
Page 1 of 73
Mid Essex Clinical
Commissioning Group
Annual Report:
April 2022 – June 2022
Page 2 of 72
Contents
Chair’s Foreword ........................................................................................................ 4
PERFORMANCE REPORT ....................................................................................... 5
Accountable Officer’s Introduction .............................................................................. 5
What Mid Essex CCG does ....................................................................................... 6
Mid and South Essex Health and Care Partnership ................................................... 8
Local Achievements ................................................................................................. 10
How we have performed .......................................................................................... 10
Key issues and risk .................................................................................................. 13
Performance analysis ............................................................................................... 14
Introduction .............................................................................................................. 14
Performance summary ............................................................................................. 14
Improve Quality ........................................................................................................ 18
Reducing Health Inequality ...................................................................................... 20
Engaging People and Communities ......................................................................... 20
Health and Wellbeing Strategy ................................................................................. 24
Financial Review ...................................................................................................... 24
Risks ........................................................................................................................ 24
Sustainable Development ........................................................................................ 28
ACCOUNTABILITY REPORT .................................................................................. 31
Corporate Governance Report ................................................................................. 31
Members Report ...................................................................................................... 31
Governance Statement ............................................................................................ 37
REMUNERATION AND STAFF REPORT ............................................................... 54
Page 3 of 72
Remuneration Report ............................................................................................... 54
Staff Report .............................................................................................................. 64
PARLIAMENTARY ACCOUNTABILITY AND AUDIT REPORT ............................... 71
ANNUAL ACCOUNTS .............................................................................................. 72

Accountable Officer’s Foreword
This annual report covers the period between 1 April 2022 and 30 June 2022. It will be
our last report as a Clinical Commissioning Group, with our move to being an Integrated
Care System.
During this time period, we have continued to widen collaboration with our local
authorities, service providers and voluntary organisations so we are all working together
for better lives. I’m hugely proud of all my NHS colleagues – health and care
professionals and non-clinical staff alike – for the efforts they continue to make for local
residents.
We do recognise that many people have had challenges accessing healthcare in recent
months. The “digital first” approach that NHS England and NHS Improvement asked all
CCGs to follow has made accessing services easier for some people, but many people
have also found such significant and rapid change a challenge. The CCG has continued
to listen to our communities and work with them to develop models of care that meet
everyone’s needs. This work will carry on as we begin the next chapter as an
Integrated Care System.
As we move into the new financial year, a robust plan is also being developed within
national guidelines to significantly reduce the number people waiting for operations and
treatments. Momentum on this programme will build as we move into our new
partnership for local working.
Finally, I was to pass on my heartfelt thanks to our local workforce without whom none
of this would be possible. I look forward to pushing forward together as an alliance with
our local authority, trusts, community providers and wider community and voluntary
sector.
Anthony McKeever
Accountable Officer
26 June 2023
Page 4 of 72
PERFORMANCE REPORT
Performance Overview
The purpose of the performance report is to provide information on the CCG’s
objectives for the 2022/23 financial year, the principal risks to their achievement and
how the CCG performed against these objectives. This section provides a precis of the
rest of the annual report and accounts.
Accountable Officer’s Introduction
Across the mid and south Essex system all services continue to be under extreme
pressure with demand higher than capacity. We need to work with our partners to
ensure that services are able to safely support our residents with long term conditions
and respond to their health needs in a timely manner. Across acute, community and
mental health partners the increase in the acuity of people presenting to their services
is impacting on length of stay and the ability to meet demand and release
capacity. Work continues with wider System partners including local authority and
voluntary sector who work collaboratively to enable discharge and care out of hospital
enabling people to return to their usual place of residence with the right package of
care.
Public services depend on trust. Every time the question of trusted professionals is
raised, doctors and nurses are near the top of the list. This shows the mutual
confidence our residents and healthcare professionals have in one another and is
evident across the public services we all rely upon. During difficult times collaboration
and confidence helps us work effectively and support one another.
Our transition to an “integrated care system” (ICS) on 1
st
July 2022 – will promote
confidence and enhance collaborative working. Over the first quarter of 2022/23 we
have been preparing the new ICS to build on the legacy of the five clinical
commissioning groups to show that people’s best interests and improved health
outcomes are at the heart of everything we do. Now and in the future. This document
reflects the seriousness with which we take our responsibilities as part of an ICS.
Anthony McKeever
Accountable Officer
26 June 2023
Page 5 of 72
What Mid Essex CCG does
Our Purpose
NHS Mid Essex CCG is a clinically led organisation, established on 1 April 2013, that
decides how to spend the NHS budget on the majority of health services for people
living in the mid Essex area.
This includes the care and treatment you receive in hospital, maternity services,
community, and mental health services. The CCG also assumes full responsibility for
commissioning of GP services (since 1 April 2021).
Our role is to specify outcomes that we want to achieve for our population, and then
contract with Providers to provide care to achieve those outcomes. We’re committed to
ensuring the provision of local, high-quality services that meet the specific needs of our
population.
We’ve a statutory obligation to achieve our financial targets and ensure that we live
within our means, whilst assuring all centrally set performance targets are met.
Established under the Health and Social Care Act 2012 as a statutory body, every GP
from the mid Essex GP practices is a member of NHS Mid Essex CCG. As a CCG, we
work hard to understand the needs of people living in mid Essex to commission the
right services for the those that live there.
To do this, the vast majority of decisions about how we use public money is made by
local clinicians who are closest to the people they look after. We work in partnership
with health and social care partners (e.g., local hospitals, local authorities, the
community, and voluntary sector). Our governing body is made up of 4 representatives
of general practice (GPs) from across mid Essex along with a Joint Accountable Officer,
Joint Chief Finance Officer, Executive Director of Nursing, NHS Alliance Director,
secondary care (hospital) specialist and three Lay Members that are part of a joint
management team across mid and south Essex.
The key providers from which the CCG buys health services for the residents of mid
Essex are:
• Mid and South Essex NHS Foundation Trust (MSEFT) is the main provider of
acute hospital services from its sites at Basildon, Southend, and Broomfield.
• Essex Partnership University NHS Foundation Trust (EPUT) is the main provider
of mental health services.
• Provide Community Interest Company are our main providers of community
services.
• Emergency health services and transport are provided by the East of England
Ambulance Service NHS Trust and urgent care services by IC24.
In addition, the CCG has a range of contracts with other providers of services such as
palliative care and end of life services, specialist health services for fertility and
termination of pregnancy and community elective care services. We also buy services
from a number of Independent Sector providers.
Page 6 of 72

Page 7 of 72
GP Practices within our CCG have formed 39 Primary Care Networks (PCNs) to
develop local primary care services to meet the needs of our residents.
A formal document, called a constitution, sets out the arrangements the CCG has made
to ensure it meets its responsibilities for commissioning high quality services for the
people of mid Essex.
It describes the governing principles, rules and procedures which will ensure integrity,
honesty, and accountability. Also, it commits the CCG to taking decisions in an open
and transparent way and places the interests of patients and public at its heart. We last
refreshed our constitution in March 2021 to reflect joint working arrangements with the
mid and south Essex CCGs.
Our constitution can be requested by emailing icb.enquiries@nhs.net.
NHS Mid Essex CCG – facts and figures
CCG Headquarters
Wren House, Hedgerows Business Park,
Colchester Road, Chelmsford, Essex, CM2 5PF
Communities Covered
Chelmsford, Braintree and Maldon Districts.
Population (registered with a
GP) at 1 April 2022
Total Mid Essex GP registered population is
405,344
Number of member GP
practices at 31 March 2022
39 (with about 250 GPs between them)
Number of CCG employees
212 staff, 187.02 whole time equivalent (WTE)
Total health funding and
running costs expenditure
(Q1 2022/23)
£197.8m
Our Strategy
The MSE Health & Care Partnership developed its five-year strategy in December
2019. The strategy outlines 4 key ambitions, with the overarching aim to reduce health
inequalities. The strategy outlines that we would achieve this through:
• Creating opportunity for our residents – supporting education, employment,
and socio-economic improvements for our residents. We have developed this
ambition further - for example, extending the successful work led by MSEFT on
hospitals as Anchor institutions, and starting work to implement our agreement to
a system-wide Anchor Charter in 2021.
• Supporting health and wellbeing – including continuing our focus on
prevention, self-care, lifestyle support. We have undertaken much work in this
area continuing to work in partnership to target prevention opportunities and we
have been working with public health colleagues to focus particularly on healthy
weight as well as through schemes such as BP at Home.

Page 8 of 72
• Bringing Care Closer to Home – where this is safe and possible. We have
been progressing with a number of developments through PCNs and Alliances to
bring services closer to home.
• Improving and Transforming our Services – we know that our services are
under considerable pressure, and we are not providing the level or quality of
service that we would like. There are several transformation programmes
progressing, underpinned by system working on workforce, digital, and finance to
bring improvements in primary care, cancer care, elective recovery, urgent care,
community diagnostics, flow through the system and care arrangements. Our
Stewardship programme has started to develop and will continue to be key in our
future approach to service improvement and transformation.
We will take the five-year strategy into the new ICS and use the early period of the
Integrated Care Partnership (ICP) formation to begin work to develop the Integrated
Care Strategy – taking our three upper tier local authority Joint Strategic Needs
Assessments (JSNAs)
1
and health and wellbeing strategies to develop a single strategy
for Mid & South Essex.
As a partner in the provision of health and care services to the population PCNs are
starting to participate and help shape, where appropriate, in the production of these
needs assessments.
We have been clear that we want the hallmarks of our ICS to be:
• Evidence and data driven.
• Have a true partnership with our communities and use their lived experience and
insight to help us shape our work.
• Ensure clinical and care professionals are leading strategy formation and
supporting decision-making.
NHS Mid and South Essex
Key activities in quarter 1 of 2022/23
During 2022/23 the system completed the establishment of the ICS by:
1
A joint strategic needs assessment (JSNA) looks at the current and future health and care needs of
local populations to inform planning and commissioning of health, well-being and social care
services. They are often, but not always, led by the local authority(ies) of an area but do require
participation from all appropriate partners to:
1) Collect, analyse and interpret health and care needs information.
2) Participate in engagement work between partners or with the population.
3) Follow up and implement recommendations.
Page 9 of 72
• Successfully navigating assurance processes to establish the Mid and South
Essex Integrated Care Board (ICB) on 1July 2022.
• Developing Partnership and governance structures to enable the new Integrated
Care Partnership to meet its statutory obligations and continue our collaborative
working with partnership organisations as we become established.
• Developing our strategies, policies and processes to support our working as an
Integrated Care System.
• Supporting our four Alliances to further develop their partnership working with
local authority colleagues, Healthwatch and community and voluntary sector
organisations to further develop delivery plans for their local population.
• Undergoing a staffing re-structure to reflect the change from CCGs to the ICB,
supporting our staff through this complex process.
• Completing the closure of the five mid and south Essex CCGs and ensuring
responsibilities are appropriately transferred to the new ICB.
• Preparing to take on new responsibilities from NHS England as part of our
establishment as an ICB.
• Beginning to embed our Population Health Management (PHM) programme
working in collaboration with our PCNs.
• Publishing our engagement strategy that defines how we will gain and use
insight from our communities in the work that we do.
• Developing and agreeing a system wide quality strategy, bringing together all
aspects of the health system.
• Further developing our system finance approach through the System Finance
Leaders Group.
• Embedding joint accountability and assurance through our System Oversight and
Assurance Committee, co-chaired by the Accountable Officer and the NHSE
Regional Director for Strategy and Transformation – and further developing our
embedded assurance model with NHSE colleagues so as to reduce traditional
transactional assurance processes between the system and NHSE.
• Developing our approach to clinical and professional leadership, including how
the clinical and multi-professional congress supports the ICS and our
Stewardship programme to ensure the expertise of clinicians and care
professionals is at the heart of our work.
• Developing the work of MSE Partners as a means to supporting innovation and
improvement.

Page 10 of 72
Integrated Care Board
The ICB will take on all of the functions of the CCGs and, over time, some
commissioning functions from NHSE. It will be responsible for the system’s entire NHS
finance allocation and will take responsibility for workforce, digital, data and
engagement.
Anthony McKeever has been appointed as the Chief Executive Officer (CEO) designate
of the new ICB and Professor Michael Thorne CBE, has been appointed as Chair
designate of the ICB. Non-executive members for the new ICB Board have been
appointed and remaining appointments to the executive team have now been finalised.
NHS England confirmed the creation of the ICB and ICS on 1
st
July 2022.
Integrated Care Partnership
The ICP has been established as a joint and equal partnership between the NHS and
our upper tier local authorities. Together, we have agreed that the ICP will be chaired
by Professor Thorne so as to ensure consistency and coherence across the ICS, with
the three health and wellbeing board chairs of our upper tier local authorities acting as
vice chairs for the ICP. We have agreed membership of the ICP and started to develop
its work programme. The first task of the ICP is underway whereby we are beginning to
develop a new Integrated Care Strategy for the ICS, and for the population of Mid &
South Essex.
Local Achievements
Covid Vaccinations
During 21/22 there were multiple vaccination sites across mid Essex, run by a mix of
General Practices and Pharmacists. The table below shows the number and
percentage of people vaccinated across mid Essex last year split by first dose, second
dose and booster, this work continued during Q1 2022/23.

Respiratory Virtual Clinics
Following a successful pilot with 2 Mid Essex Primary Care Networks (PCNs), Mid
Essex commissioned MDT Respiratory Virtual Clinics for all Mid Essex PCNs. Across
the clinics, 8 different respiratory education topics have been discussed, delivered by a
respiratory consultant and respiratory specialist, and 83 individual complex patient
cases have been discussed collaboratively, with clear actions agreed for each patient.
Preliminary outcomes demonstrate strong findings of improved patient care and
collaboration across profession, with 74% primary care attendees in agreement that the
clinic improved confidence, knowledge, and attitudes regarding the management of
complex respiratory patients in primary care. 31% of patients discussed were
recommended a change to their diagnosis, and 58% were recommended a change to
their treatment (e.g., referral to mental health services or pulmonary rehabilitation, for
example). A full 12-month evaluation will be produced imminently, including follow-up
interviews of attendees. This project has been published as best practice by NHSE.
Prevention and early intervention- Freshwell low carbohydrate programme
To expand the success of the Freshwell low carb programme, the service has been
upscaled across the Colne Valley PCN, delivered by the PCN Health and Wellbeing
coaches (funded by the Additional Roles Reimbursement Scheme).
The service, originally delivered as a tier 2 weight management style of service (12-
week behaviour change), has organically evolved to further engage and involve the
local community. Examples include: weekly drop-in information sessions at GP
Practices throughout the PCN (delivered by volunteers); community groups that meet to
discuss the lifestyle (organised by volunteers), enjoy social activities, and attend
parkrun each week. The outcomes of the programme continue to demonstrate clinically
significant weight loss (maintained at 12-months), remission of Type 2 Diabetes in
some cases, reduced prescribing of medication for many patients with Type 2 Diabetes
(evidenced by significant prescribing cost savings for the Practices, in reverse of the
national trends), and improved self-assessment of wellbeing, and life satisfaction for the
majority of patients. The service leads have also engaged with the University of Essex
to explore further evaluation work.
Page 11 of 72
To increase accessibility of the programme, from March 22, the PCN will be working
with the MSE ICB to produce extra meal planners, tailored to specific groups at risk of
health inequality.
Physical Health Checks for individuals with Serious Mental Illness (SMI)
With the launch of our Integrated Primary Care Community (IPCC) programme to
deliver mental health services more holistically without organisational barriers between
primary care, secondary care, and the voluntary sector the way we deliver health
checks for people with SMI is improving. As part of the IPCC programme a Physical
Health Team pilot begun with Healthcare Assistants recruited to provide physical health
checks that are compliant with QOF indicators for mental health.
The national target for completed health checks is 60%, since the IPCC programme
and launch of the service in Oct 2021 performance has improved from 15.7% (Mar 21)
to 44% (Mar 22). The next stage is to expand the service to ensure a Health Care
Assistant is integrated into all 9 PCNs in Mid Essex and incorporate the additional
support and guidance for; nutrition, exercise, sexual health and promotion of
vaccinations programmes and public health screening programmes, as well as starting
to work with system partners to look at a more holistic approach to supporting this
cohort by looking at the wider determinants of health, their impact and support that can
be offered.
PCN Development
In 21/22, two PCNs (Chelmsford West PCN and Dengie and South Woodham Ferrers
PCN) across Mid Essex bid for Accelerator status and are subsequently being
supported with local initiatives driven primarily by population health data.
21/22 saw the forging of a working relationship with Writtle University College. The
launch of the Colleges Sports and Health Hub lends itself to collaborative working and
joined up pathways, most notably with Chelmsford West PCN, whose geographical
footprint they fall within.
The “PCN Livewell Garden” based at Tennyson House Surgery continues to be
successful as a social prescribing and volunteering space and is successfully overseen
by the Chelmsford CVS. This initiative is now being replicated at the Writtle GP surgery.
South Woodham Ferrers & Dengie PCN have been working up a model for a virtual
PCN, that will integrate teams from across health and care to support those with
complex frail needs, using data to identify those people most at risk and implement
proactive care and interventions to support them. The aim over time is to reduce
repeated, reactive, urgent demand on teams and services as capacity becomes united
and efficiently coordinated ensuring local residents get the right support, by the right
team, at the right place and time for them.
Asset Based Community Development
In May 2021, Community360, Chelmsford CVS and Maldon & District CVS were
commissioned by the mid Essex Alliance to deliver a Mid Essex Mapping exercise, the
outcome of which provided a comprehensive analysis of existing community assets and
the strengths and opportunities for growth in the voluntary and community sector across
Page 12 of 72

