in
hospitals, but IT can bring them together.
The Internet is changing medical information for patients, their
families and the public. Thirty percent of searching on Medline
Plus is done by consumers. Now patients show up at the doctor’s
office with a bunch of printouts, which is completely different from
the way we practiced medicine 40 years ago. Medline Plus has an
information prescription project in which the doctor is encouraged
to write a prescription for the patient to look at Medline Plus for
some information.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 100
101
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:36 PM Page 101

102
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 102
II.
Financing
Continuing Education:
Who, How, and Why
103
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 103

Financial Support of Continuing Education
in the Health Professions
Robert Steinbrook, M.D.
New England Journal of Medicine
Continuing education in the health professions is a multibillion-dollar-
a year industry. In 2006, the total income from continuing medical
education (CME) in the United States for activities presented by
providers accredited by the Accreditation Council for Continuing
Medical Education (ACCME) was $2.4 billion (Figure 1, Table 1).
1
A decade ago, the total income was less than $1 billion, and the major-
ity of support came from the registration fees of CME participants
or funds from the parent organization of a program’s sponsors. Since
2003, however, the majority of income has come from industry.
2
Does the commercial funding of continuing education distort medical
practice away from what is best for health professionals and patients?
Should changes be made to the funding and existing safeguards
against financial bias and conflict of interest? This paper provides
background for the discussion of these and related questions. Although
all sources of financial support are discussed, commercial support —
the focus of current controversy — is emphasized.
Figure 1. Income and Expenses for Accredited Continuing
Medical Education in the United States, 1998 –2006
MILLIONS OF DOLLARS
Total Income Total Expense Commercial Registration Fees Advertising and
Support and Other Income Exhibit Income
2500
2000
1500
1000
500
0
1998 1999 2000 2001 2002 2003 2004 2005 2006
Y E A R
104
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 104

Commercial support for CME quadrupled between 1998 and 2006—
from $302 million to $1.2 billion. Nearly all of this money was from
firms that manufacture products that are regulated by the US Food
and Drug Administration (FDA). Support doubled from other sources.
Advertising and exhibit income — the ACCME tabulates this sepa-
rately — increased from $126 million to $245 million. Registration
fees and other income increased from $458 million to $940 million.
In 1998, commercial support represented 34.0 percent of total CME
income. In 2003 it represented 54.7 percent. In 2006, it represented
50.3 percent, and the combined for-profit support for CME — com-
Steinbrook
632 $888.5
million
$302
million
$125.9
million
$457.7
million
$842.1
million
5.5%
655 $1.11
billion
$388
million
$148.2
million
$574.6
million
$920.9
million
20.5%
680 $1.27
billion
$467
million
$168.9
million
$635.4
million
$1.05
billion
20.6%
674 $1.39
billion
$569
million
$160.0
million
$665.2
million
$1.18
billion
18.1%
686 $1.60
billion
$746
million
$187.3
million
$662.9
million
$1.33
billion
20.3%
697 $1.77
billion
$971
million
$183.3
million
$620.1
million
$1.54
billion
15.2%
716 $2.05
billion
$1.07
billion
$197.0
million
$784.5
million
$1.61
billion
27.4%
716 $2.25
billion
$1.12
billion
$235.7
million
$899.2
million
$1.72
billion
31.0%
729 $2.38
billion
$1.20
billion
$244.9
million
$940.3
million
$1.82
billion
31.0%
YEAR
1998
1999
2000
2001
2002
2003
2004
2005
2006
Table 1. Income and Expenses for Continuing Medical
Education in the United States, 1998 –2006
ACCME
A
ccredited
O
rganizations
Total Income Commercial
S
upport
Advertising
&
Exhibit
I
ncome
Registration
F
ees & Other
I
ncome
Total
E
xpense
Profit
M
argin
Data are from the 2006 annual report of the Accreditation Council for Continuing Medical Education. Of the 729 ACCME accredited
providers, 718 reported data on total income, 601 on commercial income, 446 on advertising and exhibits, 650 on registration fees and
other income, and 721 on total expense. Data on providers that are accredited by state medical societies are not included (see text).
105
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 105

Financial Support of Continuing Education in the Health Professions
106
mercial support, advertising, and exhibits income — represented
60.5 percent of total income. Although comparable data are not
available for continuing education in nursing and pharmacy, similar-
ities are likely, in part because some programs are accredited for
multiple professions. In 2006, an industry magazine noted in its
annual medical education report: “For continuing education to con-
tinue, commercial funding must remain healthy. The future of CME
depends on it.”
3
CME is also profitable. Income has grown faster than expenses.
In 1998, the profit margin for accredited providers was 5.5 percent.
In 2006, it was 31.0 percent. The three main types of providers are
physician member organizations, publishing/education companies,
and medical schools. In 2006, their overall CME profit margins were
46.3 percent, 34.7 percent, and 20.7 percent, respectively (Table 2).
Of course, nonprofit entities, such as physician member organiza-
tions and medical schools, often use CME revenues to subsidize
other activities.
There is long-standing concern that continuing education is often a
marketing activity that promotes sales of newer and more lucrative
medical products, including their off-label use, notwithstanding the
various safeguards against conflict of interest and commercial bias
discussed below.
2,4–9
Patients and payers ultimately pay the bill,
through increased spending on prescription drugs and other prod-
ucts. In August 2002, an industry magazine asked the question,
“What’s [return on investment] got to do with CME?” Noting that
“in the commercial world, large investments of company resources
have to be justified; there has to be a tangible return,” the article
concluded that marketing professionals “must demand data that
demonstrates the worthiness of their [continuing education] invest-
ment, and they must invest in programs that change physician
practice patterns.”
10
There are multiple reasons for this concern about the commercial
aspects of CME. First, the public perceives that many gifts and pay-
ments to physicians and other health professionals from industry
amount to bribery or kickbacks, even if they are entirely legal.
11
Commercial support for CME is just one more physician-industry
relationship. Many of the physicians who are invited to speak at
CME events or to organize them have extensive financial relation-
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 106

ships with industry, and drug companies have paid them to give
other presentations. The material presented may overlap with pro-
motional events and CME courses.
2
The off-label promotion of
gabapentin (Neurotonin), which was originally developed for the
treatment of epilepsy, is a well-documented example of commercial
influence on continuing education.
12
Steinbrook
1
6 $73.5
m
illion
5
.7% 0.5% 93.9% $74.4
m
illion
(
1.3%)
93 $110.6
million
52.4% 4.3% 43.3% $110.9
million
(-0.3%)
14 $2.8
million
9.2% 1.4% 89.4% $7.1
million
(-39.6%)
34 $122.8
million
40.3% 8.2% 51.5% $96.7
million
27.0%
267 $783
million
23.0% 25.5% 51.5% $535.2
million
46.3%
29 $54.2
million
51.5% 1.7% 47.0% $41.3
million
31.4%
154 $818.8
million
75.8% 1.9% 22.3% $608.0
million
34.7%
122 $418.9
million
61.9% 3.2% 34.9% $347.1
million
20.7%
729 $2.38
billion
50.3% 10.3% 39.4% $1.61
billion
27.4%
ORGANIZATION
TYPE
Government/
Military
H
ospital/Health-
care Delivery
System
Insurance
Company/
M
anaged Care
Non-profit
(Other)
Non-profit
(Physician
Member
Organization)
Not Classified
Publishing/
Education
Company
School of
Medicine
TOTAL
Table 2. Financial Support of Continuing Medical Education
for Different Types of Organizations, 2006
N
umber Total
Income
C
ommercial
Support
A
dvertising
& Exhibit
Income
R
egistration
Fees & Other
Income
T
otal
Expense
P
rofit
Margin
Data are from the 2006 annual report of the Accreditation Council for Continuing Medical Education. Publishing/Education
Company includes for-profit medical education and communication companies (MECCs). Non-profit (Other) includes foundations,
public health organizations, and voluntary health organizations, such as the American Cancer Society and the American Heart
Association. Non-profit (Physician Membership Organizations) includes specialty societies, the American Medical Association
and other non-specialty societies, and state medical societies. About 85 percent of the organizations in this category are specialty
societies. Financial data are available for overall categories, but not for sub-groups, such as MECCs or state medical societies.
Data on providers that are accredited by state medical societies are not included (see text). Totals may not sum to 100% due
to rounding.
107
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 107

Financial Support of Continuing Education in the Health Professions
108
Second, the drug company sponsorship of continuing education
may lead to an overemphasis on topics that are beneficial to com-
mercial interests — such as programs about drug treatment or the
use of medical devices or diagnostic tests, thereby biasing “the over-
all ‘curriculum’ of topics.”
9
Too few programs relate to other aspects
of care, regardless of their importance to improving patient care.
13
Third is the accreditation of medical education and communication
companies (MECCs).
1
4
An array of such companies exists, and they
have various lines of business. For example, they may organize and
manage meetings, find speakers, assess educational needs, develop
written educational materials, provide public relations services, or
prepare advertising campaigns, among other activities. Some are
primarily education companies; others are primarily communication
companies. In 2006, the 154 accredited publishing and education
companies, a category that includes MECCs, represented about a fifth
of all accredited organizations. Publishing and education companies
receive about three quarters of their CME income from commercial
support, a higher percentage than any other type of organization. In
2006, publishing and education companies had a combined income
of $819 million, or 34.4 percent of all CME income. They had more
income than any other type of organization (Table 2).
Finally, extensive financial relationships exist between some other
large providers of CME— professional societies, medical schools, and
academic medical centers — and industry.
5,9,15,16
Industry provides a
substantial part of the budget for many specialty societies; it pays for
national meetings, medical journals, and the development of clinical
practice guidelines.
17
If commercial support were to cease at a
medical society that was heavily supported by industry, programs
would be cut and staff would lose their jobs. Physicians or others
with ties to industry may run these organizations. Some of the financial
relationships are significant enough that it may be impossible for
these providers — and their personnel directly involved with CME —
to be independent of industry. Accreditation of MECCs raises the
same issue.
18
From 2005 to 2007, the U.S. Senate Finance Committee investigated
drug company grants to fund continuing education, including
allegations that grants were being used for improper purposes. The
Committee’s report, released in April 2007, concluded: “It seems
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 108

Steinbrook
109
unlikely that this sophisticated industry would spend such large
sums on an enterprise but for the expectation that the expenditures
will be recouped by increased sales. Press reports and documents
exposed in litigation and enforcement actions confirm these suspi-
cions in some instances. There is also evidence from ACCME that
some accredited CME providers still allow commercial sponsors to
exert improper influence on educational activities that are supposed
to be independent from commercial interests.”
19
The report noted that although “major drug companies have adopt-
ed corporate policies that, on their face, do not allow educational
grants to be awarded for unlawful purposes,” the policies “still allow
this industry to walk a fine line between violating rules prohibiting
off-label promotion and awarding grant money in a manner likely
to increase sales of their products, including sales for off-label uses.”
According to the Senate committee, much of the industry funding
for CME follows this pattern. A MECC submits a grant proposal. The
drug company funds “a program on a general topic (eg, treatment of
a specific condition— and the condition is one for which at least one
of the sponsoring drug company’s products is used), but the specifics
of the content are determined by the [MECC].” Pharmaceutical
company documents reveal no “explicit agreement that the CME
program will favorably discuss a company product. However, it is
possible that both parties reasonably expect that to be the result.”
19
Industry Activities and Expenditures on Promotion
Commercial support for continuing education occurs in the context
of spending for the promotion of drugs and other medical products.
Overall expenditures on pharmaceutical promotion in the United
States grew from $11.4 billion in 1996 to $29.9 billion in 2005,
accounting for 14.2 percent and 18.2 percent of sales, respectively.
20
In 2005, the spending included $4.2 billion for direct-to-consumer
advertising, $18.4 billion for free samples, $6.8 billion for detailing,
and $0.4 billion for journal advertising. For leading therapeutic classes
of drugs, between 7 percent and 24 percent of promotional spend-
ing was for professional meetings and events.
Based on information provided by drug companies, the Senate Finance
Committee estimated that “75 percent of the total educational grant
funding is used to support accredited educational grant programs.”
19
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 109

Financial Support of Continuing Education in the Health Professions
110
Many of these grants are awarded to MECCs.
A national survey conducted in 2003 and 2004 of physicians in six
specialties found that relationships between physicians and industry
are common and vary according to specialty, practice type, and
professional activities.
21
For example, 26 percent of respondents
reported receiving reimbursements for admission to CME meetings
(free or subsidized), and 15 percent reported reimbursements for
meeting expenses (eg, travel, food, and lodging, although the ques-
tion did not distinguish between CME events and other meetings);
18 percent reported payments for consulting, and 16 percent report-
ed payments for speaking engagements or for serving on a speakers’
bureau. Cardiologists were significantly more likely to receive pay-
ments than anesthesiologists, family practitioners, pediatricians, and
surgeons, but not internists.
Another national survey, conducted in 2006, found that in the past
year 65 percent of clinical departments had received industry funds
to support CME “administered by your department” and that 62
percent of the chairs of these departments had one or more personal
relationships with industry, including 26 percent who had received
“personal compensation (such as honoraria) from industry for
participating as faculty/speaker in CME activities.”
22
More than half
of the chairs whose departments had relationships with industry felt
the support had “an overall positive effect on their ability to provide
educational offerings.” Few perceived negative effects of either
relationships between departments and industry or department
chairs and industry.
Verispan, an independent medical information company in Morristown,
NJ, collects data about physician meetings and events by surveying
a panel of about 3400 physicians in 19 specialties. Once a month,
the panel members report on all invitations they receive, regardless
of the sponsor or whether they attended the event. Physicians are
compensated for participating. Among other questions, panel mem-
bers are asked if a pharmaceutical company was associated with the
event and if CME credit was offered. Verispan codes events into
eight types: videoconferences, teleconferences, symposia (held in a
convention center for longer than 4 hours with more than 20 atten-
dees or at least 50 attendees), small meetings with a pharmaceutical
representatives (less than 21 attendees), small group meetings (held
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 110

in a restaurant or with less than 21 attendees or shorter than 3 hours
with unspecified number of attendees), third-party events (conducted
by a moderator), large group meetings (more than 20 attendees or
longer than 2 hours with unspecified number of attendees), and
other (primarily market research activities). The results are projected
to a “universe” of about 375,000 physicians in the 19 specialties.
To estimate expenditures, Verispan “benchmarks” the cost of different
Steinbrook
Year Events No CME Credit CME Credit Not Specified
2000 313,605 83.6% 13.7% 2.7%
Table 3. Panel A.
Continuing Medical Education Credit for Physician
Meetings and Events for 19 Specialities, 2000 –2006
2001 370,341 86.1% 12.3% 1.6%
2002 402,881 86.3% 12.5% 1.2%
2003 453,481 79.4% 11.2% 9.4%
2004 536,428 86.6% 12.7% 0.7%
2005 511,275 88.6% 10.0% 1.4%
2006 497,470 89.7% 8.8% 1.5%
Year Expenditures No CME Credit CME Credit Not Specified
2000 $1.87 billion 73.4% 24.5% 2.1%
Table 3. Panel B.
Estimated Expenditures in Physician Meetings and
Events for 19 Specialities, 2000 –2006
2001 $2.16 billion 76.7% 21.8% 1.5%
2002 $2.18 billion 75.4% 23.5% 1.1%
2003 $2.44 billion 67.6% 22.2% 10.2%
2004 $2.85 billion 76.0% 23.2% 0.8%
2005 $2.71 billion 78.4% 20.4% 1.2%
2006 $2.64 billion 79.5% 19.1% 1.5%
Data are from Verispan
111
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 111

Financial Support of Continuing Education in the Health Professions
112
activities; a symposium or a large group meeting is assigned a greater
cost ($50,000) than a small group meeting ($5000) or a teleconfer-
ence ($2500).
Between 2000 and 2006, CME credit was available for less than 15
percent of physician meetings and events; these activities accounted
for about one fifth of expenditures (Table 3). In 2006, CME credit
was available at a smaller percentage of meetings and events — an
estimated 8.8 percent — than in prior years, and the activities for
which credit was offered accounted for a smaller percentage of
expenditures.
In 2006, an estimated 497,470 physician meetings and events took
place, with expenditures of $2.64 billion for the Verispan “universe.”
CME credit is most commonly available for symposia and large
group meetings. In 2006, this category accounted for an estimated
2.1 percent of events and 19.2 percent of expenditures. Credit was
available for about two thirds of symposia and large group meet-
ings. By comparison, credit was available for about 7 percent of
small group meetings. Such meetings represented an estimated 81.1
percent of all events and 70.6 percent of expenditures.
In 2006, pharmaceutical companies were associated with an estimated
89.1 percent of physician meetings and events. Of such meetings
and events, CME credit was offered for an estimated 8.9 percent,
not offered for 89.6 percent, and not specified for 1.5 percent. Of an
estimated 9449 symposia and large group meetings associated with
pharmaceutical companies, CME credit was offered for 67.9 percent,
not offered for 30.9 percent, and not specified for 1.2 percent. Of
an estimated 649 symposia and large group meetings not associated
with pharmaceutical companies, CME credit was offered for 72.6
percent, not offered for 18.5 percent, and not specified for 8.9 percent.
Verispan surveys a separate physician panel of about the same size
from the same specialties to gather information about electronic
promotional activities. These include online events (a self-guided
CME program, a symposium, a Web conference), “video detailing”
(real-time online communication with a pharmaceutical sales repre-
sentative), and “virtual detailing” (a self-guided online non-CME
activity).
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 112

Steinbrook
113
In 2006, there were an estimated 3.2 million electronic promotional
activities and expenditures of $329.4 million for the Verispan “universe.”
CME credit was available for about one tenth of electronic promo-
tional activities; all were online events. Online events accounted for
17.3 percent of the activities, and credit was available for about two
fifths of them. Although activities with CME credit accounted for only
about 3 percent of expenditures on electronic promotion, they
accounted for about half of expenditures for online events. An
estimated 79.4 percent of CME events were associated with a phar-
maceutical company and 6.2 percent were not; for 14.4 percent of
events, this information was either not known or not specified.
Funding for CME
Each year, providers accredited by the ACCME submit information
about their CME programs, including the number and type of activi-
ties, and some financial data, including total income, commercial
support, advertising and exhibit income, registration fees and other
income, and total expense. The data are self-reported, based on
terms and definitions provided by the Council. Although the infor-
mation is not audited, it is considered reliable. The ACCME defines
commercial support as “financial, or in-kind, contributions given
by a commercial interest, which is used to pay all or part of the costs
of a CME activity. Advertising and exhibit income is not considered
commercial support” (emphasis in original source of quote).
1
A
“commercial interest’ is “any entity producing, marketing, re-selling,
or distributing healthcare goods or services consumed by, or used
on patients,” according to the expanded definition adopted in August
2007.
18
The ACCME compiles the information and publishes an
annual report, most recently for 2006.
1
Selected financial data from recent ACCME annual reports are shown
in Tables 1, 2, and 4. In addition to the data highlighted previously
about overall income, commercial support, and profit margins, and
the income and commercial support for publishing and education
companies, there is noteworthy information:
1. Between 1998 and 2001, income from commercial support
increased by about $90 million a year; from 2001 to 2003 it
increased by about $200 million a year, and from 2003 to 2006 it
increased by about $75 million a year (Table 1).
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 113

2. In 2006, following publishing and education companies, which
received 34.4 percent of total CME income, physician member
organizations received 32.1 percent of total income, and medical
schools received 17.6 percent. Thus, the other types of organiza-
tions combined accounted for only 15.1 percent of CME income
(Table 2).
3. In 2006, following publishing and education companies, which
received 75.8 percent of their CME income from commercial
support, medical schools received 61.9 percent and hospitals/
healthcare delivery systems received 52.4 percent. Physician
member organizations received 25.5 percent of their CME income
from advertising and exhibits, which represented about three
quarters of all advertising and exhibit income for CME. They
received 23.0 percent of their income from commercial support
and 51.5 percent from registration fees and other income. Total
for-profit support for CME — commercial support and advertis-
ing and exhibits income combined — was 77.7 percent for
publishing and education companies, 65.1 percent for medical
schools, and 48.5 percent for physician member organizations.
4. Between 2004 and 2006, overall CME income increased by 16.2
percent to 12.0 percent for commercial support, 24.3 percent for
advertising and exhibits, and 19.9 percent for registration fees
Financial Support of Continuing Education in the Health Professions
Total
Income
Commerecial
Support
Advertising
and Exhibit
Income
Registration
Fees and
other Income
Total
Expense
Organization Type
Hospital/Healthcare
Delivery System
Non-profit (Other)
Non-profit (Physician
Member Organization)
Publishing/Education
Company
School of Medicine
All
+18.8% +10.1% +2.1% +33.8% +23.0%
Table 4. Changes in the Financial Support of Continuing Medical
Education for Five Types of Organizations, 2004 –2006
+24.7% +47.2% +63.2% +7.7% +16.0%
+11.2% +2.0% +13.4% +11.3% +12.8%
+17.3% +17.7% +64.0% +13.3% +15.2%
+7.2% +1.9% +31.5% +16.4% +8.2%
+16.2% +12.0% +24.3% +19.9% +12.9%
Data are from the 2004 and 2006 annual reports of the Accreditation Council for Continuing Medical Education.
Percentages are changes over two years.
114
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 114

Steinbrook
115
and other income (Table 4). Publishing and education companies
increased their income by 17.3 percent.
The ACCME also collects data on providers that are accredited by
state medical societies. In 2006, there were 1684 such providers.
These providers had a total income of $134.5 million and expenses
of $136.4 million, as compared with the $2.38 billion in income and
$1.82 billion in expenses for providers accredited by the ACCME. Of
the income earned by providers accredited by state medical societies,
$39.4 million (29.3 percent) was from commercial support, $10.2
million (7.6 percent) was from advertising and exhibits, and $84.9
million (63.1 percent) was from registration fees and other income.
Federal Laws and Regulations
The FDA issued guidelines for industry-supported scientific and
educational activities in 1997.
23
The guidelines specified that programs
and materials about therapeutic products regulated by the FDA that
are prepared by, or on behalf of, the companies that market the
products are subject to the labeling or advertising provisions of the
Food, Drug, and Cosmetic Act. However, “truly independent and
nonpromotional industry-supported activities” are not subject to
FDA regulation. According to the Senate Finance Committee, “it
is legal for independent third parties to run educational sessions
that recommend these products for off-label uses, so long as the
educational program is independent and the decision to favorably
discuss the off-label use cannot be attributed to the drug company”.
19
Factors that the FDA considers include the control of content and
selection of presenters and moderators, disclosures of company
funding and connections to speakers, the focus of the program,
the relationship between the CME provider and the supporting
company, the involvement, if any, of the CME provider in sales or
marketing of a company’s product, and a provider’s failure to meet
standards for other programs.
23
“Beyond this guidance, the FDA
does little to ensure that educational grants are used for bona fide
educational purposes. Nor does the FDA have a system in place to
monitor educational programs.”
19
The US Departments of Justice and Health and Human Services,
through the Office of the Inspector General, enforce the anti-kickback
statute and the False Claims Act.
24
Pharmaceutical manufacturers
have been prosecuted for illegal off-label promotion. One example
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 115

Financial Support of Continuing Education in the Health Professions
116
is the $430 million that Warner-Lambert paid in 2004 to settle claims
about the promotion of gabapentin. Another is the $704 million that
Serono paid in 2005 to settle claims about the promotion of somat-
ropin (Serostim), which is a human growth hormone.
19
The Office of the Inspector General identified educational grants
from drug companies as a risk area for fraud and abuse. In 2003,
they offered guidance to reduce the risk.
25
Risk-reduction measures
include separating grant making from sales and marketing within
pharmaceutical companies, establishing objective criteria for awarding
grants that do not take into account recipients’ purchases, and
funding only bona fide activities. The manufacturer should have no
control over the speaker or the content of educational activities.
Conference organizers should not improperly compensate physicians,
for example, by paying them to attend a conference. Many pharma-
ceutical manufacturers have voluntarily adopted this guidance and
implemented internal “firewalls” to separate research grants from
marketing and sales. For example, firms may have a formal policy,
a centralized support structure, and not fund individual physicians or
group practices. Sales and marketing representatives may no longer
have authority to solicit grant requests or award funds.
3,24,26,27
Of course, a pharmaceutical company decides what events to spon-
sor and chooses the CME provider. In addition, we do not know the
effectiveness of internal “firewalls” and other measures in preventing
problematic activities. The Senate Finance Committee found that major
drug companies “have limited the direct involvement of field sales
representatives and sales and marketing departments in the educa-
tional grant-making process” and that “the overt use of educational
grants to provide kickbacks to physicians who attend educational
programs has decreased over time.”
19
However, the Committee
cautioned, “it is difficult to quantify the risk of kickbacks related to
industry-sponsored education where companies overpay high-pre-
scribing physicians as “consultants” or “speakers” for minimal work
to develop educational material or teach at educational programs.”
Pharmaceutical Industry and
American Medical Association Policies
In 2002, the Pharmaceutical Research and Manufacturers of America
(PhRMA), the leading trade association representing drug companies,
issued a “Code on Interactions with Healthcare Professionals.”
28
The
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 116

Steinbrook
117
code is voluntary; it establishes no procedures to identify violations
or enforce policy.
The PhRMA code allows member companies to sponsor CME and
other educational, scientific, or professional events that are organized
by third-party providers. The sponsorship is for overall program
costs. Payments to non-faculty healthcare professionals, such as for
travel, lodging, or time spent attending the meeting, are not allowed.
Financial support for “modest” meals or receptions may be provided.
The event should “further [attendees’] knowledge on the topic(s)
being presented” and be “primarily dedicated, in both time and
effort, to promoting objective scientific and educational activities
and discourse.” When firms “underwrite medical conferences or
meetings other than their own, responsibility for and control over
the selection of content, faculty, educational methods, materials,and
venue belongs to the organizers of the conferences or meetings in
accordance with their guidelines.” Nothing should be provided or
offered “in exchange for prescribing products or for a commitment
to continue prescribing products” or “in a manner or on conditions
that would interfere with the independence of a healthcare profes-
sional’s prescribing practices.”
In May 2007, in response to public criticism about the influence of
drug company money on medical practice, Eli Lilly & Co. began
posting online (https://www.lillygrantoffice.com/grant_registry.jsp)
all of its educational grants and charitable contributions to health-
care-related organizations in the United States; the information is
updated quarterly.
29,30
Many of these grants are for CME activities.
In the first 6 months of 2007, two of the largest recipients of Lilly’s
grants were the Pri-Med Institute, a Boston-based MECC ($1,676,978
for programs related to depression and pain, diabetes, and erectile
dysfunction), and the psychiatry department at Massachusetts General
Hospital ($1,650,000 for the 2007 Psychiatry Academy, a program
with multiple sponsors). Lilly is considering disclosing information
globally, and other drug companies are considering similar disclosures.
The ethical code of the American Medical Association (AMA) permits
“subsidies to underwrite the costs of continuing medical education
conferences or professional meetings.” According to the Council on
Ethical and Judicial Affairs of the AMA (Opinion E-8.061), “any sub-
sidy should be accepted by the conference’s sponsor who in turn
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 117

Financial Support of Continuing Education in the Health Professions
118
can use the money to reduce the conference’s registration fee.”
Payments “should not be accepted directly from the company by the
physicians attending the conference” and “subsidies from industry
should not be accepted directly or indirectly to pay for the costs of
travel, lodging, or other personal expenses of physicians attending
conferences or meetings, nor should subsidies be accepted to com-
pensate for the physicians’ time.”
ACCME Policy and Standards for Commercial Support
The ACCME has seven member organizations— the American Board
of Medical Specialties, the American Hospital Association, the AMA,
the Association for Hospital Medical Education, the Association of
American Medical Colleges, the Council of Medical Specialty Societies,
and the Federation of State Medical Boards of the United States.
It has a staff equivalent of 12 full-time employees and an annual
budget of about $3.5 million.
According to the ACCME, CME “is professional education created
for the medical profession by the medical profession or its agents.”
31
The Council’s “Standards for Commercial Support” were approved
in 2004.
32,33
The six standards are 1) independence; 2) resolution
of personal conflicts of interest; 3) appropriate use of commercial
support; 4) appropriate management of associated commercial
promotion; 5) content and format without commercial bias; and 6)
disclosures relevant to potential commercial bias. CME “must promote
improvements or quality in healthcare and not a specific proprietary
business interest of a commercial interest.” Presentations “must give
a balanced view of therapeutic options.”
32
A CME provider must ensure that the following six decisions are
made free of the control of a commercial interest.
32
They are 1)
identification of CME needs; 2) determination of educational objec-
tives; 3) selection and presentation of content; 4) selection of all
persons and organizations that will be in a position to control the
content of the CME; 5) selection of educational methods; and 6)
evaluation of the activity. A commercial interest cannot specify how
these requirements are met. The standards notwithstanding, a com-
mercial sponsor can currently designate the topic or type of activity
and, if the provider requests, suggest specific topics or speakers,
discuss the content with the provider, and furnish data, including
information about off-label uses.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 118

Steinbrook
119
The ACCME will not accredit entities that are commercial interests or
that are “owned or controlled” by a commercial interest. Providers of
clinical service directly to patients, including physician organizations,
medical groups, and academic medical centers, are not considered
commercial interests. Previously, the ACCME has not considered
MECCs to be commercial interests. However, under the expanded
definition of the term ACCME adopted in August 2007, more entities,
including some accredited MECCS, are likely to be considered com-
mercial interests. For example, advertising agencies that do promotional
work for pharmaceutical companies and companies that resell drugs
or devices are now considered commercial interests. Some of these
firms have divisions that are accredited CME providers. Such firms
must spin their CME units off as separate companies by August 2009
or withdraw from accreditation. An accredited provider “can be
owned by a firm that is not a commercial interest” or have a ‘sister
company’ that is a commercial interest, if there is “an adequate
corporate firewall in place to prohibit any influence or control by
the “sister company” over the CME program.”
18
Under the standards, relevant financial relationships within the
past 12 months must be disclosed, and conflicts of interest must be
resolved before the educational activity occurs. The ACCME defines
financial relationships as “those relationships in which the individual
benefits by receiving a salary, royalty, intellectual property rights,
consulting fee, honoraria, ownership interest (eg, stocks, stock
options or other ownership interest, excluding diversified mutual
funds), or other financial benefit.”
33
The Council has not set “a
minimum dollar amount for relationships to be significant” because
“inherent in any amount is the incentive to maintain or increase the
value of the relationship.”
33
The requirements apply to planners,
speakers, and authors with “both a current financial relationship
with a commercial interest and the opportunity to affect content
relevant to products or services of that commercial interest.”
33
In
general, there are four ways to resolve conflicts of interest: 1) find
another speaker, author or meeting planner; 2) assign the speaker or
author a different topic; 3) have an effective peer review of the content
of a presentation or written material so that unsubstantiated or
promotional content is eliminated; or 4) change the overall activity
so that there is no longer a conflict. Conflicts of interest are usually
resolved through peer review or by changing the overall activity.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 119