Mid Essex. This is the first time this information has been readily available to system
partners and is being used to support further development and growth of community
assets, as well as realising where gaps are that we need to fill to support with the
priority to reduce health inequalities and create preventative and self-care approaches
to health and wellbeing for our communities.
How we have performed
The CCG monitors health outcomes against a range of NHS Constitutional Standards’
that are set nationally
1
. Performance across the system has generally been below the
set standards due to capacity pressures throughout the health and care system.
The CCG has been working with local providers of services and NHS
England/Improvement (which is the regulatory organisation for the CCG and providers
of services) to agree the system transformation required to support improvements in
care for patients.
As seen nationally, performance against the standards has been directly impacted by
the Covid-19 pandemic. A key issue experienced nationally is the increased waiting list
and backlog sizes for planned elective care during the COVID19 pandemic. As directed
from national guidance whilst capacity was reduced, non-urgent diagnostic tests
together with elective planned appointments and procedures were paused to prioritise
emergency, urgent and cancer work.
A key risk affecting the delivery of performance and recovery is ensuring workforce is in
place to meet the delivery of the increased capacity required to recover and meet
demand.
Key issues and risk
The Covid-19 pandemic had a significant impact upon the operation of NHS services
across the country, which brought with it several associated risks, firstly in relation to
the effects of the virus itself and secondly in relation to the effects that management of
the pandemic has had on core services and the achievement of constitutional
standards.
The former has been managed well during the year, which is reflected in the lowering of
risk in relation to the effects of the virus as a result of the success of the Covid-19
vaccination programme and greater understanding of how to care for patients with the
virus. The Mid and South Essex CCGs continue to manage the impact of risks on core
services, focusing on restoring performance back to pre-Covid levels.
Further information on the CCG’s key risks and risk profile is provided in the Risks
section of the Performance Analysis report.
Page 13 of 72
Performance Analysis
Introduction
Measuring our performance against a range of indicators, including nationally agreed
quality standards, is important for our patients and the public as they relate to key areas
such as access, treatment times and quality of care. Performance against these targets,
and the plans we have to improve them, is overseen by the Finance and Performance
Committee.
2022/23 has, as outlined within this report, provided challenges to delivery and recovery
of performance standards. The below summary shows the performance as reported in
June 2022, this is the most up to date information at time of writing this report.
Mid and South Essex continues to work collaboratively with our provider partners to
support recovery of performance standards and outcomes for our population. This work
is ongoing and continues in the work of the ICB.
Performance summary
The following is an overview of how the system has performed against the constitutional
standards.
• NHS Constitution – Urgent and Emergency Care (UEC)
The UEC Strategic Board oversees performance and planning for all UEC services
(East of England Ambulance Service (EEAST), NHS111, A&E, Urgent Community
Response Team (UCRT), Mental Health Emergency Department (ED) and has
members from both health and social care.
Daily operational calls (Daily Tactical Care call) are in place with system partners,
ensuring plans are in place or reviewed to mitigate presenting pressures across the
system.
Organisations across the system are working collaboratively to improve ambulance
offload times (for conveyed patients) and the flow through ED. For example, community
providers have an Urgent Community Response Team (UCRT) team working with
EEAST to, where appropriate, provide an alternative to conveying patients to acute
hospital. The Virtual Wards work is continuing to be developed to support admission
and reduce the need for conveyance of frail elderly patients where more appropriate.
The EEAST Hospital Ambulance Liaison Officer (HALO) are working within Mid and
South Essex Foundation Trust (MSEFT) ED to facilitate the triaging and handover of
patients arriving via ambulance to release EEAST staff. To facilitate optimal flow
through the hospital, Local Authorities ensure continued support for timely discharges
from the acute.
The key issues for the UEC programme include the following where performance is
below standards:
Page 14 of 72

Page 15 of 72
Ambulance Response Times
Standards:
• Respond to Category 1 calls in 7 minutes on average, and respond to 90% of
Category 1 calls in 15 minutes
• Respond to Category 2 calls in 18 minutes on average, and respond to 90%
of Category 2 calls in 40 minutes
• Respond to 90% of Category 3 calls in 120 minutes
• Respond to 90% of Category 4 calls in 180 minutes
The ambulance response times remain below the NHS constitutional standards.
The following table shows the range of 90
th
centile and mean response times across
Mid Essex CCG for each of the four categories of calls and respective standards.
Emergency Department – waiting times.
Standard:
• 95% of patients have a maximum 4-hour wait in A&E from arrival to
admission, transfer, or discharge
Within MSEFT A&E (Type 1), the 95% four-hour performance is below the constitutional
standard as per following table.
• Elective Care
Key issues for the Elective programme include waiting time performance being below
standards for Diagnostics, Cancer and RTT (Referral To Treatment).
Diagnostics Waiting Times
Standard:
• The constitutional standard is no more than 1% of patients waiting 6 weeks
or more for a diagnostic test and no patients waiting 13+ weeks.

Page 16 of 72
As seen nationally during the COVID-19 pandemic, waiting times for diagnostic tests or
procedures has increased significantly with a large increase in the number of patients
waiting over six weeks and 13 weeks.
The waiting times for diagnostic tests remain below the NHS constitutional standards.
During Quarter one 2022/23, 75% of patients waited less than six weeks (below standard
of >= 99%) with circa 6% of patients waiting over 13 weeks (below standard of zero) at
Mid Essex CCG.
The System Diagnostic Board oversees performance and planning for diagnostics
across MSE supported by sub-groups including assurance.
A significant acute challenge lies in non-obstetric ultrasound. An identified issue
includes workforce capacity regarding Sonographers.
Cancer Waiting Times
Standards: For people with suspected cancer:
• To see a specialist within 14 days of being urgently referred by their GP or a
screening programme.
• To not wait more than 28 days from referral to getting a cancer diagnosis or
having cancer ruled out.
• To receive first definitive treatment within 31 days from decision to treat
• To start drug, radiotherapy, and surgery subsequent treatments within 31 days
• To receive their first definitive treatment for cancer within 62 days of receipt of
urgent referral.
The waiting times for patients on a cancer pathway remain below the NHS
constitutional standards.
The following table shows the Quarter one 2022/23 position for Mid Essex CCG for
each of the waiting time standards.
The MSE HCP Cancer, Palliative & End of Life Care Board oversees cancer assurance
and transformation supported by sub-groups including the Cancer Programme Delivery
Group (for assurance and focus on national, regional, and local commitments and
deliverables); Quality Cancer meeting; and the Palliative Care Delivery group.

Page 17 of 72
The wider system is working with MSEFT and Cancer Alliance through plans to
transform the diagnosis, treatment, and care for cancer patients to recover performance
for the local population.
Referral to Treatment (RTT) Waiting Times
Standards:
• The constitutional standard is starting consultant-led treatment within a
maximum of 18 weeks from referral for non-urgent conditions. Since the
significant increase in waiting times following the global COVID pandemic, the
NHS is working to achieve the following 2022/23 planning round asks:
• eliminate waits of over 104 weeks as a priority by July 2022 and maintain
this position through 2022/23 (except where patients choose to wait
longer)
• Reduce the number of patients waiting 78+ weeks on an RTT pathway to
zero by March 2023
• Reduce the number of patients waiting 52+ weeks on an RTT pathway to
zero by March 2025
As of Quarter one 2022/23, there were 5 patients waiting 104+ weeks, 193 patients
waiting 78+ weeks and 1,963 patients waiting 52+ weeks on an RTT pathway for Mid
Essex CCG.
The Elective Board oversees RTT assurance.
Mid and South Essex system through collaborative working between partner
organisations including MSEFT, Independent Sector Providers, Community Providers
and primary care are working together to ease pressure at the acute trust, ensuring
patients with 2ww or urgent referral are prioritised, and available capacity is maximised
across the system.
Community providers are working with MSEFT to, where appropriate, provide an
alternative place for treatment to waiting and being treated at MSEFT. Local
Independent Sector providers are providing additional system capacity for patients
waiting at MSEFT facilitated by commissioners and MSEFT. Primary care is supporting
with demand management/referral diversion plans.
• Mental Health
A key issue for the mental health work programme is workforce capacity and
constraints with recruitment to mitigate against workforce vacancies. In terms of
governance, performance is overseen at the Mental Health Partnership Board.
Improving access to psychology therapies (IAPT)
Standards include:
• 75% of people referred to the improving access to psychology therapies
(IAPT) programme should begin treatment within 6 weeks of referral and 95%

of people referred to the IAPT programme should begin treatment within 18
weeks of referral
The six and 18-week waiting time standards for people referred to the IAPT programme
to start treatment is being sustainably achieved across Mid Essex CCG.
A priority is to increase IAPT in terms of number of people accessing the programme.
Early Intervention in Psychosis (EIP) access
Standard:
• more than 50% of people experiencing first episode psychosis commence a
National Institute for Health and Care Excellence (NICE)- recommended
package of care within two weeks of referral.
The EIP access standard is being sustainably met for Mid Essex CCG.
Improve Quality
Q1 2022/23 has continued to bring challenges and demands on our services, during
which time colleagues from all sectors have worked hard to ensure we continue to
maintain quality care to thousands of patients across our system.
Mid and South Essex CCGs (MSE) have continued to maintain core quality functions,
such as serious incident monitoring and investigation, safeguarding, quality assurance
and infection prevention and control. At times having to prioritise our work to flex with
the needs of the system working towards the transformation of services and processes
in readiness for transition to the ICB.
Care Quality Commission (CQC)
The ratings of our primary providers remain as:
• Provide Community Interest Company - Outstanding
• Essex Partnership University Trust (EPUT) Community - Good
• Mid and South Essex Foundation Trust (MSEFT) – Requires Improvement
• EPUT Mental Health Services – Requires Improvement
• North East London Foundation Trust Community Services – Required
Improvement
• East of England Ambulance service – Requires Improvement
Following a review of Maternity services, the CQC gave an overall rating of - Requires
Improvement. This represents an improvement and acknowledges the hard work being
undertaken as part of the MSE wide Maternity Improvement Programme. The CQC
Section 31 notice for Maternity remains in place, with ongoing support provided through
the NHSE/I Maternity Safety Support Programme. The Maternity Improvement
Programme has been updated to reflect CQC’s most recent recommendations and
strengthened to include learning from the Ockenden Report, both will support and
further improve the transformation of Maternity services across MSE.
Page 18 of 72
System Quality
The establishment of the Mid and South Essex System Quality Group has significantly
strengthened the quality surveyance, oversight and wider system learning from all key
providers and partners. This group has been instrumental in developing system
strategy leading into the Integrated Care Board and Partnership.
Patient Safety Specialist meetings continued as one of the elements from the National
Patient Safety Strategy. These meetings aim to share knowledge and learning across
our system through the collaboration of all acute and community partners.
MSE Quality Teams have also supported MSEFT to undertake deep dive harm reviews
on all patients whose care pathways breached cancer standards and those breaching
referral to treatment standards. This has enabled the Trust to identify where harm has
occurred and for learning to be used to change pathways and processes moving
forward.
Mental Health Quality Teams have continued to work closely with Essex Partnership
University NHS Foundation Trust (EPUT), the newly formed Mental Health Provider
Collaborative and other local providers to ensure robust oversight of the quality and
safety of care provided.
Special Educational Needs and Disability (SEND)
Essex - The Ofsted & CQC revisit took place between 17 and 19 May 2022. The area
was found to have made sufficient progress in addressing all three of the significant
weaknesses identified at the initial inspection. They noted that:
• Area leaders had worked diligently to establish structures for strategic
oversight and governance that involve all partners
• There has been a palpable change in the culture among partners to joint
working
• Processes are in place to quality assure health and care partners’
contributions to EHC plans resulting in better quality plans. Partners from
health, social care and education are now contributing meaningfully to the
production of plans.
Infection Prevention and Control
The Infection Prevention and Control team have remained busy with continued
oversight of the Covid-19 response as well as healthcare associated infections such as
Methicillin resistant Staphylococcus aureus bacteraemia (MRSAB) and Clostridioides
difficile infection (CDI) cases. The team continue to support all providers across the Mid
and South Essex locality
Patient Experience
The Quality Teams have continued to ensure the voice of the patient is heard for
example through the programme of patient stories which capture authentic lived
experiences. This, in turn, is shared with Commissioners and has directly influenced
commissioning decisions. Furthermore, co-production with patients and services users
was a key focus of stakeholder development of the MSE Quality Strategy.
Page 19 of 72
Care Sector
The Quality team continued to support the provision of Enhanced Care in Care Homes.
This has furthered the support provided to homes during the Covid-19 pandemic with
continued training and new technology to support remote and daily hub calls to enable
rapid responses to our homes.
Reducing Health Inequality
Duty to reduce inequality
Health inequalities are the preventable, unfair, and unjust differences in health status
between groups, populations or individuals that arise from the unequal distribution of
social, environmental, and economic conditions within societies. This in turn can
determine the risk of people getting ill, their ability to prevent sickness, or opportunities
to act and access treatment when ill health occurs.
Addressing health inequalities is a core strategic ambition of the MSE Health & Care
Partnership (HCP). The significant increase in collaborative working accelerated by the
Covid pandemic has enabled us to tackle these issues across the HCP. The MSE ICS
five-year HCP strategy outlines our commitment through working with our partners to
reduce inequalities. We aim to achieve this by:
(1) Creating opportunities through education, employment, housing, and growth
(2) Supporting health and wellbeing
(3) Bringing care closer to home and
(4) Transforming and improving health and care services.
The Health Inequalities Oversight Group (HIOG) was established to provide an
enhanced focus and ensure the delivery of requirements to reduce inequalities. The
HIOG group has cross organisational representation from NHS Providers, Local
Authority Community and Voluntary Services, Public Health, Primary Care, and other
NHS organisations. This group reports into the System Leadership Executive and MSE
Healthcare Partnership Board.
The work to reduce health inequalities is driven by a maturing network of equity
leadership. All system providers have a named Inequalities Senior Responsible Officer
(SRO), and each Alliance has named inequalities leads who will support the Primary
Care Networks (PCN’s).
Progress in health inequalities improvement is established through the use of the
System Outcomes Framework which are health inequalities indicative metrics aligned to
system ambitions. System and Place-based inequalities plans are focused on the
amalgamation of Prevention, Population Health Management, Personalised Care, Self-
Care and strengthening our community-based approach. A place-based approach to
addressing inequalities is being delivered with our four Alliances which sees NHS
organisations, Primary Care, Health and Wellbeing Boards, Local Authority Public
Health, Social Care and children’s services, voluntary sector organisations working
collaboratively through a single, shared “place plan” to address agreed key priorities.
Page 20 of 72
Addressing the wider determinants of inequalities, particularly in our most deprived
areas, is crucial in reducing inequality gaps. With an explicit focus on the social
determinants of health - at system and place level - partnership working is embedded in
our approach to inequalities improvement. This can be seen in areas such as Better
Start Southend, which delivers targeted provision to children aged 4 and under in the
most deprived wards in Southend, and the Mid and South Essex Foundation Trust
(MSEFT) Anchor Programme initiatives that are targeting employment opportunities to
young people and adults in the most deprived wards.
To realise our ambition to reduce inequalities, we have identified community asset
engagement as a core principle within our engagement strategy - which is driven by our
aim to ensure local voices are heard, improved local confidence and to be unified to
creating changes. Embedding co-production into the equalities workstream has been a
key part of the MSE equalities approach. Following a co-design initiative for people with
Learning Disabilities accessing hospital services in 2021-22, MSEFT began to
implement a detailed action plan to improve access for people with Learning Disabilities
across hospital sites. We are also working with providers in other parts of Essex to
jointly take actions for the benefit of our population.
The Core20PLUS5 approach to tackle health inequalities was also introduced in 2021.
This approach outlines a framework to accelerate health inequalities improvement
through focused approaches targeted at the Core20 (the most deprived 20% of the
population) PLUS (other inclusion groups) and 5 (clinical areas of focus which are
Cardiovascular disease, Maternity, Cancer, Respiratory and Mental Health). This
Core20PLUS5 framework has been adopted across the system and health inequalities
improvement plans at system and place have been refined to reflect the Core20PLUS 5
approach.
The work across the health partners within Mid and South Essex continues to be
focused on:
• Restoring NHS services inclusively which incorporated analysing the waiting lists
by ethnicity and deprivation to support local action plan to reduce the barriers to
accessing service for certain groups
• Mitigating against digital exclusion by maintaining access to face-to-face
consultations to ensure digital access does not disadvantage some patients
• Ensuring datasets are complete and timely by improving data collection on
ethnicity across all healthcare settings
• Accelerating preventive programmes that proactively engage those at greatest
risk of poor health outcomes which includes ensuring high level of vaccination
uptake across all areas of the population, health checks are undertaken for
people with Learning Disabilities or Serious Mental Illness, and a focus on the
five clinical areas within the Core20 plus 5 framework.
Within Primary Care, the Tackling Neighborhood Inequalities Directed Enhanced
Service (DES) has called for a coordinated approach to tackling inequalities within
Primary Care. All PCNs are required to nominate a health inequalities lead will be to act
as a focal point and champion for this work. PCNs will also work with commissioners
and PHM teams to design and deliver inequalities improvement intervention(s) for a
selected population group experiencing inequality.
Page 21 of 72