Financial Support of Continuing Education in the Health Professions
120
Compared to the CME industry, the ACCME has a small staff and a
small budget. It lacks “proactive and real time oversight” of adherence
to its standards for commercial support, for example by placing
monitors in the audience at meetings.
19
Based on information pro-
vided by the ACCME, companies have exerted improper influence
over the content of CME programs. The Senate Finance Committee
noted that 18 of 76 CME providers that were reviewed in 2005 and
2006 “did not comply with at least one of the standards meant to
ensure independence.”
19
The Senate Committee also noted that
“based on ACCME policies, it can take as long as 9 years from the
date of a non-compliant educational activity for an educational
provider to lose accreditation.” Moreover, systematic data are lacking
on the frequency of adherence. According to the Senate Finance
Committee: “Compliance with ACCME standards still allows CME
providers to accommodate the business interests of their commercial
sponsors and affords drug companies the ability to target their
grant funding at programs likely to support sales of their products.
The full extent to which drug companies influence the content of
putatively independent CME programs cannot be estimated from
the information we currently have.”
19
Financial Support for Continuing Nursing Education and
Continuing Pharmacy Education
The American Nurses Credentialing Center (ANCC), a separately
incorporated subsidiary of the American Nurses Association,
accredits continuing nursing education (CNE). About half the states
mandate CNE. The Accreditation Council for Pharmacy Education
(ACPE) accredits continuing pharmacy education (CPE). All states
mandate CPE.
The ACCME, the ANCC, and the ACPE have a unified application
that a continuing education provider can use to seek accreditation
from two or three organizations. ANCC has accredited 225 providers
of CNE, including about 34 organizations with triple accreditation.
The ACPE has accredited about 408 providers; about a third have
multiple accreditations. Both the ANCC and the ACPE have adopted
the ACCME standards for commercial support.
There are no overall statistics for the funding of CNE. Although the
ACPE does not systematically collect information on funding, some
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 120

Steinbrook
121
data are available. In April 2007, the ACPE conducted an anonymous
survey of commercial support for pharmacy continuing education
providers.
34
The Council received 214 responses (response rate, 53
percent). Of the respondents, 28 percent reported no commercial
funding in 2006, 59 percent reported that such funding provided
25 percent or less of their annual income, 19 percent reported that
it provided more than 75 percent, and 11 percent reported that it
provided 100 percent. Another study found that “approximately
86 percent of providers and 43 percent of programs received
commercial support” and that “although the [ACPE] requires that
providers review instructional content and materials for commercially
supported programs before delivery, only 43 percent always did
so.”
35
This study concluded, “Commercial support of continuing
education is widespread, affects continuing education programs,
and is perceived to have significant educational and noneducational
consequences.”
Financial Support for Continuing Legal Education
In contrast to the situation in the health professions, tuition payments
by individual attorneys and their firms provide most of the financial
support for continuing legal education (CLE). About 40 states require
CLE, typically an average of 10 to 15 hours annually; the require-
ments and accreditation are state-based and vary. Programs may be
accredited by multiple states. Conferences may receive income from
sponsors and exhibitors, such as vendors of legal software or legal
publishers, but such payments provide limited revenue. Typically,
the speakers are not paid, although their travel expenses may be
reimbursed. Speakers agree to such arrangements for various reasons.
For instance, they may become better known in their legal fields,
and the exposure may attract new clients and referrals.
Because there is no central source of information about the financial
support of CLE, I spoke to officials at three leading providers — the
American Bar Association Center for Continuing Legal Education in
Chicago, the American Law Institute-American Bar Association in
Philadelphia, and the Practicing Law Institute in New York City. All
of these groups provided the same information. CLE has grown
rapidly. The funding differs from that for the health professions.
There are no external sources of funds that are analogous to funding
in the pharmaceutical industry.Payments from sponsors and advertisers
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 121

Financial Support of Continuing Education in the Health Professions
122
are small, compared with tuition income. Members of a sponsoring
organization may receive tuition discounts.
Recent Developments
The Senate Finance Committee report on the use of educational
grants by pharmaceutical manufacturers focused attention on the
ACCME. In an April 2007 letter to the Council, the Senate Committee
chair and ranking member urged greater “oversight to better ensure
that the content of continuing education programs is independent
from the business interests of the drug companies who fund the
programs.”
36,37
In its August 2007 response, the ACCME stated its
commitment to “ensure the validity of the CME enterprise.”
38
The
Council identified five areas for attention, including enhanced data
collection, such as establishing a monitoring system that would
allow “independent decisions about compliance with [ACCME]
requirements,” changes in the administration of the standards, such
as procedures for more rapid responses to serious problems, and
expanded education and outreach programs.” The Council also
said that it would review “the management of commercial support
across the CME enterprise including funding models and the role
of industry in CME. Alternate funding models will be considered
(eg, pooled funding, limits, sources) including discussions on the
value, or impact, of no commercial support.” Also in August 2007,
the ACCME announced several new policies.
18
In June 2007, the Senate Special Committee on Aging held a hearing
on the relationship between doctors and the drug industry, entitled
“Paid to Prescribe?”
39
The Committee chair, Senator Herb Kohl
(D-Wisconsin), stated, “these gifts and payments can compromise
physicians’ medical judgment by putting their financial interest ahead
of the welfare of their patients.”
40
Kohl proposed a national registry
that would require disclosure of payments and gifts. Separately,
Senator Charles Grassley (R-Iowa) proposed that drug manufacturers
make public any payments to doctors who bill the Medicare or
Medicaid programs, which includes almost all practicing physicians.
11
In September 2007, Senator Grassley, Senator Kohl, and four cospon-
sors introduced legislation to require manufacturers of drugs and
medical devices to report publicly nearly all payments and gifts to
physicians.
41
The federal government would make the information
available on “an Internet website that is easily searchable, down-
loadable, and understandable.” The information would include “a
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 122

Steinbrook
123
description of the nature of the payment,” such as “participation in a
medical conference, continuing medical education, or other educa-
tional or informational program or seminar, provision of materials
related to such a conference or educational or informational program or
seminar, or remuneration for promoting or participating in such a con-
ference or educational or informational program or seminar.” Minnesota
and Vermont already require similar but less comprehensive disclo-
sures. Maine and West Virginia have enacted legislation to do so.
42
Questions for Consideration
The conference should initially consider whether or not commercial
support distorts continuing education and medical practice in ways
that are bad for health professionals and patients. It should then
consider whether to recommend changes to the financial support
of continuing education.
At least six approaches are possible: 1) no commercial support;
2) limiting the percentage of commercial support that is permitted
for a provider or activity; 3) withdrawing the accreditation of MECCs
or other providers that are dependent on commercial support; 4)
eliminating direct or indirect commercial support of ACCME-accredited
programs but allowing contributions to a central repository, which
would provide funds to approved programs; 5) tightening the
ACCME’s standards for commercial support and monitoring com-
pliance; and 6) increasing public information about the funding of
CME, for example by establishing a comprehensive searchable online
registry of commercial and other support for providers and activities.
A registry of CME funding could also include information on indus-
try’s gifts and payments to speakers, authors, event planners, and
officials of provider organizations.
Pooling commercial support for continuing education has recently
been advocated.
43
Contributions might be made to a designated
office at a medical school, academic medical center, or medical
society, which would in turn disburse the contribution to ACCME-
approved programs. Thus, the ultimate recipient of funds would not
be subject to the influence of any one donor. At present, a single
commercial entity supports many continuing education programs.
An analogy would be the support of medical journals by multiple
advertisers, with a firewall between advertising and editorial content.
Another analogy would be medical journal supplements; supplements
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 123

Financial Support of Continuing Education in the Health Professions
124
sponsored by a single pharmaceutical company often have promo-
tional attributes and may be of lower quality than other journal
content.
44
Many of these approaches are not mutually exclusive. Some, if not
all, might reduce funding for continuing education. All continuing
education providers have strong vested interests in maintaining
their income sources, as well as their eligibility for accreditation.
If commercial support were to decrease or stop, some continuing
education programs would be cancelled, some people would lose
their jobs, some providers would change their operations or go out
of business, and many of the remaining providers would be less
profitable. The effects on educational offerings and quality are a
matter of conjecture. Health professionals or their employers, how-
ever, would pay more of the true costs of continuing education.
REFERENCES
1. Accreditation Council for Continuing Medical Education. Annual report data 2006.
(Accessible at
http://www.accme.org/index.cfm/fa/home.popular/popular_id/127a1c6f-462d-476b-
a33a-6b67e131ef1a.cfm (Access date: September 5, 2007).
2. Steinbrook R. Commercial support and continuing medical education. N Engl J Med.
2005;352:534–535.
3. Iskowitz M. CME’s new order. Medical Marketing Media. August 2006;37-7.
4. Angell M. The Truth About the Drug Companies: How They Deceive Us and What to
Do About It. New York: Random House; 2004.
5. Kassirer JP. On the Take: How Medicine’s Complicity with Big Business Can
Endanger Your Health. New York: Oxford University Press; 2004.
6. Relman AS. Separating continuing medical education from pharmaceutical market-
ing. JAMA. 2001;285:2009–2012.
7. Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA.
2000;283:373–380.
8. Elliott C. Pharma goes to the laundry: public relations and the business of medical
education. Hastings Cent Rep. 2004;34:18–23.
9. Harrison RV. The uncertain future of continuing medical education: commercialism
and shifts in funding. J Contin Educ Health Prof. 2003;23:198–209.
10. Casebeer LL, Shillman RS. What’s ROI got to do with CME? Medical Marketing
Media. August 2002.
11. Harris G. Lawmaker calls for registry of drug firms paying doctors. New York Times.
August 4, 2007;A9.
12. Steinman MA, Bero LA, Chren MM, Landefeld CS. Narrative review: the promotion of
gabapentin: an analysis of internal industry documents. Ann Intern Med.
2006;145:284–293.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 124

13. Katz HP, Goldfinger SE, Fletcher SW. Academic-industry collaboration in continuing
medical education: description of two approaches. J Contin Educ Health Prof.
2002;22:43–54.
14. Ross JS, Lurie P, Wolfe SM. Medical Education Services Suppliers: a threat to physician
education. Health Research Group Report July 19, 2000. Accessible at
http://www.citizen.org/publications/release.cfm?ID=7142 (Access date: September 5, 2007).
15. Kassirer JP. Professional societies and industry support: what is the quid pro quo?
Perspect Biol Med. 2007;50:7–17.
16. Steinbrook R. Haemoglobin concentrations in chronic kidney disease. Lancet.
2006;338:2191–2193.
17. Steinbrook R. Guidance for guidelines. N Engl J Med. 2007;356:331–333.
18. Accreditation Council for Continuing Medical Education. Policy updates August 2007.
Accessible at
http://www.accme.org/index.cfm/fa/news.detail/News/.cfm/news_id/3605f21a-
302a-40d1-ab4d-3ceb88087b1a.cfm (Access date: September 5, 2007).
19. Committee on Finance, United States Senate. Committee Staff Report to the
Chairman and Ranking Member, Use of Educational Grants by Pharmaceutical
Manufacturers. Washington, DC: Government Printing Office; 2007.
20. Donohue JM, Cevasco M, Rosenthal MB. A decade of direct-to-consumer advertising
of prescription drugs. N Engl J Med. 2007;357:673–681.
21. Campbell EG, Gruen RL, Mountford J, et al. A national survey of physician-industry
relationships. N Engl J Med. 2007;356:1742–1750.
22. Campbell EG, Weissman JS, Ehringhaus S, et al. Institutional academic-industry rela-
tionships. JAMA. 2007;298:1779-1786.
23. Department of Health and Human Services, Food and Drug Administration.
Guidance for industry: industry-support scientific and educational activities. Fed
Regist. 1997;62:64093–64100.
24. Studdert DM, Mello MM, Brennan TA. Financial conflicts of interest in physicians’
relationships with the pharmaceutical industry—self-regulation in the shadow of
federal prosecution. N Engl J Med. 2004;351:1891–1899.
25. Department of Health and Human Services, Office of Inspector General. OIG com-
pliance program for pharmaceutical manufacturers. Fed Regist. 2003;68:23731–743.
26. Liebman M. Drawing a line between education and promotion. Medical Marketing
Media. August 2003;44–49.
27. Iskowitz M. Beyond the firewalls. Medical Marketing Media. August 2005;34–46.
28. PhRMA code on interactions with healthcare professionals. Revised January 2004.
Accessible at
http://www.phrma.org/code_on_interactions_with_healthcare_professionals/
(Access date: September 5, 2007).
29. Johnson A. Under criticism, drug maker Lilly discloses funding. Wall Street Journal.
May 1, 2007;B1.
30. Iskowitz M. CME’s open gesture. Medical Marketing Media. August 2007;37–48.
31. 2004 Updated Standards for Commercial Support with Background Rationale and
Answers to Questions About Compliance. Chicago: Accreditation Council for
Continuing Medical Education; September 2004.
32. Standards for commercial support. Chicago: Accreditation Council for Continuing Medical
Education. Accessible at http://www.accme.org/index.cfm/fa/home.home/home.cfm
(Access date: September 5, 2007).
Steinbrook
125
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 125

Financial Support of Continuing Education in the Health Professions
126
33. Standards for commercial support including tools for implementation. Chicago:
Accreditation Council for Continuing Medical Education. Accessible at
http://www.accme.org/dir_docs/doc_upload/700a1624-d6f0-46d8-a4bc-
88e12a56eca2_uploaddocument.htm (Access date: September 5, 2007).
34. Travlos, DM, Sesti, AM. Status of commercialism in continuing pharmacy education.
Presentation at the ACPE 12th Conference on Continuing Pharmacy Education,
Denver, CO, October 7, 2007.
35. Smith JL, Cervero RM, Valentine T. Impact of commercial support on continuing
pharmacy education. J Contin Educ Health Prof. 2006;26:302–312.
36. Baucus M, Grassley C. Letter to Murray Kopelow, Accreditation Council for
Continuing Medical Education, Washington, DC: Committee on Finance, United
States Senate, April 25, 2007. Accessible at
http://www.accme.org/index.cfm/fa/news.detail/news_id/9a586937-430d-4384-b31a-
1e557d49f9d3.cfm (Access date: September 5, 2007).
37. Baucus, Grassley continue work for independence of continuing medical education.
Press release of the Senate Finance Committee. Washington DC; May 1, 2007.
38. Kopelow M. Letter to Max Baucus and Charles E. Grassley, Committee on Finance,
United States Senate. Chicago: Accreditation Council for Continuing Medical
Education, August 3, 2007. Accessible at
http://www.accme.org/index.cfm/fa/news.detail/News/.cfm/news_id/edf1572d-
bb76-416c-9b41-86fe1f7c1055.cfm (Access date: September 5, 2007).
39. Harris G. Senators to push for registry of drug makers’ gifts to doctors. New York
Times. June 28, 2007;A16.
40. Kohl examines drug industry practice of providing payments to doctors, influencing
prescribing behaviors. Press release of the Senate Special Committee on Aging.
Washington, DC: June 27, 2007.
41. Physician Payments Sunshine Act of 2007. S. 2029, 110th Cong., 1st Sess.
42. Harris G. Senators seek public listing of payments to doctors. New York Times.
September 7, 2007;A18.
43. Brennan TA, Rothman DJ, Blank, L et al. Health industry practices that create con-
flicts of interest: a policy proposal for academic medical centers. JAMA.
2006;295:429–433.
44. Bero LA, Galbraith A, Rennie D. The publication of sponsored symposiums in med-
ical journals. N Engl J Med. 1992;327:1135–1140.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 126

Remarks by Jordan J. Cohen, M.D.
Association of American Medical Colleges
I think the issue that we’re dealing with is really a key issue in terms
of how we articulate our values. This conference is occurring at a very
pregnant moment in the history of our profession. I think we have
an opportunity to change the paradigm, given all the things we’ve
heard and what we know is happening already in the world of contin-
uing medical education. I think we are on the verge of something
significantly transformative in terms of how we are going to be doing
this in the future. If we take the opportunity to come up with some
well-targeted and strong recommendations, they will be received in
a way that could have some significant impact.
I want to frame my editorial comments about the financing in a broader
context. First of all, I think we all acknowledge that maintaining one’s
professional competency throughout a lifetime of work is really a
key element of professionalism. It’s highlighted in a physician charter
which speaks to physicians, but I think it is true for all healthcare
professionals that this is an absolutely core component of what we
do as professionals. We maintain our competence and are account-
able for that to the public.
It is also clear from what we know that the fundamental purpose
of continuing education, be it for medical or other health profes-
sionals, is ultimately to improve the quality of patient care by
changing clinician behavior. The whole notion is that we are trying
to modify behavior that is documented to be insufficient to meet
whatever standard or whatever benchmark one is seeking, and
we’re trying to change that behavior in the direction of improving
the ultimate outcome.
What does that tell us about the current mode of continuing education?
It seems to me it’s got two fundamental flaws that are not unrelated.
One is that what has traditionally been thought of as continuing
education, the presentations, the courses, the large lectures and
so forth, is largely ineffective. There is some utility to the lectures,
certainly in passing on new information and keeping people abreast
of new developments, so I wouldn’t entirely discount the value of
large lectures and presentations, but in terms of improving quality,
it has not proven to be an effective modality. So that’s the first flaw:
It is an ineffective way of achieving the end that we’re looking for.
127
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 127

Remarks
128
The second major flaw is that it is funded predominantly by com-
mercial entities with self-interested motives. Commercial entities are
defined by the ACCME as entities that produce, market, resell, or
distribute healthcare goods or services consumed by or used on
patients. The fact that we have allowed the system to become so
dependent on the funding from sources that have an ulterior motive,
that is clearly related to their self interest and not in the ultimate
interest of the continuing education enterprise, is what we are
talking about.
How did we get to a point where we’ve allowed so much of this
core responsibility of ours to be funded by external forces that have
other interests in mind? It reminds us of the parable of the frog in
boiling water: It has happened gradually. Obviously the ramping up
in recent years has been quite dramatic, but over the past several
decades this has been a gradual process. We’ve been immersed in
this gradually warming boiling water to the point where we haven’t
really sensed the changes that have occurred or sensed how close
we are to the fatal boiling point.
On the other hand, if you put a frog in boiling water immediately,
it dies instantly. And that’s what our students perceive when they
come into our system. They get it. It’s not a surprise, and not difficult
for the students to recognize, that they are in a system that really
doesn’t make any sense. One bit of evidence to support that is what
the American Medical Student Association (AMSA) has done with
“no free lunch.” They actually request students to sign a pledge that
they will not accept any gifts or any support from any commercial
entities. If we tap into their perceptions of what is really correct and
right and appropriate, we will have done a good deal of our job.
The next question I would ask is why should we be concerned
about the commercial entity supporting so much of our education?
I think that tolerating commercial intrusion into one of our core
responsibilities, namely educating ourselves as professionals, is
opening ourselves to biased information. I’m not suggesting that
all of the information that emanates from commercial sources is,
ipso facto, biased, but certainly there is the perception that it could
be and there is no doubt that there are instances where it flagrantly
is. So, there is no question about the fact that the information that
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 128

Cohen
129
is ultimately supported by these sources has that very unwanted
consequence.
That raises the question about how our vow to place patients’
interests uppermost is really being maintained. It belies our commit-
ment to evidenced-based information, undermines our commitment
to cost-effective prescribing, and validates and reinforces an entitle-
ment mentality. One thing that we have to be cognizant of is how
our current system so generates the sense of entitlement on the
part of our graduates and practicing physicians that they feel that
they have an entitlement to other people helping them do their job.
It also signals to the public that we are, in fact, for sale. Any sort
of knowledgeable public person looking at what we’re doing certainly
would raise the question of why we are willing to sell ourselves
for a price.
There are opportunity costs here as well. The extent to which we
devote energy and administrative activities to garnering and manag-
ing this commercial support takes time and effort away from doing
the core mission of education. Another reason for being concerned
is that these commercial courses and commercially supported
education are so seductive that it impedes the adoption of more
effective continuing educational activity. To the extent that this is
seen as the easy, the very seductive road it diverts people’s attention
from actually doing what we now are recognizing as more effective
kinds of continuing education.
The next question, and I think it is an obvious one, is why does the
industry support medical education? In theory, one could argue, it is
in gratitude for all of the hard work that doctors and nurses do. This
is a sustainable hypothesis, but, of course, the fact is that industry’s
support is clearly in the hope of garnering a favor for its products.
This is an openly avowed objective by the industry. They make
no bones about it. This is no secret among the industry. They admit
it openly.
Then the question is, if the industry is supporting education for
reasons of trying to garner a favor, does it in fact work? Again, the
answer is obvious. Prescribing behavior and other behaviors are clearly
influenced. The documentation for that is overwhelming, so I don’t
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 129

Remarks
130
think we need to debate whether or not what the industry or com-
mercial entities do in supporting education is effective. One doesn’t
need any other evidence than the fact that they are spending billions
of dollars doing it. Obviously they are not spending money because
they don’t think it’s effective. Clearly we are in a situation where we
are opening ourselves to the biased influences of the commercial
entities that have these other negative consequences as well.
If you accept all that, could we still enjoy the financial support if we
could erect a sufficiently impermeable firewall between the industry
support and the educational activity? This, it seems to me, is what
the Accrediting Council for Continuing Medical Education, ACCME,
has been trying to do. I give them credit. I think they have tried hard
to develop policies that would ensure that commercial influences
are minimized in the educational activities that they accredit. The
most recent modification of their guideline has strengthened that
firewall considerably. But, given the strong and legitimate motivation
of industry to market its goods to doctors, there is no firewall that
we could conceivably construct that they wouldn’t be able to find
a way around and still have the influence that they desire.
I think there are a lot of things we can criticize about the way the
industry tries to influence physician behavior, but, in the final analysis,
it seems to me that we can’t quarrel with their fundamental motivation.
This is a capitalist society. They are obligated to return rewards to
their shareholders, so they market their activities to those individuals
who have most influence over the financial success of their operations.
To put the entire blame on commercial entities, I think, is totally
wrong. The burden is really on us, on the profession. We have, in
my judgment, failed to construct sufficiently robust policies and
procedures to prevent the unwanted influence of commercial entities
that are simply doing what any of us would do were we in their
place, and that is trying to influence our colleagues.
We know that doctors rationalize their acceptance of industry sup-
port. When you ask doctors whether they are influenced by the gifts
and the support that they receive, they say of course not. “I’m not
influenced, but she is for sure influenced.” So there’s an acknowl-
edgment that the influence is there, it just isn’t touching them
personally. They argue that other business people get perks, too,
giving rise to the notion that medicine is just another business, which
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 130

Cohen
131
again is one of the major consequences of the commercialization
of what goes on in medicine today. Medicine is not just another
business. It is a calling. It is a profession. It has different values.
It seems to me that what we need to do is to regain control of our
medical education from these commercial entities and deposit it
where it belongs, namely firmly within the profession itself. That
raises the question of whether physicians can afford to pay for their
own continuing education. Of course they can. No other profession
depends upon vendors of their activities to support their continuing
education. There is a fundamental obligation of professionals to
support their own continuing professional development and to
pay whatever is required to do that.
My final thoughts are these: We recognize that we are witnessing
a paradigm shift in continuing professional development and we
recognize that the paradigm we have lived with, with all of this
commercial support, is not effective. It is certainly not sufficiently
effective to warrant the kind of investments that we’re making
presently. We have new modes of continuing professional develop-
ment, particularly practice-based learning, that are more effective,
more efficient, and a much more targeted way of ensuring that we
achieve the goals of continuing professional development.
Given the fact that we’ve got this new mode that is much more
effective and is going to enjoy the benefits of the information tech-
nologies and is on the threshold of becoming the dominant mode,
and we’ve got this archaic, commercially supported mode, it seems
to me that we are in a very good position to say let’s get rid of
that old mode. We’re not going to give up much of anything by
abandoning the commercial support for this outmoded, ineffective
way of continuing education.
But I would argue that we need to be very careful if we move towards
a more practice-based learning mode of continuing education. We
have to be very cognizant that commercial entities are going to want
to get into that area, just as they have invaded the traditional area
of CME, so we’ve got to protect it. We can’t repeat the mistakes of
the past and let the new mode of continuing education also become
dominated in a decade or two by commercial intrusion. How we go
about doing that, I don’t know. But I think caution is essential, that
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 131

Remarks
132
we need to be careful not to repeat history as we move to this new
mode of continuing education.
My recommendations would be that, first of all, we strongly endorse
the obligation of health professionals to provide for their own
continuing professional development. This is a variation on the
theme of “doctor, heal thyself.” Secondly, we ought to prohibit all
commercial interests, as defined by the ACCME, from making any
contribution to continuing professional development. Perhaps we
would want to put a timeline on that, by 2025 or some definite period
of time. We need to recognize we simply cannot ignore the fact that
we have a heavy dependence on the financial support that’s coming
from these sources. We can’t ignore that reality and say that we
ought to stop this cold in its tracks while institutions need an
opportunity to somehow modify their activities to accommodate
this. It seems to me that it would make sense to recognize that some
kind of phase out period may be necessary, and maybe, in the interim,
some mechanism of pooling. I think the likelihood of commercial
entities being willing to pool their support at a level that would really
make sense, namely at the institutional level, is unlikely to yield any
significant financial support, so I don’t think we ought to be lulled
into a sense of security about that. If we wanted to have an interim
position to allow for some continued commercial support, it seems
to me the only way in which we could do that, and be dutiful to
the professional values, would be to ensure that it is pooled in such
a way that it is clearly more than an arm’s length away from the
actual distribution of those funds.
DISCUSSION HIGHLIGHTS
Although there is a great deal of commercial support of accredited
continuing education programs (estimated at about $1.5 billion in
2006), this pales in comparison to commercial support of unaccred-
ited continuing education, which is estimated to be anywhere from
$20 to $60 billion annually.
An entire enterprise outside of the ACCME umbrella offers physi-
cians and surgeons courses in the use of new devices, yet many are
not accredited by anybody. They are run by industry over weekends
and physicians return home to try out these devices on their own or
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 132

Discussion Highlights
133
with minimal help. That’s a big problem.
Effects of Commercial Support
A lot of concern is about the conflict of interest commercial support
may be causing. The International Committee of Medical Journal
Editors points out that conflict of interest doesn’t have to exist to
cause a problem; it just has to be clearly possible.
It is not only clinicians who profit from commercial support.
Continuing education providers enhance their bottom line by work-
ing with commercial providers. They don’t have to do a lot of work
because industry is happy to do the entire planning of an activity.
When we banned commercial support for planners, providers sud-
denly had to start planning their own activities but didn’t have a
clue how do that because, even though they had been “planning”
for years, they didn’t pick the topics or the speakers, and they didn’t
set objectives or measure outcomes. All they did was show up and
put their names on it.
I cannot understand how we can call ourselves professionals if we
sell our educational souls for a commercial pot of porridge, which is
usually not specific to our patients’ needs or our educational needs
and is dictated by commercial self-interest needs.
As primary care doctors, and probably this is true for others, we
guess 70-80 percent of the time and 95 percent of the decisions are
directly or indirectly influenced by the pharmaceutical industry, not
by best practices.
Most pharmaceutical influence is below the radar and physicians
don’t even realize it’s there. The evidence says the more that people
think they’re not influenced, the more they actually are. As educa-
tors we have to recognize that and work hard to overcome it,
realizing we have to overcome what’s below the radar and help
people to become more aware of it.
While a number of companies, based on guidance from the Inspector
General of the Department of Health and Human Services, have
divorced their continuing education operations from marketing, they
are still positioned to promote the fields of medical inquiry and the
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 133

Discussion Highlights
134
areas of work that the company’s line of products naturally come
upon. As long as doctors are writing prescriptions and companies
are selling for profit products that are the object of those prescrip-
tions, the companies will find legal ways to seek to influence the
judgments and choices of those who are writing the prescriptions.
We are not going to eliminate that reality. But there should be serious
recommitment to developing a fire walled entity that would be an
intermediary between the companies and recipients of the direct
support for education.
Any medical school will say they are training for life-long learning,
but they need to recognize that just training doctors how to critically
read the primary literature is not going to work for them. We have
to train them how to evaluate secondary sources, have specific tools
to evaluate secondary sources, and make sure those sources are put
together carefully without either commercial or non-commercial bias.
And as much as we try to stop students or residents from undue
influence from pharmaceutical reps during their training, when they
go into practice they will be exposed to them. We have to train future
practitioners how to deal with pharmaceutical reps.
At least one study has shown that commercial support of continuing
education narrows the focus of courses primarily to new therapies,
often therapies that include recent FDA approval of a product man-
ufactured by the commercial supporter. Whole areas of practice are
ignored. Bias may not be so much in individual talks as in the over-
all spectrum of what is covered.
When there is a gift, even a small gift, there’s an inescapable sense
of obligation that comes with it. This has been well documented.
Sadly, commercialism has developed within our specialties, which
see their knowledge and skills as proprietary, not to be shared with
other members of the profession. We need to minimize the conflict
of interest which doesn’t come only from pharmaceutical compa-
nies. Academic conflicts may be more pervasive and difficult to
measure than financial conflicts of interest.
The physicians who teach continuing medical education are the
same ones who teach residents and medical students and are doing
research. Several studies show the extent to which those at the
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 134

Discussion Highlights
135
highest levels and in the greatest position of influence in academic
medicine personally profit from their relationships, and the extent to
which solvency and discretionary dollars within a departmental
budget come from these sources. These relationships affect the con-
tent and topics of research, as well as whether research findings can
even be disseminated. These relationships affect teaching at every
level, not just in continuing education.
The issue of fraud and abuse is important for people at the front
lines. As an example, you organize a conference, you recruit partici-
pants who pay a registration fee, and then you send a letter to the
referring physicians who are invited to attend for nothing. For
instance, you have a new gamma knife and get a CME provider to
put on a conference. Then you invite the physicians who could refer
patients for the procedure to tell them about the gamma knife, and
they get the whole thing for free.
Industry funding is less of an issue in nursing, but it is growing.
This is particularly true for advanced practice nurse continuing
education, when nurse practitioners can prescribe.
The Roles and Responsibilities of Industry
The industry has to be responsible for ethically responsible dissemi-
nation of its information in ways physicians will understand. Industry
has to be more responsible for post-marketing surveillance and for
comparative effectiveness studies.
A huge public good comes from the interaction between academia
and industry in terms of promoting the transfer of new discoveries
into useful products and services, but that produces a different set
of conflicts, such as protecting patients who are subjects of human
investigation. I would draw the line in terms of involvement with
education, not with research.
Not all pharmaceutical influences are bad. A lot of great things have
come through research grants with money that was at arm’s length.
The pharmaceutical industries provide new drugs and new cures
and, because of them, we’ve had substantial advances in medicine.
It would be a mistake to exclude commercial exhibits from continuing
education, particularly in the nursing arena with national conferences.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 135

Discussion Highlights
136
The exposure during exhibit times is a form of learning.
I’m against commercial support but I have to say that the pharma-
ceutical companies have certainly changed the lives of people with
asthma, hypertension, coronary artery disease, osteoporosis and
infectious disease, plus many others. Those have been the bulk of
what a number of the conferences have been around and that’s
been a good thing.
Not all commercial funding is bad. Samples save patients time and
money. Free pads and pens save money that can go to patient care.
A free clinic had to close when it was told it could take nothing.
Who Should Finance Continuing Education
Why should we seek support of any kind in any model from com-
mercial entities to educate ourselves to maintain our competence?
That is part of our core professional responsibility.
Funding for continuing education should come from us, or our
employers, so we can control the destiny of our education. Once
commercial groups, governments, or foundations become involved,
the patient is no longer the focus.
We should pay for it ourselves. Education is a personal responsibility.
If it is system-based responsibility, other elements will come in to
support it.
While philosophically it makes sense for the profession to pay for
continuing education, one could make a case that it would be in the
enlightened self-interest of the government, through what it already
pays directly and indirectly, to promote better care. That would be
a net savings in the long run, if you look at a big enough picture.
When the government gets involved, ideology and politics, especially
if somebody is being adversely affected, often do too. An example
about a decade ago was the AHRQ-sponsored recommendation
about back pain, and the effort of politicians supporting the spinal
surgeons to zero-budget the agency. Currently, there is a big lobby-
ing effort regarding reimbursement for erythropoietin treatments in
oncology and nephrology patients.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 136

Discussion Highlights
137
If we pursue the purity of elimination, how would we set a bound-
ary so that any organization in healthcare would be able to provide
continuing education? If a school has a corporate gift, does that make
it ineligible? If you are a professor whose chair has been funded by
a company, does that make you ineligible? What the goal ought to
be is to eliminate the distortion by neutralizing and pooling, and by
public disclosures.
Though some would love to paint the industry as being responsible,
it has been with the willing collusion of physicians and continuing
medical education providers who have created an atmosphere where
physicians have come to expect that continuing medical education
will be free or low cost, that they will not have to do any work, that
they are just going to sit in a dark room and listen, that it will
include food, and will mainly be updating their knowledge.
Many doctors have a sense of entitlement, the idea that someone
else should pay for their continuing education. They see it as a
bureaucratic burden rather than a moral obligation. This is a vastly
neglected aspect of undergraduate and graduate medical education.
We have to start early and change the culture so doctors view their
continuing education as a professional obligation.
Do you think of professionalism as lettuce or potato? Lettuce rots from
the outside in, potatoes rot from the inside out. So is commercial
contamination, contamination of education, and promotion, a slimy
brown leaf of lettuce that can be removed, or is there a deeper
lesion? I think it’s an interesting question.
Continuing education and lifetime learning is a form of higher edu-
cation. This is a public good. Two funding sources for continuing
education have been eroded. One is federal and state support,
which funded AHECs that played a phenomenally important role in
educating community clinicians. The other is the ability to use dol-
lars that come into academic health centers for continuing
education.
We need to model what the future would look like under revised
rules. What would happen if commercial support went away com-
pletely, 50 percent, 25 percent? We also need to create the vision of
an alternative form of continuing education that might be smaller.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 137

Discussion Highlights
138
The enterprise might be smaller in its measurable size, fewer lec-
tures, etc., but the amount of education might be the same or larger,
using new technology.
If you take away commercial support, you are going to eliminate a
vast majority of the people who now provide continuing education.
It would be appropriate to look at what might be the unintended
consequences, and trying to address those in advance instead of
trying to pick up the pieces later.
If you look at hours of instruction by provider category, state
medical societies and schools of medicine are at the top, but state
medical societies get very little commercial support.
Without industry, someone has to play a larger role, maybe state
professional associations, or groups like Kaiser and the VA system
that are interested in quality of care. That applies to medicine, nursing
and everybody else. Kaiser has already stopped commercial support
of its continuing education programs.
It is possible that physicians would under invest in their own edu-
cation because they don’t think they get sufficient return on that
investment. One problem in medicine is that it is an imperfect
system for rewarding good performance, for there is no good way of
measuring quality at the individual physician level. But if physicians
under invest, there must be a societal investment that might come
from many sources, from corporations, from insurance companies,
from individual health organizations.
Top journals take ads from many companies to provide a pooling
of resources. They also build a firewall so that the advertising staff
does not know what is happening editorially. This may be a model
for funding CE.
We always talk about the cost when we should be talking about the
investment, but until we can demonstrate the return on investment,
we may not be able to make the business case.
If you separate everything immediately, there will be a huge vacu-
um and lack of support for continuing medical education. If there’s
no support, what happens to physicians in remote areas, who work
hard and have no time off? Perhaps the profession should find a
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 138

Discussion Highlights
139
way to help those members.
A common plea in community practice is that physicians don’t have
access to resources, that they’re too expensive. It is almost seen as
justification for getting their continuing medical education from
drug reps who visit their offices. This is a real issue that needs to be
addressed. If we pay for our stethoscopes, we should pay for infor-
mation we need. It is the job of the profession at large to help
doctors who don’t have the access.
A lot of department chairs will be absolutely petrified at the idea
that the slim profit margins they get from their continuing medical
education courses might go away. Institutions that are doing this in
a very profitable way are not going to want to give up that profit if
they can hang on to it.
I don’t have any problem with commercial people putting funding
into a pool and the only recognition is that they be listed along with
all the foundations and the government and other sources of revenue.
One approach could be to establish an independent commission
or some other entity that would be empowered to receive money
from any source and to promote improved patient care through
education and improvement in practice, that would reach across
professions, capitalize on the electronic capabilities, and represent
an enterprise for learning and improving the quality of care through
lifelong practice.
The government ought to have a major role in funding for research in
continuing education and funding for the development and acquisition
of IT capability by providers, The funding of continuing education,
per se, ought to reside with the profession in some form, individually,
by employers, or by professional organizations.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 139

140
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 140
III.
Designing Systems for
Lifelong Learning
to Improve Health
141
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 141
Continuing Health Professional Education
Delivery in the United States
David A. Davis, M.D. and Trina Loofbourrow, B.A.
Association of American Medical Colleges
This report focuses on the scope and delivery of continuing medical
education (CME) for physicians with respect to regulatory policy,
research, and data collection. There is less information available
for continuing education for nursing and pharmacy professionals;
continuing education for these professions is addressed in Appendix
A and Appendix B, respectively.
Background
The History of CME
The history of CME has been marked by two distinct areas of devel-
opment. The first is the development, production, and delivery of
CME activities and events themselves; the second is the CME credit
movement, leading to certification, membership in specialty organi-
zations, and licensure.
Developing and Producing CME Programs and Activities
. How old
is CME? Although the self-education of physicians has probably
existed for as long as the profession itself, the first formal reference
to continuing education for physicians came in the early 1900s,
when Sir William Osler articulated the importance of physician
education and urged the profession toward a position that recognized
clinical advances and sought methods to deliver them to practicing
physicians. Along with other advice, he urged the profession toward
a position in which it recognized clinical advances and sought
methods to deliver them to its member physicians.
The ensuing century brought with it many changes, including the
following:
— Changes in the model or delivery mode of CME from early out-
rider programs to large conferences and medical update sessions
— A clear understanding of adult learner theory and its application
to the CME process
— Adaptation of Tyler’s model of program design and evaluation
to CME
1
142
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 142

Davis & Loofbourrow
143
— A rapid increase in the number of courses and conferences
following World War II, brought about by new advances in the
biomedical sciences and physicians returning to practice
The last half of the twentieth century has been marked by the
following developments:
— The establishment and application of accreditation principles
to CME program design and delivery
— The use of information and distance education technology
— A focus on research and outcomes, leading to a stronger
emphasis on clinical performance and healthcare outcomes
— The growing presence of commercial interests in CME
Requiring CME for Licensure and/or Recertification
. Almost concur-
rently, there were movements in the licensure and expectations
of physicians about the “amount” of CME they might need in order
to maintain their competence. The first to reify CME “hours,” the
American Academy of Family Physicians (AAFP; then General
Practice), stipulated a 150-hour/3-year membership requirement
in the late 1940s, using the terms “formal” and “informal” CME. The
AAFP replaced this nomenclature in 1955 with the terms Category 1
and Category 2 to recognize these two forms of learning. Subsequently,
the American Medical Association (AMA) Physician’s Recognition
Award (PRA) was created, requiring a similar number of hours of
credit and consolidating, in 1985, several categories of learning into
two, following the lead of the AAFP.
2
Several changes in the credit system have evolved over the subse-
quent years. First, while formal CME can be conveniently measured
in hours, informal and self-directed activities cannot. Thus, “credit,” as
opposed to “credit hours,” has become the preferred term. Second,
given the self-reporting and immeasurable qualities of self-directed
learning, credit regulators have chosen to place caps on these latter
activities. Although it was not initially intended for this purpose, CME
credit has been used to meet the need for establishing or guaranteeing
practice competence. As a consequence, a robust movement has
arisen over the past three decades to link these credits to other
regulatory and membership requirements.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 143

Continuing Health Professional Education Delivery in the United States
144
First, licensure is strongly linked to CME participation. In 1971, the
state of New Mexico adopted a policy of relicensure based on
CME participation.
3
Many states have followed suit. Currently, CME
participation is mandated by the majority of state medical boards.
4
Within these policies, however, there are wide variations: Some of
the boards require that these credits be all or partly from the AMA
Physician’s Recognition Award system, and the number of hours
required ranges from 20 hours a year to 50 hours a year.
Second, the role of the medical specialty boards in assuring the
competence of their members is a long and familiar story. Physicians
who have met the (re)certification requirements of an American
Board of Medical Specialties (ABMS) member board receive an AMA
Physician’s Recognition Award certificate. Following its efforts to
standardize methods to ensure competence in the trainees of
graduate programs, the ABMS has undertaken the creation of an
extensive Maintenance of Certification program, with several ele-
ments, including 1) professional standing; 2) lifelong learning and
self-assessment; 3) demonstration of cognitive expertise; and 4)
practice performance assessment.
5
Third, the AMA Physician’s Recognition Award certificate meets the
CME requirements of the Joint Commission on Accreditation of
Healthcare Organizations (JCAHO) related to hospital accreditation.
Accreditation Bodies
Because most of the data in this report are derived from CME
accreditation sources, and these sources are important in the
delivery of CME, we outline some of the history and background
related to the accreditation processes.
The Accreditation Council for Continuing Medical Education
(ACCME) is the accrediting body for institutions and organizations
administering and accrediting CME programs used by physicians.
ACCME was established in 1981, taking over the accreditation
process from the AMA. Accreditation of CME providers in medicine
has been the subject of consideration and action for nearly four
decades. In the 1960s, under the rubric of a “coordinating commit-
tee” for medical education, initiatives were launched that led to the
creation of “liaison committees” for undergraduate, graduate, and
continuing medical education. In CME, the Liaison Committee on
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 144

Davis & Loofbourrow
145
Continuing Medical Education (LCCME) operated until 1978, when
it disbanded. Subsequently, the five major parents groups (AAMC,
AMA, Federation of State Medical Boards, American Hospital Associ-
ation, and American Board of Medical Specialties) joined with the
Council on Medical Specialty Societies and the Association for
Hospital Medical Education to form ACCME. Initially ACCME was
a small and voluntary organization with support from the AMA, but
ACCME has evolved to more robust and independent status, with
clear regulatory authority for the accreditation of CME providers in
the United States. In particular, its position on commercial support
and CME is widely regarded as the clearest statement about the
permissible nature and extent of such support in the United States.
ACCME is the most complex and detailed of the accrediting bodies,
and it is important to understand it fully. All providers, according to
ACCME standards, must have a clear mission, purpose, and scope;
have an organizational structure and business process appropriate
for its purpose; engage in a planning process that identifies learning
needs, states objectives, and presents CME in a way that complies
with clear commercial support standards; and evaluate the effective-
ness of programming for individual activities and for the program
as a whole.
Definitions
Shaped in large part by these historical and regulatory forces, CME
can be seen as a huge “enterprise,” comprising the production of
large numbers of courses, conferences, rounds, and other activities,
and led by the need to acquire credit hours. In this report, we use
the acronym CME to refer to the last and longest phase of education
undertaken by physicians. CME consists of any activity undertaken
to enhance competence, increase learning, and provide better care
for patients. It does not include master’s or doctoral level work
leading to an additional degree, and further, does not encompass
non-clinical learning, for example, education in the areas of business
management. More definitions are included in Appendix C. Other
definitions commonly used throughout this report include the
following:
— CPD, Continuing Professional Development: term used to
describe advancement by members of professional associations
to maintain, improve, and broaden the knowledge and skills
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 145

Continuing Health Professional Education Delivery in the United States
146
required by their profession; CPD may be seen as broader than
“CME” in the sense that it might encompass all forms of learning
and personal development, not just clinical education
— CEU, Continuing Education Unit: measurement used in continu-
ing education programs to define hours of participation in
qualified instruction
Methods
First, we looked for data reported in the United States produced
by the accreditation bodies of continuing education providers and
by other providers or provider organizations. Second, we made a
concerted effort to contact key informants in each discipline to
determine and validate our search strategies and to indicate other
data sources where available. Third, we searched and reviewed the
literature, using the key words “accreditation of continuing education
providers”and similar terms, to round out our findings and to provide
a perspective that would be helpful in generating comments for the
paper’s conclusions. We augmented this process with a Google
search on relevant key words and on the websites of professional
associations and authorities in five countries. Key words used to
elicit results were accreditation, CME/CNE/CPE accrediting body,
continuing medical education, continuing nursing education, and
continuing pharmacy education, as well as their respective acronyms.
In each discipline, we developed a series of questions and compiled
the responses we found. For results dealing with continuing educa-
tion in the nursing profession see Appendix A, and for results
dealing with the pharmacy profession, see Appendix B.
Results
I. Using the most recent data available, what are the major cate-
gories of CME providers? A wide variety of CME providers exists
in the United States, and these providers are categorized various-
ly across the disciplines. The ACCME employs the following
categories of CME providers:
6
1. Government/military (e.g., Centers for Disease Control and
Prevention; US Food and Drug Administration Center for
Drug Evaluation and Research; and National Institutes of
Health Foundation for Advanced Education in the Sciences)
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 146

Davis & Loofbourrow
147
2. Hospital/healthcare delivery system, including
consortium/alliance (e.g., Advocate Healthcare; Children’s
National Medical Center; and Georgetown University
Hospital)
3. Insurance company/managed care company (e.g.,
American Physicians Assurance; America’s Health
Insurance Plans; and Medical Mutual Group)
4. Nonprofit, including not-for-profit foundation, voluntary
health association (e.g., American Cancer Society;
BioSymposia, Inc.; and Brain Trauma Foundation)
5. Nonprofit, including physician membership organization
and specialty physician member organization (e.g.,
Academy of Psychosomatic Medicine; Alliance for
Continuing Medical Education; and American Academy of
Allergy Asthma and Immunology)
6. Not classified/other (e.g., American Academy of Medical
Management; American Board of Quality Assurance and
Utilization Review Physicians; and American Society of
Health-System Pharmacists)
7. Publishing/education company, including communications
company, education company, and publishing company
(e.g., The Academy for Continued Healthcare Learning;
Academy for Healthcare Education, Inc.; and Advanced
Health Education Center)
8. School of medicine (e.g., Albany Medical College; Baylor
College of Medicine; and Boston University School of
Medicine)
9. State medical societies
The ACCME provides two avenues of accreditation: accreditation as
a provider and accreditation of an organization as an approver. The
first eight categories listed above are accredited by the ACCME as
providers of CME. In contrast, state medical societies are accredited
as approvers of CME. The state medical societies then accredit
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 147

Continuing Health Professional Education Delivery in the United States
148
organizations within their own states as providers of CME. In 2005,
the AACME reported 2322 separate providers, only a slight increase
from 2003, in which they reported 2295 providers (no data available
prior to 2003). State medical society–approved providers comprised
69 percent of providers offering CME.
The publishing/education company category includes medical
education and communication companies (MECCs). This is a hetero-
geneous category, comprising entities that are public or private,
profit or not for profit, and focused on publications or other forms
of CME that provide medical education and information to health-
care professionals. These bodies provide CME mostly in the form of
courses, enduring materials, Internet activities, and journals. Courses
comprise almost half (48 percent) of the CME activities provided by
the publishing/education companies; they contribute 12 percent
of all CME course activities offered by CME providers. The Alliance
for Continuing Medical Education (ACME) and North American
Association of Medical Education and Communication Companies
(NAAMECC) are two organizations advocating for these companies;
the former group provides membership through a section (the
Medical Education/Communication Company Alliance, MECCA).
The NAAMECC provides advocacy and education for its member
companies. It represents 87 member organizations, of which 47
percent are accredited by the ACCME as providers of CME.
In addition to those findings recorded under “medicine” are the
activities reported by the American Osteopathic Association and its
accrediting body. In 2003, 162 provider organizations were accredited
by the American Osteopathic Association. In this instance, provider
organizations included affiliates (nonpractice and practice) (1),
colleges (19), foundations (6), hospitals (53), military (1), profes-
sional associations (1), and societies (81). In 2004 through 2006,
a total of 14.1 million credit hours were recorded by the American
Osteopathic Association over a 3-year cycle. This number is a slight
increase from the previous 2001 to 2003 cycle with a value of 13.1
million total credit hours.
7
The American Osteopathic Association
establishes the accreditation policy for sponsors of osteopathic CME,
but the Council on Continuing Medical Education has been given
the authority to monitor the osteopathic CME by the American
Osteopathic Association Board of Trustees.
8
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 148

The role of the states in accrediting CME providers seems, if not
particular to medicine, then certainly a striking feature in that disci-
pline: it is by far the largest accrediting category. Finally, a number
of educational companies and pharmaceutical companies or com-
mercial interests produce accredited CME, often for profit.
II.
What are their “activities”? To what extent do they list and describe
the courses and other learning formats (e.g., self-assessment
programs, quality assurance/improvement, etc.). The following
activities are listed as major categories of CME activities from
the ACCME:
1. Courses
2. Regularly scheduled conferences
3. Test item writing
4. Committee work
5. Performance improvement
6. Internet
Davis & Loofbourrow
12000
11500
11000
10500
10000
9500
9000
8500
8000
7500
7000
6500
6000
5500
5000
4500
4000
3500
3000
2500
2000
1500
1000
500
0
Courses Regularly Test Item Committee Performance Internet Other Journal CME &
Scheduled Writing Work Improvement Enduring Journal-Based
Conferences Materials
Government/ Hospital/ Insurance Non-profit Non-profit Not Publishing/ School of State Medical
Military Healthcare Company/ (Other) (Physician Classified Education Medicine Society
Delivery Managed Care Membership Company
System Company Organization)
P R O V I D E R C A T E G O R Y
N U M B E R O F A C T I V I T I E S
Figure 1.
Accreditation Council for Continuing Medical Education 2005
Annual Report Data Depicting the Breakdown of Number of
Activities by Provider Category
149
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 149

7. Other enduring materials
8. Journal CME and journal-based manuscript review
Overall, CME activities are focused on courses, regularly scheduled
conferences (the current name for rounds and other regular confer-
ence such as tumor boards), and activities through the Internet.
Courses comprise 57 percent of the activities offered by providers,
followed by regularly scheduled conferences at 19 percent and
Internet activities at 15 percent. Figure 1 shows the number of CME
activities reported in the Council’s 2005 annual report. Here again,
we see that the largest number of accredited providers were state
medical societies, and as expected, these societies delivered a large
portion of the activities. The state medical societies provided all of
the activities listed under the major categories. Sixty-seven percent
of their approved offerings were described as courses; regularly
scheduled conferences generated 26 percent of their activity.
The state medical society category includes all data by all providers
approved by these societies. These accredited providers produced
41 percent of the CME activities for medical education in 2005. In
2005, state society–accredited providers produced courses, regularly
scheduled conferences, test item writing, committee work, perform-
Continuing Health Professional Education Delivery in the United States
460000
440000
420000
400000
380000
360000
340000
320000
300000
280000
260000
240000
220000
200000
180000
160000
140000
120000
100000
80000
60000
40000
20000
0
Figure 2.
Accreditation Council for Continuing Medical Education 2001
through 2005 Annual Report: Accredited Hours of Instruction
by Provider Category
2001 2002 2003 2004 2005
Government/ Hospital/ Insurance Non-profit Non-profit Not Publishing/ School of *State Medical
Military Healthcare Company/ (Other) (Physician Classified Education Medicine Society
Delivery Managed Care Membership Company
System Company Organization)
P R O V I D E R C A T E G O R Y
N U M B E R O F H O U R S
150
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 150
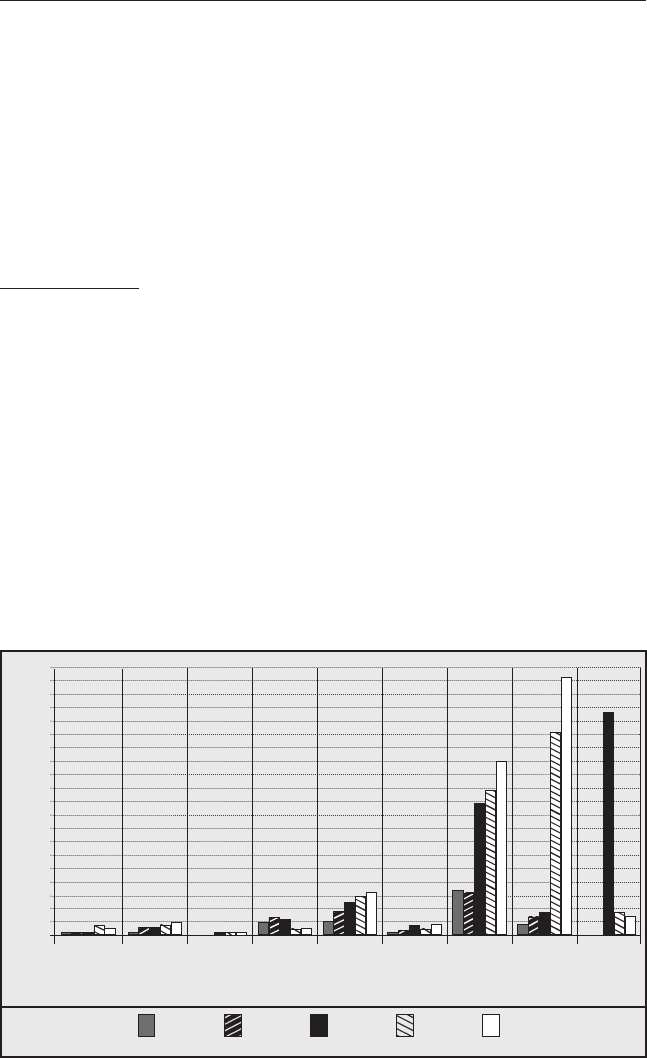
ance improvement, Internet activities, enduring material, and journal-
based activities with courses and regularly scheduled conferences
comprising 94 percent of the activities delivered.
III. What trends can be observed over time?
The data reveal several trends over the 5-year period covered by this
report, primarily from ACCME data from 2001 to 2006, augmented
by data from the Society for Academic CME (SACME) in 2006.
General trends
. Figure 2 shows accredited hours of instruction from
2001 through 2005, obtained from the ACCME annual report. Hours
of instruction have increased gradually (along with an increase in
the number of accredited providers, from 674 [2001] to 2322 [2005]).
Because data were not available for 2001 and 2002 for state medical
societies, we used data from 2003 through 2005. A slight downward
trend can be observed in the reporting of the number of hours of
state medical society accredited provider activities from 2003 to
2005. In contrast, and with the additional exception of the non-profit
category, all providers appear to have increased production of their
activities. Several of these providers report a peak in 2004 and
slightly less production in 2005, although overall the trends are
upwards. Clearly the production of 360,000 hours of accredited CME
Davis & Loofbourrow
Figure 3.
Number of Internet Activities by Provider Category, 2001–2005
2001 2002 2003 2004 2005
Government/ Hospital/ Insurance Non-profit Non-profit Not Publishing/ School of *State Medical
Military Healthcare Company/ (Other) (Physician Classified Education Medicine Society
Delivery Managed Care Membership Company
System Company Organization)
P R O V I D E R C A T E G O R Y
NUMBER OF INTERNET ACTIVITIES COMPLETED
10000
9500
9000
8500
8000
7500
7000
6500
6000
5500
5000
4500
4000
3500
3000
2500
2000
1500
1000
500
0
151
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 151

Continuing Health Professional Education Delivery in the United States
152
activity by medical schools continues to lead the field among single-
provider entities.
Self-study Activities (Internet and Media-based Programs)
. Internet
activities, including live activities, searching and learning, online,
and Web-based enduring materials, have increased dramatically over
the past 3 years, a trend we observed especially among the publish-
ing/education companies and schools of medicine (Figure 3).
Since 2001, the ACCME data show a rise in the use of online courses,
online use of enduring materials, and accessing information using
the Internet for most of the providers. The largest increase occurred
for publishing/education companies beginning in 2003, and for
school of medicine providers, who significantly increased their
Internet-enabled activities in 2004. Harris et al.
9
studied the use of
online programs for CME and discovered that younger physicians
and women physicians appear to be using online programs at a
faster rate than their male, older counterparts. In 2003, state medical
society–approved providers first reported data on Internet-based
CME to the ACCME. The first year there was a spike of Internet
activities followed by a dramatic decrease in the number of activities
for 2004 and 2005. Explanations for this spike include the reporting
of a backlog of activities launched prior to 2003 and adjustments to
the ACCME activity category titles.
In contrast, the use of the Internet for conferences or self-study
activities, as recorded by a biennial survey of the Society for
Academic CME (SACME), has not increased. In 2006, the SACME
noted that only 9 percent of the schools reported using the Internet
to broadcast conferences, a slight increase from 1998 at 5 percent.
Internet self-study activities reported for 2004 and 2005 remained at
68 percent, essentially unchanged from other comparative data
(2002–2006) but much greater than the 25 percent reported in 1998.
Self-study CME in some format (Internet, written, audio, and video)
has increased slightly from 74 percent in 1998 to 80 percent in 2006.
Based on data from the SACME, four of five medical school CME
divisions offer self-study activities: over two thirds offer Internet
courses, 56 percent offer print-based materials, 51 percent provide
computer-based learning, and about a quarter offer video- or audio-
based resources.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 152

Davis & Loofbourrow
153
Courses and Regularly Scheduled Conferences. Courses continue to
be the main area of CME activity for all ACCME-approved sponsors
and state medical societies. Whereas the percentage of courses
produced has declined (from 57 percent of all activities in 2001 to
49 percent in 2005), their total number has risen.
Over a 5-year period, we noted a clear downward trend in the num-
ber of regularly scheduled conferences, from 40,000 to less than
15,000 since 2003. This phenomenon may be accounted for in part
by the rise in the number of Internet activities, course activities,
audio and video activities, and Web-based learning.
Conferences conducted by hospitals, healthcare delivery systems,
and state medical societies have dropped in number by 50 percent
since 2003. It appears that these providers have shifted to course
activity. In contrast, accredited regularly scheduled conferences
conducted by schools of medicine remain a large and rather fixed
component of their activity, based on data from the SACME.
Courses remain a high percentage of the CME reported by the
SACME. In the 2006 survey data, 36 percent of the medical schools
reported more than 100 courses being offered. This is an increase
from 1998, when only 21 percent of the medical schools reported
more than 100 courses.
Performance and Quality Improvement
. In 2004 the AMA and AAFP
approved performance improvement as a CME activity, following
calls for such activity on the part of other specialty societies, the
Accreditation Council for Graduate Education,
10
and clear directions
from the research literature about the efficacy of more direct, point-
of-care educational interventions based on performance and other
objective data. The response, however, has been lukewarm. In their
annual survey, the SACME reported in 2006 that only one quarter
of the responding medical schools provided between one and 20
performance improvement activities. A further 5 percent offered
Internet point-of-care learning activities. In addition, while over 80
percent of schools had full affiliations with hospitals, less than a
third were “somewhat” or “a lot” linked with hospital programs
geared toward education or quality improvement.
ACCME began reporting on performance improvement activities in
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 153

2005. In 2005, performance improvement activities constituted less
than 1% of the total number of activities provided by CME sponsors
and state medical societies. These numbers were unchanged in 2006.
Commercial Support
. In 2005, accredited providers reported a
total income of $2,250,468,669 to the ACCME. Of this amount,
$1,115,597,071 was income from commercial support, or slightly
under half of the total income. This overall figure is identical to that
reported by the SACME in 2006 and similar data from the same year
developed by the ACCME; however, the ACCME data indicate about
60 percent of commercial support. In contrast, in 2001, 41 percent of
the income was reported as emanating from commercial support. In
2005, the hospital/healthcare delivery systems, publishing/education
companies, and schools of medicine received more than 50 percent
commercial income. Commercial income reported by the state med-
ical society providers is reflected in the commercial total in 2003
and 2004 and does not include the income total for comparison. The
total commercial income reported by state medical society providers
has declined from $51,775,737 to $37,588,680 since the first year of
reporting in 2003.
The categories of publishing/education companies, non-profit
(physician membership organization), and schools of medicine
Continuing Health Professional Education Delivery in the United States
Figure 4.
Accreditation Council for Continuing Medical Education
2001 through 2005 Annual Commercial Income by
Provider Category
2001 2002 2003 2004 2005
Government/ Hospital/ Insurance Non-profit Non-profit Not Publishing/ School of *State Medical
Military Healthcare Company/ (Other) (Physician Classified Education Medicine Society
Delivery Managed Care Membership Company
System Company Organization)
P R O V I D E R C A T E G O R Y
INCOME DOLLARS / MILLIONS
600
550
500
450
400
350
300
250
200
150
100
50
0
154
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 154