Page 22 of 72
We have also begun the development of an overarching ICS Health Inequalities
Strategy.
Engaging People and Communities
We put patients and the public at the heart of our CCG. Working in partnership with
patients, carers, families, and local people within their own communities brings a
different perspective to our understanding and can challenge our view of how we think
services are received and should be delivered in the future. Service provision can be
improved if we can learn more about the views, experiences and concerns of patients,
service users, carers, and our wider communities. We believe that better decisions are
made when patients and professionals work together. We strive to make sure we get
the community involved at the very beginning of a project and build things around local
need rather than organisations.
Our legal duties and principles of engagement
The CCG has a duty, under Section 14Z2 of the NHS Act 2006, to involve the public in
commissioning. Here we provide an overview of the engagement activities that have
taken place in this reporting period (April – June 2022).
We know from experience that engagement with patients, carers and our local
communities can result in:
• Better outcomes and patient experience
• Improved services
• Reduced demand
• Deliver change
Engagement from Mid Essex CCG within the Mid and South Essex Health and
Care Partnership
Collectively the CCGs and partner organisations across mid and south Essex have
benefitted from sharing best practice. So, we have been expanding the ways we work
with local people and to join the conversation in a way that suits them:
• The Mid Essex Patient and Community Representatives Group held every two
months with invitees including delegates Healthwatch Essex, GP patient
participation groups, charities and local authorities.
• Attending CCG meetings and Governing Body meetings held in public.
• Seeking involvement with Primary Care Networks (PCNs) as they begin to
deliver on their obligation to engage with their residents.
• Joining ad hoc meetings to inform our work – for example, we hosted gatherings
of patient representatives who helped us to design recent communications
campaigns on GP pressures and other key topics.
• Being part of our Citizen Panel, called Virtual Views, that can be found here.
In 2022 we asked for their views on; GP access and shared decision making.
Following and interacting with the CCG on social media or visiting our website or
subscribing to one of our newsletters.
• Contacting the CCG with specific ideas, questions, or concerns.
Partnerships across the health and care system
We actively worked and collaborated with our local Healthwatch and voluntary,
community and faith sector colleagues.
Following the successful work undertaken by the Essex Vax Van which enabled a new
model of outreach and ensured a culturally sensitive approach for communities not
engaging in the national Covid-19 vaccination programme, was then used for
spirometry testing into the community.
We listened to feedback on a local weight management clinical pathway which has
informed a new model and covers the whole of mid and south Essex.
Improving accessibility to healthcare information
The CCGs have continued to improve accessibility to healthcare information working
closely with the Council for Voluntary Services (CVS). Work includes providing
information in a number of formats; easy read, information in different languages or
through for learning disabilities and videos produced by the CCG with subtitles and
where possible a British Sign Language interpreter on the screen.
Children’s Health Matters: we worked with parents and carers of children aged 0-5
living in mid and south Essex to co-design a useful guide to better manage childhood
Illnesses. It provided an opportunity for them to influence local communications and
behaviour interventions and support our campaign. This has led to the delivery of
regular electronic newsletters to the right audiences, with the right messages, that
parents and carers have supported.
Social media and digital marketing
The CCG has also presented appealing, insights-driven digital communications in line
with priorities, offer opportunities for engagement and are viewed as a trusted source of
information.
Our digital communications channels including social media, website and e-publications
have been used to:
Explain and showcase CCG work to residents of mid and south Essex, health
and social care colleagues and beyond.
To encourage residents to engage with the CCG via its digital channels,
motivate those individuals to take action that will help them stay well and use
health and care resources appropriately, and support them to lead their best
lives.
To build the CCGs online presence.
To analyse digital engagement data to build insight-driven campaigns that are
supported, shaped, and shared by organisations across the Partnership, and to
measure and evaluate the effectiveness of those campaigns.
Our ambition
Our ambition is to place engagement at the forefront of all we do in mid and south
Essex, creating healthier communities that people recognise and feel a part of.
Page 23 of 72

Together we will aim to co-design and deliver new models of care and different ways of
working that make a real difference to people and their local communities. We will work
collaboratively across local authority, health, and voluntary sector to understand and
build our communities, maximising the collective impact we can have on the health of
our population.
Health and Wellbeing Strategy
The MSE Health & Care Partnership’s 5-year strategy is built upon the priorities agreed
through the three upper tier Health and Wellbeing Boards which continues to underpin
the work we do together.
Through the ICS and our four Alliances we have been involved with and contributed to
the development of refreshed joint Health and Well Being strategies and will continue to
ensure our plans are supportive of delivering the aims of these strategies at system,
Alliance and PCN level.
Senior leaders from the CCGs have engaged with all three upper tier local authority
Health and Wellbeing (HWB) Boards, as well as district, borough, and city fora. CCG
leaders are core members of the HWB Boards and have proactively participated in
attending meetings, workshops, and events, contributing to the refresh of joint health
and wellbeing strategies and co-producing Alliance plans. Across the three Upper Tier
Local Authorities (UTLAs) we have continued work on a joint mental health strategy, as
well as a children’s partnership plan.
The chairs of the three UTLA HWB Boards sit on the MSE Health & Care Partnership
Board, as do senior officers, including Directors of Adult Social Care and Directors of
Public Health.
Financial Review
Financial overview
Our full statutory financial accounts are included from page 72 onwards. This section
provides a summary of our 2022/23 financial position from 1 April 2022 to the cessation
of the CCG on 30 June 2022. Our Head of Internal Audit offers an opinion on Financial
Systems Key Controls and other matters which can be found on page 52. whilst our
overall financial management arrangements and financial statements were subject to
audit review and opinion by our external auditors, KPMG, as part of their annual review
of our accounts (see page 100 for their full audit opinion).
CCG funding
During the period 1 April 2022 to 30 June 2022 (Q1) the CCG has continued to operate
under the financial regime and allocation methodology that was put in place at the
beginning of 2020/21 to support the ongoing response to the Covid pandemic this has
been subject to a few modifications.
Firstly, arrangements for healthcare have been considered to be in a period of post
pandemic recovery resulting in a cessation of funding for the Hospital Discharge
Programme (HDP) to support discharges from Hospital once patients have been
medically optimised to allow for recovery of the Elective backlog and secondly the
Page 24 of 72

Page 25 of 72
transition from CCGs to Integrated Care Boards that has been agreed nationally and
became effective from 1 July 2022.
This has led to funding changes for the final CCG reporting period where the final CCG
allocation has been matched to equal CCG costs incurred with any under or over
expenditure compared to the anticipated allocation being adjusted in the remaining
allocation for the successor body the Integrated Care Board.
Mid Essex CCG has continued as the nominated lead CCG for receiving and managing
the distribution of most non-organisational specific system allocations. As a CCG we
received and managed funds across and on behalf of our CCG partners in Thurrock,
Southend, Castle Point and Rochford and Basildon and Brentwood.
In Q1 2022/23, our in year total healthcare funding including system funding was
£192.02m. CCG expenditure for Q1 was £192.02m, resulting in a net breakeven
position.
NHS planning guidance requires CCGs to meet the ‘Mental Health Investment
Standard’ (MHIS). This requires CCGs to demonstrate that expenditure on mental
health services has grown year on year. In 2022/23 the MHIS was set for the whole
financial year and was achieved.
How your money was spent
The following chart shows the areas of expenditure we have made for healthcare
(including CCG running costs). (Core GP-led services (primary care) are commissioned
by NHS England and are not accounted for in the CCGs accounts).
Expenditure April to June 2022
Acute Services £127.4m
Mental Health Services £12m
Community Health Services
£14.1m
Continuing Care Services
£7m
Primary Care Services
£13.6m
Primary Care Co-
Commissioning £14.6m
Other Programme Services
£1.6m
Running Costs £1.7m

Page 26 of 72
Capital spending
We did not require a CCG capital allocation for Q1 2022/23, but the Mid and South
Essex Health and Care Partnership footprint was awarded Estates and Technology
Transformation Funding (ETTF) towards primary care estates projects and GP IT. ETTF
expenditure is accounted for by NHSEI.
Paying our suppliers and providers
National rules mean we must aim to pay all valid invoices by the due date or within 30
days of receiving them, whichever is the latter. The NHS aims to pay at least 95% of
invoices within 30 days of receipt, or within agreed contract terms. In Q1 2022/23 we
met all four targets (based on invoice numbers and value of expenditure) for NHS and
non-NHS invoices – see Note 6 of the Financial Statements for details.
We are also an approved signatory of the Prompt Payment Code. The government
designed this initiative with the Chartered Institute of Credit Management to tackle the
crucial issue of late payment and to help small businesses. Suppliers can have
confidence that any organisation signed up to the code will pay them within clearly
defined terms and that proper processes are in place to deal with any disputed
payments. Approved signatories have committed to:
• Paying suppliers on time
• Giving clear guidance to suppliers and resolving disputes as quickly as possible
• Encouraging suppliers and customers to sign up to the code.
The national measures for payment performance do not include any delays in payment
during the time that an invoice is on hold.
2022/23 financial plans and looking to the future
The unprecedented impact of the Covid pandemic has inevitably delayed the return to
normal financial arrangements. CCGs ceased to exist on 30 June 2022 and on 1 July
2022 the 5 CCGs became Mid and South Essex Integrated Care Board.
Published allocations for 2022/23 have been split between CCGs and the Mid and
South Essex Integrated Care Board although performance will be monitored on a full
year basis. Following the demise of the CCGs on 30 June 2022 the Mid and South
Essex Integrated Care Board manage and oversee the balance of £1.891bn healthcare
funding and investment on behalf of the healthcare system and will report following
closure of its first period of accounts running from 1 July 2022 to 31 March 2023.
Risks
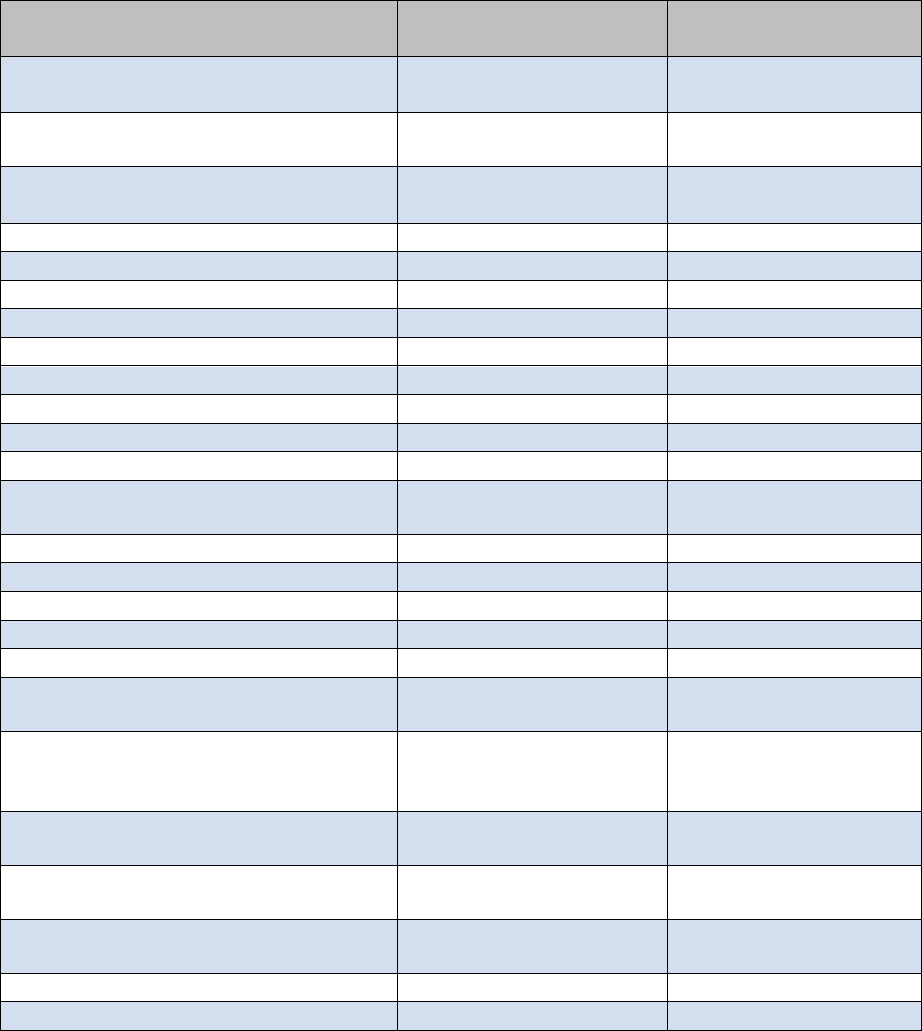
The CCG’s risk profile as of 30 June 2022 is detailed in the table below:
Workstream
RAG Rating
Total No of
Risks
Green
Amber
Red
Cancer and End of Life
0
1
1
2
Children and Young People
0
6
0
6
Community
1
4
0
5

Workstream
RAG Rating
Total No of
Risks
Green
Amber
Red
Digital and Business
Intelligence
1
3
0
4
Estates
0
2
0
2
Finance
0
2
3
5
Health Inequalities
0
1
0
1
Integrated Care System
2
3
0
5
Maternity
0
2
1
3
Medicines Optimisation
0
1
0
1
Mental Health and Learning
Disability
0
4
3
7
People
1
1
1
3
Planned Care
1
2
2
5
Population Health
Management
1
2
0
3
Primary Care
2
5
0
7
Stewardship
0
0
0
0
Urgent Emergency Care
1
6
0
7
Vaccination
0
1
0
1
Total as of 30 June 2022
13
46
8
67
Total as of 31 March 2022
13
47
8
68
During Q1 of 2022/23 the MSE CCGs’ risk profile has seen the total number of risks
reduce by 1 (from 68 as of 31 March 2022 to 67), although the number of red rated
risks remains static.
As of 30 June 2022, there were 8 red-rated risks, which related to the following 4 areas
of the CCG’s business:
Referral to Treatment (RTT) standard, cancer, access to service and capacity
The MSE CCGs continue to work with the Mid and South Essex NHS Foundation Trust
(MSEFT) to address Licence Undertakings. Arrangements are in place to ensure
oversight of the required actions to address RTT poor performance. There has been a
significant impact on performance as a direct result of the Covid-19 pandemic. Delayed
discharges and capacity out of hospital, both within health and social care, have also
impacted upon performance. In partnership with NHS England, plans, oversight groups
and reporting processes have been established to oversee restoration.
The System Quality section of this report provides an overview of action taken by the
MSE Quality teams to support MSEFT to undertake deep dive harm reviews on all
patients whose care pathways breached cancer and RTT standards.
Maternity services
Arrangements are in place (as part of the MSEFT Licence Undertakings) to address
significant concerns relating to maternity services, particularly those identified in the
Care Quality Commission report for Basildon Hospital. The Mid and South Essex
Local Maternity and Neonatal System (LMNS) are working with MSEFT to support
workforce recruitment and retention measures and the Maternity Improvement Plan,
Page 27 of 72
including a review of the findings set out in Donna Ockenden’s reports following an
independent review of maternity services to assur
e the system and identify any further
action required. Further information on maternity services is provided under the Care
Quality Commission section of this report.
Mental Health and Learning Disability Services
The Essex Mental Health Independent Inquiry is investigating matters surrounding the
deaths of mental health inpatients across NHS Trusts in Essex between 2000 and
2020. The Inquiry is in Phase 2 and will hear evidence from families, carers, and
friends of those who died; others with experience of mental health inpatient care in
Essex during the 21-year period; as well as staff, former-staff, relevant professionals,
and organisations. The Inquiry is independent of government and the health care
system. The Inquiry is planned to be concluded and to publish its report in Spring
2023.
The quality assurance of Autism Spectrum Disorder (ASD) services was added to the
risk register in May 2022 due to a significant number of individuals waiting over 12
months for assessment and diagnosis.
An impact of this is primarily due to an overall increase of referrals which has meant
patients dealing with longer waiting times, and large referral backlogs across the ICB.
Having to wait a long time for an ASD diagnosis can have a negative impact on the
person’s daily life, their physical and mental health, social functioning, and
employment.
Workforce
Workforce vacancy levels persist across MSE particularly in nursing and midwifery
areas. Ongoing international and domestic recruitment initiatives are in place with a
targeted retention strategy running in parallel. The MSE system has recently trialled a
large in-person recruitment event for entry level roles, which resulted in 170 plus offers
being made in one day. Similar initiatives will be rolled out across the system during
2022/2023. The system will begin a one workforce approach through a Health
Education England funded academy for Health Care Support Workers. The aim is to
develop a sustainable pipeline by onboarding and developing our unqualified workforce
through associate and apprenticeship roles.
Sustainable Development
As an NHS organisation, and as a spender of public funds, we have an obligation to
work in a way that has a positive effect on the communities for which we commission
and procure healthcare services. Sustainability means spending public money well,
the smart and efficient use of natural resources and building healthy, resilient
communities. By making the most of social, environmental, and economic assets we
can improve health both in the immediate and long term even in the context of rising
cost of natural resources. Spending money well and considering the social and
environmental impacts is enshrined in the Public Services (Social Value) Act (2012).
We acknowledge this responsibility to our patients, local communities, and the
environment by working hard to minimise our carbon footprint.
In October 2020, the Greener NHS National Programme published its new strategy,
Delivering a Net Zero National Health Service. This report highlighted that left unabated
Page 28 of 72