Davis & Loofbourrow
155
exhibit an increase over time in the amount of commercial support
for CME activities (Figure 4). In 2005, all categories declined in the
amount of commercial income except the publishing/education
companies, which increased their commercial support by almost
$70 million. Commercial income for publishing/education companies
also increased in 2006.
Based on the 2006 biannual report of the SACME, more than 60
percent of medical schools reported that commercial support for
their CME activities was increased by more than a third. These
figures showed an increase from 1994 to 1995, when only 6 percent
of medical schools reported more than 60 percent of commercial
revenue. In addition, 15 percent of the medical schools indicated
that more than 20 percent of courses were supported by only one
commercial company. This is an increase from 1994 and 1995, when
15 percent of the medical schools reported support from one
commercial company.
The SACME summarizes this issue by indicating that commercial
support forms the largest source of income for their medical school
members. A useful way to express this is to describe the “typical”
(or median) medical school. Based on the same report, the “typical”
medical school produces 83 courses per year, generating over 700
hours of credit and attracting nearly 3000 physicians and 1500 other
professionals. Of these courses, slightly over half, or 45 courses,
were sponsored by commercial interests. This support is sufficiently
robust that an average of 11 courses/year would be cancelled if
it were not for the financial aid provided by commercial entities.
Further, of these 45 courses, two, on average, were supported by
only one company.
Forces Affecting the CME Enterprise
Apart from the need to maintain competence, we see several major
forces, challenges. or directions which form integral parts of the
picture of CME in the United States.
Accreditation of CME Providers
Along with the credit system, another movement in CME has led
to the accreditation of CME/CPD providers. ACCME was the first
organization in the United States, and perhaps the world, to develop
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 155

standards for CME. Providers seeking this accreditation status must
demonstrate that their programs have met the standards, referred to
as the Essential Areas and Elements (including the Standards for
Commercial Support) and Accreditation Policies, developed by
ACCME. Accreditation is awarded for a period of 4 to 6 years. CME
providers maintain compliance during the term by voluntarily
continuing to meet the ACCME standards and are required to submit
annual reports to maintain accreditation. Recognition as an accreditor
is awarded to state medical societies, which subsequently accredit
providers within their state.
There is a strong dependence on formal CME, such as courses,
conferences, and similar live, face-to-face meetings. None require
content-specific learning objectives to be met, though two groups
specify discipline-based content in family medicine (AAFP) and
osteopathic medicine (American Osteopathic Association). In all
these programs,
— “Other” categories form an eclectic mix. They can include teach-
ing or preceptoring activities; attaining credit at the master’s or
graduate level or subspecialty certification; writing/publishing
in the medical literature; poster presentations; and advanced
degrees, self assessments, and research (American Medical
Association CME Physician resources for CME, 2005).
— There exists a clear movement away from exclusively formal CME
to acknowledging participation in a wide range of educational
activities, now including Web-based learning, although these
activities are still considered voluntary.
— While clearly linked to quality in the description of categories,
there is no or little specific mention of quality improvement
or peer-reviewed programs in the materials produced by the
appropriate organizations, for example, the AMA Physician’s
Recognition Award materials. Pilot programs have been docu-
mented,
11
but where such initiatives are mentioned, they are
considered optional.
We identified some unique elements among the programs, including
the following:
Continuing Health Professional Education Delivery in the United States
156
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 156

Davis & Loofbourrow
157
— Recognition of excellence: the American Osteopathic Association
offers a certificate of excellence, and fellowship in the College of
Family Physicians of Canada is awarded based on extra work of
a reflective, or performance-based nature, leading to extra credits
in a program called Mainpro-C.
— Specific content: certain associations (American Academy of
Family Physicians, American Osteopathic Association) distinguish
between those programs designed for and by their members, or
with their membership in mind, and those accredited programs
accredited or developed by other organizations.
— The Royal College of General Practitioners in the UK is the first
program to remove the requirement for “credit” entirely. The
requirement in this program — the formal annual peer appraisal
process — is unique among its peer programs in medicine.
In medicine, parallel to the accreditation process for CME, the
Accreditation Council for Graduate (residency) Medical Education
(ACGME) has also made a sizable impact on the training of residents
and the expectations of their programs. In particular, we note the
advent of the ACGME competencies, which articulate new dimen-
sions of care and learning. These competencies are instructive not
only at this level of training but also at the CME level. They include
systems-based practice, which focuses on the healthcare system; the
judicious use of resources and other matters related to the practice
environment and its constraints and resources; and practice-based
learning and improvement.
A listing of continuing education requirements for medicine by state
is available at thewebsite of theAmerican College of Emergency
Physicians.
12
Professionalization and Training for CME Providers
A further force for change in the context of CME/CPD has been the
drive toward certification and increased training on the part of CME
providers. Coming from a wide variety of backgrounds — confer-
ence management and planning, adult education, educational
psychology, medicine and allied fields, business management —
such providers have formed two professional associations in North
America. The first of these is the Alliance for CME (ACME), an
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 157

organization with over 2000 member groups comprising CME/CPD
professionals in medical schools, hospitals, private organizations,
communication companies, and other commercial interests. Much
smaller, at a tenth the size, the SACME has its roots primarily among
medical school deans and directors of CME and focuses less on
the technology and broad scope of CME (the primary interest of the
Alliance) and more on its research and development interests. Both
organizations, now in their third decade, have grown in size and
importance in the number and type of training programs offered
to expand the professional repertoire of CME providers.
In addition, the Journal of Continuing Education in the Health
Professions and the Journal of Continuing Nursing Education
provide scholarly work to drive this provision, based in adult
education, informatics, quality improvement, and other disciplines.
Commercialization of CME
We note the strong influence of pharmaceutical (and increasingly)
technology-based companies, evident in the reports from the
ACCME and in the survey data from the SACME. Concern about the
extent to which such influence might drive the CME/CPD “agenda”
or its curriculum has given rise to clear statements from ACCME
and other organizations about creating firewalls and reducing bias
in presentations or content. Nonetheless, concerns remain, and
increasing pressures (as recently as this summer, from the Senate
Finance Committee about the question of oversight in this area) may
well affect this picture. The picture of commercialization of CME has
also been marked by an increased presence of medical education
and communication companies, originally constituted as a section
within the ACCME, and now represented by NAAMEC, the North
American Association of Medical and Education Companies. Initially
construed as publishing companies, these organizations now provide
a wide range of educational activities, are of a profit or not-for-profit
nature, and are heavily subsidized in many instances by commercial
interests. There has been some debate as to whether these companies
should be considered legitimate purveyors of CME.
The Methods of Continuing Education: Outcomes and Options
Increasing attention has been paid to the “outcomes” of CME, with
examples including competency-based assessment, performance, and
Continuing Health Professional Education Delivery in the United States
158
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 158

Davis & Loofbourrow
159
healthcare outcomes. Competency-based assessments of skills or
knowledge are commonplace in CME. Examples include self-assess-
ment programs and tests of knowledge frequently mounted by the
specialty societies. Increasing emphasis on simulation techniques
(post-course testing of resuscitation skills on mannequins, for example)
has made this process simpler and more ubiquitous and may drive
some of the CME agenda in future years. Further, emphasis has
also grown on the performance of physicians in the work or practice
setting, giving rise to consideration of performance measures and
their utility to measure such outcomes. Finally, patient outcomes—
though somewhat distal to the CME or CPD activity, are also key to
any discussion about the future of CME. It is clear that the “clinical
practice gap,” expressed by the Institute of Medicine
13
and Rand
reports,
14
is a product of some failures on the part of the CME enter-
prise to transfer knowledge in a way that is timely and useful.
Results from studies of the effectiveness of CME, especially in medi-
cine, shape the discussion of the future of CME. While not the focus
of this paper, these studies lend themselves to an observation of the
mismatch between “what is” (a situation in which less than effective
didactic lectures and conferences dominate the CME delivery picture)
and “what should be” (using methods such as academic detailing,
reminders, or feedback, which have a larger effect, relative at least
to physician performance improvement). This is not to say that
formal conference-based CME should cease to exist, but rather that
it has a purpose (the dissemination of new information, for example)
that would be useful at least to some clinicians but that must be
carefully tailored and matched to learning and course objectives
and the practical and clinical learning needs of all professionals
considered the target of an educational intervention.
Commensurate with our understanding of the delivery of educational
interventions and their effect — or lack of it—has grown an increased
awareness of the lack of self-assessment abilities. As summarized by
Davis and colleagues,
15
it appears as though in many situations, and
across many disciplines, professionals have difficulty judging their
past performance, current learning needs, or future competencies
without some form of benchmarking or feedback.
Finally, while the research in this area is still descriptive, it appears
that the technology of CME/CPD is changing rapidly. New vehicles
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 159

to “deliver” educational content include information and communi-
cation technology, represented by personal digital assistants (PDAs),
audio- and video-casting, Web-casting, and computer-based programs.
Despite its wide variety of modalities, such technology holds both
the promise and the reality of bringing informational resources to
the practice setting, addressing the need for “just in time” learning.
To the extent that such learning is therefore more useful and can
directly affect patient care, and that it might provide the clinician
with more feedback or benchmarking, we imagine that these tech-
nologies will be more effective and widespread.
Social, Contextual, and Practical Issues Shaping CME
Many forces for change arise from the current practice environment.
First among these is the nature of the environment itself, which is
marked by increased demands on time, the pressures of generalism,
the advent of new biopsychosocial pathologies, and the social
implications of disease and its management. Second and added to
this complex picture is the heavy information burden that challenges
all health professionals, described as the “drinking from a fire hose”
phenomenon. Compelling reasons for changing the system also come
from a heightened awareness of gaps in the delivery of healthcare,
with a gap between what is known in prevention, disease manage-
ment, or treatment and what is actually done.
13,14
Finally, we note
the issue of social accountability for physicians and the need to
assure the public of the safety of their practices. In this process of
advocacy, perhaps the most compelling voice is that of the patient.
Norcini
16
suggests that patients believe that revalidation is necessary,
focusing on performance in practice.
Summary: Certain Challenges, Possible Solutions
This report focuses on the numbers of clinicians participating or the
numbers of courses. Little if any attention is paid— either in the report
or the data from which it is derived — to the content or method of
educational delivery, the site of this “delivery,” or its effect on the
patient or the healthcare system. Thus, it is evident to us that what
we portray here — the numbers and types of courses and other
offerings, the history and processes of accrediting bodies, and the
processes of producing education — operates at a level removed
from the actual delivery of care or even the delivery of education.
Further, these elements operate in ways that appear to be at odds
with what is currently known about physician learning and change.
Continuing Health Professional Education Delivery in the United States
160
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 160

Davis & Loofbourrow
161
Examination of this complex structure reveals a heavy dependence
on at least two major premises on which these systems are built,
and on which their linkages to competence, performance, and
healthcare outcomes are maintained. The first is the dependence on
the physician’s ability to self-assess learning needs and to direct his
or her attention to meeting them; the second is the heavy depend-
ence — despite attempts to augment this category of learning or
add new independent learning methods to it — on formal CME or
similar educational activities, such as clinical meetings, rounds, and
conferences.
We do not wish to say that any aspects of this system are broken or
irreparable, or that the system has not been based on a strong and
expressed intent to monitor quality. Instead, we end this report with
a summary of each of the areas we have looked at along with sug-
gestions for consideration of possible solutions.
The Physician
Among the major issues this report identifies is the extent and perva-
sive nature of commercial interests in the production of CME. While
some have called for a complete disengagement of commercial
funding from accredited CME, it is clear that such influences will
remain—whether in accredited formats or otherwise. Further, it
appears from the literature that self-assessment of professionals is
limited — despite its use in determining learning needs — and is at
least to some extent contingent on benchmarking and feedback.
A more coherent solution to the issues of bias in content and less-
than-adequate self-determination of learning needs may involve the
training and assurance of competency for physicians in the domains of
evidence-based healthcare and in appraising their own performance.
Including these measures as requirements of CME professionals may
ensure that these groups are better equipped to critically appraise
the research literature, judging for themselves the effect of med-
ications, weighing management strategies, and making rational,
evidence-based decisions. Further, training in self-assessment and
critical reflection based on objective feedback appear to be important
elements in training from undergraduate to graduate education and
certainly beyond. We note the introduction of “required” instruction
in certain elements mandated by some states and suggest that courses on
evidence-based medicine also be considered in this manner.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 161

Continuing Health Professional Education Delivery in the United States
162
The Educational System: Methods and Means
Despite a large and growing body of literature indicating that didactic
conferences appear to be less than optimally effective in changing
provider performance, the CME enterprise continues to concentrate
its efforts in the production of courses and regularly scheduled
conferences. This is not to say that there are no examples of other
interventions, such as academic detailing or reminders at the point
of care, but these appear not to be generated by CME providers, or
at least not documented in the activity profiles of CME providers.
In this light, we suggest that CME providers, led by an active and
evidence-based accreditation process, move to a more comprehensive
understanding of the literature of CME and to incorporation of its
results into the production and delivery of educational interventions.
Further, we urge providers to document these changes in a way that
makes tracking more readily achievable.Such a process may be enabled
by stronger and more explicit accreditation criteria in these areas.
Accrediting Educational Systems
Our investigation has shown a wide variety in accreditation and
reporting customs in the United States. Medicine has developed
a robust and detailed process leading to the accreditation of its
providers. Other developed nations appear to have much less need
for such accounting and rarely report these activities. These models
permit us to imagine a world with several possibilities:
— No CME accreditation system except for that provided by the
health systems and health professionals themselves to monitor
their own competence and performance. Such systems appear to
be much more commonplace outside the United States. We would
argue against such “deregulation” for two reasons. First, accredit-
ing educational competency appears to be a tall order for the
more clinical accrediting bodies to undertake. Second, such a
process might permit serious irregularities in the delivery of
educational interventions and puts too much weight on the
consumer-clinician-learner to judge the value of all educational
materials. Finally, the lack of an accrediting body leaves a void,
allowing no one to act as spokesperson or to lead the profes-
sions toward a posture of best educational practice.
— An accreditation system that is less individualized and less focused
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 162

on the specifics of the programs and content, allowing for more
focus on establishing standards or structural criteria to show a
provider the right path for developing a CME program. Here for
example, ACCME or an equivalent body would set high standards
or guidelines that organizations could adopt and implement in
their set of accreditation standards/processes. To some extent,
this has already occurred at the state medical society level.
— A more robust and rigorous accreditation system, including the
following features:
– Increased attention to making essentials and standards match
the principles of effective CME delivery.
– Heightened capacity to measure and provide feedback to
CME providers at a more detailed practice-based level to
ensure compliance with standards and essentials. Such feed-
back would not preclude the use of accreditation processes
as educational.
– An increase in measuring performance or outcomes rather
than and in addition to numbers of activities, hours, and
providers.
– Increased attention to the content of CME interventions,
stressing adherence to best evidence (and downplaying the
more negative approach to reducing commercial interests).
Such a process would allow for encouragement and tracking
of the incorporation of new competencies, such as those
proposed by the Accreditation Council for Graduate Medical
Education.
– The possibility of co-locating CME, CNE, and CPE data, allow-
ing for common terminology, agreed upon across systems, as
well as certification, transportability, clarity, and observability.
Strong movements toward more focus on accreditation provide an
argument for increased measurement of performance or outcomes.
First, an international commitment to improving quality medical
education began in 2004 when the World Health Organization
(WHO) and the World Federation for Medical Education (WFME)
developed the WHO/WFME Guidelines for Accreditation of Basic
Medical Education. These guidelines or recommendations provide
Davis & Loofbourrow
163
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 163

Continuing Health Professional Education Delivery in the United States
164
assistance for providers and institutions in developing best practices
and an accreditation system. The Guidelines, which are accessible at
http://www.wfme.org/, consist of fundamental requirements of an
accreditation system, the legal framework, organizational structure,
standards and criteria, the process of accreditation, main elements
in the process of accreditation, decisions on accreditation, public
announcement of decisions, and benefits of accreditation. Second, in
healthcare and business, examples of this movement toward quality
and accreditation include the Baldridge Awards, Toyota’s lean prin-
ciples, and the International Organization of Standardization.
We urge support for a stronger and more evidence-based accredita-
tion system of CME. Such a process would meet the goals we have
outlined and help to close the gap in clinical care.
Certifying the Competence of the Learner-Clinician
and the Healthcare System
In the clinical realm, two major regulatory forces exist: the accreditation
of hospitals and healthcare systems and the licensing of physicians
by state medical boards and their certification by specialty boards. The
Joint Commission (until 2007 called the Joint Commission on Accredi-
tation of Healthcare Organizations [JCAHO]) develops standards and
provides evaluation and accreditation services for healthcare organi-
zations and programs in the United States.
17
The Joint Commission
uses surveyors who conduct onsite surveys at healthcare organiza-
tions to evaluate their operational practices and facilities.
Here we note the clear disconnect between the degrees to which
clinician competencies are determined in undergraduate and gradu-
ate health professional training versus CME. In CME, competency is
determined by the proxy measure of total number of hours spent in
lectures, the equivalent of awarding a medical degree based on class
attendance.
In this area, we note several findings from other jurisdictions and
studies of relevance to a discussion about improving the CME
“system” and its role in healthcare:
— Appraisal and the learning portfolio: The UK has developed a
system of peer appraisal using a learning portfolio for its general
practitioners, who comprise 50 percent of the physician popula-
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 164

Davis & Loofbourrow
165
tion. Here a senior, trained physician meets on a yearly basis
with a colleague and reviews a file of performance and compe-
tency data, along with a list of CME activities. Such a process
recognizes the complex layering and dimensionality of physician
competence and performance and “triangulates” self-learning
and self-identified needs, competency, and performance. In such
systems, strict adherence to the science (ie, reliability, validity,
and generalizability) of measurement should be incorporated
along with principles of adult learning.
— The concept of relative value, as described by Davis and Willis.
2
— Applied principles of quality improvement, such as METRIC
(Measure, Evaluate, Translate Research into Care), developed by
the AAFP.
— Finally we note the advent of 360-degree assessments of clini-
cian performance adapted from the business world. Here
measurements of performance are made by questionnaire or
survey of colleagues and patients.
18
We urge a more complete understanding of CME requirements and
their role in the assurance of competency and quality, both individu-
ally and collectively in the healthcare system. Such an understanding
may come from convening separate meetings to address this ques-
tion across disciplines, or in providing support for the work of one
or more national groups already engaged in this process.
Acknowledgments
The data collection efforts of this report were the responsibility of
Trina Loofbourrow, employed as an intern by the Association of
American Medical Colleges in 2007. In addition, we recognize the
significant help and input of Dr. Murray Kopelow, Laure Perrier,
Paul Mazmanian, Anne-Marie Sesti, and Marian Taliaferro.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 165

REFERENCES
1. Tyler RW. New trends in education. Am J Psychiatry. 1966;122:1394–1398.
2. Davis NL, Willis CE. A new metric for CME Credit. J Contin Educ Health Prof.
2004;24:129–144.
3. Derbyshire RC. Relicensure for continued practice. J Med Licens Discipline.
2003;89:16–22.
4. Johnson DA, Austin DL, Thompson JN. The role of state medical boards in CME.
J Contin Educ Health Prof. 2005;25:183–189.
5. Miller SH: ABMS and reposition for excellence in lifelong learning: maintenance of
certification. J Contin Educ Health Prof. 2005;25:151–156.
6. Accreditation Council for Continuing Medical Education. Accessible at
http://www.accme.org (Access date: March 15, 2008).
7. Rodgers DJ. Osteopathic continuing medical education. J Am Osteopath Assoc.
2007; 107:67–81.
8. DO-Online Accreditation and Program Approval. Accessible at https://www.do-
online.org/index.cfm?PageID=acc_main. (Access date: March 10, 2008).
9. Harris JM Jr, Novalis-Marine C, Harris RB. Women physicians are early adopters of
on-line continuing medical education. J Contin Educ Health Prof. 2003;23:221–228.
10. Accreditation Council for Graduate Education. Accessible at
http://www.acgme.org/acWebsite/home/home.asp (Access date: March 10, 2008).
11. American Medical Association Physician Recognition Award. Accessible at
http://www.ama-assn.org/ama/pub/category/15889.html (Access date: March 10, 2008).
12. American College of Emergency Physicians. CME Requirements by State. Accessible
at http://www.acep.org/cme.aspx?id=22366 (Access date: March 15, 2008)
13. Committee on Quality of Healthcare in America, Institute of Medicine. Crossing the
Quality Chasm: A New Health System for the 21st Century. Washington, DC:
National Academy Press; 2004.
14. McGlynn EA, Asch SM, Adams J, et al. The quality of healthcare delivered to adults in
the United States. N Engl J Med. 2003; 348:2635–2645.
15. Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy
of physician self-assessment compared with observed measures of competence.
JAMA. 2006;296:1094–1102.
16. Norcini JJ. Where next with revalidation. BMJ. 2005;330:1458–1459.
17. The Joint Commission, About Us. Accessible at http://www.jointcommission.org/
(Access date: March 10, 2008).
18. Lipner RS, Blank LL, Leas BF, Fortna GS. The value of patient and peer ratings in
recertification. Acad Med. 2002;77(Suppl):S64–S66.
Continuing Health Professional Education Delivery in the United States
166
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 166

APPENDIX A:
Continuing Education in the Nursing Profession
The earliest continuing nursing educational activities date back to
the late 1800s, when alumnae associations sponsored continuing
education (CE) activities for their members. In 1899, the Teachers
College at Columbia University, Department of Domestic Science,
offered a course in Hospital Economics—the first that would corre-
spond to what we currently consider CE.
1
At the time, nursing
education took place through hospital apprenticeship, and physician
education was moving toward the university. Nursing education,
including postgraduate work, grew substantially in the 1900s, but
nurses’ salaries remained very low. The concept of a “free” course
evolved, wherein nurses would trade work in order to attend a
course. In the 1920s, the American Nurses Association (ANA) and
the National League for Nursing Education (NLNE) began offering
“institutes” or short courses, and the Teachers College at Columbia
University began offering free CE.
In the 1960s, federal legislation (Title VIII in 1964 and the Medicare
Act in 1965), along with the establishment of the first coronary care
unit, laid the groundwork for federally funded CE efforts, in turn
leading to increased support at the university and college level.
The growing movement toward nursing specialization led to further
CE opportunities to establish certification in specialty areas. In 1976,
the American Nurses Association established the first accreditation
system for providers of nursing CE, and hospitals began sponsoring
CE programs for staff and non-employees through colleges, univer-
sities, and outside consultants. Professionalism in nursing remains
an important topic. Decreased government funding for CE and a call
to reduce non–bachelor degree nurses will reduce the number of
nurses requiring CE. One emerging area for nurses is in home care,
which will require a new form of CE focusing on home care tech-
niques and technologies.
1
State boards of nursing were established over 100 years ago to ensure
safe nursing practices. Requirements for maintaining licensure vary by
state. A summary of nursing requirements organized by state is avail-
able online at http://www.allnursingschools.com/faqs/boards.php.
The renewal period may be yearly or bi-yearly and varies from state
167
Davis & Loofbourrow
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 167

to state, as do contact hour requirements, which may be specific for
one topic, such as a 4-hour course on infection control every 4 years
(New York State Board of Nursing), or constitute a general require-
ment, such as 30 contact hours per renewal period (California State
Board of Nursing).
Methods
First, we looked for data reported in the United States produced by
the relevant accreditation bodies. Second, we made a concerted effort
to contact key informants to determine and validate our search
strategies and to indicate other data sources where available. Third,
we searched and reviewed the literature, using the key words “accredi-
tation of CE providers” and similar terms to round out our findings
and to provide perspective helpful in generating comments for the
paper’s conclusions.
Accrediting Bodies
The American Nurses Credentialing Center (ANCC) is a subsidiary
of the ANA tasked with managing its accreditation and certification
programs. The ANA established a voluntary accreditation system in
1974 for continuing nursing education. The governing organizations
of the accreditation system formed a National Accreditation Board,
and its five regional accrediting committees (RACs) accredited the
first program in 1976. Since that time, the governing bodies have
been consolidated into three regional committees, and in 1984,
the National Accrediting Board changed its name to the Board on
Accreditation. In 1988, the governance permitted the designations
of provider and approver accreditation. The new system provided
two common pathways for organizations seeking accreditation:
through the Board on Accreditation or through an accredited
approver. The ANA Center for Credentialing Services incorporated
itself as a separate entity called American Nurses Credentialing
Center (ANCC) in 1991. The ANCC takes on the additional roles of
examinations and certification renewals through the Certification
Program. The Center is accredited by the American Board of Nursing
Specialties and the National Commission for Certifying Agencies.
Categories of CE Providers
Similar to its colleagues in medicine, The ANCC employs the following
categories of CE providers:
168
Appendix A
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 168
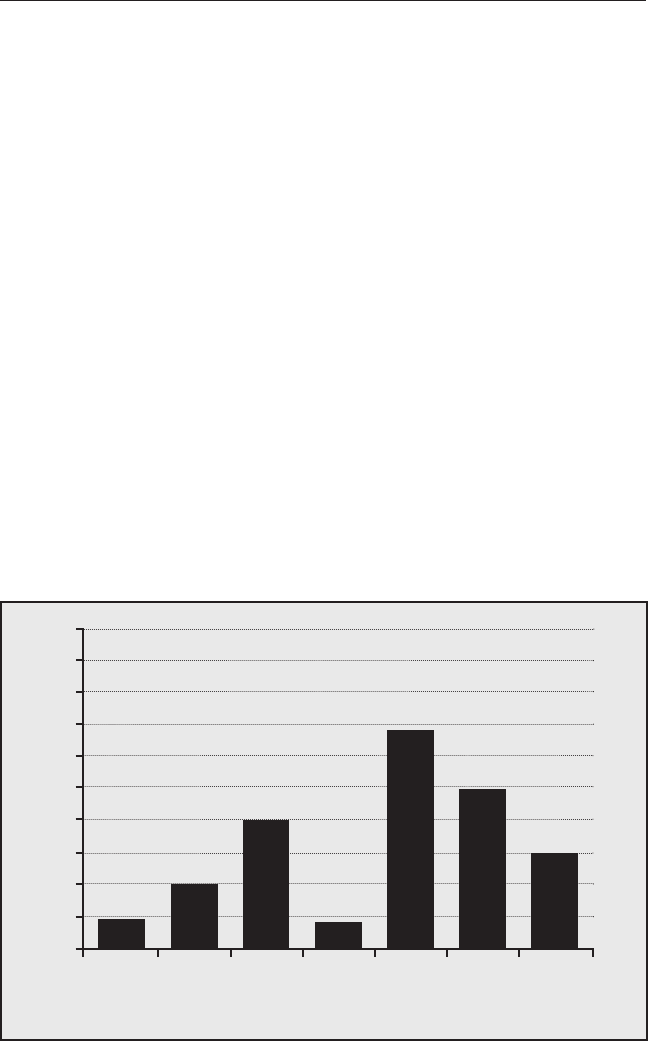
169
Figure 1.
The Number of American Nurses Credentialing Center
Accredited Providers of Continuing Nursing Education in
Each Provider Category for the Year 2005
100
90
80
70
60
50
40
30
20
10
0
Government/ Hospital/ Specialty Private Publishing/ School State
Military Healthcare Education of Nursing Association
System Company
PROVIDER CATEGORY
NUMBER OF PROVIDERS
Davis & Loofbourrow
1. Government/Military (e.g., Centers for Disease Control and
Prevention; Naval Medical Education and Training Command;
and Joint Commission Department of Education)
2. Hospital/Healthcare Delivery System (e.g., Albany Medical
Center Hospital; Allina Hospitals and Clinics; and Children’s
Hospitals and Clinics)
3. Private (e.g., American College of Cardiology Foundation;
Annenberg Center for Health Sciences at Eisenhower; and
Audio-Digest Foundation)
4. Publishing/Education Company (e.g., Allegra Learning Solutions,
LLC; American Academy of CME, Inc.; and Anderson Continuing
Education)
5. School of Nursing (e.g., Georgetown University School of Nursing;
Indiana State University School of Nursing; and Indiana University
School of Nursing)
6. Specialty (e.g., American Association. of Occupational Health
Nurses; American Association of Critical Care Nurses; and American
Association of Diabetes Educators)
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 169

170
7. State Association (e.g., Alabama State Nurses Association;
American Holistic Nurses Association; and Arizona Nurses
Association)
In order to draw a comparison with physician data, we assigned a
provider category to each of the 224 providers based on the ACCME
categories. A large proportion of accredited providers for nursing
CE are publishing/education companies, at 30 percent, and schools
of nursing, at 22 percent (Figure 1). These percentages differ from
those for CME, in which the state medical societies comprise most of
the accredited providers.
Activities and Commercial Support
Searching the professional organizations’ websites and contacting
key individuals failed to yield data or statistics for recent or compar-
ative years on continuing nurse education activities and commercial
support. We learned through correspondence with the ANA that
they do not collect data from accredited providers, and previously
collected data were distributed only to those who were accredited.
Accreditation of Continuing Education Providers
Providers seeking ANCC accreditation must demonstrate that their
programs have met the Commission on Accreditation (COA) criteria
developed by the ANA. Continuing nursing education programs are
either accredited as providers for a 6-year term or by an Approver,
called a Constituent Member Association (CMA), for a 3-year term.
CMA-approved recognition is only available for ANA constituent
member associations, nursing specialty organizations, and federal
nursing services. CE activities approved by a CMA are only valid
for 2 years.
REFERENCES
1. Stein AM. History of continuing nursing education in the United States. J Contin Educ
Nurs. 1998;29:245–252.
Appendix A
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 170

APPENDIX B:
Continuing Education in the Pharmacy Profession
In the 1940s, about 35 schools of pharmacy began offering some form
of continuing pharmacy education.
1
After World War II, workers return-
ing to the pharmacy profession found a need for refresher courses,
and by the 1970s healthcare workers were encouraged at the federal
level to continue education in their field. Florida and Kansas were
the first states to establish regulations of minimum CE for renewal of
the pharmacist license. These regulations stimulated new programs
and concern for development of standards and assessing results.
1
Currently, all states have legislation mandating pharmacy CE for re-licen-
sure. These requirements are available in summary form online at
(http://www.acpe-accredit.org/pdf/2006StateBOPRequirements.pdf.)
Methods
First, we looked for data reported in the United States produced
by the relevant accreditation bodies. Second, we made a concerted
effort to contact key informants to determine and validate our
search strategies and to indicate other data sources where available.
Third, we searched and reviewed the literature, using the key words
“accreditation of CE providers” and similar terms to round out our
findings and to provide perspective helpful in generating comments
for the paper’s conclusions.
Accrediting Bodies
The Accreditation Council of Pharmacy Education is a national
agency accrediting professional degree programs and providers
of continuing pharmaceutical education. In 1932, the American
Association of Colleges of Pharmacy helped establish the American
Council on Pharmaceutical Education as an accrediting body setting
standards initially for pharmacy baccalaureate degree and doctor
of pharmacy programs. The formal accreditation process replaced
the earlier practice of school visits. The Accreditation Council for
Pharmacy Education expanded in 1975 to establish standards for
CE providers, and in 2003 the American Council on Pharmaceutical
Education changed its name to the Accreditation Council of
Pharmacy Education.
171
Davis & Loofbourrow
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 171

172
100
90
80
70
60
50
40
30
20
10
0
Colleges or Educational Local, State Publishers, Hospitals,
Schools Companies and or National Government Healthcare
Pharmaceutical Associations Agencies, etc. Networks
Manufacturers
PROVIDER CATEGORY
Figure 1.
The Number of Accreditation Council for Pharmacy Education
Accredited Providers of Continuing Pharmacy Education in
Each Provider Category for the Year 2005
NUMBER OF PROVIDERS
Appendix B
Categories of Continuing Education Providers
The Accreditation Council for Pharmacy Education (ACPE) employs
the following categories of CE providers in its reports.
1. Colleges and Schools
2. Education Companies and Pharmaceutical Manufacturers
(Pharmaceutical manufacturers were no longer accredited as of
July 2005 and did not supply data)
3. Local, State or National Associations
4. Publishers, Government Agencies, etc.
5. Hospitals, Healthcare Networks
Figure 1 shows the breakdown of number of providers by provider
category for the year 2005 year. The distribution of the 388 providers
is spread evenly among all the categories. Educational companies
and pharmaceutical manufacturers; colleges or schools; and local,
state, and national societies show the highest number of CE
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 172

173
Davis & Loofbourrow
providers.
We compared the ACPE 2005 data to data they published in 1985.
Colleges, schools, and associations remain the largest providers,
although, as is the case for continuing medical education, the
number of medical education companies has increased.
Activities
The following activities are listed as major categories from
the ACPE:
1. Live Activities
2. Home Study Activities
3. Combined Activities (activities that contain both live and home
study or mediated components)
4. Computer/Internet Activities
The total number of activities accredited in 2005 was 22,876. The
number has remained relatively stable since 1985. Live CE activities
composed almost two thirds (59 percent) of the total for 2005,
a percentage unchanged over time (in 1985 this figure was 54
percent). Home study CE activities comprised 39 percent, and
Internet activities 16 percent.
Accreditation of Continuing Education Providers
Providers seeking ACPE accreditation must demonstrate that their
programs have met a published set of standards, and accredited
programs can apply to the ACPE if they wish to grant ACPE certifi-
cation to their participants.
REFERENCES
1. Sonnedecker G. Kremers and Urdang's History of Pharmacy. American Institute for
the History of Pharmacy; 1986:246–248.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 173

APPENDIX C:
Definitions and Acronyms
DEFINITIONS
Categories of credit:
1
— Category 1: Activities such as publishing articles, poster presenta-
tions, medically related advanced degrees, and independent
learning. Examples include the American Medical Association
Physician’s Recognition Award Category 1 (AMA PRA Category
1), developed by the AMA as a method of assigning credit for
CME activities provided by approved CME providers and American
Osteopathic Association (AOA) method of assigning credit for
formal (A) and less formal (B) osteopathic CME activities.
— Category 2: Activities such as consultation with peers and medical
experts, small group discussion, self assessment activities, med-
ical writing and teaching residents. Examples include American
Medical Association Physician’s Recognition Award Category
2 (AMA PRA Category 2), developed by the AMA as a method
of assigning credit for CME activities provided by approved CME
providers and American Osteopathic Association (AOA) method
of assigning credit for formal (A) and less formal (B) non-osteo-
pathic CME activities.
• Committee Work: involvement in formal committees of hospitals
or professional organizations
• Computer-based, Instructional Program: accessed on a CD-ROM
or other computerized modality
• Conference: live, audio- or video-mediated, face-to-face or
web-based meeting of people planned in order that learners
acquire knowledge and/or discuss a topic
• Course: generally a live instructor-led session planned on a
one-by-one basis with learner participation in person
• Credit: the designation used to assign a value to continuing
education classes or time performed by the learner; in general,
174
Appendix C
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 174

credit is referred to in hours, as in hours of credit obtained
• Enduring Materials: learning resources used by clinicians,
generally printed, recorded or computer-based
• Internet or Web-based Activity: a CE experience available online
(e.g., live, enduring material, searching and learning)
• Journal CME and Journal-based: reading of an article, a
provider stipulated/learner directed phase (include reflection,
discussion, or debate about the material contained in the article)
and requirement for the completion by learner of a pre-deter-
mined set of questions or tasks relating to the content of the
material as part of the learning process
• Manuscript Review: participation in pre-publication review
process of a journal article
• Performance Improvement: physician identifies an educational
need through a measure of performance in practice, engages in
educational experience, integrates into patient care and then re-
evaluates performance
• Regularly Scheduled Conferences (RSC): planned, ongoing series
of sessions, generally involving members of a staff or organiza-
tion (e.g., hospital rounds)
• Regularly Scheduled Series (RSS): previously described as RSCs,
these have a series with multiple sessions occurring on an ongo-
ing basis, primarily planned and presented by an accredited
organization (e.g., Grand Rounds, Tumor Boards)
• Self Study: educational materials provided in paper, video, or
web-based to be completed at the learner’s convenience, often
accompanied by self-assessment examinations or other tests of
knowledge and skill acquisition
• Test Item Writing: participation in pre-publication development
and review of test items (e.g., multiple choice questions)
• Video and Audio: media used to assist with learning activities,
often used to assess clinical-decision making
175
Davis & Loofbourrow
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 175

• Workshop: live face-to-face meeting marked by the instructor-led
presentations of concepts and principles followed by real-time
application, such as the presentation of cases, to generate dis-
cussion, analysis, and demonstration of knowledge
ACRONYMS
• AAFP, American Academy of Family Physicians
• ACCME, Accreditation Council for Continuing Medical Education
• ACPE, Accreditation Council for Pharmacy Education
• AMA, American Medical Association
• ANA, American Nurses Association
• ANCC, American Nurses Credentialing Center
• AOA, American Osteopathic Association
• CACME, Committee on Accreditation of CME
• CFPC, College of Family Physicians of Canada
• MOC, Maintenance of Certification
• RCPSC, The Royal College of Physicians and Surgeons of Canada
• SACME, Society for Academic Continuing Medical Education.
REFERENCES
1. Accreditation Council for Continuing Medical Education. Accessible at
http://www.accme.org/index.cfm/fa/index.cfm/fa/home.home/home.cfm
(Access date: April 4, 2008).
176
Appendix 3
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 176

177
Remarks by Pamela H. Mitchell, Ph.D, M.S., B.S.
University of Washington School of Nursing
I appreciate David Davis’s paper because when I was asked to
provide some information about CE from nursing, I wondered where
I was going to get that information. His paper confirmed that we
don’t have the same kind of information in nursing as is available in
medicine. However, we do have a substantial amount of continuing
education in much the same formats and courses as medicine, most
of which are accredited by The American Nurses Credentialing
Center (ANCC). It is useful to spend a bit of time talking about the
providers in nursing because most of our discussions have been
specific to continuing medical education.
As in medicine, several groups provide continuing nursing education.
Historically, university programs in nursing have been involved
in continuing education. In the 70s and 80s, specialization began
through the HRSA programs. (Nursing has Title 8 and medicine has
Title 7.) The two together, were part of what started specialization.
I would group the six categories in the Davis paper into four for
nursing. First are the schools of nursing. These include university
based schools of nursing that target primarily people who have
been prepared at the bachelors level or the advanced practice level,
such as nurse practitioners who are now doctors of nursing practice.
The community college programs are aimed primarily at the begin-
ning level and provide basic refreshers. Practice-based education in
hospitals is driven largely by requirements of the Joint Commission
and is aimed at point-of-care certification, maintenance of skills, and
development of new skills, with some team-based work. The nurs-
ing specialty organizations are another major force, and specialized
nursing programs are analogous to medicine. Finally, some state
nursing organizations are involved in CNE.
For the specialty organizations, maintaining and upgrading skills
in a particular nursing specialty certification that doesn’t require an
advanced degree often drives continuing education. That is probably
the area where commercialization is most evident in continuing
nursing education. If you go to the critical care nurses’ annual
meeting, with the big exhibits and all of the monitoring devices,
many of the exhibitors are also providing CE independent of the
CE that is being provided in the courses.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 177

I don’t think the state organizations for nursing are as prominent as
they are in medicine, although I am from a state that does not have
mandatory continuing education, so our state nurses association
does relatively little. Those states with mandatory continuing educa-
tion have more active state nursing associations. Whether you have
mandatory continuing education or not drives the CE effort. In my
state we briefly had mandated CE, but then the state board of nursing
realized that it didn’t have the money to monitor a program, so it
cancelled it. So we are basically on our own as to whether or not
to do continuing education.
All the accreditation of providers is through ANCC. ANCC doesn’t
collect data about the number and categories of courses, but it does
accredit providers on the basis of whether the planning committee
knows something about the topic, the same sort of thing as in medical
education. We have not gone as far as medicine has in terms of the
competencies and practice based provision and assessment, and
those are areas where we can learn a great deal.
In nursing, everybody and nobody is responsible for CE. Everyone
has some stake as an individual, namely his or her own accreditation.
But the accreditation authority does not set the standards for what
CE should look like. There are simply standards for whether you are
documenting appropriately, who planned it, how long each session
is, and whether it is a lecture, but not whether it is interactive.
There has been some work on outcomes and whether CE really
changes practice, but not to the extent that we see in continuing
medical education.
My guess is that commercialization is probably about the 10 percent
of what was shown in Robert Steinbrook’s graph, but it is mostly the
vendors who help support the conference. Some of the vendors also
provide some CE but most don’t. If we ask is there a model for what
it would look like if we had to pay for our own continuing educa-
tion, CNE is one model because such a small percentage is paid for
commercially. That is not because we are purer than everybody
else. It is an accident of history that we haven’t been prescribing as
long and only a small part of the nursing workforce prescribes.
However, in hospitals and in some of the specialty organizations,
nurses do influence what gets bought in terms of specialized beds
178
Remarks
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 178

and monitoring equipment and the like, so that is where you see the
opportunity for commercialization to bias the education. In states
where CNE is mandatory, nurses themselves and their employers
pay for CE and we have good continuing education, so I think it is
entirely possible to do it without 60 percent of it being funded by
commercial sources.
Another question that I would ask is whether we should have a
more centralized set of expectations about what is appropriate CE.
That gets to the topic of lifelong learning, which is not the same thing
as delivering CE. My personal belief is that we ought to start with
the expectation that we must learn throughout our lifetime of pro-
fessional practice from the very date we start professional education.
We should be educating ourselves together around those things
where we have common interests with the expectation that we will
continue to do it and not simply with a set of CE offerings. It should
be a habit of professionalism that we should expect of ourselves,
and of our students. I think that we should be doing a great deal
more of this together across the professions. Nursing and medicine
have much more in common than we have separately. In particular,
when we are talking about team-based performance, we should be
having some team-based learning, and that means that we should
have common sets of expectations for the lifelong learning and for
that which is accredited.
Formalized credit does drive what becomes part of continuing
education. In nursing what is counted has been far more the confer-
ence, the continuing education hours of lecture because it is easier
to count; self-learning doesn’t count as much. We need to rethink
that, and this is a prime opportunity to rethink it together. I think
we could blow it up and try all over again.
DISCUSSION HIGHLIGHTS
The evidence base for what works or is needed for continuing edu-
cation must be fairly flimsy, given the range of requirements state by
state. For instance, osteopaths in Vermont must be three and a half
times more effective than physicians in New Hampshire because
they have to take that many more hours.
179
Mitchell
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 179

It makes no sense for states to have such different requirements.
The continuing medical education community needs to define what
is important to deliver the best care and then go to the Federation
of State Medical Boards.
The status quo means that marketing products is the major incentive
of CME, not improving the quality of healthcare. It is time to develop
a system that cleans up the wildness of the status quo. Both under-
graduate and graduate medical education are structured and regulated
and produce a standard product, with a guarantee that most
graduates have a comparable set of competencies. It is time for
continuing medical education to have a system with some kind of
institutional oversight, curriculum design, a focus on quality and
outcome measurements, and no conflict of interest. We need a faculty
that can do that, using modern methods, and practice-based learn-
ing based on patient needs and outcome evaluation.
The incompetencies of physicians to teach are striking. Will new
competencies be required to provide the kind of help people are
asking for, or will excellent models be lost because of the absence
of education for the educators in this new kind of education?
Already many institutions have established teaching academies
utilizing excellent faculty educators to help faculty improve the way
they teach.
The purpose of continuing education is to assure competence and
provide accountability. We should be open to radically different
systems that can provide that assurance. One way might be a system
that rewards high performing organizations. Why should individuals
who are part of such organizations have to undergo continuous
competency assessment? The organization has demonstrated it
produces a good product and takes responsibility for the competency
of people who work there. Or, if individuals maintained certification
through a demanding and intense process, that should substitute
for continuing education requirements. What we need is to accredit
systems and groups that perform on a reliable basis and produce
high quality healthcare, but because we lack measures for that kind
of performance, we have to look at the individual.
In hospitals, it is amazing how much linking reimbursement and
publicly provided quality information has focused attention on qual-
180
Discussion Highlights
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 180

ity improvement. For example, at our institution, influenza vaccina-
tion rates were especially low; suddenly, groups of professionals
came together to address this issue and came up with solutions.
Mobilization of the system became much easier and vaccination
rates went up. Contrast that with the more traditional approach in
which you test a clinician on the criteria for vaccination — what age
group, comorbidities, etc.
How much responsibility should academic medical centers have
for CE? We clearly are responsible for undergraduate education,
nursing, allied health, medicine, public health, etc. Every school
of medicine has infrastructure for GME and graduate nursing educa-
tion, but that is not necessarily true for CME. System CE is beyond
most academic medical centers. Maybe we can provide the support
for the educational part, but we cannot reformat whole health systems.
Our role should be to support the educational piece.
In North Carolina, practice-based networks link pediatric practices to
the medical school, so that the practices can continuously improve
their performance. That is one way academic medical centers can
support healthcare systems.
We need a consistent approach to collect CE information across pro-
fessions. Sixty percent of states now require CNE, but we have few
details about it. Also, CNE is too often influenced by “disease-of-the-
month” state legislation.
Regularly scheduled accredited conferences are decreasing in fre-
quency because it is too difficult to get accreditation, especially now
with the new requirements about conflict of interest. Medical educa-
tion and communication companies do not offer regularly scheduled
conferences because they don’t fit their business model.
We’ve had conversations, at least among continuing medical educa-
tion providers, that sounded like this for 30 years, but nothing ever
came of them, For the first time in three decades, we have the
opportunity to take these ideas and work them into something tan-
gible and workable.
181
Discussion Highlights
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 181

182
Learning to Work Together
to Improve the Quality of Healthcare
Maryjoan D. Ladden, Ph.D., R.N.
Harvard Medical School
Reports from the US Institute of Medicine have highlighted the fact
that almost 100,000 people die each year due to medical errors.
1
,2
These reports have focused national attention on the quality and
safety of healthcare. In addition, they have generated a considerable
amount of research on the causes of medical errors, strategies for
improving the quality and safety of care, and redesigning the health-
care system.
According to the Joint Commission,
3
communication failure was the
cause of over 70 percent of the errors or sentinel events reported to
them in the 10 years between 1995 and 2005. Several factors contribute
to communication failures. These include early training that teaches
nurses and physicians to communicate differently, historical power
differentials between the health professions that prevent patients
from speaking up, and lack of standardized communication proce-
dures to help create a shared mental model.
4
Many of the Joint
Commission’s 2008 Patient Safety Standards are aimed at structuring
and improving communication between health professionals.
The Institute of Medicine reports led researchers to develop and test
strategies for improving communication, collaboration, and teamwork.
Researchers have also explored links between effective communica-
tion, teamwork, and improved quality and safety. Jain et al.
5
found
that implementing four key system changes in the intensive care unit
(ICU) — including interdisciplinary rounds and a focus on team
decision making — had a significant impact on nosocomial infection
rates, the number of daily adverse events in the ICU, average length
of stay, and average cost of an ICU episode. Between baseline and
re-measurement periods, nosocomial infection rates declined for
ventilator-associated pneumonia (from 7.5 to 3.2/1000 ventilator
days, P = 0.04) and bloodstream infections (from 5.9 to 3.1/1000 line
days, P = 0.03), with a downward trend in the rate of urinary tract
infections (from 3.8 to 2.4/1000 catheter days, P = 0.17). The
researchers also observed a strong downward trend in the rates of
adverse events in the ICU and in the cost of an average length of
stay per episode (from $3406 to $2973). The authors concluded that
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 182

a systematic approach, including implementation of multidiscipli-
nary teams and the use of evidence-based bundles, improved
communication and patient outcomes.
The US Department of Veteran’s Affairs (VA) has also focused on
enhancing communication, interprofessional collaboration, and
teamwork to decrease adverse events and improve patient outcomes
within the VA system. From 2003 to 2007 they implemented a VA
Medical Team Training program in 43 VA medical centers across the
United States.
6
The program, which is based on aviation principles
of crew resource management, includes a full-day interactive learning
session, administration of pre-and post-intervention safety attitudes
questionnaires, and follow-up semi-structured interviews.
The Reality of Collaboration and Teamwork in Practice
Every day in practice, health professionals must work together to
address a patient care issue or solve a systems problem. In some
situations (ICU, operating room), an explicit structured interprofes-
sional approach is necessary. In others, health professionals may
come together once or twice around a specific patient or clinical
issue and then return to their independent work. Both of these
examples require a team, defined as two or more individuals who
have specific roles, perform interdependent tasks, are adaptable,
and share a common goal.
7
Most clinicians learn about teamwork on the job. Health professionals
are educated on improving relationships between patients and
healthcare providers. However, enhancing communication, collabo-
ration, and teamwork among health professionals is rarely included
in educational curricula. Effective communication and teamwork are
not a consequence of grouping health professionals together in the
same location or designating them as a team. Teamwork requires
knowledge of and respect for the skills and contributions of others
as well as positive attitudes toward collaboration.
8
In its 2003 report on education in the health professions, the Institute
of Medicine included “work in interdisciplinary teams” as one of the
five core competencies to be required by all healthcare professionals
to meet the needs of the 21st century healthcare system.
9
These
recommendations have been embraced by healthcare organizations,
the health professions, and accreditors.
3,10–13
183
Ladden
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 183

Preparing Health Professionals for Teamwork
and Collaboration
Despite the recommendations and the evidence that effective team-
work is necessary for high-quality, safe care, health professionals
have few real opportunities to learn how to work together. Most
health professional education in the formative years remains in
discipline-specific silos. Didactic instruction occurs in separate
buildings, and even though medical and nursing students may share
the same site for their clinical training, they (and their faculty) do
not know each other or work together — even if they are caring for
the same patient.
Education in the Formative Years
Many individuals have suggested that exposure to other disciplines
early in the professional education continuum will foster respect
for one another’s skills and positive attitudes toward collaboration,
leading to improved communication and teamwork. Since the 1960s,
interprofessional education, defined as when healthcare professionals
learn together, learn from each other, and learn about each others’
roles, has been promoted as a way to stimulate collaboration.
However, in the formative years of professional training, interpro-
fessional education is often stymied by such factors as scheduling
logistics, mismatch in learner’s age and educational level, and
academic policies.
14
The results of early interprofessional education efforts have also
been mixed. Anecdotally, educators report positive changes in
attitudes toward collaboration. However, in 2001, Zwarenstein et al.
15
concluded in a Cochrane meta-analysis that evaluation studies
lacked the methodological rigor to show the impact of interprofes-
sional education in the formative years on professional practice
and/or healthcare outcomes.
Some might still argue that, because the formative years in profes-
sional education are an impressionable time, this period represents
the best opportunity to instill the values and skills required for
effective teamwork and collaboration. Interprofessional teaching
and learning efforts during these years are necessary, but they are
not sufficient to assure successful collaboration and teamwork after
graduation. Once in practice, health professionals experience a
184
Learning to Work Together to Improve the Quality of Healthcare
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 184

healthcare system that supports a discipline-specific focus and
upholds the norms and attitudes that deter collaboration.
1
6
They also
often see their colleagues modeling behaviors and attitudes that do
not support collaboration.
17–19
Education in the Practice Years: Using Continuing Education to
Improve Collaboration and Teamwork
The early training years are just the beginning of a long continuum
in professional education. In most states, continuing education (CE)
is required for re-licensure. CE is also one component of professional
certification. Medicine has developed a professional competency
framework, with its Maintenance of Certification program, that
encourages life-long learning and practice improvement. Nursing
is not far behind in the competency movement.
Over the course of their career, health professionals spend more years
in continuing professional education, both formal and informal, than
they do in their early professional training. The audience for most
CE programs, from small office-based activities to large auditorium
conferences, is already often interdisciplinary. Physicians and nurses
learn side by side about best practices in clinical care management.
How can we use CE to foster collaboration and teamwork values
and skills and improve the quality of the care we deliver? In their
re-analysis of the Zwarenstein et al.
15
findings on interprofessional
education, Koppel et al.
20
identified three factors that make CE an
ideal venue for teaching and learning interprofessional skills and
values. These factors are the duration of the program, the location of
the program, and the developmental stage of the learner. Koppel et
al.
20
found that programs that engage interprofressional learners
over a longer time period are more likely to generate behavior change
in the individual (provider or patient) or organization. Many CE
programs are held over several days, with content presented in
a variety of learning formats. In these programs, interprofessional
concepts and skills could be (and should be) integrated with the
clinical content to demonstrate interprofessional management of
acute and chronic conditions.
Teamwork and collaboration could be presented in a didactic case-
based format and then reinforced over the next few days in smaller
185
Ladden
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 185

discussion groups, active exercises using real-life patient scenarios,
and skill-based workshops with feedback. Likewise, simulations of
common team management situations or resource management
principles would be useful interprofessional additions to a clinical
CE program. Because many clinicians attend the same professional
meeting each year, a curriculum could be developed to reinforce
and then expand interprofessional concepts, teamwork, and collab-
oration skills over time.
In terms of location, Koppel et al.
20
found that CE programs at
the practice site are more likely to produce behavior change in the
clinician, patient, and organization. Small CE programs at a practice
site or hospital draw clinicians who are already working together.
Interprofessional concepts and skills could easily be integrated into
clinical case presentations, as well as into other venues, such as
team meetings and quality and safety rounds. Because the clinician
audience is generally stable, new knowledge and skills can also be
tested and reinforced over time.
To be successful, interprofessional education and practice efforts
need strong administrative and political support from clinical and
organizational leaders. Programs at the practice site are highly visible
and can easily engage both groups as faculty. In the era of pay-for-
performance and other financial practice incentives, political capital
can also be generated by linking CE programs promoting collabora-
tion and teamwork with improvements in quality and safety. These
improvements are more likely to occur when all the clinicians
responsible for a patient group or service come together to share
knowledge and experiences and then plan for and test practice
changes.
21
Koppel et al.
20
also found the learner’s developmental stage to be
an important factor in the success of interprofessional education.
Interprofessional education interventions early in professional training
had a positive impact on attitudes and knowledge, but these effects
did not last over time or translate into behavior change in practice.
However, when interprofessional education was used in CE with
practicing clinicians, it was more likely to produce individual and
organizational behavior change. Perhaps experienced clinicians,
because they have a broader world view, can more quickly recog-
nize the relevance of new knowledge and skills and integrate them
186
Learning to Work Together to Improve the Quality of Healthcare
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 186

187
Ladden
more easily into their practice repertoire.
Professional socialization plays an important role in how health
professionals approach collaboration and teamwork. Socialization
begins prior to and continues during professional training.
22
Attitudes
are often difficult to change until health professionals have the
opportunity to get to know each other in real-life practice situations.
Until that happens, stereotypes prevail and there can be only a
superficial understanding of other health professionals’ skills and
contributions to practice.
Health professional learners and practicing clinicians learn best when
new knowledge and skills are presented within the context of their
work and they can immediately recognize the applicability to patient
care. Presented outside the appropriate clinical context, collaboration
and teamwork can easily be seen as theoretical and “nice to know”
rather than practical and “need to know.” Quality and safety are
powerful incentives for health professionals. Educational programs
that link collaboration and teamwork with high-quality, safe, and
effective patient care may have the best chance of success.
23
REFERENCES
1. Institute of Medicine. To Err Is Human: Building a Safer Healthcare System.
Washington, DC: National Academy Press; 2000.
2. Institute of Medicine. Crossing the Quality Chasm: A New Healthcare System for the
21st Century. Washington, DC: National Academy Press; 2001.
3. The Joint Commission. Sentinel Events Statistics, 1995-2005. Accessible at
http://www.jointcommission.org/SentinelEvents/Statistics (Access date: August 25,
2007).
4. Leonard M, Graham S, Bonacum D. The human factor: the critical importance of
effective teamwork and communication in providing safe care. Qual Saf Healthcare.
2004;13:i85–i90.
5. Jain M, Miller L, Belt D, King D, Berwick DM. Decline in ICU adverse events, noso-
comial infections and cost through a quality improvement initiative focusing on
teamwork and culture change. Qual Saf Healthcare. 2006;15:235–239.
6. Dunn EJ, Mills PD, Neily J, Crittenden MD, Carmack AL, Bagian JP. Medical team
training: applying crew resource management in the Veterans Health Administration.
Jt Comm J Qual Patient Saf. 2007;33:317–325.
7. Salas, E, Dickinson, TL, Converse, SA. Toward an understanding of team perform-
ance and training. In: RW Swezey and E Salas, editors. Teams: Their Training and
Performance. Norwood, NJ: Ablex; 1992.
8. Firth-Cozens, J. Multidisciplinary teamwork: the good, bad, and everything in-between.
Qual Healthcare. 2001;10:65–66.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 187

9. Institute of Medicine. Health Professions Education: A Bridge to Quality.
Washington, DC: National Academy Press; 2003.
10. Accreditation Council for Graduate Medical Education: Outcome Project. Accessible
at http://www.acgme.org/outcome/project (Access Date: July 20, 2007).
1
1. American Association of Colleges of Nursing 2002. Nurse Practitioner Primary Care
Competencies in Specialty Areas: Adult, Family, Gerontological, Pediatric, and Women’s
Health. Accessible at http://www.aacn.nche.edu/Education/pdf/competencies
(Access date: July 20, 2007).
12. O’Neil EH and the PEW Health Professions Commission. Recreating Health
Professional Practice for a New Century. San Francisco: PEW Health Professions
Commission; 1998.
13. Walker PH, Baldwin D, Fitzpatrick JJ, et al., and the National League for Nursing
Appointed Interdisciplinary Health Education Panel. Building community: developing
skills for interprofessional health professions education and relationship-centered
care. Nurs Outlook. 1998;46:88–89.
14. Ladden MJ, Blair K, Moore S, Roberts K. Educating health professionals for collaborative
interprofessional team practice: lessons from the field. In: New Paradigms in
Advanced Nursing Practice: Teaching & Technologic Strategies in Nurse Practitioner
Education [monograph]. Washington, DC: National Organization of Nurse
Practitioner Faculties; 2003.
15. Zwarenstein M, Reeves S, Barr H, Hammick M, Koppel I, Atkins J. Interprofessional
education: effects on professional practice and healthcare outcomes. Cochrane
Database Syst Rev. 2001;1:CD002213.
16. McPherson K, Headrick L, Moss F. Working and learning together: Good quality care
depends on it, but how can we achieve it? Qual Healthcare. 2001;10:ii46-ii53.
17. Curran VR, Sharpe D, Forristall J. Attitudes of health sciences faculty members
toward interprofessional teamwork and education. Med Educ. 2007; 41:892–896.
18. Gardner SF, Chamberlin GD, Heestand DE, Stowe CD. Interdisciplinary didactic
instruction at academic health centers in the United States: Attitudes and barriers.
Adv Health Sci Educ. 2002;7:179–190.
19. Thomas EJ, Sexton BJ, Helmreich RL. Discrepant attitudes about teamwork among
critical care nurses and physicians. Crit Care Med. 2003;31:956–959.
20. Koppel I, Barr H, Reeves S. Establishing a systematic approach to evaluating the
effectiveness of interprofessional education. Issues in Interdisciplinary Care.
2001;3:41–49.
21. Langley GJ, Nolan KM, Nolan TW, Provost L. The Improvement Guide. San Francisco:
Jossey-Bass; 1996.
22. Oandasan I, Reeves S. Key elements of interprofessional education. Part 2: factors,
processes and outcomes. J Interprof Care. 2005;1(suppl):39–48.
23. Ladden MJ, Bednash G, Stevens D, Moore G. Educating interprofessional learners for
quality, safety, and systems improvement. J Interprof Care. 2006;20:497–505.
188
Learning to Work Together to Improve the Quality of Healthcare
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 188