Page 29 of 72
climate change will disrupt care, with poor environmental health contributing to major
diseases, including cardiac problems, asthma, and cancer. The report set out
trajectories and actions for the entire NHS to reach net zero carbon emissions by 2040
for the emissions it controls directly, and 2045 for those it can influence (such as the
supply chain). As part of the NHS, public health, and social care system, it is our duty to
contribute towards the targets set out in this document.
As a commissioner of services, the CCG sets out a commitment to sustainable
procurement in its Procurement Policy. The CCG has taken measures to encourage
greater awareness among staff. In November 2019, the Governance Committee
recommended adoption of the NHS England pledge to eliminate single use plastics. In
December 2019, the Staff Engagement Group supported an initiative for staff to make a
“Green Pledge”.
An ICS Green Plan has been in development and sets out actions to achieve Net Zero
Carbon across the ICS. The CCG is fundamental to the delivery of this plan.
Sustainability will become business as usual across all service areas.
Modelled Carbon Footprint
In England, the NHS is estimated to account for 5.4% of the country’s greenhouse gas
emissions. The health and social care system reduced its carbon footprint by an
estimated 62% between 1990-2020, however, drastic action is now required.
Figures 1 and 2 below illustrate the key areas of focus that the NHS must deliver on to
reduce its carbon footprint and meet the Greener NHS targets of being a net carbon
zero health care service by 2045.
F
igure 1: Greenhouse Gas Protocol (GHGP) scopes in the context of the NHS

Page 30 of 72
Figure 2: Sources of carbon emissions by proportion of NHS Carbon Footprint Plus
Page 31 of 72
ACCOUNTABILITY REPORT
Corporate Governance Report
Members Report
Member Profiles
CCGs are clinically led membership organisations made up of general practices. As of
30 June 2022, the following 39 NHS practices are members of Mid Essex CCG:
Practice
Area served
Primary Care
Network
Baddow Village Surgery
Great Baddow
Chelmsford City
Health
Beacon Health Group
Chelmsford and
Danbury
Aegros
Beauchamp House Surgery
Chelmsford
Chelmsford City
Health
Blackwater Medical Centre
Maldon
Witham and Maldon
Blandford Medical Centre
Braintree
Braintree
Blyth’s Meadow Surgery
Braintree
Braintree
Burnham Surgery
Burnham-on-Crouch
Dengie and SWF
Chelmer Medical Partnership
Western Chelmsford
Chelmsford West
Chelmer Village Surgery
Chelmsford
Chelmer
Church Lane Surgery
Braintree
Braintree
Coggeshall Surgery
Coggeshall
Colne Valley
Collingwood Road Surgery
Witham
Witham and Maldon
Dengie Medical Partnership
Tillingham, the
Maylands
Dengie and SWF
Dickens Place Surgery
Chelmsford
Chelmsford West
Douglas Grove Surgery
Witham
Aegros
Elizabeth Courtauld Surgery
Halstead
Colne Valley
Fern House Surgery
Witham
Witham and Maldon
Freshford Practice
Finchingfield
Colne Valley
Greenwood Surgery
South Woodham
Ferrers
Dengie and SWF
Hedingham Medical Centre
Castle Hedingham,
Sible Hedingham,
Yeldham
Colne Valley
Kelvedon and Feering Health
Centre
Kelvedon
Colne Valley
Kingsway Surgery
South Woodham
Ferrers
Dengie and SWF
Little Waltham and Great Notley
Surgeries
Little Waltham and
Great Notley
Aegros
Longfield Medical Centre
Maldon
Phoenix (Mid Essex)
Mount Chambers Surgery
Braintree
Braintree

Practice
Area served
Primary Care
Network
North Chelmsford Healthcare
Centre
Chelmsford
Chelmer
Pump House Surgery
Earls Colne
Colne Valley
Rivermead Gate Medical Centre
Chelmsford
Chelmer
Sidney House & The Laurels
Surgeries
Hatfield Peverel,
Boreham
Aegros
Silver End Surgery
Witham
Braintree
Stock Surgery
Stock
Chelmsford City
Health
Sutherland Lodge Surgery
Chelmsford
Chelmer
Tollesbury Surgery
Tollesbury
Phoenix (Mid Essex)
Trinity Medical Practice
The Maylands
Dengie and SWF
Whitley House Surgery
Chelmsford
Chelmsford City
Health
William Fisher Medical Centre
Southminster
Dengie and SWF
Witham Health Centre
Witham
Witham and Maldon
Writtle Surgery
Writtle
Chelmsford West
Wyncroft Surgery
Bicknacre, East
Hanningfield
Dengie and SWF
Composition of Governing Body
The CCGs Governing Body is the accountable body for the performance of the CCG. It
has four GP members elected by their fellow GPs to lead the organisation alongside the
Executive membership. One of these elected GPs, Dr Anna Davey, chairs the
Governing Body meeting.
The Governing Body also has three lay members. Their roles include ensuring views
and suggestions from patients and the public are properly considered by the CCG,
providing independent judgement and sound commercial knowledge, and helping to
ensure the CCG is well run and uses public funds properly. In addition, the role of the
secondary care member ensures that the views of secondary care providers, which
includes acute and mental health services, are considered by the Governing Body.
The Governing Body also comprises of the Accountable Officer, Chief Finance Officer,
Executive Director of Nursing, NHS Alliance Director. Representatives from the Local
Authority and other CCG Executive Directors are regular attendees.
As of 30 June 2022, the board consisted of 12 members. Of these, 7 are female and 5
are male.
The main function of the Governing Body is to ensure that the group has appropriate
arrangements in place to exercise its functions effectively, efficiently, and economically
and in accordance with the group’s principles of good governance. The other key
functions are outlined in the CCGs constitution.
In February 2022, the Governing Bodies of Basildon and Brentwood, Castle Point and
Rochford, Mid Essex, Southend, and Thurrock CCG, collectively referred to as Mid and
South Essex (MSE) CCGs, agreed to ‘meet in common’ until establishment of the MSE
Page 32 of 72
Page 33 of 72
Integrated Care Board on 1 July 2022. This meant that each Board met in the same
place (virtually via MS Teams), at the same time, although they still made decisions as
separate bodies. These arrangements enabled decisions affecting the whole MSE
population to be made collectively.
The following people have been CCG Board Members during 2022/23:
• Dr Anna Davey, Elected GP, and Chair
Dr Anna Davey qualified from the Guy’s and St. Thomas’ Medical School in
1999, going on to train at The Ipswich Hospital NHS Trust and Colchester
Hospital University NHS Trust in junior doctor posts.
Anna worked as a GP in Halstead for 12 years before moving to Coggeshall
Surgery in 2017. She became a clinical lead for out-of-hospital care at Mid Essex
CCG in 2016 and became Chair in October 2018. Her clinical interests are
women’s health, dermatology, and the complex care of frail elderly patients.
• An
thony (Mac) McKeever,
Accountable Officer, Mid and South Essex
CCGs and Executive Lead, Mid and South Essex Health and Care
Partnership
Anthony, known to all as Mac, has more than 40 years’ experience in the NHS
and other healthcare organisations. Before joining the mid and south Essex
CCGs he served as Director General for Health and Community Services for the
States of Jersey.
Originally a “fast stream” civil servant, Mac joined the NHS in 1987, operating for
25 years as a CEO, helping to turn around performance at several hospitals and
commissioning organisations. Having established his own business, he served
on the Future Forum in 2010, and returned to work in the NHS in 2015.
Mac was appointed Interim Joint Accountable Officer for the Mid and South
Essex CCGs from 1 March 2020.
Mac has since been appointed Chief Executive Officer Designate for the Mid and
South Essex Integrated Care Board and System.
• Mark Barker, Chief Finance Officer
Prior to joining the NHS over 20 years ago, Mark was a Senior Manager at
KPMG, Director of Finance in various housing associations and business
controller at Transport for London. Mark has worked in a number of NHS
organisations, most recently as the Chief Finance Officer for Castle Point and
Rochford and Southend CCGs and, from 1 January 2021, he was appointed as
Joint Chief Finance Officer for the five mid and south Essex CCGs.
• Rachel Hearn, Executive Director of Nursing and Quality
Rachel is a Registered Nurse and Executive Director of Nursing and Quality
across the five Mid and South Essex CCGs. Rachel has over 20 years’ clinical
experience as a nurse within the NHS. Having worked predominantly in
Page 34 of 72
emergency and general medicine, Rachel has clinically led work on the changing
face of emergency care. Rachel’s role in commissioning focuses on quality
improvement, safeguarding adults and children and continuing health care
provision.
• Dan Doherty, Alliance Director for Mid Essex and Deputy Accountable
Officer for Mid and South Essex CCGs
Dan was previously Director of Clinical Commissioning and from 15 January
2018 was appointed Director of Clinical Transformation and Deputy Accountable
Officer. In March 2016 Dan was seconded to the Mid and South Essex Success
Regime (Locality Health and Care) for 18 months, working on system
transformation with a particular focus on innovation in health and care. Dan was
appointed as the Alliance Director for Mid Essex on 2 November 2020 and also
acts as Deputy Accountable Officer for the mid and south Essex CCGs.
Dan is a practising physiotherapist who previously worked at St Peter's Hospital
in Maldon.
• John Gilham, Lay Board Member (Governance) and Deputy Chair
John Gilham was appointed as Lay Member for Governance in July 2018. He
was formerly chief executive of two NHS hospital trusts in Essex covering a
period of almost nine years.
John has over 35 years’ management experience across a range of functions in
the NHS. Prior to joining Mid Essex CCG, he served as a public sector non-
executive director with the NHS, including undertaking the role as Chair of the
Risk and Quality Committee at East and North Hertfordshire NHS Trust.
John also has experience of working with the private sector over the last nine
years as a management consultant, focusing on how their services can best be
matched to the needs of the NHS and to give patients an improved service
experience.
• Nathalie Wright, Lay Member (Patient and Public Engagement)
Nathalie joined the CCG in 2018 as Lay Member for Patient and Public
Engagement.
Following a career in Senior Management within Financial Services Nathalie
joined the NHS within the Oncology Services team for Mid Anglia Cancer
Network.
Nathalie has experience in both the private and public sector and is a qualified
counsellor. Since 2016 Nathalie has undertaken voluntary roles working as a
mental health therapist in local education settings and is a Young Minds
ambassador.
• Pauline Stratford, Third Lay Member
Before joining the NHS, Pauline was a senior commissioner for social care
mental health services. Prior to that Pauline was a human resources and
change manager with a lead in equalities in central government. Pauline also
serves as the Lay Member for Primary Care of the Castle Point and Rochford
and Southend CCGs.
• Dr Julia Hale, Secondary Care Specialist from 1 August 2021
Dr Hale has been a consultant paediatrician for 21 years, specialising in neuro-
disability, safeguarding and adoption. She has an MSc in Community Child
Health and was a member of the CoramBAAF Health Advisory Committee for 7
years. She has experience in clinical governance, patient experience and
service reconfiguration in community services. Dr Hale also serves as the
Secondary Care Specialist member of Basildon and Brentwood CCG.
•
Dr Julie McGeachy, Elected GP and Clinical Vice Chair
Dr Julie McGeachy qualified from Nottingham University medical school in 1987
and trained as a GP in Derby. She has been a GP at the Tillingham Medical
Centre for more than 20 years.
Julie also spent five years experiencing primary care in different settlings – New
Zealand and the South Pacific – and has an interest in change and innovation in
a challenging NHS environment.
Julie completed the Future Clinical Commissioning Leadership course run by the
NHS Leadership Academy in 2018. Her clinical interests are dermatology, care
of the elderly and mental health.
•
Dr Fatai Salau, Elected GP
Dr Fatai Salau qualified from the College of Medicine, University of Lagos,
Nigeria in 1992 and has been a GP at the Douglas Grove Surgery in Witham
since 2006.
Fatai is a member of the Royal College of Physicians and has been involved with
developing changes to primary care in the Witham area. His clinical interests are
acute medicine and gastroenterology.
• Dr Elizabeth Towers, Elected GP
Dr Liz Towers was a GP at Whitley House Surgery for more than 30 years,
having spent three years as a junior doctor in the Chelmsford area. Her interests
were particularly cancer and end of life care. Liz became a Macmillan GP in
Committees, including Audit Committee
A full list of the committees supporting the Board, including the Audit Committee, and
membership of those committees is provided within the Governance Statement from
page 38 onwards.
Page 35 of 72

Page 36 of 72
Register of Interests
At all formal meetings of the board and its committees, members must declare if they
have an interest in any agenda items under discussion.
The CCG maintains a register of interests declared by board members. The register of
board members’ interests is regularly updated and included within the papers for
publicly held board meetings. This is available upon request by contacting
mseicb.enquiries@nhs.net.
Modern Slavery Act
The CCG fully supports the Government’s objectives to eradicate modern slavery and
human trafficking. The Modern Slavery Act statement of the MSE CCGs has been
adopted by the MSE ICB and is published on the website at Modern Slavery Act
Statement (hyperlinks)
Complaints to Parliamentary and Health Service Ombudsman
The CCG receives complaints from patients, carers, family members and Members of
Parliament. Where the complaint relates directly to a provider the permission of the
individual is sought to refer to the relevant provider. The CCG will analyse any trends and
themes arising from complaints and works with providers to address these. Complaints
relating to primary care services are managed by NHS England.
During Q1 2022/23, there were 74 complaints opened and 55 complaints closed, with 19
complaints still under investigation at the year end. Themes and trends included difficulty
accessing face to face GP appointments, Covid vaccination queries and funding
requests, including funding for ADHD referrals and IVF.
No complaints were referred to the Parliamentary and Health Service Ombudsman
(PHSO) in 2022/23.
Statement of Accountable Officer’s Responsibilities
The National Health Service Act 2006 (as amended) states that each Clinical
Commissioning Group shall have an Accountable Officer and that Officer shall be
appointed by the NHS Commissioning Board (NHS England). NHS England has
appointed Anthony McKeever to be the Accountable Officer of Mid Essex CCG.
The responsibilities of an Accountable Officer are set out under the National Health
Service Act 2006 (as amended), Managing Public Money and in the Clinical
Commissioning Group Accountable Officer Appointment Letter. They include
responsibilities for:
• The propriety and regularity of the public finances for which the Accountable
Officer is answerable,
• For keeping proper accounting records (which disclose with reasonable accuracy
at any time the financial position of the Clinical Commissioning Group and
enable them to ensure that the accounts comply with the requirements of the
Accounts Direction),
• For safeguarding the Clinical Commissioning Group’s assets (and hence for
taking reasonable steps for the prevention and detection of fraud and other
irregularities),
• The relevant responsibilities of accounting officers under Managing Public
Money,
• Ensuring the CCG exercises its functions effectively, efficiently, and economically
(in accordance with Section 14Q of the National Health Service Act 2006 (as
amended)) and with a view to securing continuous improvement in the quality of
services (in accordance with Section14R of the National Health Service Act 2006
(as amended)),
• Ensuring that the CCG complies with its financial duties under Sections 223H to
223J of the National Health Service Act 2006 (as amended).
Under the National Health Service Act 2006 (as amended), NHS England has directed
each Clinical Commissioning Group to prepare for each financial year a statement of
accounts in the form and on the basis set out in the Accounts Direction. The accounts
are prepared on an accruals basis and must give a true and fair view of the state of
affairs of the Clinical Commissioning Group and of its income and expenditure,
Statement of Financial Position, and cash flows for the financial year.
In preparing the accounts, the Accountable Officer is required to comply with the
requirements of the Government Financial Reporting Manual and in particular to:
• Observe the Accounts Direction issued by NHS England, including the relevant
accounting and disclosure requirements, and apply suitable accounting policies
on a consistent basis;
• Make judgements and estimates on a reasonable basis;
• State whether applicable accounting standards as set out in the Government
Financial Reporting Manual have been followed, and disclose and explain any
material departures in the accounts; and
• Prepare the accounts on a going concern basis; and
• Confirm that the Annual Report and Accounts as a whole is fair, balanced, and
understandable and take personal responsibility for the Annual Report and
Accounts and the judgements required for determining that it is fair, balanced,
and understandable.
As the Accountable Officer, I have taken all the steps that I ought to have taken to make
myself aware of any relevant audit information and to establish that Mid Essex CCG’s
auditors are aware of that information. So far as I am aware, there is no relevant audit
information of which the auditors are unaware.
Anthony McKeever
Accountable Officer
26 June 2023
Page 37 of 72
Governance Statement
Introduction and Context
Mid Essex CCG (the CCG) is a body corporate established by NHS England on 1 April
2013 under the National Health Service Act 2006 (as amended).
The CCG’s statutory functions are set out under the National Health Service Act 2006
(as amended). The CCG’s general function is arranging the provision of services for
persons for the purposes of the health service in England. In particular, the CCG is
required to arrange for the provision of certain health services to such extent as it
considers necessary to meet the reasonable requirements of its local population.
As at 1 April 2022, the CCG is not subject to any directions from NHS England issued
under Section 14Z21 of the National Health Service Act 2006.
The CCG is part of the Mid and South Essex Health and Care Partnership (the HCP)
covering the geographic areas of Mid Essex, Basildon and Brentwood, Castle Point and
Rochford, Southend, and Thurrock CCGs (the MSE CCGs). The HCP has been
created to bring local health and care leaders together to plan for the long-term needs
of local communities.
In July 2017, the five MSE CCGs formally established a CCG Joint Committee (JC) to
act collectively in the planning, securing, and monitoring of services to meet the needs
of their 1.2 million population, as well as representing the HCP footprint for services
commissioned over a larger area. As outlined within the CCG’s 2021/22 Annual
Report, due to business continuity arrangements implemented by the CCGs from mid-
December 2021 to the end of February 2022, all business delegated to the JC was
conducted by the CCG Boards meeting in common and consequently the JC did not
meet again.
All other decisions about healthcare continued to be taken locally by the relevant CCG.
Scope of responsibility
As Accountable Officer, I have responsibility for maintaining a sound system of internal
control that supports the achievement of the CCG’s policies, aims and objectives, whilst
safeguarding the public funds and assets for which I am personally responsible, in
accordance with the responsibilities assigned to me in Managing Public Money. I also
acknowledge my responsibilities as set out under the National Health Service Act 2006
(as amended) and in my Clinical Commissioning Group Accountable Officer
Appointment Letter.
I am responsible for ensuring that the CCG is administered prudently and economically
and that resources are applied efficiently and effectively, safeguarding financial
propriety and regularity. I also have responsibility for reviewing the effectiveness of the
system of internal control within the CCG as set out in this governance statement.
Governance arrangements and effectiveness
The main function of the governing body (the Board) is to ensure that the group has
made appropriate arrangements for ensuring that it exercises its functions effectively,
Page 38 of 72