189
Remarks by Carol Havens, M.D.
Kaiser Permanente Health Center
If we think of interdisciplinary education as simply putting people
from different disciplines in the same room so they all hear the same
thing, we’re wasting an opportunity to get the best that we can out
of the opportunity of educating team members to work together.
I was fortunate in my training as a family practice resident at UC
Davis, where they had an NP training program. As residents, we
were paired in teams with the NP and PA students. In the clinic, we
had a team with a resident paired with a PA student or an NP stu-
dent paired with a clinic nurse and a medical assistant. In this way,
we had the opportunity, as residents, to discover the highest and
best use of all the people on that team with the patients we were
seeing. Challenging complex patients fascinated the PA student I
was paired with and I liked well baby checks, so she had all the
really difficult patients and I took all the well baby checks.
As long as we are going to blow up this continuing education sys-
tem and start over again, I’d like to put in a plug for another step in
the process. Don Moore talked about establishing activities based on
the need — the gap between what is and what could be — and
designing your activities with that end in mind, so that you know
what you want to get out of the activity as you are planning it. I’d
like to add as a next step what is the process to get there and who
needs to be involved in that process, and then what is the best way
to educate for that. Then we can start looking at this team, this
group of people taking care of patients, and who should be provid-
ing what part of care.
That’s not unlike the collaboration between primary care providers
and specialists. I’m a primary care provider and I’m also a specialist
so I get to do both ends. There’s always that challenge between
when is it no longer a primary care problem and at what point should
I refer, and then who is going to do the follow up EKG after we’ve
done the CABG? If it’s not clear who’s going to do that, either things
don’t get done, or things get done twice and lead to unnecessary
duplication. It’s really important that we look at the process of care
and I think it’s great that we’re talking about systems of care, because
that is where it’s going to happen. We should be looking at the
whole process, at who should be responsible for what part and at
what point that hand off occurs.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 189

We talked about culture change, and this is another culture change.
We talked about the Lone Ranger physician in the United States, and
it’s interesting when I talk to my colleagues in a variety of practice
settings about team based care and the opportunities to work together,
they’re all for it. They think it’s a great idea. But, when you get
down to the nitty gritty, such as who is going to call back patients
with normal labs, the answer is always the physician, because that’s
my job and the buck stops with me. No matter what the job, the
physician should be doing it. I never quite understood the concept of
team care when the physician is supposed to be doing everything.
That’s not true for everybody, but a lot of physicians still feel that
way. Just getting them even to think about the team process, and
what the opportunities are and who could be doing what, is going
to be a challenge.
I am going to describe what we have done at Kaiser around the
issue of interdisciplinary education. The concept of team based care,
I think, is one that’s easier to understand in the practice than it is
in the theory. Our greatest successes have been in two areas. One
centers around patient safety, particularly around things like critical
events practice where we actually train teams and physicians to deal
with critical events. This is the process: First we explain your role,
then show this is where your role changes to this role, and how
you hand it off, and, finally, we actually have them practice. We do
simulations; we record who did what and we ask questions. How
did it happen? How did the hand offs work? Did anything fall
through the cracks? And, by the way, how did the patient do?
The other has been in chronic conditions management, where we’ve
had some success, and that’s very much team based care. It follows
the same process of looking at where we are with chronic conditions
and where we want to be, also what could be and what we need
to do to get there. Clearly, physicians are not going to be able to
do this all by themselves; they have a role. Nurses can’t do it all by
themselves; they have a role. We have the opportunity to look at
what’s the best way to provide the care for these patients with chronic
conditions. We ask who should be responsible for what and how
do we set it up so that everything happens as smoothly and as easily
as possible so that we get the best use of everybody involved, and
we make sure that the patients get the best care possible.
190
Remarks
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 190

191
All that was done with the end in mind, with a clear picture of how
we wanted those teams to function and what the roles were of
everyone on the team. Everybody agreed to what those roles were.
And our hope is that we can start building on those successes and
start demonstrating the opportunities and the advantages of both
team based care and training as teams so that people will start looking
for other opportunities and other places where that approach might
also be a success.
DISCUSSION HIGHLIGHTS
We need to think in a broader perspective about continuing education.
We fail if we fail to think of the continuing professional development
of all the health professionals with whom we are working.
Nurses and physicians follow a different path; physicians focus on a
specialty right after their residency while nurses tend to be prepared
as generalists and then either may stay generalists or may focus on a
specialty. One thing continuing education providers in nursing do is
role development because a nurse who is a good clinician and then
becomes a manager doesn’t necessarily have management skills.
The same is true with administration.
The whole staff development function is more characteristic of
nursing than medicine, partly because most nurses are “staff,” but also
because staff development is embedded in the culture of nursing.
These programs are not well organized or systematic. Some are
accredited, some are not, but a lot of money goes into this work
and it isn’t looked at in any systematic way.
Maybe where we should do this together is where we come together
in places like hospitals, ambulatory care clinics, and home health.
There we come together around staff development and learning is
practice based.
If we really believe that teamwork and cross-disciplinary and spe-
cialty and professional training are critical and important, we ought
to recommend increasing the credit value of learning in a team rela-
Havens
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 191

192
Discussion Highlights
tive to learning in solo or isolation. That would be an incentive that
would make people pay attention.
The American Association of Colleges of Nurses (AACN) and the
American Association of Medical Colleges (AAMC) meet at the same
time of the year, every year, yet they never meet together. AAMC
seems more involved with CME than AACN with CNE. Bringing these
organizations together to think about the continuum of education
could help.
We need to create measures to count what is valued. We are not
counting the right things now. One measurement is how well a
team works together.
The idea of a whole system that links all the health professions
together in a way that directly affects outcome makes sense, but
how do rural primary care practices get linked into a system? Those
have nurse practitioners and pharmacists who are providing care
and they, too, need to be linked into a system somehow.
Health professionals work together so why shouldn’t they learn
together? We need to get state and national accrediting boards to
agree. We need to find ways to give credit for that kind of learning.
Are things changing with respect to teamwork? The composition of
specialty teams seems to be changing. More and more nurses are
PhDs; how will this change teams? Does good teamwork enhance
payment? Perhaps it should.
In the UK, there are inter-, multi- and trans-disciplinary activities.
This is creating a huge research agenda.
The doctor does not have to be captain of the team. In our practice,
the team leader changes. The office nurse is team leader for OSHA
issues. The diabetic nurse leads us for diabetes. Also, we find we
need a good deal of cross training to make teams work.
The ACGME requires evaluations of residents by nurses. Perhaps
that approach should be built into CE.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 192
193
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 193

194
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 194
195
IV.
Reaction from
the Trenches
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 195

196
Reaction from the Trenches
Remarks by Grant S. Fletcher, M.D., M.P.H.
University of Washington School of Medicine
My topic is CME from the trenches. My first thought on hearing
this topic was that I don’t know anything about CME. Having only
recently completed my training, I have never submitted any credit
for CME, so I did a little investigative work and asked a colleague
what he does for CME. He said that, when the time arises, it consists
of going to a website at an academic medical center the night before,
cramming all night, and completing his credits. And that was that.
It sounded scary to me. Through this conference I’ve gotten a better
appreciation of what we’re talking about, and it depends on how
you define CME.
In the context of CME as continued learning, as a recent graduate of
the medical education system, I think about how we keep that fund
of knowledge and expand on it afterwards. For me, this perspective
comes from several sources. Before going to medical school I had
public health training and looked at decision analysis and cost-effec-
tiveness analysis. I felt I had some tools, but not the questions, going
into medicine. I thought a lot about how we acquire knowledge and
then use it. In medical school, I had my antenna up to understand
how it’s done there. I went to nine different institutions during my
medical training. They ranged from community medical centers to
academic health centers, to tertiary private centers and the VA system,
so I saw how I was taught from a lot of different perspectives. After
my medical education, I spent a couple of years as part of a group
that formed a hospitalist program in a community hospital, so I saw
how it was done in the community as well, and then, in more recent
times, I have come back to an academic medical center.
I found a lot of interesting contrasts in these various settings. In my
medical training, one of the interesting things was what we were
taught and what we were not taught so well. I acquired some skills
and knowledge, I saw a great diversity of patients and I think pro-
fessionalism was instilled during that time. However, I think the
actual learning to learn beyond the residency and medical school
suffered greatly. I think, for the most part, we’re not taught much
about the learning process. During medical school, you are inundated
with facts and you have to pare it down, get very quick information,
and move on. What that means, often, is the path of least resistance,
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 196

and that means looking to fellow residents, students, attendings, and
specialists, asking them what they think, and then looking up very
composite references. You’re not doing an idealized sifting through
the evidence and reasoning through multiple sources of evidence. It
is quick and dirty, but that’s the learning habit that I think is instilled
at the time.
When I went to the community hospital after my medical education,
what struck me first of all are the sources of information that people
use. They have their limitations and their advantages, but I don’t
think it is anywhere near the idealized view of strictly evidence
based and thinking through it on your own. And second, I was
struck by the lack of access I had to information. I took access for
granted during my medical education, but suddenly I was having
very limited access. I had an UpToDate subscription, and I kept that
going, but beyond that, I was used to going to various journals to
read more. Access to journals was available in the academic medical
center, but what was available in the community hospital was paltry.
In thinking about ongoing education, access to information always
is important, not just in the formal settings but in self development
as well.
Then, when I went from a community setting back to the academic
setting, it struck me how much easier it is to acquire information
within the academic center. You feel like you’re on an island in the
community center, especially if you’re in a small group. I had this
visceral sense that my knowledge and skills would be decaying and
it would be a struggle to keep those up, whereas with an academic
center, you can take some shortcuts because of the questions that
are raised. If there’s a new set of guidelines and people are talking
about them, you automatically keep abreast of some of the latest
information. You can always go to the guidelines later. Just knowing
that there are developments out there is helpful to begin with. A lot
of our discussion has been around academic medical centers or
large practices, whereas I think it’s much more difficult to access
information in the very large number of small, isolated practices that
we have in this country.
Another area that I like but had very little of in community practice,
was actual feedback on what I was doing. I can recall receiving only
one feedback report in the two and a half years that I was in com-
197
G. Fletcher
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 197

198
munity practice. The report was looking at whether I prescribed the
appropriate antibiotic. They sampled four patients and I had not
given the appropriate antibiotics to one. They didn’t know which
patient this was and there was no connection to the records, so I
had to go through multiple hoops to get the information to learn the
specifics of the case. That was only one report in the entire two and
a half years. If we really want to know how we’re doing, having
some sort of regular formalized feedback would be ideal.
I believe being instilled with professionalism during medical training
is absolutely key. It is my impression that many situations that arise
during practice are far beyond quality measurement. In these situa-
tions, medical education instills an internal professionalism motor
to go to the trouble to find the correct clinical answers. It is very
important to keep that motor running when physicians are out in
practice. We often talk about guidelines but these are very general
approaches for medical conditions that you see again and again.
The reality is, in practice, you see many clinical problems that do
not lend themselves to guidelines and easily measured outcomes.
I’m not sure if there’s an easy way to measure how well a clinician
has developed these habits and has that sense of professionalism.
For example, I was consulting on a neuro-surgery patient who had
an inferior vena cava filter placed for a deep venous thrombosis.
The patient had been bounced around to many teams and had a
very complicated hospital course. I was being consulted for some-
thing else and noticed that this IVC filter had been in for eight
weeks. It was a retrievable filter that was supposed to come out at
six weeks. I called around, but nobody seemed to know whether six
weeks was set in stone, what would happen after the six weeks, or
what were the consequences of keeping the IVC filter in place. That
was well beyond a 30 second info button question. These kinds of
clinical questions arise all the time, so I’m not sure how you would
measure the quality of care in that patient. I could have taken the
easy route, say somebody said just leave it in, and be done with it.
There may be no information about what is the correct thing to do,
but sometimes even discovering that there’s no information is diffi-
cult and time consuming.
I had very little exposure to simulations during my training, but I
Reaction from the Trenches
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 198

think it’s an excellent idea, if done in a realistic fashion. Another
difference between the academic center and the community is that
we’re often sheltered from financial pressures in an academic center.
As a practitioner, that’s very much in the forefront. Trying to take
into account time and cost imperatives, and rewarding clinicians for
doing the right thing is very important.
Remarks by James A. Clever, M.D.
Marin County, CA
First, about the title, “From the Trenches.” That’s a military term. The
only other kind of trench I can think of is when the public works
department is digging up the sewers and the water lines, but I think
it is a military term and that goes along with the rubber hitting the
sky when you’re sending up a recognizance balloon to see what’s
going on. Furthermore, trench warfare is way passé; later on, I will
say more about the military terms that pervade our profession and
some things that need correction.
I’d like to say a bit about motivation as far as continuing education
is concerned because that it is really important. A little story about
motivation: Jerry Reinsdorf, who owns the Chicago Bulls, was having
a conversation with Phil Jackson, who was the coach of the Bulls
during the time that Michael Jordan was playing for them, and they
were the outstanding team in the NBA for several years. They were
talking about motivation of players, and Reinsdorf said that what
motivates people is fear and greed, and Phil Jackson said, “Jerry,
you’ve got it all wrong. It’s pride and love.” I think that all four of
those things actually motivate people. I dislike people being motivated
by greed and fear, but fear is important for professionals to keep
up, fear of being sued, fear of not being re-licensed or re-certified.
If practitioners take on a new project — for instance, a primary care
internist might learn how to shave moles or something like that, and
charge enough for that to be equal to a couple of hours of regular
work — that probably is of some importance. But I think pride and
love are the real things, love of the profession, love of your patient.
You can love your patients but you have to take good care of them
as well. And having some pride that you are practicing well and get
feedback that is good is also an important motivator for continuing
education.
199
Clever
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 199

We haven’t talked about what I see as an increasing lack of collegiality
among professionals. We touched on collegiality in the teamwork
situation between physicians, nurses, pharmacists, students, and
house staff, but the profession of medicine has lost a great deal of
collegiality. Twenty years ago, we had an annual dinner dance and
a lot of staff would come, black tie and nicest gowns, and we had
a great time. We’ve lost that. Now maybe 20 people show up at
quarterly staff meetings; that’s out of an active medical staff that
must be about 600 or 700. For medical grand rounds, it seems like
the majority of the people in the audience are retired physicians,
like myself, and all too few house staff come, in part because morning
report is probably better education and a better use of their time,
but we miss that collegiality. Furthermore, I don’t think there ever
was very good collegiality between physicians, nurses, and other
hospital personnel and that’s something we need to do better.
Now the military aspect, and this comes back to what I think is
detrimental. Doctors write the orders and other people carry out
the orders, just as it’s done in the military, and I think that is wrong.
I don’t know what the medical legal consequences would be if we
changed orders to suggestions, or to advice, but the most effective
way of taking care of the orders situation would be that every time
doctors input the orders into the computer, and maybe even before
those orders are put in, they discuss it with the nurses, in a team
way, to decide what is the best way to do things. Another part of
the military attitude is no fraternization with the enlisted. We shouldn’t
treat the nurses and everyone else as enlisted people; they are our
colleagues.
Remarks by Susan W. Wesmiller, M.S., R.N.
University of Pittsburgh Medical Center
Some interesting things are happening in nursing. When you talk
about who pays for continuing education, in nursing it is mostly the
nurse or the employer. We actually budget for 16 hours a year of
continuing education for every single staff nurse. That doesn’t sound
like a lot, but it’s certainly better than zero. It is something that we’ve
continued, even though we know that we need to pull each staff
nurse off her assignment at least two full days a year to make sure
that, at least, competencies, are maintained. In addition, we pay the
200
Reaction from the Trenches
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 200

entire way for anyone who is speaking at a conference, whether it is
a regional conference or a national conference, so if a nurse shows
professionalism and writes an abstract and has that abstract accepted,
then we support that nurse by paying those expenses. Because we
realized that everybody can’t write an abstract that very first year,
we started a system where staff nurses can write an application, an
essay about why they need continuing education and why they should
go to a conference, and get some help. You talked about conferences
being passé, but a lot of socialization occurs for young staff nurses,
for young professionals to be able to network with their peers
across the country. I’m glad that we’re supporting that.
Is the nursing shortage having an effect on continuing education
and nursing? We’d all like to say no, but the answer is yes. It becomes
increasingly difficult for us to pull nurses off a schedule to send
them anywhere when we are just trying to cover the schedule. It’s
sometimes hard to get them to ACLS or CPR, let alone send them to
a conference. That is something we continue to struggle with. We
don’t have the nursing shortage in Western Pennsylvania that the
coasts have, but you definitely can see changes. We have more nurses
retiring from bedside nursing positions than I have seen before.
We might have six or seven retirement parties a month for nurses
leaving bedside nursing at 65 or 66 years of age.
We heard about team building and about the importance of simula-
tion. We’ve combined those two and have all our code training in
the simulation lab. We have a wonderful simulation lab and we send
nurses, respiratory therapists, pharmacists, and physicians in teams to
do simulation. They are assigned their roles for the team and given
three different scenarios. Then they are videotaped. The debriefing
and the discussion that follows the videotaping are where learning
takes place. But again, it’s hard to get our staff nurses down there,
though we’re working on it.
We also talked about the influence of generations and I don’t think
we should forget that. For the first time in the history of the United
States, we have four generations in the workplace, side by side.
If any of you think that millennials are going to put up with what
worked for baby boomers, think again. They don’t want lectures in
the traditional ways. They want a lecture on their iPod so that they
can listen to it while they’re on the treadmill. Or they want to do
201
Wesmiller
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 201

experiential learning. They are techno savvy. We don’t have to
worry about their technical competence because they come with it.
We just need to make sure that they know how to think critically.
One of my reactions to the discussion about technical competence
versus understanding is that I can see it both ways. Our new nurses
are so techno savvy that they don’t need us to show them how to
use a computer, but our older staff nurses need help, and we need
to help them get to that technical competence.
We have a wonderful nursing grand rounds program that we give
monthly. It’s offered live, but we also Web cast it so that anybody
can catch it 24/7. That is available as continuing education for any-
one, whenever they’re working. We had a 100 percent increase in
the number of people who watched grand rounds when we elimi-
nated paper paychecks and people had to go online to see their
paycheck. If you want to know how much you made, you have to
go online and find your paycheck. All of a sudden, everybody was
on the computer because everybody wanted to know their paycheck,
and while they were there, they saw You Learn and Grand Rounds.
It’s really interesting to see how we drove that change. Unintended
consequences.
We talked about SBAR (Situation/Background/Assessment/Recom-
mendation) training. We are adding to SBAR a line called “I Need
Clarity.” That is going to be our code — nurse to nurse, nurse to
physician, nursing assistant to physician, nursing assistant to nurse
— to say, “Please stop. I don’t understand what you are asking me
to do and I need some help.” We are starting an across the board
education program for everyone, to teach us how to work together,
but we needed that code. We needed something to say to the physi-
cian, “please just stop what you’re doing right now and help me
because I don’t understand this. I need some clarity.” I hope it works.
We’ve done a lot of SBAR training so I think our staff nurses under-
stand those steps, but they needed something more and the physicians
needed to know that when they hear “I need some clarity” that they
should stop what they’re doing.
My final reaction goes back to what we talked about at the begin-
ning of this conference, and that was the idea of a clean slate, of
starting where we would like to end. I thought wouldn’t it be won-
derful if we could waive all the regulatory, mandatory education
202
Reaction from the Trenches
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 202

that takes up so many resources, or if we could demonstrate that
we’re a top tier hospital in outcomes and they could say, “If you are
top tier and you are meeting all of your outcomes, you don’t have to
do regulatory education this year.” Imagine how many more
resources we’d have for providing good patient care.
Remarks by Regina Benjamin, M.D., M.B.A.
Bayou Clinic, Inc., Bayou La Batre, AL
Most of you around the table are from large institutions or represent
large groups. I would submit to you that most practices, and most
physicians, maybe one in two doctors, are more like me than not
like me. I’m in solo practice. I’ve been in solo practice for 18 years,
but I now have a PA. My town has 2,500 people, mostly uninsured,
and the demographics are 60 percent white, 30 percent Asian —
Vietnamese, Cambodian, Laotian — and 10 percent black and other.
I do house calls, and I know my patients and they know me. I go to
their funerals. In fact, recently we were listed on the program, in the
thank you portion. So we get to know each other and it’s a little
different from what I’ve been hearing.
I’ve been asked to react to the conversation over the past two days,
and I think that it’s very fearful. I’m sure I’m speaking for many
other doctors out there. The question I face is how can I improve
my skills and stay current and give the best care that I can to my
patients. And then I ask how can I possibly do all those perform-
ance measures, every measure that you can think of and still have
time to see patients. That’s very scary.
I guess the risk I see is that physicians will start to do things to look
good on paper and not necessarily to take care of patients. I can
make my HEDIS score look great and never do anything to improve
my practice per se. That’s a risk that we have getting ready to re-
certify for boards. Physicians are stressed out, nervous, cramming to
take a test when they’re going to test me again on the Krebs cycle
and how many times I use the Krebs cycle. I need to know what it
was about, but I don’t need to re-certify on it.
People learn in different ways. We still have our quarterly medical
society meetings, and we still have the CME, but it’s more social
203
Benjamin
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 203

now so the topics are not as didactic as they used to be. I learn a lot
in our doctors’ lounge. I don’t know if many people around the
country are still doing that, but our hospital just renovated the
lounge so that we have our breakfast and our lunch there. There’s a
lot of interaction. We talk to other doctors. We consult with the spe-
cialists, and they ask us questions. A lot happens in that breakfast
lounge and during lunch. I’m 30 miles from the hospital, but when I
go there, I try to go around those times when I know the docs will
be there and I can talk to them.
Lectures are important because they tell us what’s new out there.
I can ask myself questions and I can go ask consultants, but I don’t
know what the new things are. I thought about where I learned the
most things that made me actually change things in my practice.
I used to serve on an underwriting committee for a malpractice
insurance company. Every month we’d meet and I’d see how things
would happen there, and I’d come back to my office and make a
change. Those were things like how to follow up on labs or do a
sticker file. That brings me to the idea of service learning, and we
don’t have a way to measure that. Service learning is what we are
starting to teach kids in high school and in college, but we should
be doing it with physicians as well. And if we can measure it, how
can we evaluate it or how can we get credit for it?
I want to tell you a bit about what I would like to have. I need to
tell you about Katrina. Two-and-a-half years ago, Katrina hit our
town; we got 25 feet of water. Out of 2,500 people, 2,000 had no
homes and I lost my clinic. We lost our medical records. We were
able to rebuild and renovate our building and, thanks to the Institute
of Medicine, we were able to get back. We were going to open on the
day after New Years, but on New Year’s Eve, the building burned
down, so we lost all those records again. Needless to say, my staff
said we don’t want to do any more paper records. We need an
electronic record. We got an electronic health record system and
that’s been great. I think the prices will come down, and, as the
costs come down, more people will get it.
I have a program on the computer so I can look up and see right
then the interactions of drugs. That really helps. I’d like to have
UpToDate and things like that integrated in the patient record, so
that when I have a question and I look something up and get the
204
Reaction from the Trenches
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 204

answer, I can document that answer in the record. That documenta-
tion will be there two years from now if I go back to that record, so
I don’t have to go back and look it up again. Those are the kinds of
things I think would help. We don’t have a lot of time in the office,
so anything that would make it more efficient would be better.
The other thing I’d like would be simulation or an interactive game,
a virtual game, where you could do whatever you want. I’d like to
see, for example, what would happen if I give this patient with con-
gestive heart failure a meal with salt in it, or if I changed the diet or
if I didn’t change the diet. Or, if I gave a diabetic a pill but then the
diabetic exercised, what would happen? That’s the kind of game I
think would help me a lot, just being able to play it on my own time.
We talked about CME funding and I think the comments were very
much on point, but I don’t share the level of vilifying the industry
that I heard from some. I don’t feel like I’m a bad person because
I take a drug pen or notepad. The clipboards might have a drug
company’s name. Advertising is advertising, and if you know it is
advertising, you know that’s what it is. I’ve asked patients if it bothers
them to see these things and they’ll tell me they don’t care, that it’s
just advertising. Those notepads and pens save me about $100 a
month in supplies, and for us that’s almost our entire electrical bill.
I can put that money towards treating people who don’t have insur-
ance, versus buying some pens and paper. The other thing is the
drug samples. We didn’t talk about the samples but they serve a
major role. These pharmaceutical companies aren’t taking me out
to $200 dinners because I’m not treating the patients that they want,
but they provide samples and we use them a lot. There’s a prescrip-
tion-in-need program, but it takes 30 days to get those back. You
have to fill out the paper work and then wait. Why do that when
you can have samples? A student run free clinic on the East Coast
had to close because the medical school said no gifts from industry,
so they didn’t get samples anymore.
The idea about the single pool of money sounds good. I do have
one concern, and that’s that it would become like NIH. At NIH, the
large institutions with great grant writers who have the wherewithal
and the means can get the funding, but the small ones can’t. The
individual doctor may not have a role so I’d have to see the details.
205
Benjamin
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 205

206
Reaction from the Trenches
As for the role of the academic health center in CME, I just caution
you that in many parts of the country a town and gown problem
persists. The community and the academic health center don’t
always see eye to eye and it may be a real challenge to get them to
do so. The few practice-based research networks that are around
are working really well, but they’re what we call the early adapters.
It will be a while before we can change some of those other cultures.
DISCUSSION HIGHLIGHTS
Doctors need to get rid of the idea that they are launched into practice
with everything they need to know. They need to see continuing
education as an opportunity to improve the quality of care. How
do we bring evidence that matters to the bedside? How do we stop
doing what doesn’t work and do what does?
Most people think of continuing education as a Holiday Inn
experience, where a bunch of doctors look at a screen, nodding
occasionally, but continuing medical education is truly every bit
of learning from what the patient brings to the office to formal
presentations.
Many physicians look at CME courses as something they have to
do, not something that will provide benefit.
I hear lots of community physicians say they don’t have enough
access to information resources. I think this is a real issue that we
have to confront. Some of these resources can be provided by
medical societies. They can both assess and provide information
resources for their members.
A lot of questions in practice are almost impossible to anticipate,
so I don’t think any one information resource should have a
monopoly. We should make the access as broadly based as possible
for community practitioners.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 206

Conferences serve useful roles beyond CME. I think they help com-
munity physicians in professional development, recharging the
batteries, and networking. They definitely shouldn’t go away.
How many clinicians in practice have mentors? A major way one
learns and is guided is through collegial mentorship. Maybe mentor-
ship ought to be formalized a little more for practicing clinicians
because it is one way we learn an awful lot.
A lot of good things have been happening in journals over the past
decade to help practitioners— publishing systematic reviews and
articles about how to appraise evidence and evaluate diagnostic
testing. But the down side is that more and more is being published,
which is intimidating. It makes it hard to keep up.
If CE requirements just are add-ons to what clinicians are already
doing, it will be very scary. The ideal situation would be that CE and
certification and licensure requirements are tied almost completely
to the electronic medical record, so that the evidence of acquisition
of knowledge and keeping up and quality performance are auto-
matic and just part of the clinician’s work.
In my view, the perfect CE experience for practitioners is broken
down into thirds. One third comes from examining one’s practice
and sitting down with the practice team to say, how are we doing
and what do we need to do differently. One third is point-of-care
learning during the course of patient care. Then, I would reserve a
third for course work. I don’t mean lectures necessarily, but getting
together with peers and colleagues different than my practice team
for the infusion of new ideas and skills. This is where I would get
my collegial fix and connection to professionalism.
The patient’s role in all this is important. We need to figure out some
way to measure communication skills and some way to involve
patients in that.
207
Discussion Highlights
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 207

208
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 208
209
V.
Moving Towards
the Future
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 209