efficiently, and economically and complies with such generally accepted principles of
good governance as are relevant to it.
CCGs are clinically led membership organisations made up of general practices. The
members of the CCG have determined the governing arrangements for the CCG as
set out in its constitution, which was based on the Model Constitution Framework for
CCGs. The CCG undertook a thorough review of its constitution, in line with the NHS
CCG New Model Constitution, to enable the CCG to take on fully delegated primary
care commissioning with effect from 1 April 2021 and to align its constitution with the
other mid and south Essex CCGs in preparation for the development of an Integrated
Care System.
The revised constitution was approved by the Board at its meeting on 25 March 2021.
There are 39 member practices within Mid Essex CCG, serving a registered population
of 405,344 patients as of 1 April 2022. The practices were formed into nine Primary
Care Networks (PCNs) across mid Essex from 1 July 2019. Details of the PCNs are
shown in the table below:
Primary Care Network Number of
Practices
Registered Patient
Population as at
1 April 2022
Braintree
5
56,436
Colne Valley
6
55,015
Aegros
3
37,514
Witham and Maldon
4
37,496
Phoenix
3
45,895
Dengie and South Woodham Ferrers
7
48,951
Chelmer
4
40,504
Chelmsford West
3
41,082
Chelmsford City
4
42,451
Practices work together within their PCNs to collaborate on the effective provision of
primary care in their local areas and to engage in the commissioning of services on
behalf of their populations.
In some PCNs these working together arrangements are facilitated through the sharing
of workforce, sharing back-office functions, and collaborative working in certain
chosen clinical areas. Practices are gradually working towards developing
standardised policies, processes and agreed governance structures.
Governing Body (the Board)
The CCG’s constitution sets out the governance arrangements, roles and
responsibilities of the Board and its membership.
In February 2022 the CCG Board met in common with the other MSE CCG Boards and
agreed that they would continue to meet in common until the MSE Integrated Care
Board (ICB) was established. The Boards met in common on one occasion during
Page 39 of 72

Quarter 1 (Q1) of 2022/23 on 26 May 2022. The Boards also approved the MSE
System Financial Plan for submission to NHS England in June 2022 via an Emergency
Powers decision.
The Board meeting was broadcast via ‘MS Teams’ which enabled members of the
public to listen to discussions held and submit questions.
The decisions of the CCG Board were quorate whereby any member who was not
present at the meeting confirmed their support for the recommendations made.
Membership of the Board is set out on page 32 of the Members Report.
The Board undertakes an annual review of its effectiveness. The 2021/22 review
determined that it fulfilled its role effectively either all or most of the time and that there
is good engagement of members.
To support the Board in carrying out its duties effectively, committees reporting to the
Board are formally established. The current committee structure is set out below.
During Q1 of 2022/23 the five MSE CCGs held their main committee meetings in
common, these being Audit; Finance & Performance; Patient Safety & Quality (or
equivalent); Primary Care Commissioning; and Remuneration.
The Mid and South Essex Health and Care Partnership Board, which includes
representation from the CCG, local authorities, Healthwatch Essex, the voluntary
sector, Anglian Ruskin University and the MSE CCGs’ main providers, met in private
during Q1 of 2022/23.
In principle, each main committee submits its approved minutes to the Board
2
. The
main committees providing assurance to the Board are set out below.
Audit Committee
This Committee provides the CCG Board with an independent and objective view of the
CCG’s financial systems, financial information and compliance with laws, regulations
and directions governing the CCG insofar as they relate to finance, good corporate
governance, information governance, cyber-security, emergency planning, resilience
and response (EPRR), business continuity management (BCM) and the CCG’s
responsibility to act effectively, efficiently and economically.
The Audit Committee is chaired by the Lay Member (Governance) and Deputy Chair of
the CCG, John Gilham. As of 30 June 2022, the Committee’s other members were
Dr Elizabeth Towers, elected GP Board member, and Nathalie Wright, Lay Member
(Patient and Public Engagement).
During Quarter 1 of 2022/23, the Committee met in common with the other MSE CCG
Audit Committees on 2 occasions, plus 1 extraordinary meeting to review draft policies
2
where minutes had not been approved in time to submit to the final meeting of the CCG Boards, they
were submitted to the relevant committee of the Integrated Care Board.
Page 40 of 72
developed for the MSE ICB. Decisions were quorate in line with its Terms of Reference
(minimum of two core members) on all occasions. Where any member was not present
at the meeting their support for the recommendations made were submitted virtually.
During Q1 of 2022/23 the Audit Committee continued to focus upon ensuring the review
of the systems, policies, procedures, and processes fundamental to the governance of
the organisation. The committee also undertook a review of policies being developed
for the MSE ICB relating to areas within the committee’s remit and had oversight of the
governance of transition to the ICB.
The Committee has received assurance from internal audit of key systems and
processes and, in addition to routine reporting, has received updates on counter-fraud
initiatives and investigations and implementation of audit recommendations. The
Committee reviewed the CCG’s draft accounts and approved the final accounts and
management response to the auditor for 2021/22 on behalf of the Board.
The Committee also reviews the CCG’s risk register/Board Assurance Framework
(BAF) and associated risk management processes and procedures.
The Committee also received the minutes of the Primary Care Commissioning
Committee, the Patient Safety and Quality and the Finance & Performance Committee
meetings held in common with the other M&SE CCG committees.
In line with NHS England guidance on the management of Conflicts of Interest, the
Chair of the Audit Committee acts as the CCG’s Conflicts of Interest Guardian.
The Audit Committee Chair received assurance that the CCG was adhering to NHS
England mandatory guidance on the management of conflicts of interest via the annual
internal audit of conflicts of interest for 2021/22 which identified ‘reasonable’ assurance.
The requirement to submit quarterly returns to NHS England regarding the CCG’s
adherence to the mandatory guidance continued to be suspended during Q1 of
2022/23.
Remuneration Committee
The Remuneration and Terms of Service Committee is a committee of the CCG Board
with delegated responsibility for making recommendations to the Board on all aspects
of remuneration and terms of service of employees, including the Accountable Officer,
Directors, and Lay Members.
In addition, the Committee is responsible for making recommendations to the Board
concerning the remuneration and terms of service for Elected GP members and other
people who provide services to the CCG (all of whom are not employees of the CCG),
taking in to account any national or local guidance as appropriate, to ensure that
individuals are fairly rewarded for their contribution to the CCG.
As of 30 June 2022, the membership of the Remuneration Committee comprised of
three lay members. The committee is chaired by the Lay Member (Patient and Public
Engagement).
The Remuneration Committee met in common with the other MSE CCG Remuneration
Committees on 2 occasions. Decisions were quorate in line with its Terms of
Page 41 of 72
Reference (minimum of two core members) on all occasions. Where any member was
not present at the meeting their support for the recommendations made were submitted
virtually.
Patient Safety and Quality Committee
The Committee provides assurance regarding the safety and quality of services directly
commissioned by the CCG, i.e., acute, community, learning disability and mental health
services, as well as the quality of services within primary care and the care home
sector.
The committee also maintains oversight of safeguarding (adults and children) and
medicines optimisation.
The Committee was chaired by the Lay Member for Patient and Public Engagement
and its core decision making membership comprised a GP Representative (Vice Chair),
Director of Nursing and Quality and the NHS Alliance Director for Mid Essex.
Committee meetings were also attended by other senior managers with specific
responsibility for areas within the remit of the committee.
The committee met in common with the other MSE CCG Patient Safety and Quality
Committee’s on one occasion during Q1 of 2022/23 in May 2022, with a further ‘virtual’
meeting held in June 2022 to approve the CCG’s responses to the Quality Accounts of
its main providers.
The Committees meeting in common focused on arrangements to provide care for
patients diagnosed with COVID-19 within acute, community and care home settings,
the safety of staff and workforce capacity issues, and the effect that the pandemic was
having on patients requiring routine and elective care.
Other key areas discussed included arrangements for monitoring the quality of provider
contracts; review of NHS Patient Safety Updates; review of the Quality Accounts
2021/22 from the main Providers of services commissioned by the CCG; and agreeing
the CCGs’ responses to the Quality Accounts; serious incidents and never events;
review of arrangements for the implementation of the Patient Safety Incident Response
Framework; update on Special Educational Needs and Disabilities services; updates on
Learning Disabilities Mortality Review (LeDeR) Programme; System Quality Strategy;
Infection Prevention and Control Strategy; approval of policies; all age continuing care;
personal health budgets; review of patient safety and quality risks; quality and equality
impact assessments; complaints and a review of any virtual decisions taken since the
last committee meeting.
Decisions were quorate in line with its Terms of Reference on all occasions. Where any
member was not present at the meeting their support for the recommendations made
were submitted virtually.
Finance and Performance Committee
This Committee scrutinises and provides the CCG Board with assurance on the delivery
of the CCG’s remit in respect of the CCG’s overall financial position (including running
costs) and for service performance for commissioned services not delegated to the JC.
Page 42 of 72
The Committee also maintains local oversight of information management and
technology, estates developments and the Savings Programme Board’s scrutiny and
challenge role to ensure the delivery of the CCG’s programme of financial savings. The
Committee acts as a point of approval for major changes to existing projects and plans,
where these are based on considerations related to the achievement of financial or
other benefits. The Committee also assesses whether there is continued business
justification for existing projects and programmes where the financial or other benefits
have changed.
At the start of the year the Committee was chaired by the Lay Member (Governance)
and its core membership comprised a GP Representative (Vice Chair), Executive Chief
Finance Officer, NHS Alliance Director for Mid Essex (or nominated deputy), and
Executive Director of Nursing and Quality (or nominated deputy nurse).
During Q1 of 2022/23 it met on two occasions in common with the other MSE CCG
Finance & Performance Committees to review finance and performance issues across
all health care services, including those ordinarily within the remit of the Mid and South
Essex STP CCG Joint Commissioning Committee (JC).
The quoracy arrangements for meetings held in common with the other CCG
committees, mirrored those described under the ‘Patient Safety and Quality Committee’
section.
During Q1 of 2022/23 the Committee particularly focused upon review of finance and
performance risks, receipt of monthly finance reports, Joint Committee finance
reports, Elective Recovery Framework updates, Hospital Discharge Programme,
contract planning, awards and procurement decisions, performance reports from
System Oversight and Assurance Group (SOAG), Adult Mental Health
Transformation Plan contracts, system financial sustainability, 2022/23 Business Plan
and CCG budgets, approval of terms of reference/frequency of meetings, receipt of
System Finance Leaders Group (SFLG) minutes.
Mid Essex Alliance
The aim of the Mid Essex Alliance is to bring all key partners from across mid Essex
together to provide the localism needed within the Mid and South Essex system to
create opportunities for people to live well in mid Essex.
Its membership comprises Director level representation from the ICB mid Essex place
team, PCN Clinical Directors, the Clinical Alliance Director, Essex County Council and
Braintree, Chelmsford and Maldon District Councils, Provide Community Interest
Company, Essex Partnership University NHSFT, North East London NHSFT, Mid and
South Essex Foundation Trust, Farleigh Hospice, Chelmsford and Maldon CVS,
Community 360 and Virgin Healthcare.
The Alliance meets monthly with good representation from all partners.
The Alliance has been involved in a three month Place Development Programme, led
by NHS England, to support the development of priorities and plans, governance and
the Alliance approach to population health management for 2022/23 and beyond. This
was a successful programme which has helped to develop a number of actions that the
Alliance now needs to take forwards.
Page 43 of 72
Primary Care Commissioning Committee
This Committee is chaired by the Lay Member for Patient and Public Engagement.
During Q1 of 2022/23 two meetings were held in common with the other MSE CCGs
Primary Care Commissioning Committees.
The Committee focused on contractual updates/breaches/requests for contractual
changes from general practices; local contract decisions; GP primary care quality and
safety reports; budget reports; information technology and digital updates; estates
issues; primary care workforce; and review of primary care risks.
Better Care Fund (including Improved Better Care Fund) Governance
A Better Care Fund (BCF) Partnership Board meets to fulfil the governance
requirements with Essex County Council.
In line with the terms of the Section 75 Better Care Fund Agreement, decision-
making relating to the BCF is delegated to two nominated representatives of the
CCG and two representatives of Essex County Council. As national guidance had
not been received in relation to the 2022/23 BCF utilisation of the BCF funds was in
line with the latest Section 75 Agreement and reporting for the period focused upon
expenditure on the approved services and monitoring against previously agreed
performance targets.
UK Corporate Governance Code
The CCG is not required to comply with the UK Code of Corporate Governance.
However, we have reported on our Corporate Governance arrangements by drawing
upon best practice available, including those aspects of the UK Corporate Governance
Code we consider to be relevant to the CCG and best practice.
As part of its annual review of effectiveness for 2021/22 the CCG Board undertook an
assessment which encompassed the relevant principles of the UK Corporate
Governance Code.
The Board concluded from this assessment that it was generally following best practice
in relation to providing effective leadership, having an appropriate balance of skills,
experience, independence, and knowledge to enable Board members to discharge their
duties and responsibilities effectively, presenting a balanced and understandable
assessment of the CCG’s position in its financial and other reporting and ensuring that
remuneration is set appropriately.
A review of Board effectiveness was not undertaken during Q1 of 2022/23 as the CCG
was dis-established on 30 June 2022.
Discharge of Statutory Functions
In light of the recommendations of the 2013 Harris Review, the clinical commissioning
group has reviewed all of the statutory duties and powers conferred on it by the
National Health Service Act 2006 (as amended) and other associated legislative and
regulations. As a result, I can confirm that the clinical commissioning group is clear
about the legislative requirements associated with each of the statutory functions for
Page 44 of 72
which it is responsible, including any restrictions on delegation of those functions. The
CCG’s current Scheme of Reservation and Delegation (SoRD) was approved by the
Board in March 2021. The CCG worked with the other MSE CCGs to develop a new
SoRD for the MSE ICB.
Risk management arrangements and effectiveness
The CCG is committed to ensuring that risk management forms an integral part of its
philosophy, practices and business plans, rather than viewed or practised as a separate
programme, and that responsibility for implementation is accepted at all levels of the
CCG.
An aligned MSE CCG Risk Management Policy, which encompasses both clinical and
non-clinical risks and the CCGs’ agreed risk appetite statement, was approved by all
MSE CCGs in November 2021. The Policy is based on the Australia/New Zealand risk
management model and sets out the risk management system, supporting processes
and reporting arrangements which aim to protect patients, the public, staff and the
CCG’s assets and reputation.
The overarching M&SE Board Assurance Framework (BAF) originally implemented in
June 2020, has been further developed. Risks are mapped against the MSE CCGs
common strategic objectives and key workstreams, these being:
• Cancer and End of Life
• Children and Young People
• Community
• Digital and Business Intelligence
• Estates
• Finance
• Health Inequalities
• Integrated Care System
• Maternity
• Medicines Optimisation
• Mental Health and Learning Disability
• People
• Planned Care
• Population Health Management
• Primary Care
• Stewardship
• Urgent Emergency Care
• Vaccination
The risk appetite statement assists managers to identify when risk levels are tolerable
or where further action is required to reduce risk ratings to an acceptable level. The
BAF is reviewed at each Part I Board meeting.
Capacity to Handle Risk
During Q1 of 2022/2 the CCG had the following arrangements in place:
Page 45 of 72
Page 46 of 72
• Clear ownership of risks, with responsible Directors and lead officers identified,
with escalation arrangements in place to the Board.
• A Board Assurance Framework within which the latest updates from lead officers
were recorded and reported to relevant committees and the Board.
• Recording and investigation processes for incidents, including identification of
learning.
• Triangulation of learning from incidents, complaints, and claims (should they
arise) as a standing item on the agenda of the Patient Safety and Quality
Committee.
• Monitoring of completion of Equality and Health Inequality Impact Assessments,
Quality Impact Assessments and Privacy Impact Assessments
• Regular review of anti-fraud, bribery, and security arrangements by the Audit
Committee.
• Emergency Planning, Resilience and Response and Business Continuity
Management Policies and Procedures.
The CCG’s Whistleblowing Policy and arrangements, including the appointment of a
Freedom To Speak Up Guardian, also support risk management by providing a
framework for employees to raise concerns, in line with the Public Interest Disclosure
Act 1998, without the perception of being disloyal to colleagues, managers or the
organisation.
The CCG is committed to identifying the underlying or root causes of incidents, claims
and complaints, and the principal objective is to identify ‘system failures’, rather than
focusing on individual failures.
Stakeholders, including staff, patients and the public have been involved in the risk
management process, for example by ensuring that relevant staff were identified to
input into any risk assessments in their function or area of work; that CCG staff and
contractors were made aware of agreed risk reporting procedures including risks
associated with COVID-19; that contracts clearly stated the responsibilities of
contracted personnel with regard to risk identification, reduction, mitigation and
reporting; that feedback on risk issues was encouraged via the CCG’s complaints and
enquiries services and through its public engagement and consultation mechanisms,
e.g. patient stories at Board meetings, engagement with the public and other
stakeholders on future plans for services.
The effectiveness of these risk management arrangements is summarised under the
‘Review of the Effectiveness of Governance, Risk Management and Internal Control’
section, which includes the monitoring, review and management of the Assurance
Framework by the Audit Committee and Board.
Prevention of Risk
The application of this framework enables the prevention of risk through:
• Commitment to identifying the underlying or root causes of incidents,
complaints, and claims (should they arise)
• Promoting an open, just, and non-punitive culture
• Driving an ongoing information and education programme which empowers
and supports Board members and staff in the risk management process
generally and in relation to specific areas of risk
• All staff being familiar with the Anti-fraud, Anti-bribery and Security policies’
terms through promotion and training and the issuing of fraud alerts, with the
help of counter-fraud services
• All staff being familiar with the terms of the Conflicts of Interest, Gifts and
Hospitality and Standards of Conduct Policies.
• Registers of Interests being produced for Board and Committee meetings and
those Sub-committees with decision-making powers, or capacity to influence
decisions made by the CCG, so that the relevant Chair can ensure that potential
conflicts are managed appropriately.
Other sources of assurance
Internal Control Framework
A system of internal control is the set of processes and procedures in place in the
CCG to ensure it delivers its policies, aims and objectives. It is designed to identify
and prioritise the risks, to evaluate the likelihood of those risks being realised and the
impact should they be realised, and to manage them efficiently, effectively, and
economically.
The system of internal control allows risk to be managed to a reasonable level
rather than eliminating all risk; it can therefore only provide reasonable and not
absolute assurance of effectiveness.
The system of control in place is set out within the Board, Committee and Risk
Management sections of this statement.
Financial Arrangements
The CCG’s key financial systems are operated by third party providers. The CCG
Finance team oversee the operation of internal financial control arrangements and the
dissemination of good financial management and professional standards. The CCG’s
financial arrangements are assessed annually by external parties as part of the internal
and external audit functions.
The Finance and Performance Committee, which met in common with the other M&SE
CCGs during Q1 of 2022/23, exercises the Board’s functions in respect of the oversight
of financial control.
Risk Assessment
Risk assessments have been carried for each workstream identified on page 45 above.
Each risk recorded on the BAF is scored on the basis of inherent and residual risk.
Continued efforts are made to strengthen controls where residual risk scores remain
above the CCG’s Risk Appetite.
The CCG also undertakes other risk assessments, for example, health and safety/fire
workplace risk assessment of its premises and COVID-19 risk assessment to ensure
that its premises are COVID-19 secure. These risk assessments have associated
Page 47 of 72
action plans, policies, and procedures to ensure that risks identified are managed on an
ongoing basis.
Annual Audit of Conflicts of Interest Management
The revised statutory guidance on managing conflicts of interest for CCGs (published
June 2017) requires CCGs to undertake an annual internal audit of conflicts of interest
management.
To support CCGs to undertake this task, NHS England has published a template audit
framework. The annual internal audit of conflicts of interest 2021/22, which was
undertaken as part of the wider audit of the CCG’s risk management and governance
arrangements, identified ‘reasonable’ assurance.
Data Quality
In 2020/21 and 2021/22, when the annual contracting round coincided with peak
periods of the pandemic, the requirement for signed contracts with NHS Trusts and
NHS Foundation Trusts was relaxed. However, in 2022/23, as we revert to more normal
working arrangements, it is important, from a governance perspective, that properly
documented contracts are put in place in all cases.
The NHS Standard Contract (SC28) includes a specific requirement for the provider to
use all reasonable endeavours to optimise its performance under NHS Digital’s Data
Quality Maturity Index (DQMI), where applicable, demonstrating its progress through
implementation of a DQIP or other appropriate mean. The DQMI currently covers the
national datasets for admitted patient care, A&E, community services, diagnostic
imaging, IAPT, mental health, maternity, and outpatients.
Data Quality Improvement Plans (DQIPs) allow the commissioner and the provider to
agree a local plan to improve the capture, quality, and flow of data to meet the
requirements of the Information Schedule (6A) and to support both the commissioning
and contract management processes, generally targeting areas of particular concern, or
in relation to new data capture as a result of service transformation. Completion of a
DQIP is not mandatory for each contract, however in 2022/23 there are a number of
recommended DQIPs depending on the nature of the service provided. These include
providers of maternity services (to improve the accuracy and completeness of maternity
services data), providers of mental health and LD services (focussing on mental health
clinically led review of standards), providers of inpatient services (to record diagnoses
of LD and autism), and providers of community services (to improve the accuracy and
completeness of Community Dataset submissions).
Commissioners are able to use DQIPs (where agreed) to address data quality issues
highlighted through direct reporting or through the nationally available NHS Digital’s
Data Quality Maturity Index (DQMI).
Information Governance
The NHS Information Governance (IG) Framework sets the processes and procedures
by which the NHS handles information about patients and employees, in particular,
personal identifiable information. The NHS Information Governance Framework is
supported by a data security and protection toolkit and the annual submission process
Page 48 of 72
provides assurances to the CCG, other organisations and to individuals that personal
information is dealt with legally, securely, efficiently, and effectively.
We place high importance on ensuring there are robust information governance
systems and processes in place to help protect patient and corporate information. We
have established an information governance management framework and have
developed information governance processes and procedures in line with the Data
Security and Protection Toolkit. We have ensured all staff undertake annual information
governance training and have implemented a staff information governance handbook to
ensure members of staff are aware of their information governance roles and
responsibilities, and how to access information or assistance.
There are processes in place for incident reporting and investigation of serious
incidents. No serious incidents requiring investigation involving personal data were
reported to the Information Commissioner in Q1 of 2022/23.
The CCG has nominated information asset owners who have completed the new data
flow mapping and information asset registers to ensure compliance with the General
Data Protection Regulations (GDPR). This was undertaken with support from the IG
Team to ensure consistency of approach.
The CCG submitted a “Standards Met” Data Security and Protection Toolkit for 2021/22
on 22 June 2022.
Business Critical Models
The CCG supports the principles of the Macpherson Report and is committed to
embedding best practice in relation to quality assuring our prioritised business critical
models and other functions.
The Essex CCGs each have a Business Continuity Plan supported by an overarching
Essex-wide Business Continuity Policy, all of which have been approved by the CCGs'
Audit Committee. The documents are updated when a material change occurs, and
usually a comprehensive annual review takes place each year, although during the last
two years events have curtailed this process.
A memorandum of understanding has been signed by the Essex CCGs which sets out
the intentions of the CCGs to provide mutual aid and assistance to each other during a
business continuity incident which cannot be managed internally within each CCG’s
own business continuity arrangements, and which involves one or more of the following:
critical loss of key staff, temporary loss of premises or loss of a significant amount of IT
hardware. The CCGs have worked jointly since March 2020 on the response to the
Covid-19 pandemic.
Since March 2020, the CCGs have reviewed, tested, and updated their internal
business continuity arrangements as a result of the COVID-19 pandemic and continued
to update these throughout Q1 of 2022/23 in line with operational and Government
requirements and have developed new policies and procedures for the MSE ICB.
Page 49 of 72
Third party assurances
The CCG relies on a number of third-party providers which are listed below, together
with information on how assurance is received from each provider, the effectiveness of
these arrangements and whether any improvements are planned in the future.
The CCG relies on a third-party provider for payroll and pension services. This service
is provided by Whittington Health NHS Trust which is based in North London. The CCG
continues in a positive relationship with Whittington Health and regular virtual MS
Teams meetings are held between Whittington and the HR Managers at the CCG.
Human Resources transactional, recruitment and workforce services are now provided
in house directly by the CCG. From 1 July 2021, Occupational Health support has been
provided by Optima Health.
The CCG retains the services of a procurement expert company (Attain) to ensure
probity during procurement processes. The Finance & Performance Committee
receives procurement reports at each meeting and a register of procurement decisions,
which is published on the CCG’s public-facing website, is reviewed by the Audit
Committee to ensure rigour is being applied.
The MSE CCGs hold a monthly contract review meeting with Arden and Greater East
Midlands (AGEM) Central Support Unit (CSU) to monitor all aspects of the contract and
review performance against service level agreements and key performance indicators.
This includes extended services such as back-ups and business continuity planning.
Exceptions or escalations are reported to the Primary Care Digital Board. The CCGs
receive copies of all NHS Digital CareCert alerts and confirmation when AGEM has
updated against them.
Control Issues
EPUT have developed a Quality Strategy ‘Safety First, Safety Always’ which aims to
ensure that EPUT provide safe and high-quality care. The Essex mental health system
is one of the first areas in the country to roll out the new Patient Safety Incident
Response Framework. The CCG continues to monitor safety via the CQRG
mechanism. In September 2020 the CCGs began a joint pan Essex review (known as
the Taskforce) of the systems and processes within CCGs for the commissioning of
mental health services as provided by Essex Partnership University NHS Trust. The
Mental Health Taskforce has completed its review and the final report has been
produced. The ongoing work to fully deliver the taskforce recommendations are being
taken forward and overseen by the Mental Health Partnership Board to ensure that
delivery and progress is maintained going forward.
Review of economy, efficiency & effectiveness of the use of resources
As described in the Financial Overview section, many of the amendments made to the
financial regime during 2021/22 remained in place during Q1 2022/23 in response to
the ongoing challenges of the Covid-19 pandemic. The CCG reported a breakeven
position at the end of Q1 2022/23.
Page 50 of 72
The MSE CCGs’ Finance and Performance Committees in common (F&P CiC) and the
Board have each received regular financial reporting and had the opportunity for
detailed review of the CCG’s position.
The F&P CiC continued to monitor the CCG’s procurement and planning arrangements
in order to ensure value for money from commissioned services.
The CCG’s Q1 2022/23 running (management) costs were within nationally permitted
expenditure limits.
The Internal Auditor has reviewed the CCG’s financial systems and processes,
including the arrangements for financial reporting, and confirmed that the CCG has
reasonable arrangements in place. The external auditor’s comments on our
arrangements for securing economy, efficiency, and effectiveness in use of resources
in Q1 2022/23 are included in their report immediately preceding the Annual Accounts
(see page 100 onwards).
Delegation of functions
Acute services are commissioned by a central Mid and South Essex Acute
Commissioning Team, which is hosted by Mid Essex CCG.
Acute adult and older adult mental health services are commissioned by a central
mental health commissioning team hosted for Mid and South Essex by Thurrock CCG.
The individual placements team, which commissions placements for individuals with
Section 117 after-care rights as well as specialist placements for children and for adults
requiring tertiary care, is hosted by North East Essex CCG, which provides this function
on a pan-Essex basis.
Early intervention (Tier 2- Local Authority) and Specialist Community Mental Health
Services (Tier 3- CCGs) for Children is known as Southend, Essex and Thurrock
Children and Adolescent Mental Health Services (SET CAMHS). This has been
procured on a pan-Essex basis with a Commissioning Collaborative Agreement in place
for all 10 partner organisations. West Essex CCG is the Host commissioner for this
service. Children’s in-patient services continue to be commissioned by NHS England
and managed through the establishment of the Provider Collaborative for Children’s
Mental Health.
Learning Disability (LD) services are commissioned by Essex County Council, with
Castle Point and Rochford and Southend CCGs leading on this for health for Mid and
South Essex.
In common with other CCGs, the Executive Director of Nursing and Quality Chief Nurse
was a member of the Quality Surveillance Group which allows quality intelligence to be
shared across Essex with other commissioners and with the CQC.
No adverse information has been received from third party assurance reports relating to
West Essex’s host commissioner role for EWMHS or North East Essex CCG’s host
commissioner role for section 117 services.
Page 51 of 72

Page 52 of 72
Counter fraud arrangements
An accredited Local Counter Fraud Specialist (LCFS), who is an employee of the
CCG’s internal auditors, is contracted to undertake counter fraud work proportionate to
identified risks. The Audit Committee receives an update from the LCFS regarding any
counter-fraud initiatives or investigations at each meeting and reports progress and
outcomes against each of the Government Counter Fraud Functional Standards
GovS 013.
There is executive support and direction from the Chief Finance Officer for a
proportionate proactive work plan to address identified risks. The Chief Finance Officer
is the identified member of the executive team named within the Anti-Fraud, Bribery and
Corruption Policy who is proactively and demonstrably responsible for tackling fraud,
bribery and corruption.
The CCG is committed to robustly investigating all reports of fraud, bribery and
corruption and will seek to recover lost NHS funds where proportionate and necessary.
At the end of the financial year, the CCG submits a self-assessment to the NHS
Counter Fraud Authority against the Government Counter Fraud Functional Standards.
The Chief Finance Officer and Chair of the Audit Committee authorise the assessment
prior to submission.
Head of Internal Audit Opinion
Following completion of the planned audit work for the financial year for the clinical
commissioning group, the Head of Internal Audit issued an independent and objective
opinion on the adequacy and effectiveness of the clinical commissioning group’s
system of risk management, governance, and internal control.
During 2022/23 Internal Audit issued the following audit reports:
Assignment Assurance Opinion
Review to confirm that governance processes
continued to operate during Q1 of 2022/23
Reasonable
Part 1 - Review of ‘due diligence’ processes
established in preparedness for transition to the
ICB
Reasonable
Part 2 - Review of ‘due diligence’ processes
established in preparedness for transition to the
ICB
Reasonable
Action plans have been established to address all recommendations made in internal
audit reports. Regular updates on progress are submitted to Audit Committee.
Review of the effectiveness of governance, risk management and internal control
My review of the effectiveness of the system of internal control is informed by the work
of the internal auditors, executive managers and clinical leads within the clinical
commissioning group and the Acute Commissioning Team who have responsibility for
the development and maintenance of the internal control framework. I have drawn on
performance information available to me. My review is also informed by comments
made by the external auditors in their annual audit letter and other reports.
Our assurance framework provides me with evidence that the effectiveness of controls
that manage risks to the clinical commissioning group achieving its principal objectives
have been reviewed.
I have been advised on the implications of the result of this review by:
• The Board
• Audit Committee
• Remuneration Committee
• Quality and Governance Committee
• Finance and Performance Committee
• Primary Care Commissioning Committee
• The Joint Committee
• Internal audit
• Other explicit review/assurance mechanisms.
Conclusion
I concur with the Head of Internal Audit Opinion that during Q1 2022/23 there has been
a generally sound system of internal control, designed to meet the organisation’s
objectives, and that controls have been generally applied consistently.
Action plans to implement any outstanding recommendations from audits are in place
and will continue to be monitored during the 2022/23 financial year.
I confirm that there are no risks which may affect the CCG’s Licence or serious lapses
in control.
Anthony McKeever
Accountable Officer
26 June 2023
Page 53 of 72
REMUNERATION AND STAFF REPORT
Remuneration Report
For 2022/23 the membership of the Remuneration Committee was as follows:
• Nathalie Wright, Lay Member (Patient and Public Involvement) - Chair
• John Gilham, Lay Member (Governance)
• Pauline Stratford – Third Lay Member
This committee met in common with the other 4 MSE CCGs on 2 occasions during Q1
2022/23 both meetings were quorate.
HR and remuneration advice was provided by Human Resources and the committee
was informed by local and national guidance on remuneration matters.
Policy on remuneration of senior managers
Senior managers are subject to Agenda for Change terms and conditions, with the
exception of those roles which are subject to the VSM (Very Senior Managers)
framework. The salaries of governing body members are determined by remuneration
committee with national and local guidance (provided by the Chief Finance Officer and
Interim Director of Human Resources) being considered in all decisions.
Remuneration of Very Senior Managers
The Accountable Officer/CEO salary is set within national salary boundaries for the
AO/CEO of a CCG/ICB. The determination within this broad salary boundary is set with
NHS England and the CCG Remuneration Committee.
Senior Manager’s Performance Related Pay
The performance of all staff (including the Accountable Officer, directors, and senior
managers) is monitored and assessed through the use of a robust appraisal system. A
formal appraisal review is undertaken at least annually.
Agenda for Change contracts do not contain provision for performance-related
remuneration beyond the element introduced in 2018 for bands 8c, 8d and 9.
Specifically, in the year after an employee has reached the top of any of those bands,
subject to performance the employee will retain their basic salary, or their salary will be
reduced by five per cent or 10 per cent. The employee will be able to restore their
salary at the end of the following year by achieving agreed levels of performance.
Under the VSM pay framework, there is the potential for performance-related pay under
the terms and conditions of the contract. No proportion of remuneration for any staff
member has been subject to performance conditions at the CCG during the accounting
period.
Page 54 of 72

Page 55 of 72
Senior manager remuneration (including salary and pension entitlements)
CCG Remuneration Reports 2022/23 (April 22 to June 22)
This Clinical Commissioning Group Remuneration Report for 2022-23 is shown in two
sections, representing the Salary and Allowances and Pension entitlements of the
senior leadership of the CCG.
CCG Salaries and Allowances Table:
This includes the Clinical Commissioning Group specific Remuneration Report table of
directors and senior managers.
CCG Pension Table:
This includes the Clinical Commissioning Group specific Pension entitlements of
directors and senior manager.
For the April 22 to June 22 period the CCGs operated a Board Meeting in Common and
did not operate the Joint Committee.