210
i In addition to the Federation of State Medical Boards the participants included:
the Association of American Medical Colleges (AAMC), National Board of Medical
Examiners (NBME), Accreditation Council for Continuing Medical Education (ACCME),
Accreditation Council for Graduate Medical education (ACGME), American Osteopathic
Association (AOA), American Medical Association (AMA), American Board of Internal
Medicine (ABIM), Educational Commission for oreign Medical Graduates (ECFMG),
American Hospital Association(AHA), the American Academy of Family Physicians
(AAFP), Harvard School of Public Health, the Council of Medical Specialty Societies
(CMSS), Blue Cross/Blue Shield Association, Physician Insurers Association of America,
Harvard Medical International, the Milbank Memorial Fund, Robert Wood Johnson
Foundation, five state licensing boards, some certifying boards from the Osteopathic
community, some State Medical Societies, and Columbia Law School. Subsequent
meetings have attracted the participation of the American Association of Retired
People (AARP) and Consumer Union as well.
Continuing Medical Education:
Some Important Odds and Ends
David C. Leach, M.D.
Accreditation Council for Graduate Medical Education
This paper summarizes three important initiatives that have emerged
from the medical profession and will affect continuing medical edu-
cation (CME) in the near future: the National Alliance for Physician
Competence, the Trusted Agent, and the Conjoint Committee on
CME. These three initiatives, each self-organized and still emerging,
have engaged committed people and organizations in conversations
in which they seek to clarify the purpose and principles of CME,
the assessment of physician competence, and the use of technology
in facilitating these goals. Each aims to strengthen the relationship
between the profession and society and each member of the profes-
sion with the whole. This paper focuses on medicine; however, the
need for relevant lifelong learning applies to all health professions.
Perhaps these models from medicine will inform the larger effort.
The National Alliance for Physician Competence
On March 24 and 25, 2005, 45 participants representing 34 organi-
zations met in Fort Worth, Texas to improve medical care in the
United States by supporting consistency in the definition and assess-
ment of physician competence.
i
The first meeting was convened by
the Federation of State Medical Boards (FSMB), but very quickly the
National Alliance became a coalition of organizations with the col-
lective goal of assuring the public of physician competence. At that
first meeting the group reviewed historical trends for the past 100
years, projected likely trends that might characterize the future, and
created several scenarios. For each of the scenarios the group
explored answers to the question: How would/should the healthcare
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 210

community determine and measure physician competence over
the career of a physician for the purpose of assuring the public?
The dialogue was enabled and invigorated through exploration of
alternative futures and their impact on trust, data availability, changing
needs, and other important variables. Together, the group members
created five scenarios.
1
The exercise helped participants envision
the healthcare environment in which physician competence would
be assessed.
A second summit, held in December 2005, produced a draft defini-
tion of physician competence, leading to the document that came
to be known as Good Medical Practice–USA
2
— and a concept of
the organizational model for the National Alliance for Physician
Competence. During a third summit in June 2006, participants
continued to develop the Good Medical Practice–USA document,
created a basic plan for the Alliance, and proposed concepts for a
portfolio tool that physicians could use to provide information about
and to reflect on their competence and performance. A fourth
summit, held in January 2007, refined the document and developed
possible models for assessment of competence. A discovery summit
in August 2007 introduced new models of complex adaptive systems,
the use of positive deviance, and the use of technology to foster
distributed decision making and learning communities. The group
also reviewed various not-for-profit organizational models and out-
lined basic strategies for managing change. Experts joined the group
for these topics.
The mission of the National Alliance for Physician Competence is
to assure the public and the healthcare community that individual
physicians are competent to provide safe medical care of the highest
quality. Through partnership and collaboration, the Alliance will 1)
advocate continuity in the definition, measurement, and determination
of physician competence across the continuum of education, training,
and practice; 2) support seamless collaboration among organizations
that contribute to physicians’ pursuit of lifelong learning and improve-
ment; and 3) seek ways to enable reform of the system of physician
self-regulation so that it is efficient and effective.
3
The Good Medical Practice–USA document
2
organizes physician
competence around the six general competencies: patient care, med-
ical knowledge and skills, practice-based learning and improvement,
211
Leach
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 211

interpersonal and communication skills, professional behavior, and
systems-based practice. It clarifies patients’ expectations for their
doctors and doctors’ expectations of themselves.
The Alliance is self-funding, with each organization responding to
requests for donations as needed. The Alliance’s main product has
been the ability to maintain a dialogue about physician competence.
The conversations have been substantive, civil, and professional.
Participants are held together by common purpose and principles.
The Alliance has also developed a concept paper about a Physician
Learning and Continuous Improvement System (PLACIS). The purpose
of PLACIS is to support lifelong learning, self-assessment, reflection,
and continuous improvement as specified by the principles of the
“Good Medical Practice” document and also to support external
reporting requirements. PLACIS is used to describe a system that
provides a broad range of educational, developmental, and admin-
istrative support. If supplied with appropriate data, PLACIS could
greatly simplify how physicians respond to the increasing demand
for information by various stakeholder groups. Such data could
include scores on standardized examinations, certification status,
hospital privileges, measures of practice performance, results of
self-assessments, and other related data.
The Trusted Agent
While not directly related to CME, the “Trusted Agent” concept, a
brainchild of Bob Galbraith, M.D., co-head of the National Board
of Medical Examiners (NBME) Center for Innovation, may facilitate a
more coherent approach to lifelong learning. The concept describes
a system in which secure data from multiple sources can be tem-
porarily compiled and displayed for such purposes as licensure,
credentialing, and maintenance of certification. The data could,
upon request and with the permission of the physician, be obtained
from multiple sources (“Trusted Agents”), displayed and viewed,
and then, like a sand mandala, all traces are removed. The original
data would continue to reside on the Trusted Agents’ servers.
This concept is now being tested in three states and among three
organizations: the NBME, the FSMB, and the individual state boards.
In the test, a physician applying for licensure in one of the three
states gives permission, and with such permission, data from the
212
Continuing Medical Education: Some Important Odds and Ends
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 212

FSMB’s Federation Credentials Verification Service (FCVS) and from
the NBME are transmitted in a temporary display to the relevant state
for verification of credentials. Verification in the test states (including
assembling relevant documents, such as medical school transcripts,
residency experiences, and board scores) used to take 6 months;
now the process takes 6 minutes from permission to completion.
The concept and the successful pilots have demonstrated the power
of temporary data displays to reduce the burden of and enhance
accountability to regulatory bodies. The ability to accommodate data
about CME remains untested but is a compellingly attractive feature
of the system. Most records of CME now reside on paper in the
individual physician’s files. No national database exists that can link
continuing education with a given physician’s educational and practice
needs. Successful deployment of this system will encourage develop-
ment of such a database, which in turn, will allow individual physicians
to maintain a portfolio of experiences relevant to their needs.
The Accreditation Council for Graduate Medical Education (ACGME)
has developed a “learning portfolio” for residents. The learning port-
folio, which is currently in alpha testing, is an electronic, Web-based
tool that supports resident learning, evaluation, and professional
development. The portfolio is centered around the learner, allowing
residents to chronicle their learning experiences and to seek feed-
back on these experiences. It contains preloaded evaluation tools
that are competency based, and tools can be created easily from a
pool of evaluation items. Residents entering their programs frequently
have had experience with learning portfolios in college or even in
grade school. To date, they have expressed great enthusiasm for the
portfolio as a way to catalog and reflect on their experiences. The
residents are using the system as an interactive tool for ongoing
physician development. It is not yet clear what will happen when
these residents graduate. The data exist and are stored on ACGME
servers. The larger community of organizations would probably
govern the principles and function of physician portfolios after this
test group graduates from residency. In that case ACGME could
become a Trusted Agent and at the request of the physician could
contribute data about the physician’s experiences in residency to
larger data displays or could, alternatively, contribute to the devel-
opment of a learning portfolio for lifelong physician development.
213
Leach
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 213

214
Continuing Medical Education: Some Important Odds and Ends
ii ACCME, ACGME, the Alliance for Continuing Medical Education (ACME), the
American Academy of Family Physicians (AAFP), the American Board of Medical
Specialties (ABMS), the American Hospital Association (AHA), the American Medical
Association (AMA), the American Osteopathic Association (AOA), the Association for
Hospital Medical Education (AHME), the Association of American Medical Colleges
(AAMC), the Council of Medical Specialty Societies (CMSS), the Federation of State
Medical Boards (FSMB), the Joint Commission, the Liaison Committee on Medical
Education (LCME), the National Board of Medical Examiners (NBME), and the
Society for Academic Continuing Medical Education (SACME). The Journal of
Continuing Education in the Health Professions also participates.
The Conjoint Committee on Continuing Medical Education
In October 2002, representatives of 16 major stakeholder organizations
in CME
i
i
began to meet and have since met regularly and voluntarily
to explore and propose changes in the existing system of CME.
4
This
group, the Conjoint Committee on Continuing Medical Education
(CC-CME), drafted a document entitled “Reforming and Repositioning
Continuing Medical Education”.
5
The document describes perceived
inadequacies of the current system of CME, in particular that it has
not consistently accommodated diverse learning styles; applied
advances in educational research; supported practice performance
assessment; and facilitated rapid integration of new knowledge and
skill; and that it has relied excessively on commercial support.
The CC-CME has stated that effective CME for physicians should
1) enhance quality care, 2) support professional activities, 3) assess
professional educational needs, 4) evoke professionalism,
5) motivate learners, and 6) produce measurable outcomes. The
Committee agreed that the six competencies (and a seventh from
the American Osteopathic Association) should serve as the frame-
work for CME.
The CC-CME recommended the following changes: reinforcement
of the continuum of medical education by all relevant organizations;
improved physician self-assessment of the competencies and life-
long learning; development of specialty-specific core curricula for
each specialty and subspecialty; evidence-based valid content for all
patient care recommendations in educational programs; continuous
improvement in the evaluation of CME’s effectiveness; metrics to
measure and recognize physician learning and behavioral change;
and convening a “blue ribbon” panel to propose proper ways of
funding CME. The recommendations were assigned to the relevant
organizations, and the work has begun.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 214

215
Leach
A white paper published in 2007 recommended that each specialty
society and corresponding certifying board reach consensus on
the competencies of the physicians in that specialty using the six
competencies as a framework.
4
A continuum from novice to master
was also proposed.
Summary
These three examples provide evidence that many in organized
medicine are thinking about and engaging in significant efforts to
reform CME. A common vocabulary about physician competence
and its assessment; inclusion of the perspective of patients in the
expectations of competence; the opportunities afforded by technol-
ogy; and further consensus about core expectations by specialty
have all been identified as important needs.
All efforts have developed organizational models to accommodate
the fragmented house of medicine. ACGME has 44 nominating
organizations that select review committee members and participate
actively in graduate medical education. The National Alliance for
Physician Competence attracts between 35 and 45 organizations at its
summits. The Conjoint Committee on Continuing Medical Education
convenes representatives from 16 organizations at each meeting. The
Trusted Agent fully expressed may involve over 70 state licensing
jurisdictions and several more suppliers of data.
5
Dee Hock
6
would call these organizational models chaordic. They
are organized around common purpose and principles rather than
by command and control hierarchical structures. Hock would argue
that this approach may be a more effective way of coping with com-
plex problems. Chaordic models function at the interface of chaos
and order and are designed to enable both fidelity to purpose and
intelligent adaptation to particular microenvironments. The reform
of CME and lifelong learning for physicians is certainly a complex
problem. As specialties and subspecialties adapt to particular needs, a
common language, common assessment expectations, and intelligent
use of technology can foster coherence as well as accountability.
Improving patient care by improving the professional development
of health professionals remains the overriding goal.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 215

216
REFERENCES
1. Physician Accountability for Physician Competence Summit. Accessible at
http://www.innovationlabs.com/summit/summit1/ (Access date: March 2, 2008)
2. Good Medical Practice–USA. Accessible at http://www.gmpusa.org (Access date:
March 2, 2008).
3. Physician Accountability for Physician Competence Summit: Session Overview.
Accessible at http://www.innovationlabs.com/summit/discovery1/r6_mission.html.
(Access date: September 5, 2007).
4. Jackson MJ, Gallis HA, Gilman SC, et al. The need for specialty curricula based on
core competencies: a white paper of the Conjoint Committee on Continuing Medical
Education. J Cont Educ Health Prof. 2007;27:124–128.
5. Reforming and Repositioning Continuing Medical Education. Accessible at
www.jcehp.com/vol25/2503_CMEReport.pdf (Access date: September 23, 2005).
6. Hock D. One from Many. San Francisco: Berrett-Koehler; 2005.
DISCUSSION HIGHLIGHTS
A Set of Principles
When systems need to be changed, it is good to think of the
principles upon which you want to base the new system. Canada
followed that approach when the Canada Health Act was developed.
Five primary principles were chosen. Several principles have come
up in these discussions, but maybe they should be made explicit
and listed.
I like the idea of developing foundational principles. One should be
simplicity. Others are inter-professional CE and evidence-based CE.
Another is practicality.
Some of the principles conference participants have pointed out
include minimizing bias, flexibility, burdens aligned with values,
integrating CE into practice, stressing innovation and evaluation,
addressing needs of practitioners from a broad spectrum — from
specialists in academic health centers to solo rural practitioners —
and aligning CE with quality improvement and health systems
improvements.
An Institute for Continuing Education
There is need for a national public/private entity to explore, consid-
er, evaluate and experiment, to keep the continuing education
agenda on the front burner so it is not scattered among the current
Continuing Medical Education: Some Important Odds and Ends
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 216

groups around the country. The public should support an organization
that would allow us to explore policy and outcomes.
The purpose of a national authority or institute would be to improve
patient care and health outcomes through enhancing professional
knowledge, skills, practices, teamwork and decision-making. It
ought to be independent. It ought to be governed predominantly by
the relevant professions, not as representatives of groups but rather
as individuals coming together to form this body for this purpose. It
should be grounded by the principles we’ve been articulating about
what we want continuing education and life long learning to be in
the professions, including the notion that it would stress innovation
and evaluation as well as the ideas of flexibility and outreach to
accomplish all of the needs from the academic health centers to solo
practitioners in the rural community. It should have, perhaps, a way
of putting some seal of performance or quality on those entities that
met certain standards. It has to obtain its support from government
agencies, foundations, or interested professional groups. If it were
independent and managed by professionals, and had all these attrib-
utes, you could legitimately accept corporate sponsorship in addition
to other sources if it were redirected and merged in a non-specific
way with no one company supporting any one project.
I see the new entity as an exciting way to push forward the science
of continuing education, just as the NIH pushed forward the science
of basic science and clinical medicine. In the long run, continuing
education isn’t going to go far unless we have a better science base.
Over and over again in these discussions, we have pointed out
the lack of information bases and the lack of rigorous studies of
innovations.
I’m looking for an enterprise that will have a capacity to innovate, to
experiment, to evaluate, to disseminate, to bring together the kind
of forward thinking we’ve had here in a regular way that could be
implemented. A national entity that would be a research entity could
explore broader policies and expand the science of education and
quality improvement.
A national entity responsible for continuing education should propose
and promulgate and investigate standards for continuing education.
217
Discussion Highlights
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 217

An Umbrella Organization for Accrediting
Inter-professional CE
We need an accrediting mechanism that incorporates all of the
relevant health professionals so there is an opportunity to reconcile
the differences and commonalities involved in the continuing educa-
tion of healthcare professionals. The ACCME and other accrediting
organizations ought to come together or a task force should be formed
to do this. We need a timeline to create an accrediting mechanism
that represents all the health professionals.
The ANCC and ACPE both have adopted the ACCME’s conflict of
interest requirements this year, so there is movement to align the
accrediting requirements of the three organizations. We should
encourage more rapid progress and movement to an approach that
makes it easier to provide accredited inter-professional CE.
We ought to get the ACCME and other accrediting organizations to
work together, or get a task force to facilitate the discussion, with a
timeline, to create an accrediting mechanism that represents all the
health professionals and that operates with these principles.
The current accrediting process, with ACCME and the ANCC and the
other organizations, can meet the principles and concepts we’ve
outlined, if given a deadline of two years and impetus to make that
change.
We ought to be very specific about a timeline. I’d like to go for a two-
year timeline that people need to meet and come up with something,
and the people who need to meet are the people who see themselves
as currently having responsibility for this. One characteristic of being
a professional is that we are voluntarily self-regulating and we
have established a set of standards by which we accredit and certify
ourselves, and in many cases license ourselves in conjunction with
a public jurisdiction. We need to hold that mechanism accountable,
so there should be a timeline.
218
Discussion Highlights
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 218

219
Conference Conclusions
and Recommendations
After two and a half days of discussion, participants agreed to the
following conclusions and recommendations:
CONCLUSIONS
Continuing Education and the Public
The quality of patient care is profoundly affected by the performance
of individual health professionals.
The fundamental purposes of continuing health professional
education (CE) are:
— To improve the quality of patient care by promoting improved
clinical knowledge, skills, and attitudes, and by enhancing
practitioner performance.
— To assure the continued competency of clinicians and the
effectiveness and safety of patient care.
— To provide accountability to the public.
CE fulfills a critically important, indeed essential, public purpose.
Given the accelerating pace of change in clinical information and
technology, CE has never been more important.
Responsibilities of Individual Professionals, Professional
Teams, and Health Systems
Maintaining professional competence is a core responsibility of
each health professional, regardless of discipline, specialty, or type
of practice.
The individual clinician has been the principal unit of accountability
for performance in the healthcare delivery system. Given that the
performance of health systems also profoundly affects patient care,
CE fails to take into account systems of care.
Effective patient care increasingly depends on well-functioning
teams of healthcare professionals. Therefore, CE must address the
special learning needs of collaborating teams.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 219

Quality improvement efforts and CE activities overlap and ideally
are mutually reinforcing.
CE Methods
Traditional lecture-based CE has proven to be largely ineffective in
changing health professional performance and in improving patient
care. Lecture formats are employed excessively relative to their
demonstrated value.
Professional conferences play an important role in CE by promoting
socialization and collegiality among health professionals. Health
professionals have the responsibility to help one another practice
the best possible care. Meeting together provides opportunities for
cross-disciplinary and cross-generational learning and teaching.
Practice-based learning and improvement is a promising CE
approach for improving the quality of patient care. Maintenance
of certification programs (in which clinicians review the care they
actually deliver in their own practices, compare the results with
standards of excellence, and create a plan for improvement) and
maintenance of licensure programs are moving CE in this direction.
Currently, most CE faculty are insufficiently prepared to teach
practice-based learning.
Information technology is essential for practice-based learning by:
— Providing access to information and answers to questions at the
time and place of clinical decision-making (point-of-care learning).
— Providing a database of clinician performance at the individual
and/or group practice level, which can be compared to best
practices and used to make plans for improvement.
— Providing automated reminder systems.
Interactive scenarios and simulations are promising approaches to
CE, particularly for skills development, whether the skill is a highly
technical procedure, history taking, or a physical examination
technique.
Insufficient research is currently directed at improving and evaluating
CE. There is no national entity dedicated to advancing the science of
220
Conclusions and Recommendations
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 220

CE as there is for biomedical and clinical research.
Financing CE
The majority of financial support for accredited CME, and increas-
ingly for CNE, derives directly or indirectly from commercial entities.
Pharmaceutical and medical device companies and healthcare pro-
fessionals have inherently conflicting interests in CE. Commercial
entities have a legitimate obligation to enhance shareholder value
by promoting sales of their products, whereas healthcare profession-
als have a moral obligation to improve patient/public health without
concern for the sale of products.
Commercial support for CE:
— Risks distorting the educational content and invites bias.
— Raises concerns about the vows of health professionals to place
patient interest uppermost.
— Endangers professional commitment to evidence-based decision
making.
— Validates and reinforces an entitlement mindset among health
professionals that CE should be paid for by others.
— Impedes the adoption of more effective modes of learning.
No amount of strengthening of the “firewall” between commercial
entities and the content and processes of CE can eliminate the
potential for bias.
Academic health centers and other healthcare delivery systems are
not sufficiently attentive, either to their roles in planning, providing,
and assessing CE or to their responsibilities in managing their own
conflicts of interest and those of individual faculty and administrators
when paid by commercial interests for CE teaching.
Accrediting CE
Current accreditation mechanisms for CE are unnecessarily complex
yet insufficiently rigorous. Compared to earlier, formal stages of
221
Conclusions and Recommendations
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 221

health professions education, the CE enterprise is fragmented, poorly
regulated, and uncoordinated; as a result, CE is highly variable in
quality and poorly aligned with efforts to improve quality and
enhance health outcomes.
With the increasing need for inter-professional collaboration,
accrediting bodies of the various health professionals need closer
working relationships.
RECOMMENDATIONS
CE Methods
The CE enterprise should shift as rapidly as possible from excessive
reliance on presentation/lecture-based formats to an emphasis on
practice-based learning.
New metrics are needed:
— To assess the quality of CE. These metrics should be based
on assessment of process improvement and enhanced patient
outcomes.
— To identify high-performing healthcare organizations. The
possibility of awarding CE credit to individual health professionals
who practice in such organizations should be explored.
— To automate credit procedures for point-of-care learning.
Federal and state policymakers should provide financial support
for the further development of information technology tools that
facilitate practice-based learning and should strongly encourage all
clinicians to use these tools.
The responsibility for lifelong learning should be emphasized
throughout the early, formal stages of education in all health
professions. Students should be taught the attitudes and skills to
accomplish CE throughout their professional lifetimes.
A national inter-professional CE Institute should be created to
advance the science of CE. The Institute should:
222
Conclusions and Recommendations
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 222

— Promote the discovery and dissemination of more effective
methods of educating health professionals over their profession-
al lifetimes and foster the most effective and efficient ways to
improve knowledge, skills, attitudes, practice, and teamwork.
— Be independent and composed of individuals from the various
health professions.
— Develop and run a research enterprise that encourages increased
and improved scientific study of CE.
— Promote and fund evaluation of policies and standards for CE.
— Identify gaps in the content and processes of CE activities.
— Develop mechanisms needed to assess and fund research
applications from health professional groups and individuals.
— Stimulate development and evaluation of new approaches to
both intra- and inter-professional CE, and determine how best
to disseminate those found to be effective and efficient.
— Direct attention to the wide diversity and scope of practices
with special CE needs, ranging from highly technical specialties
on the one hand to solo and small group practices in remote
locations, on the other.
— Acquire financial resources to support its work and provide
funding for research. Possible funding sources include the
Federal government, foundations, professional groups, and
corporations.
A concerted effort is needed to make the concept of a Continuing
Education Institute a reality. To achieve this, The Institute of Medicine
should convene a group to bring together interested parties to propose
detailed steps for developing a Continuing Education Institute.
CE Financing
Accredited organizations that provide CE should not accept any
commercial support from pharmaceutical or medical device compa-
nies, whether such support is provided directly or indirectly through
subsidiary agencies. Because many professional organizations and
223
Conclusions and Recommendations
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 223

224
institutions have become heavily dependent on commercial support
for current operations, an abrupt cessation of all such support would
impose unacceptable hardship. A five-year “phase out” period
should be allowed to meet this recommendation.
The financial resources to support CE should derive entirely from
individual health professionals, their employers (including academic
health centers, healthcare organizations, and group practices),
and/or non-commercial sources.
Faculty of academic health centers should not serve on speakers’
bureaus or as paid spokespersons for pharmaceutical or device
manufacturers. They should be prohibited from publishing articles,
reviews, and editorials that have been ghostwritten by industry
employees.
CE Accreditation and Providers
Organizations authorized to provide CE should be limited to profes-
sional schools with programs accredited by national bodies, not-for-
profit professional societies, healthcare organizations accredited by
the Joint Commission, multi-disciplinary practice groups, point-of-care
resources, and print and electronic professional journals.
Existing accrediting organizations for continuing education for
medicine (the Accreditation Council for Continuing Medical
Education) and nursing (the American Nurses Credentialing Center)
should meet and within two years develop a vision and plan for a
single accreditation organization for both nursing and medicine.
The new organization should incorporate the guiding principles for
CE and the recommendations laid out in this report where relevant.
The American Academy of Nursing and the Association of American
Medical Colleges should convene the two accrediting bodies for
this purpose.
Academic health centers should examine their missions to determine
how to strengthen their commitment to CE. They should help their
faculty gain expertise in teaching practice-based learning and incor-
porate information technology, simulations, and interactive
scenarios into their CE activities.
Conclusions and Recommendations
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 224
225
Additional References
Suggested by Conference Participants
General References
Agency for Healthcare Research and Quality. Effectiveness of Continuing Medical
Education (Evidence Report/Technology Assessment; 149). Rockville, MD: US
Department of Health and Human Services; 2007.
Boonyasai RT, Windish DM, Chakraborti C, Feldman LS, Rubin HR, Bass EB.
Effectiveness of teaching quality improvement to clinicians. JAMA. 2007;298:1023–1037.
Center for the Advancement of Interprofessional Education (CAIPE). Interprofesional
education: a definition. CAIPE Bulletin. 1997;13:19.
Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and
research agenda. Acad Med. 2005;80(Suppl):546–553.
Gardner M. Diagnosis using search engines. BMJ. 2006;333:1131.
Golden GA, Parochka JN, Overstreet KM. Medical education and communication compa-
nies: an updated in-depth profile. J Cont Educ Health Prof. 2002;55–62.
Headrick, LA, Wilcox, PM, Batalden, PB. Interprofessional working and continuing med-
ical education. BMJ. 1998; 316:771–774.
Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, Oxman AD. Audit and feedback
versus altermative strategies: effects on professional practice and healthcare outcomes.
Cochrane Database Syst Rev. 2006;2:CD000259.
Johnson J, Dutton S, Briffa A, Black C. Broadband learning for doctors. BMJ.
2006;332:1403–1404.
Manning PR, DeBakey L, editors. Medicine: Preserving the Passion in the 21st Century.
New York: Springer-Verlag; 2004.
McDonald, FS, Zeger SL, Kolars JC. Factors associated with medial knowledge acquisi-
tion during internal medicine residency. J Gen Intern Med. 2007;22:962–968.
O’Brien MA, Freemantle N, Oxman AD, Wolf F, Davis DA, Herrin J. Continuing education
meetings and workshops: effects on professional practice and healthcare outcomes.
Cochrane Database Syst Rev. 2001;1:CD003030.
O’Brien MA, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional
practice and healthcare outcomes. Cochrane Database Syst Rev. 2007;4:CD000409.
Sachdeva AK. Acquiring skills in new procedures and technology: the challenge and
the opportunity. Arch Surg. 2005;140:387–389.
Sachdeva AK. The new paradigm of continuing education in surgery. Arch Surg.
2005;140:264–269.
Sachdeva AK. Surgical education to improve the quality of patient care: The role of
practice-based learning and improvement. J Gastrointest Surg. 2007;11:1379–1383.
Sachdeva AK, Russell TR. Safe introduction of new procedures and emerging technologies
in surgery: Education, credentialing, and privileging. Surg Clin North Am. 2007;87:853–866.
Tang H, Ng JH. Googling for a diagnosis: use of Google as a diagnostic aid: internet
based study. BMJ. 2006; 333:1143–1145.
Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a
collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 225

226
Financing Continuing Education
Abramson J, Starfield B. The effect of conflict of interest on biomedical research and
clinical practice guidelines: Can we trust the evidence in evidence-based medicine?
J Am Board Fam Pract. 2005;18:414–418.
Agrawal S, Saluja I, Kaczorowski J. A prospective before-and-after trial of an educational
intervention about pharmaceutical marketing. Acad Med. 2004;79:1046–1050.
Allman RL. The relationship between physicians and the pharmaceutical industry:
Ethical problems with the every-day conflict of interest. Hospital Ethics Committees
Forum. 2003;15:155–170.
Andersson SJ, Troein M, Lindberg G. General practitioners’ conceptions about treatment
of depression and factors that may influence their practice in this area: a postal survey.
BMC Fam Pract. 2005;16:21.
Antonuccio DO, Danton WG, McClanahan TM. Psychology in the prescription era:
building a firewall between marketing and science. Am Psychol. 2003;58:1028–1043.
Ashar BH, Miller RG, Getz KJ, Powe NR. Prevalence and determinants of physician
participation in conducting pharmaceutical-sponsored clinical trials and lectures. J Gen
Intern Med. 2004;19:1140–1145.
Association of American Medical Colleges. The Scientific Basis of Influence and
Reciprocity: A Symposium. Washington, D.C: Association of American Medical Colleges;
2007. Accessible at www.aamc.org/publications as a pdf download (Access date: April 1,
2008).
Bellande BJ, Fonarow GC, Nishimura RA, Shah PM. Task force 3: Disclosure of relation-
ships with commercial interests: Policy for educational activities and publications.
Circulation. 2004;110:2524–2528.
Bergeron L. Psychological aspects of gifts from drug companies. JAMA.
2003;290:2406–2407.
Berwick DM. Disseminating innovations in healthcare. JAMA. 2003;289:1969–1975.
Bickell NA. Drug companies and continuing medical education. J Gen Intern Med.
1995;10:392–394.
Boyd EA, Cho MK, Bero LA. Financial conflict-of-interest policies in clinical research:
issues for clinical investigators. Acad Med. 2003; 78:769–774.
Brett AS, Burr W, Moloo J. Are gifts from pharmaceutical companies ethically problemat-
ic? A survey of physicians. Arch Intern Med. 2003; 163:2213–2218.
Cain JM. Conflict of interest in healthcare: a subtle but significant issue in women’s
health. Curr Womens Health Rep. 2003; 3:87–88.
Campbell EG. Doctors and drug companies: scrutinizing influential relationships.
N Engl J Med. 2007;357:1796–1797.
Carroll AE, Vreeman RC, Buddenbaum J, Inui TS. To what extent do educational inter-
ventions impact medical trainees’ attitudes and behaviors regarding industry-trainee and
industry-physician relationships? Pediatrics. 2007;120:e1528–e1535.
Chabner BA. CME: The “third phase” of a doctor’s education. Oncologist. 2004;9:241.
Chen P. Paul, Weiss, Rifkind, Wharton & Garrison LLP, New York, NY, USA. Education or
promotion?: Industry-sponsored continuing medical education (CME) as a center for the
core/commercial speech debate. Food Drug Law J. 2003;58:473–509.
Chepesiuk R. Supported by an unrestricted educational grant. Can Med Assoc J.
2003;169:421–422.
Additional References
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 226

227
Cleary JD. Impact of pharmaceutical sales representatives on physician antibiotic
prescribing. Pharm Technol. 1992;8:27–29.
Collins J. Professionalism and physician interactions with industry. J Am Coll Radiol.
2006;3:325–332.
C
osta-Val R. The imminent paradigm shift toward the relationship between pharmaceutical
industry and medicine. Jornal Vascular Brasileiro. 2007;6:104–106.
Coyle SL, Ethics,and Human Rights Committee American College of Physicians-American
Society of Internal Medicine. Physician-industry relations. Part 1. Individual physicians.
Ann Intern Med. 2002; 136:396–402.
Coyle SL. Ethics and Human Rights Committee, American College of Physicians-American
Society of Internal Medicine. Physician-industry relations. Part 2. Organizational issues.
Ann Intern Med. 2002;136:403–406.
Dana J, Loewenstein G. A social science perspective on gifts to physicians from industry.
JAMA. 2003;290:252–255.
Davis DA. CME and the pharmaceutical industry: two worlds, three views, four steps.
CMAJ. 2004;171:149–150.
DelSignore JL. Current guidelines regarding industry-sponsored continuing medical
education. Clin Orthop. 2003;412:21–27
Dietz HP. Don’t regulate—abolish. Med J Aust. 2006;185:673–675.
Donohue JM, Berndt ER, Rosenthal M, Epstein AM, Frank RG. Effects of pharmaceutical
promotion on adherence to the treatment guidelines for depression. Med Care.
2004;42:1176–1185.
Dyer O. Drug company and pharmacy send unsolicited samples of Prozac to Florida
residents. BMJ. 2003 327:950.
Fisher MA. Physicians and the pharmaceutical industry: a dysfunctional relationship.
Perspect Biol Med. 2003;46:254–272.
Fugh-Berman A, Ahari S. Following the script: How drug reps make friends and influence
doctors. PLOS Med. 2007;4:0621–0623.
Goldblum OM, Franzblau MJ. Academic medical centers and conflicts of interest. JAMA.
2006; 295:2845–2846.
Green JA. Pharmaceutical marketing research and the prescribing physician. Ann Intern
Med. 2007;146:742–748.
Gross CP, Gupta AR, Krumholz HM. Disclosure of financial competing interests in ran-
domised controlled trials: cross sectional review. BMJ. 2003;326:526–527.
Halperin EC, Hutchison P, Barrier RC Jr. A population-based study of the prevalence and
influence of gifts to radiation oncologists from pharmaceutical companies and medical
equipment manufacturers. Int J Radiat Oncol Biol Phys. 2004;59:1477–1483.
Hamaty D, Villarreal A, Murphy T. Continuing education or bribe?. Pain Med. 2003;4:295.
Harrison RV. The uncertain future of continuing medical education: commercialism and
shifts in funding. J Contin Educ Health Prof. 2003;23:198–209.
Hemminki E, Karttunen T, Hovi SL, Karro H. The drug industry and medical practice—
the case of menopausal hormone therapy in Estonia. Soc Sci Med. 2004;58:89–97
Henney JE. Safeguarding patient welfare: Who’s in charge? Ann Intern Med. 2006;
145:305–307.
Additional References
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 227