Page 56 of 72
Salaries and allowances (SUBJECT TO AUDIT)
Name and Title
Note
Date served
2022/23 (April 22 to June 22) 2021/22
Commenced Ceased
Salary
(bands
of
£5,000)
Expense
Payments
(taxable)
(total to
nearest
£100)
Other
Remunerati
on (bands
of £5,000)
All Pension
Related
Benefits
(bands of
£2,500)
1
Total
(bands of
£5,000)
Salary
(bands of
£5,000)
Expense
Payments
(taxable)
(total to
nearest
£100)
Other
Remuner
ation
(bands of
£5,000)
All Pension
Related
Benefits
(bands of
£2,500)
Total
(bands of
£5,000)
£000
£
£000
£000
£000
£000
£
£000
£000
£000
Anthony McKeever
Joint Accountable
Officer – Joint
Executive Team
2 03-Oct-20 30-Jun-22 0 0 0 0 0 50-55 0 0 7.5-10 60-65
Mark Barker
Joint Chief Finance
Officer - Joint
Executive Team
2 & 8 01-Jan-21 30-Jun-22 0 0 0 0 0 40-45 0 0 0 40-45
Rachel Hearn
Executive Director of
Nursing and Quality -
Joint Executive Team
2 02-Nov-20 30-Jun-22 30-35 0 0 25-27.5 55-60 40-45 0 0 62.5-65 105-110
Daniel Doherty
NHS Alliance Director,
Mid Essex - Joint
Executive Team and
Deputy Accountable
Officer
3 02-Nov-20 30-Jun-22 30-35 0 0 10-12.5 40-45 125-130 0 0 72.5-75 195-200
John Gilham
Lay Member,
Governance and Audit
Chair
01-Jul-18 30-Jun-22 0-5 0 0 0 0-5 15-20 0 0 0 15-20

Page 57 of 72
Nathalie Wright
Lay Member, Patient &
Public Participation
01-Apr-18 30-Jun-22 0-5 0 0 0 0-5 10-15 0 0 0 10-15
Pauline Stratford
Lay Member
6 01-Aug-21 30-Jun-22 0 0 0 0 0 0-5 0 0 0 0-5
Dr Anna Davey
Elected GP –
Governing Body
Member and
CCG Chair (Clinical)
5 01-Apr-18
01-Oct-18
30-Jun-22
30-Jun-22
15-20 0 0 0 15-20 65-70 0 0 0 65-70
Dr Elizabeth Towers
Elected GP -
Governing Body
Member
4 01-Apr-15 30-Jun-22 15-20 0 0 15-20 65-70 0 0 0 65-70
Dr Julie McGeachy
Elected GP –
Governing Body
Member
5 01-Apr-18 30-Jun-22 0-5 0 0 0 0-5 10-15 0 0 0 10-15
Dr Fatai Salau
Elected GP –
Governing Body
Member
5 01-Apr-18 30-Jun-22 0-5 0 0 0 0-5 10-15 0 0 0 10-15
Dr Julia Hale
Secondary Care
Consultant
7 01-Aug-21 30-Jun-22 0 0 0 0 0 0-5 0 0 0 0-5
Notes:
1 The pension-related benefit figures do not represent cash payments made to an individual's pension provider. The quoted figures
provided by NHS Pensions Agency are an estimate of the increase in the accrued pension over their estimated pensionable life.
Each organisation reports a disclosure value appropriate to the length of time the senior manager was employed by their
organisation.
2 Anthony McKeever, employed by Basildon and Brentwood CCG, Mark Barker, employed by Castle Point & Rochford CCG, and
Rachel Hearn, employed by Mid Essex CCG are members of the Joint Executive Team, a single executive body covering the five
CCGs in mid and south Essex. Their remuneration is shared across the five CCGs, and our share is shown in the table above.
The total remuneration (inclusive of pension benefits and taxable expense payments) for Rachel Hearn, was in the range £30k-
£35k, for Mark Barker in the range £35k-£40k, and for Anthony McKeever in the range £65k-£70k.
3 Daniel Doherty is a member of the Joint Executive Team, as an NHS Alliance Director supporting the mid Essex locality and
leading on Community services across the five CCGs in mid and south Essex. Daniel Doherty’s total remuneration is shown in
the Salaries and Allowances table above.
4 The Salary Band for Elizabeth Towers includes work undertaken for the CCG under separate contracts. These are: Macmillan
GP Facilitator and Clinical Lead - Rapid Diagnostic Centre initiative. The Macmillan GP Facilitator role is partly funded by
Macmillan Cancer Support, with the Clinical Lead – Rapid Diagnostic Centre being funded by NHS England. The remuneration
band for this additional work was £15k-£20k.
5 Drs Anna Davey, Julie McGeachy and Fatai Salau, GP Elected members of the Governing Body, are employed as ‘Off Payroll
Workers’ but processed through the CCG’s payroll to ensure the statutory HMRC deductions are made. The salary disclosure
includes employer pension contributions (where applicable). They are not reported in the ‘Off-Payroll’ section of the
Remuneration Report.
6 Pauline Stratford, Lay Member is also a member of NHS Southend CCG, NHS Castle Point & Rochford CCG and NHS Thurrock
CCG Boards. Her salary was not recharged to Mid Essex CCG in the period. Her total remuneration, paid by Castle Point &
Rochford CCG, was in the range £0k-£5k.
7 Dr Julia Hale, Secondary Care Specialist, is also a member of NHS Basildon and Brentwood CCG Board. The remuneration
shown above is the total remuneration as none was recharged to NHS Basildon & Brentwood CCG in the period.
8 The pension figures for staff who are also included in CCG remuneration reports are shown in full in their employing CCG's
remuneration report and have not been apportioned to more than one organisation.
Dr Maggie Pacini, Consultant in Public Health and Councillor Mike Steel attend the board in a non-voting capacity as Essex County
Council representatives. No remuneration is paid to Essex County Council, and they are therefore not included in the above table.
Performance pay and bonuses, and Long-Term performance pay and bonuses, are not paid by the CCG.
Page 58 of 72
Page 59 of 72
Pension benefits as at 30 June 2022 (SUBJECT TO AUDIT)
Name and
Title
(a)
Real
increase
in
pension
at
pension
age
(bands of
£2,500)
(b)
Real
increase in
pension
lump sum
at pension
age
(bands of
£2,500)
(c)
Total
accrued
pension at
pension
age at 30
June 2022
(bands of
£5,000)
(d)
Lump sum
at pension
age related
to accrued
pension at
30 June
2022
(bands of
£5,000)
(e)
Cash
Equivalent
Transfer
Value at 1
April 2021
(f)
R
eal
Increase in
Cash
Equivalent
Transfer
Value
(g)
C
ash
Equivalen
t Transfer
Value at
30 June
2022
(h)
Employers
Contribution to
partnership pension
£000 £000 £000 £000 £000 £000 £000 £000
Rachel Hearn
Executive Director
of Nursing and
Quality – Joint
Executive Team
0-2.5 0 35-40 65-70 553 19 594 0
Daniel Doherty
NHS Alliance
Director, Mid
Essex – Joint
Executive Team
and
Deputy
Accountable
Officer
0-2.5 0 35-40 60-65 524 6 551 0
As non-executive directors do not receive pensionable remuneration, there will be no
entries in respect of pensions for their non-executive director’s role.
Cash equivalent transfer values
CETV figures are calculated using the guidance on discount rates for calculating
unfunded public service pension contribution rates that was extant at 31 March 2023.
HM Treasury published updated guidance on 27 April 2023; this guidance will be used
in the calculation of 2023 to 24 CETV figures.
A Cash Equivalent Transfer Value (CETV) is the actuarially assessed capital value of
the pension scheme benefits accrued by a member at a particular point in time.
The benefits valued are the member’s accrued benefits and any contingent spouse’s (or
other allowable beneficiary’s) pension payable from the scheme. CETVs are calculated
in accordance with SI 2008 No.1050 Occupational Pension Schemes (Transfer Values)
Regulations 2008.
The CETV figures and the other pension details include the value of any pension
benefits in another scheme or arrangement which the individual has transferred to the
NHS pension scheme. The pension figures shown relate to the benefits that the
individual has accrued as a consequence of their total membership of the pension
scheme, not just their service in a senior capacity to which disclosure is required. They
also include any additional pension benefit accrued to the member as a result of their
purchasing additional years of pension service in the scheme at their own cost.
Real increase in CETV
This reflects the increase in CETV effectively funded by the employer.
It does not include the increase in accrued pension due to inflation or contributions paid
by the employee (including the value of any benefits transferred from another pension
scheme or arrangement)
The pension-related benefit figures quoted do not represent cash payments made to an
individual's pension provider. The quoted figures provided by NHS Pensions Agency
are an estimation of the increase in the accrued pension over their estimated
pensionable life. Where an individual joins the pension fund after a significant gap, this
can result in a higher estimate than would normally be expected. However, the pension
benefit figures are expected to return to normal levels in the second year of disclosure.
NHS Pensions are using pension and lump sum data from their systems without any
adjustment for a potential future legal remedy required as a result of the McCloud
judgement. (This is a legal case concerning age discrimination over the manner in
which UK public service pension schemes introduced a CARE benefit design in 2015
for all but the oldest members who retained a Final Salary design). We believe this
approach is appropriate given that there is still considerable uncertainty on how the
affected benefits within the new NHS 2015 Scheme would be adjusted in future as a
result of these legal proceedings.
Page 60 of 72

Page 61 of 72
Compensation on early retirement or for loss of office
There have been 0 compensation payments on early retirement or for loss of office.
Payments to past directors
There have been 0 payments to past directors.
Fair Pay Disclosure (SUBJECT TO AUDIT)
Percentage Change in Remuneration of Highest Paid Director
% Change from previous
financial year in Salary
and Allowances
% Change from previous
financial year in
Performance Pay and
Bonuses
The percentage change
from the previous financial
year in respect of the
highest paid director
+4.1% N/A*
The average percentage
change from the previous
financial year in respect of
employees of the entity,
taken as a whole.
+6.3% N/A*
*No Performance Pay and Bonus payments are made by the CCG.

Pay Ratio Information
Reporting bodies are required to disclose the relationship between the remuneration of
the highest-paid director / member in their organisation against the 25th percentile,
median and 75th percentile of remuneration of the organisation’s workforce. Total
remuneration is further broken down to show the relationship between the highest paid
director's salary component of their total remuneration against the 25th percentile,
median and 75th percentile of salary components of the organisation’s workforce.
The banded remuneration of the highest paid director/member in Mid Essex CCG in the
financial period April to June 2022 was £125k-130k (+4% against 2021-22: £120k-125k)
and the relationship to the remuneration of the organisation's workforce is disclosed in
the below table.
Pay Ratio information table
2022-23 25th percentile Median 75th percentile
Total remuneration (£) £27,361 £42,446 £56,625
*Salary component of total
remuneration (£)
£27,361 £42,446 £56,625
Pay ratio information 4.7:1 3.0:1 2.3:1
2021-22
Total remuneration (£) £26,721 £41,890 £54,904
*Salary component of total
remuneration (£)
£26,721 £41,890 £54,904
Pay ratio information 4.8:1 3.0:1 2.3:1
*No Performance Pay and Bonus Payments are paid by the CCG, therefore both Salary
component and Total Remuneration are the same.
In the period April – June 2022, 1 (2021/22, 0) employee received remuneration in
excess of the highest-paid director/member.
As at 30 June 2022, remuneration ranged from £5k to £140k (2021/22: £3k to 125k)
based on annualised, full-time equivalent remuneration of all staff (including temporary
and agency staff)
Page 62 of 72
P
age 63 of 72
Policy on the duration of contracts, notice periods and termination payments
The duration of contracts is determined by the duration of the roles and responsibilities
to be undertaken. The contracts of the Accountable Officer, directors and other CCG
staff are permanent unless applicable to a time-limited project or funding, in which case
contracts will be offered on a fixed-term.
The notice period applying to the Joint Accountable Officer is six months. For directors
and other senior managers, the notice period is three months. Any termination
payments would be in accordance with relevant contractual, legislative and HMRC
requirements.

Page 64 of 72
Staff Report
Number of senior managers
In 2022/23, the CCG had 31 senior managers.
Staff numbers and costs
Pay Band 2 3 4 5 6 7 8a 8b 8c 8d 9 Other Grand Total
Senior Managers
Female 14 21 17 27 27 23 15 10 9 2 7 172
Male 1 1 3 3 2 7 2 7 5 5 4 40
Grand Total 1 15 24 20 29 34 25 22 15 9 7 11 212
Staff composition
EMPLOYED STAFF
Employee category Headcount WTE
Permanent 178 162.64
Fixed-term 28 24.38
TOTAL 206 187.02
AGENCY & INTERIM
TOTAL 6 0.00
GRAND TOTAL 212 187.02

Sickness absence data
Average FTE for
2022
Average Annual
Sick Days per FTE
Sum of FTE
Days Sick
Sum of FTE
Days
Available
Months
177
6.8
648
21,524
4
Sickness absence data can be found here: https://digital.nhs.uk/data-and-
information/publications/statistical/nhs-sickness-absence-rates
Staff turnover percentages
Staff Engagement
For the first year, all of the 5 CCGs in Mid and South Essex have participated in the
NHS Staff Survey on a combined basis and the results have been presented across
joint Directorates and teams.
The CCGs had an excellent response rate of 78%. Key themes have been shared with
the CCGs Executive Team and they have been asked to work with their teams to write
action plans in response to the staff survey results. In addition to this, the 5 CCGs
formed a staff engagement group in January 2022 and this group is also developing an
organisational action plan to look at key themes such as health and wellbeing, and
diversity and inclusion. This group has representation of staff from across the 5 CCGs
and will be tasked with feeding into the organisational development work required as
the CCGs transition into an ICB.
There are regular all-staff briefings across the 5 CCGs to communicate key messages
around organisational change, as well as operational updates and regular updates on
system priorities.
There are also opportunities for staff to meet at a more local level through Alliance
briefings as well as team briefings and regular one-to-one meetings with their
manager.
Page 65 of 72
Staff policies
The CCG has given full and fair consideration to applications for employment made by
disabled persons, having regard to their particular aptitudes and abilities.
The CCG has continued the employment of and arranged appropriate training for
employees who have become disabled persons during their period of employment.
It is the policy of the CCG to ensure that any member of the CCG Board, its staff and its
member practices are able to raise concerns about unlawful conduct, financial
malpractice/fraud and risks to the environment and to patient care in line with legislation
and good practice. This is covered under our whistleblowing policy.
Equality, Diversity, and Inclusion
The CCGs are committed to providing equal opportunities and to avoiding unlawful
discrimination and the Recruitment and Selection Policy is designed to assist the CCGs
in putting this commitment into practice. The policy is compliant with the Equality Act
2010 and sets out specific actions undertaken by the CCGs, in the context of
employment and people management, in order to fulfil its Public Sector Equality Duty.
All CCG staff were offered further equality, diversity, and inclusion training as part of the
transition into the ICB - the offering included unconscious bias training, awareness of
protected characteristics, allyship and also a complete review of policies, procedures
and practices to eliminate bias. This was offered in line with the recommendations of
the No More Tick boxes report.
The CCGs also worked with the Mid and South Essex Health and Care Partnership to
develop an organisational and system response to the regional Anti-Racism Strategy,
being implemented through the Equality, Diversity and Inclusion Subgroup that is
accountable to the Mid and South Essex People Board. In addition, an EDI dashboard
is also in development for the MSE Partnerships, which the CCGs will feed into.
The CCGs also participated in the MSE reciprocal mentoring programme through the
NHS Leadership academy, a commitment that has been made by the Executive teams
from across the system.
Trade Union Facility Time Reporting Requirements
There was no Trade Union Facility Time in the accounting period.
Health and Wellbeing
The CCGs have benefitted from a comprehensive staff health and wellbeing offer
through the Live Life Connected programme, which offers a vast array of health and
wellbeing interventions, such as online talks around health topics, online exercise
classes, mindfulness, and gratitude practice.
In addition, there is also an employee assistance programme available to all staff which
provides a telephone support line and counselling, as well as a comprehensive
occupational health provision.
Page 66 of 72