Hensley S. When doctors go to class, industry often foots the bill: lectures tend to
feature pills made by course sponsors; companies deny influence; a purple heartburn
brochure. Wall Street Journal (East Ed) 2002 A12; Dec 4:A1.
Hilliard T, Chambers T. The relationship between paediatricians and commerce.
Paediatr Respir Rev. 2006;7:54–59.
Holmes JS, Shevrin M, Goldman B, Share D. Translating research into practice: are physi-
cians following evidence-based guidelines in the treatment of hypertension? Med Care
Res Rev. 2004; 61:453–473.
Kerridge I, Maguire J, Newby D, et al. Cooperative partnerships or conflict-of-interest?
A national survey of interaction between the pharmaceutical industry and medical
organizations. Intern Med J. 2005; 35:206–210.
Komesaroff PA, Kerridge IH. Ethical issues concerning the relationships between
medical practitioners and the pharmaceutical industry. Med J Aust. 2002;176:118–121
Lexchin J. Interactions between physicians and the pharmaceutical industry: What does
the literature say? CMAJ. 1993;149:1401–1407.
Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and
research outcome and quality: systematic review. BMJ. 2003;326:1167–1170.
Lexchin J, Cassels A. Does the C in CME stand for “Continuing” or “Commercial”?
[comment]. CMAJ. 2005;172:160–162.
Lexchin J, Mintzes B. Transparency in drug regulation: mirage or oasis? CMAJ.
2004;171:1363–1365.
Majumdar SR, McAlister FA, Soumerai SB. Synergy between publication and promotion:
Comparing adoption of new evidence in Canada and the United States. Am J Med.
2005;60:1323–1334.
Marlow B. The future sponsorship of CME in Canada: industry, government, physicians,
or a blend? JAMC. 2004;171:150–151.
McCoy C, Oshman L. Psychological aspects of gifts from drug companies. JAMA.
2003;290:2406–2407.
Mintzes B, Barer ML, Kravitz RL, et al. How does direct-to-consumer advertising (DTCA)
affect prescribing? A survey in primary care environments with and without legal DTCA.
Can Med Assoc J. 2003;169:405–412.
Mizik N, Jacobson R. Are physicians easy marks? Quantifying the effects of detailing and
sampling on new prescriptions. Management Science. 2004;50:1704–1715.
Morgan JM, Marco J, Stock L, Zannad F. Educational governance for the regulation of
industry sponsored continuing medical education in interventional and device based
therapies. Heart. 2005; 91:710–712
Morgan MA, Dana J, Loewenstein G, Zinberg S, Schulkin J. Interactions of doctors with
the pharmaceutical industry. J Med Ethics. 2006;32:559–563.
Moynihan R. Drug company sponsorship of education could be replaced at a fraction
of its cost. BMJ. 2003;326:1163.
Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and
drug companies. 1: Entanglement. BMJ. 2003;326:1189–1192.
Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and
drug companies. 2: Disentanglement. BMJ. 2003;326:1193–1196.
Mueller PS, Hook CC, Litin SC. Physician preferences and attitudes regarding industry
support of CME programs. Am J Med. 2007;120:281–285.
228
Additional References
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 228

Orlowski JP, Wateska L. The effects of pharmaceutical firm enticements on physician
prescribing patterns. There’s no such thing as a free lunch. Chest. 1992;102:270–273.
Prosser H, Almond S, Walley T. Influences on GPs’ decision to prescribe new drugs-the
importance of who says what. Fam Pract. 2003;20:61–68.
R
elman AS. Separating continuing medical education from pharmaceutical marketing.
JAMA. 2001;285:2009–2012.
Relman AS, ACCME. Defending professional independence: ACCME’s proposed new
guidelines for commercial support of CME. JAMA. 2003;289:2418–2420.
Rentmeester CA. Pharma PR or medical education? [comment]. Hastings Cent Rep.
2005;35:6.
Rutledge P, Crookes D, McKinstry B, Maxwell SR. Do doctors rely on pharmaceutical
industry funding to attend conferences and do they perceive that this creates a bias in
their drug selection? Results from a questionnaire survey. Pharmacoepidemiol Drug Saf.
2003;12:663–667.
Schneider JA, Arora V, Kasza K, Harrison RV, Humphrey H. Residents’ perceptions over
time of pharmaceutical industry interactions and gifts and the effect of an education
intervention. Acad Med. 2006;81:595–602.
The scientific basis of influence and reciprocity: a symposium sponsored by the
Association of American Medical Colleges. Washington, DC. June 12, 2007.
Steinman MA, Baron RB, Marlow B. Is continuing medical education a drug promotion
tool? Debates. Can Fam Physician. 2007;53:1650–1653.
Steinman MA, Baron RB. Rebuttal: Is CME a drug-promotion tool?: YES. Can Fam
Physician. 2007;53:1877–1879.
Susman JL. Commercial sponsorship of CME: There are alternatives. J Fam Pract.
2004;53:676–690.
Takhar J, Dixon D, Donahue J, et al. Developing an instrument to measure bias in CME.
J Contin Educ Health Prof. 2007;27:118–123.
Tenery RM Jr. Interactions between physicians and the healthcare technology industry.
JAMA. 2000;283:391–393.
Wall LL, Brown D. The high cost of free lunch. [review] [37 refs]. Obstet Gynecol;
2007;110:169–173.
Waring GO III. On what information do ophthalmologists base their clinical practice?
J Refract Surg. 2004;20:414–416.
Watkins C, Moore L, Harvey I, Carthy P, Robinson E, Brawn R. Characteristics of general
practitioners who frequently see drug industry representatives: national cross sectional
study. BMJ. 2003;326:1178–1179.
Wilson A. Giving and receiving of gifts between pharmaceutical and medical specialists
in Australia. Intern Med J. 2006;36:795–796.
Wilson FS. Continuing medical education: ethical collaboration between sponsor and
industry. Clin Orthop. 2003;412:33–37.
229
Additional References
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 229
230
Biographical Sketches and Statements of Potential
Conflicts of Interest of Conference Participants
Barbara Atkinson, M.D., one of the country’s 13 women medical school deans,
serves simultaneously as Dean of the Medical School and as Executive Vice
Chancellor at the University of Kansas Medical Center. In those roles, she oversees
the Schools of Medicine and Nursing and Allied Health, with more than 2,700 stu-
dents and 780 faculty members, and leads the medical school’s curriculum change
which is designed to ensure that students are learning basic and clinical sciences
from faculty members on the leading edge of advancing medical knowledge. She
reports no potential conflicts of interest related to continuing education in the
health professions.
Denise Basow, M.D., who trained in internal medicine at Johns Hopkins and
practiced in Boston, joined UpToDate as Deputy Editor in 1996. Since then she has
progressed to the position of Executive Editor, where she supervisors the Deputy
Editors, plans new specialties, and provides overall vision for UpToDate. She has
been involved with the CME accreditation process at UpToDate and has experience
with online CME. She reports a potential conflict of interest related to continuing
education in the health professions because UpToDate is a CME provider and she
owns UpToDate stock.
Regina M. Benjamin, M.D., M.B.A., is founder and CEO of the Bayou La Batre
Rural Health Clinic in Bayou La Batre, Alabama. As a former associate dean at the
University of South Alabama College of Medicine, she administered the Alabama-
AHEC program and USA Telemedicine Program. She is a past president of the
American Medical Association Education and Research Foundation and serves as
vice-chair of the AMA Council on Ethical and Judicial Affairs. Other positions
include the Council of Graduate Medical Education and the NIH Committee on
Minority Health and Health Disparities. Dr. Benjamin reports no potential conflicts
of interest related to continuing education in the health professions.
David Blumenthal, M.D., M.P.P., is Director of the Institute for Health Policy at
the Massachusetts General Hospital/Partners HealthCare System, Samuel O. Their
Professor of Medicine and Professor of Healthcare Policy at Harvard Medical
School, and Director of the Harvard University Interfaculty Program for Health
Systems Improvement. His research interests include the dissemination of health
information technology, quality management in healthcare, and the extent and
consequences of academic-industrial relationships in the health sciences. He
reports no potential conflict of interest related to continuing education in the health
professions.
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 230

James A. Clever, M.D., retired in 2005 after 35 years in private practice in general
internal medicine in San Francisco. He was elected to a four-year term on the Marin
Healthcare District Board of Directors in 2006. His CME continues to include one
national and several regional meetings each year, attending 35 to 40 grand rounds,
and reading some 200 journal publications. He reports no potential conflicts of
interest related to continuing education in the health professions.
Jordan J. Cohen, M.D., currently Professor of Medicine and Public Health at
George Washington University, is President Emeritus of the Association of American
Medical Colleges. During his tenure at AAMC, Dr. Cohen led Association efforts
to strengthen its programs for medical students, residents, and constituents and its
data gathering, communications, and advocacy capabilities. He also introduced
initiatives to improve medical education, research, and patient care. Dr. Cohen
reports no potential conflicts of interest related to continuing education in the
health professions.
Ellen M. Cosgrove, M.D., is Senior Associate Dean for Education and is responsible
for undergraduate, graduate, and continuing medical education at the University of
New Mexico School of Medicine, where she is also a professor of internal medicine.
Both the Accreditation Council for Continuing Medical Education and the Alliance
for CME, where she has held leadership positions, have honored Dr. Cosgrove
for her long-time commitment and service to continuing medical education. She
reports a potential conflict of interest related to continuing education in the health
professions because UNM is an accredited CME provider.
Linda Cronenwett, Ph.D., R.N., is Dean and Professor of the School of Nursing at
the University of North Carolina at Chapel Hill as well as the Associate Chief
Nursing Officer for Academic Affairs at the University of North Carolina Hospitals.
Her other commitments include: principal investigator for a national initiative on
Quality and Safety Education for Nurses funded by the Robert Wood Johnson
Foundation; the board of directors of the Institute for Healthcare Improvement, and
national advisory committee for Robert Wood Johnson’s Transforming Care at the
Bedside initiative. Dr. Cronenwett reports a potential conflict of interest related to
continuing education in the health professions because UNC is an accredited
CE provider.
David A. Davis, Jr., M.D., is Vice President for Continuing Healthcare Education
and Improvement at the American Association of Medical Colleges and founding
director of the University of Toronto’s Knowledge Translation Program at St.
Michael’s Hospital in Toronto. As the author of numerous articles and editor of two
major books on CME, Dr. Davis is widely recognized for his contributions to the
231
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 231

field. These include the application of problem-based learning principles, the use of
innovative needs assessment and evaluation techniques, the use of standardized
patients, and a systematic, outcomes-based focus on CME. He reports potential
conflicts of interest related to continuing education in the health professions
because of funding by Merck Canada and occasional speaking and consultancy to
medical schools, commercial interests, and specialty societies, with all funds trans-
ferred to the CME research fund at the University of Toronto.
Catherine D. DeAngelis, M.D., M.P.H., is Editor-in-Chief of Scientific Publications
and Multimedia Applications, and oversees the Journal of the American Medical
Association (JAMA) as well as nine Archives publications. She is also Professor of
Pediatrics at Johns Hopkins University School of Medicine. She is author and editor
of 11 books on pediatrics and medical education and has published more than 200
original articles, chapters, editorials, and abstracts in those fields. Recent works
have focused on women in medicine, conflicts of interest in medicine, and on med-
ical education. Dr. DeAngelis reports no conflicts of interest related to continuing
education in the health professions.
Lyn (Lynore) DeSilets, Ed.D., R.N.-B.C., is Assistant Dean of the Villanova
University College of Nursing, where she has served as Director of Continuing
Education in Nursing and Healthcare for 28 years. The program is a nationally
accredited provider of CNE by the American Nurses Credentialing Center
Commission on Accreditation. She also serves as an appraiser for ANCC’s
Commission on Accreditation, is a member of the Continuing Education Review
Panel for the Pennsylvania State Nurses Association, and is an associate editor
for the Journal of Continuing Education in Nursing. Dr. DeSilets reports potential
conflicts of interest related to consultancies for the American Public Health
Association, the ANCC, and the Pennsylvania State Nurses Association.
F. Daniel Duffy, M.D., is Senior Advisor to the President of the ABIM and Adjunct
Professor of Medicine and director of the community health track at the University
of Oklahoma College of Medicine-Tulsa, where he heads a program to integrate
a safety-net primary care system in the region. At the American Board of Internal
Medicine, he introduced a new maintenance of certification process based on
evaluation of practice performance. He is a member of the Ambulatory Measures
Steering Committee of the National Quality Forum, the Performance Measurement
Committee of the National Committee for Quality Assurance, and the Board of
Directors of the American Board of Medical Specialties. Dr. Duffy reports potential
conflicts of interest related to continuing education in the health professions relat-
ing to his work with ABIM.
232
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 232

233
Harvey V. Fineberg, M.D., Ph.D., is currently President of the Institute of Medicine,
a position he assumed in 2001 after serving as Provost of Harvard University from
1997 to 2001 and, for the previous 13 years, as Dean of the Harvard School of
Public Health. His academic career focused mainly on the fields of health policy
and medical decision making. At IOM, he has chaired and served on a variety of
panels dealing with health policy issues, ranging from AIDS to vaccine safety. Dr.
Fineberg reports no potential conflicts of interest related to continuing education
in the health professions.
Grant S. Fletcher, M.D., M.P.H., is an attending physician in the Consultation and
Hospitalist Medicine Program at the University of Washington’s Harborview Medical
Center in Seattle. He completed his masters in public health at the University of
North Carolina-Chapel Hill and helped to start the hospitalist program at a Salt
Lake City hospital. His research interests include developing and assessing clinical
decision support tools with the electronic medical record, and clinical research on
hospital care. Dr, Fletcher reports no potential conflicts of interest related to contin-
uing education in the health professions.
Suzanne W. Fletcher, M.D., M.Sc., is Professor Emerita of Ambulatory Care and
Prevention at Harvard Medical School, Adjunct Professor of Epidemiology at the
University of North Carolina School of Public Health, and Adjunct Professor at the
UNC School of Medicine. At Harvard, Dr. Fletcher served as director of the CME
course for primary care clinicians given at PRI-MED. The course was held each
year in five cities, with total attendance of more than 200,000. She also serves as
co-editor of primary care for the electronic text, UpToDate, on the International
Advisory Board for The Lancet, and as associate editor of the Journal of the
National Cancer Institute. She was founding co-editor of the Journal of General
Internal Medicine, has served as co-editor of the Annals of Internal Medicine
and, in 1995, organized the conference that led to the formation of the World
Association of Medical Editors. She chaired the committee that developed the
first MOC module at the American Board of Internal Medicine. Dr. Fletcher
reports potential conflicts of interest related to continuing education in the health
professions because Harvard Medical School and Harvard Pilgrim Healthcare are
accredited CME providers, and because of honoraria from the American Board of
Internal Medicine, Susan G. Komen Foundation, Research Triangle International,
Josiah Macy, Jr. Foundation, The Lancet, and several medical schools for visiting
professorships. She receives royalties from Lippincott Williams & Wilkens, Wolters
Kluwer, and UpToDate.
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 233

234
Melvin I. Freeman, M.D., is Emeritus Director of Continuing Medical Education
at the Virginia Mason Medical Center in Seattle, where he currently is a research
scientist in ophthalmology. Previously in private group practice, he was head of
ophthalmology at Virginia Mason Clinic and Medical Center and is Emeritus Clinical
Professor of Ophthalmology at the University of Washington School of Medicine.
He is Vice Chair of the Washington State Medical Association’s Continuing Medical
Education Committee, a surveyor for the Accreditation Council for Continuing
Medical Education, and for the American College of Surgeons Program for
Accreditation of Educational Institutes and past president of the Alliance for
Continuing Medical Education. Dr. Freeman reports potential conflicts of interest
relating to continuing education in the health professions due to honoraria from
ACCME and the American College of Surgeons, and royalties from Elsevier/Mosby
Publishers and Slack, Inc.
Michael Green, M.D., M.Sc., is Associate Professor of Medicine and Associate
Director of the Primary Care Residency Program at Yale University School of
Medicine. His interests include curriculum development, evaluation of clinical
competence, evidence-based practice, and lifelong self-directed learning in
medicine. He has developed an Internet-based “Point of Care Clinical Question”
module and is collaborating on research with ABIM to define the characteristics
of physicians’ information needs and information seeking behavior, and the
association of self-directed learning with self-directed learning “readiness” evaluation
instruments. Dr. Green reports potential conflicts of interest related to continuing
education in the health professions because of his employment, and his funding as
a Kimball Scholar at the American Board of Internal Medicine.
Carol Havens, M.D., is Director of Clinical Education for Northern California
Kaiser-Permanente and a practicing physician in addiction medicine. At Kaiser-
Permanente, she has been involved in CME for 22 years and has served as regional
director of clinical education for the past 14 years. She is chair of the California
Medical Association CME Committee, a member of the Accreditation Review
Committee for the ACCME, and a member of the CME committees for the
Permanente Federation and Audio-Digest. She has been involved in a variety
of educational interventions, including live programs, video conferences, and
academic detailing training and evaluation. Dr. Havens reports potential conflicts
of interest related to continuing education in the health professions due to
employment with the Permanente Medical Group, honoraria from the California
Academy of Family Physicians and CMA’s Institution for Medical Quality, and
royalties from Wolters-Kluwer.
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 234

235
Paul C. Hébert, M.D., M.H.Sc., is Editor-in Chief of the Canadian Medical
Association Journal, a critical care physician at The Ottawa Hospital, and clinical
researcher at the Ottawa Health Research Institute. He is also professor in the
department of medicine with cross appointments in the departments of anesthesiol-
ogy, surgery, epidemiology, and community medicine. Dr. Hébert’s research has
focused on transfusion practice, including alternatives to transfusion, blood conser-
vation, and resuscitation fluids. His groundbreaking trial on critical care transfusion
requirements, published in the New England Journal of Medicine, changed the way
clinicians throughout the world approach transfusion. Dr. Hébert reports no poten-
tial conflict of interest related to continuing education in the health professions.
Maryjoan D. Ladden, Ph.D., R.N., Assistant Professor in Ambulatory Care and
Prevention at the Harvard Medical School, is a pioneer in developing inter-profes-
sional education and practice models to improve the quality and safety of healthcare,
and to enhance collaboration between nurses and physicians. She is a course
director of Current Clinical Issues in Primary Care, PRI-MED, which is the largest
inter-professional primary care continuing education program in the world. Dr.
Ladden reports potential conflicts of interest related to continuing education in the
health professions due to her work with MJ Ladden & Associates, a consulting firm,
honoraria as co-director for Current Clinical Issues in Primary Care and the National
Medical Advisory Board Take Care Health System, and royalties from UpToDate.
David C. Leach, M.D., Immediate Past Executive Director of the Accreditation
Council for Graduate Medical Education, has focused on how physicians acquire
competence and become practitioners of the art, science, and craft of medicine.
Grants from the Robert Wood Johnson Foundation and the Pew Charitable Trusts
supported his work to develop innovative curricula for both medical students and
residents. His current interests include the teaching of improvement skills, aligning
accreditation with emerging healthcare practices, and the use of educational out-
come measures as an accreditation tool. Dr. Leach reports no potential conflicts of
interest related to continuing education in the health professions.
Donald A.B. Lindberg, M.D., has been director of the National Library of Medicine,
the world’s largest biomedical library, since 1984. Prior to his NLM appointment,
he was Professor of Information Science and Professor of Pathology at the University
of Missouri-Columbia. His work has enhanced the role of information and computer
technology in medical diagnosis, artificial intelligence, and education programs.
He was the first President of the American Medical Informatics Association and serves
on numerous boards, including the Computer Science and Engineering Board of
the National Academy of Sciences, the National Board of Medical Examiners, and
the Council of the Institute of Medicine. He has written three books on the use of
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 235

computers and medical information systems and more than 200 articles and reports.
Dr. Lindberg reports no potential conflicts of interest related to continuing educa-
tion in the health professions.
Phil R. Manning, M.D., Paul Ingalls Hoagland Hastings Professor of Continuing
Medical Education and Professor of Medicine Emeritus at the Keck School of
Medicine, University of Southern California, is founding president of the Society
of Medical College Directors for Continuing Medical Education. He has been a
governor, regent, and vice president of the American College of Physicians and
serves on several educational committees of the American College of Cardiology.
He is also co-editor of Medicine: Preserving the Passion in the 21st Century and
author of 46 peer-reviewed publications. Dr. Manning reports potential conflicts
of interest related to continuing education in the health professions because of
honoraria from the National Library of Medicine.
Paul Mazmanian, Ph.D., serves as Associate Dean for Continuing Professional
Development and Evaluation Studies at the Virginia Commonwealth University
School of Medicine, where he is also a professor in the Department of Family
Medicine with a joint faculty appointment in the Department of Epidemiology and
Community Health. His research interests include learning and change in physician
performance. For the past eight years, he has been Editor of the Journal of
Continuing Education in the Health Professions and also has served on study
sections or as a consultant to the Agency for Healthcare Research and Quality,
the National Cancer Institute, The National Heart, Lung, and Blood Institute, and
the Institute of Medicine. Dr. Mazmanian reports no potential conflicts of interest
related to continuing education in the health professions.
Pamela H. Mitchell, Ph.D., M.S., holds numerous positions at the University of
Washington, where she is Associate Dean for Research, Professor of Biobehavioral
Nursing and Health Systems, and the Elizabeth S. Soule Distinguished Professor
of Health Promotion at the School of Nursing, and is Adjunct Professor of Health
Services at the School of Public Health and Community Medicine. She also is
founding director of the Center for Health Sciences Inter-professional Education
and Research, past chair of the American Academy of Nursing’s expert panel on
quality care, and president-elect of the American Academy of Nursing. Dr. Mitchell
reports potential conflicts of interest related to continuing education in the health
professions because of her employment (a self-supporting unit of the School of
Nursing that provides CNE) and honoraria for numerous speaking engagements
for non-commercial conferences and symposia that provide CE credit, including
the Washington State University Research Symposium, Washington State Nurses’
Association, and the Association for Prevention Teaching and Research.
236
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 236

Donald E. Moore, Jr., Ph.D., directs the Division of Continuing Medical Education
at the Vanderbilt University School of Medicine, where he is also Professor of
Medical Education and Administration. For more than 25 years, Dr. Moore has held
positions in medical schools, hospitals, and the government, where he helped to
develop and coordinate continuing medical education for physicians and hospital
staff, worked on faculty development, managed an educational technology center,
and established a diabetes care education and research program. His research
interests include practice-based CME, evidence-based medicine, the role of CME
in physician change, and the impact of CME on healthcare outcomes. Dr. Moore
reports potential conflicts of interest related to continuing education in the health
professions due to his employment, research funding from Wyeth Pharmaceuticals,
and consultancies with Wyeth, Rockpointe Communications, The Chatham Institute,
Fortis-Spectrum Communications, the Pennsylvania Consortium for Academic
CME, and Yale University School of Medicine.
June E. Osborn, M.D., served as the President of the Josiah Macy, Jr. Foundation
from 1996 until she retired at the end of 2007. Trained in pediatrics as well as
virology and infectious diseases, she previously served as Associate Dean of the
Graduate School for Biological Sciences at the University of Wisconsin-Madison
and as Dean of the School of Public Health at the University of Michigan. She has
served in many advisory roles for federal health agencies, private foundations, and
the World Health Organization, particularly on issues relating to virology, vaccines,
infectious diseases, and public health. She chaired the National Commission on
AIDS from 1989-1993 and was a member of WHO’s Global Commission on AIDS.
Dr. Osborn reports no potential conflicts of interest related to continuing education
in the health professions.
Ajit K. Sachdeva, M.D., established and directs the division of education at the
American College of Surgeons, where he oversees the development and implemen-
tation of innovative educational programs for surgeons, surgical residents, and
medical students. His initiatives include core competencies in surgery, enhanced
safety for surgical patients, expanding the repertoire of experiential learning pro-
grams, distant education, the use of simulations and simulators in surgery, and
evaluation of educational outcomes. He is widely recognized for his contributions
to the field of continuing medical education. Dr. Sachdeva reports no potential
conflicts of interest related to continuing education in the health professions.
Marla E. Salmon, Sc.D., R.N., is Dean of the Nell Hodgson Woodruff School of
Nursing at Emory University, where she is also professor of both nursing and public
health. Her interests are in national and international health policy, administration,
public health, and workforce development. Dr. Salmon has held senior leadership
237
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 237

roles in professional and national government service. Her many positions
include membership on the Nursing Advisory Council of the Joint Commission on
Accreditation of Healthcare Organizations, the Board of Directors for the National
Council on Healthcare Leadership, and the Board of Trustees of the Robert Wood
Johnson Foundation. Dr. Salmon reports no potential conflicts of interest related to
continuing education in the health professions.
David C. Slawson, M.D., is the B. Lewis Barnett, Jr. Professor of Family Medicine
and Vice Chair for Academic Affairs for the Department of Family Medicine at
the University of Virginia Health System. He also is founder and director of the
Center for Information Science and holds a joint appointment as Professor in
the Department of Public Health Sciences. He directs the Faculty Development
Program for the Family Medicine Department and is a member of the editorial
board of the American Family Physician. Dr. Slawson reports potential conflicts
of interest related to continuing education in the health professions due to his
employment, consultancies with J. Wiley & Sons, honoraria from Tufts University,
and stock ownership/options with InfoPOEM, Inc.
Robert Steinbrook, M.D., is a national correspondent for the New England
Journal of Medicine and an Adjunct Professor of Medicine at Dartmouth Medical
School. He served as deputy editor of the New England Journal of Medicine from
1993 to 2001 and before that was a medical writer for the Los Angeles Times.
Dr. Steinbrook is a graduate of Amherst College and the University of Pennsylvania
School of Medicine and trained in internal medicine at the University of California,
San Francisco. Dr. Steinbrook reports no potential conflicts of interest related to
continuing education in the health professions.
William M. Tierney, M.D., is Chancellor’s Professor in the Indiana University
School of Medicine’s Department of Medicine. He also is a senior investigator in
the Regenstrief Institute, where he serves as Executive Director of the Regenstrief
Center for Healthcare Improvements and Research. His research interests include
the effects of innovative, computer-based interventions to improve healthcare
quality and lower costs and a major HIV/AIDS research program in collaboration
with Moi University in Kenya. He also directs ResNet, a PBRN within IU. Dr. Tierney
reports potential conflicts of interest related to continuing education in the health
professions because he serves as unpaid co-editor in chief of the Journal of General
Internal Medicine, which has a continuing medical education mission.
Thomas R. Viggiano, M.D., M.Ed., is Associate Dean for Faculty Affairs and
Barbara Woodward Lips Professor at the Mayo Medical School. He specializes in
curriculum integration and evaluation, and designed an innovative system for cur-
238
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 238

riculum evaluation based on quality improvement principles. Among other posi-
tions, he chairs the AAMC Group on Faculty Affairs, where he has helped develop
collaborative research projects involving AAMC’s Council of Teaching Hospitals.
Dr. Viggiano reports no potential conflicts of interest related to continuing education
in the health professions.
Susan W. Wesmiller, M.S., R.N., is Director of Nursing Education and Research
at the University of Pittsburgh Medical Center, where she also is a doctoral student
and adjunct faculty member at the School of Nursing. Recent presentations include
the use of technology in nursing education and the research process for nurse
educators. Her recent research involves communication strategies to improve co-
worker relationships and using a learning management system in a computerized
education program in a transplant intensive care unit. She reports no potential
conflicts of interest related to continuing education in the health professions.
Michael S. Wilkes, M.D., Ph.D., is Professor of Medicine and Director of Global
Health Programs at the University of California, Davis, School of Medicine. With
NIH funding, he has developed Web-based CME tools on topics such as ethics,
communications, clinical genetics, epidemiology, and end-of-life care. Other
research interests involve medical education and physician behavior change,
particularly around physician prescribing behavior. Dr. Wilkes also is an award
winning journalist and a long-standing medical commentator for National Public
Radio. Dr. Wilkes reports potential conflicts of interest related to continuing
education in the health professions because the University of California is a CME
provider and he holds an NIH grant to develop CME.
Patricia S. Yoder-Wise, R.N., Ed.D., is Editor-in-Chief of the Journal of
Continuing Education in Nursing: Continuing Competence for the Future. As a
professor of nursing at Texas Tech University Health Sciences Center-Lubbock, she
teaches in the graduate nursing administration program. She also teaches policy
and politics at Texas Woman’s University-Houston. As President of the American
Nurses Credentialing Center from 2005-2007, she was involved in numerous
discussions about certification, Magnet and continuing education accreditation,
and will serve as guest editor for both Nursing Administration Quarterly and Nurse
Leader. Dr. Yoder-Wise reports potential conflicts of interest related to continuing
education in the health professions due to honoraria from the Journal of Continuing
Education in Nursing, the ANCC, and Glaxo-Wellcome, and for speaking at several
continuing education events, and royalties received from Elsevier, Jones and Bartlett
and Nursing Administration Quarterly.
239
Biographies
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 239
240
Editors: Mary Hager, Sue Russell, and Suzanne W. Fletcher, M.D., M.Sc.
Design & production: David Klaboe, Klaboe Design, NYC
Conference photos: Ernest McCreight, Bermuda
Cover photos in montage from Corbis, Getty Images, Masterfile, and iPhoto
Printed in USA by Cinnamon Graphics, Inc., New York
CEHP 5-9 with final edits (forhiresPDF):050306 NeuroMngrph11/17/05AA 5/9/08 5:37 PM Page 240

Continuing Education in
the Health Professions
Proceedings of a Conference
Chaired by Suzanne W. Fletcher, M.D., M.Sc.
Edited by Mary Hager, Sue Russell,
and Suzanne W. Fletcher
, M.D., M.Sc.
Continui ng Educ ation in the Health Profess ions
Fl etcher
The Josiah Macy, Jr. Foundation is a private philanthropy dedicated to improving
the health of individuals and the public. Since its establishment in 1930, the
Foundation has focused its support principally on projects and conferences
designed to enhance the education of health professionals, especially physicians.
ISBN 0-914362-49-6