Page 67 of 72
During the Covid pandemic, there have also been enhanced national, regional and local
offers available to staff, including the regional mental health hubs and the Here For You
service is available to all CCG employees and has continued this year.
The CCGs also have a trained network of mental health first aiders and have also
provided bespoke Change and Resilience workshops for staff, as well as benefitting
from ICS offers such as Kindness masterclasses.
The CCGs are committed to supporting disabled colleagues within the workplace
through making reasonable adjustments as well as the use of regular risk assessments
and also supporting colleagues’ mental health through the use of stress risk
assessments and other support tools.
Health and Safety
The CCG’s Health and Safety Policy sets out our responsibilities and those of
employees under the Health and Safety Work Act 1974. Health and safety, fire safety
and manual handling are included in the mandatory training programme for all CCG
staff.
Risk assessment and inspections identify health and safety issues to enable
appropriate action to be taken to reduce risks to staff and other users of CCG premises.
Although CCG staff have worked from home since the beginning of the pandemic,
regular health, and safety inspections, building system tests and maintenance
continued throughout the year.
Expenditure on consultancy

Page 68 of 72

Page 69 of 72

Page 70 of 72
Losses and Special Payments
In the accounting period, the total number of NHS clinical commissioning group losses
and special payments cases were nil (2021/22: nil).
Exit packages, including special (non-contractual) payments
In the accounting period, the total number of NHS clinical commissioning group exit
packages were nil (2021/22: nil)
Page 71 of 72
PARLIAMENTARY ACCOUNTABILITY AND
AUDIT REPORT
The CCG is not required to produce a Parliamentary Accountability and Audit Report
but has opted to include disclosures on remote contingent liabilities, losses and special
payments, gifts, and fees and charges in this Accountability Report at page 70. An audit
certificate and report is also included in this Annual Report.
Page 72 of 72
ANNUAL ACCOUNTS
I confirm that the annual accounts adhere to the reporting framework.
Anthony McKeever
Accountable Officer
26 June 2023

Entity name:
NHS Mid Essex CCG
Statutory Accounts
This period
1-Apr-22 to 30-Jun-22
Last year 2021-22
This period ended
30-Jun-22
Last year ended 31-Mar-22
This period commencing:
1-Apr-22
Last year commencing:
1-Apr-21
Page 1 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Page
Number
The Primary Statements:
Statement of Comprehensive Net Expenditure for the period ended 30-Jun-22 3
Statement of Financial Position as at 30-Jun-22 4
Statement of Changes in Taxpayers' Equity for the period ended 30-Jun-22 5
Statement of Cash Flows for the period ended 30-Jun-22 6
Notes to the Accounts
Accounting Policies 7-10
Operating Revenue 11
Employee Benefits, Staff Numbers and Pension Costs 12-13
Operating Expenses 14
Better Payment Practice Code 15
Finance Costs 15
Leases 16-17
Trade and Other Receivables 18
Cash and Cash Equivalents 19
Trade and Other Payables 19
Provisions 20
Financial Instruments 21-22
Operating Segments 23
Joint Arrangements - Interests in Joint Operations 23
Related Party Transactions 24
Events After the End of the Reporting Period 25
Financial Performance Targets 25
CONTENTS
Page 2 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Statement of Comprehensive Net Expenditure for the period ended
30-Jun-22
1-Apr-22 to
30-Jun-22
2021-22
Note £'000 £'000
Income from sale of goods and services
2 (177) (720)
Total operating income
(177) (720)
Staff costs
4 3,064 9,443
Purchase of goods and services
5 189,036 917,926
Depreciation and impairment charges
5 47 -
Provision expense
5 - 973
Other operating expenditure
5 55 675
Total operating expenditure
192,202 929,017
Net operating expenditure
192,025 928,297
Finance costs
7 0 -
Comprehensive expenditure for the period
192,025 928,297
The notes on pages 7 to 25 form part of this statement
Page 3 of 32
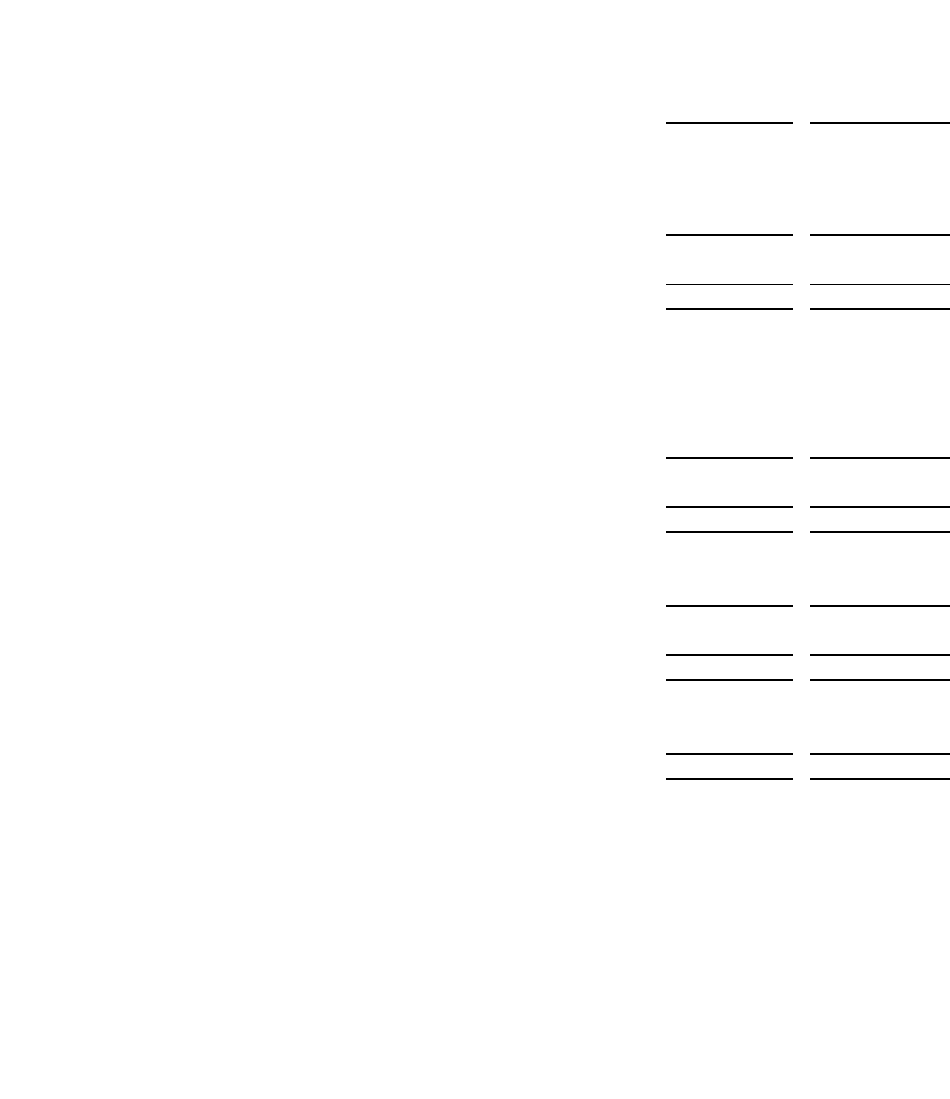
NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Statement of Financial Position as at
30 Jun 22
30-Jun-22
31-Mar-22
Note £'000 £'000
Non-current assets:
Right-of-use assets 8 175 -
Total non-current assets 175 -
Current assets:
Trade and other receivables 9 4,428 1,653
Cash and cash equivalents 10 0 0
Total current assets 4,428 1,653
Total assets 4,603 1,653
Current liabilities
Trade and other payables 11 (21,501) (46,420)
Lease liabilities 8 (185) -
Borrowings (2,588) (4,300)
Provisions 12 (2,093) (1,568)
Total current liabilities (26,367) (52,288)
Non-current assets plus/less net current assets/liabilities (21,764) (50,635)
Non-current liabilities
Provisions 12 (2,549) (2,549)
Total non-current liabilities (2,549) (2,549)
Assets less Liabilities (24,313) (53,184)
Financed by taxpayers’ equity
General fund (24,314) (53,184)
Total taxpayers' equity: (24,314) (53,184)
The notes on pages 7 to 25 form part of this statement
Chief Accountable Officer
Anthony McKeever
The financial statements on pages 3 to 6 were approved by the governing body on 26 June 23 and signed
on its behalf by:
Page 4 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Statement of Changes In Taxpayers Equity for the period ended
30-Jun-22
General fund
Total
reserves
£'000 £'000
Changes in taxpayers’ equity for 1-Apr-22 to 30-Jun-22
Balance at 1-Apr-22 (53,184) (53,184)
Adjusted NHS clinical commissioning group balance at 31-Mar-22 (53,184) (53,184)
Changes in NHS clinical commissioning group taxpayers’ equity for 1-Apr-
22 to 30-Jun-22
Net operating expenditure for the financial period (192,025)
(192,025)
Net recognised NHS clinical commissioning group expenditure for the
financial period
(192,025) (192,025)
Net funding 220,895
220,895
Balance at 30-Jun-22 (24,314) (24,314)
General fund Total reserves
£'000 £'000
Changes in taxpayers’ equity for 2021-22
Balance at 1-Apr-21
(38,528) (38,528)
Adjusted NHS Clinical Commissioning Group balance at 31-Mar-21 (38,528) (38,528)
Changes in NHS clinical commissioning group taxpayers’ equity for 2021-22
Net operating expenditure for the financial year (928,297)
(928,297)
Net recognised NHS clinical commissioning group expenditure for the
financial year
(928,297) (928,297)
Net funding 913,641
913,641
Balance at 31-Mar-22 (53,184) (53,184)
The notes on pages 7 to 25 form part of this statement
Page 5 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Statement of Cash Flows for the period ended
30-Jun-22
1-Apr-22 to
30-Jun-22
2021-22
Note
£'000 £'000
Cash flows from operating activities
Net operating expenditure for the financial period (192,025) (928,297)
Depreciation 5 47 0
(Increase)/decrease in trade & other receivables 9 (2,774) 7,071
(Decrease)/Increase in trade & other payables 11 (24,919) 2,971
Provisions utilised 12 525 (110)
Increase in provisions 12 0 973
Net cash (outflow) from operating activities (219,147) (917,392)
Net cash (outflow) before financing (219,147) (917,392)
Cash flows from financing activities
Grant in aid funding received 220,895 913,641
Repayment of lease liabilities (37) 0
Net cash inflow (outflow) from financing activities 220,858 913,641
Net increase/(decrease) in cash & cash equivalents 10 1,711 (3,752)
Cash & cash equivalents at the beginning of the financial period (4,299) (548)
Cash & cash equivalents at the end of the financial period (2,588) (4,300)
The notes on pages 7 to 25 form part of this statement
Page 6 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1
Accounting Policies
NHS England has directed that the financial statements of NHS clinical commissioning groups shall meet the accounting
requirements of the Group Accounting Manual issued by the Department of Health and Social Care. Consequently, the
following financial statements have been prepared in accordance with the Group Accounting Manual 2022-23 issued by the
Department of Health and Social Care. The accounting policies contained in the Group Accounting Manual follow International
Financial Reporting Standards to the extent that they are meaningful and appropriate to clinical commissioning groups, as
determined by HM Treasury, which is advised by the Financial Reporting Advisory Board. Where the Group Accounting Manual
permits a choice of accounting policy, the accounting policy which is judged to be most appropriate to the particular
circumstances of the clinical commissioning group for the purpose of giving a true and fair view has been selected. The
particular policies adopted by the clinical commissioning group are described below. They have been applied consistently in
dealing with items considered material in relation to the accounts.
1.1
Going Concern
These accounts have been prepared on a going concern basis.
Public sector bodies are assumed to be going concerns where the continuation of the provision of a service in the future is
anticipated, as evidenced by inclusion of financial provision for that service in published documents.
Where an NHS clinical commissioning group ceases to exist, it considers whether or not its services will continue to be
provided (using the same assets, by another public sector entity) in determining whether to use the concept of going concern
for the final set of financial statements. If services will continue to be provided the financial statements are prepared on the
going concern basis. The statement of financial position has therefore been drawn up at 30 June 22 on a going concern basis.
Following the approval of the Health and Care Bill on 28 April 2022 the NHS Basildon and Brentwood Clinical Commissioning
Group (the CCG) was dissolved on 30 June 22. Whilst the CCG as an entity ceased to exist on that date, the activities
undertaken by the CCG continued to be undertaken by the Mid and South Essex Integrated Health and Care Board. In
accordance with the Department of Health and Social Care Group Accounting Manual, the continuation of the provision of
services within the public sector means that the accounts of the CCG should be and have been prepared on a going concern
basis.
1.2
Accounting Convention
These accounts have been prepared under the historical cost convention modified to account for the revaluation of property,
plant and equipment, intangible assets, inventories and certain financial assets and financial liabilities.
1.3
Movement of Assets within the Department of Health and Social Care Group
As Public Sector Bodies are deemed to operate under common control, business reconfigurations within the Department of
Health and Social Care Group are outside the scope of IFRS 3 Business Combinations. Where functions transfer between two
public sector bodies, the Department of Health and Social Care GAM requires the application of absorption accounting.
Absorption accounting requires that entities account for their transactions in the period in which they took place, with no
restatement of performance required when functions transfer within the public sector. Where assets and liabilities transfer, the
Other transfers of assets and liabilities within the Department of Health and Social Care Group are accounted for in line with
IAS 20 and similarly give rise to income and expenditure entries.
1.4
Joint Arrangements
The NHS clinical commissioning group has not been part of any pooled budget arrangements in 2022-23. The NHS
commissioning group and Essex County Council have continued to operate a Better Care Fund during 2022-23 under a
Section 75 agreement. The arrangements under which the Better Care Fund operated in 2022-23 do not constitute a pooled
budget as the risks of each scheme have remained with the respective commissioners. See Note 15 for further information.
1.5
Operating Segments
Income and expenditure are analysed in the Operating Segments note and are reported in line with management information
used within the clinical commissioning group.
Page 7 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1.6
Revenue
In the application of IFRS 15 a number of practical expedients offered in the Standard have been employed. These are as
follows:
• As per paragraph 121 of the Standard the clinical commissioning group will not disclose information regarding performance
obligations part of a contract that has an original expected duration of one year or less,
• The NHS clinical commissioning group is to similarly not disclose information where revenue is recognised in line with the
practical expedient offered in paragraph B16 of the Standard where the right to consideration corresponds directly with value of
the performance completed to date.
• The FReM has mandated the exercise of the practical expedient offered in C7(a) of the Standard that requires the NHS
clinical commissioning group to reflect the aggregate effect of all contracts modified before the date of initial application.
The main source of funding for the NHS clinical commissioning group is from NHS England. This is drawn down and credited to
the general fund. Funding is recognised in the period in which it is received.
Revenue in respect of services provided is recognised when (or as) performance obligations are satisfied by transferring
promised services to the customer, and is measured at the amount of the transaction price allocated to that performance
obligation.
Where income is received for a specific performance obligation that is to be satisfied in the following year, that income is
deferred.
Payment terms are standard reflecting cross government principles.
The value of the benefit received when the NHS clinical commissioning group accesses funds from the Government’s
apprenticeship service are recognised as income in accordance with IAS 20, Accounting for Government Grants. Where these
funds are paid directly to an accredited training provider, non-cash income and a corresponding non-cash training expense are
recognised, both equal to the cost of the training funded.
1.7
Employee Benefits
1.7.1
Short-term Employee Benefits
Salaries, wages and employment-related payments, including payments arising from the apprenticeship levy, are recognised in
the period in which the service is received from employees, including bonuses earned but not yet taken.
The cost of leave earned but not taken by employees at the end of the period is recognised in the financial statements to the
extent that employees are permitted to carry forward leave into the following period.
1.7.2
Retirement Benefit Costs
Past and present employees are covered by the provisions of the NHS pensions schemes. These schemes are unfunded,
defined benefit schemes that cover NHS employers, General Practices and other bodies allowed under the direction of the
Secretary of State in England and Wales. The schemes are not designed to be run in a way that would enable NHS bodies to
identify their share of the underlying scheme assets and liabilities. Therefore, the schemes are accounted for as if they were a
defined contribution scheme; the cost recognised in these accounts represents the contributions payable for the period. Details
of the benefits payable under these provisions can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions.
For early retirements other than those due to ill health the additional pension liabilities are not funded by the scheme. The full
amount of the liability for the additional costs is charged to expenditure at the time the clinical commissioning group commits
itself to the retirement, regardless of the method of payment.
The schemes are subject to a full actuarial valuation every four years and an accounting valuation every year.
1.8
Other Expenses
Other operating expenses are recognised when, and to the extent that, the goods or services have been received. They are
measured at the fair value of the consideration payable.
1.9
Leases
A lease is a contract, or part of a contract, that conveys the right to control the use of an asset for a period of time in exchange
for consideration. The NHS clinical commissioning group assesses whether a contract is or contains a lease, at inception of the
contract.
Page 8 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1.9.1
The NHS Clinical Commissioning Group as Lessee
A right-of-use asset and a corresponding lease liability are recognised at commencement of the lease.
The lease liability is initially measured at the present value of the future lease payments, discounted by using the rate implicit in
the lease. If this rate cannot be readily determined, the prescribed HM Treasury discount rates are used as the incremental
borrowing rate to discount future lease payments.
The HM Treasury incremental borrowing rate of 0.95% is applied for leases commencing, transitioning or being remeasured in
the 2022 calendar year under IFRS 16.
Lease payments included in the measurement of the lease liability comprise
-Fixed payments;
-Variable lease payments dependent on an index or rate, initially measured using the index or rate at commencement;
-The amount expected to be payable under residual value guarantees;
-The exercise price of purchase options, if it is reasonably certain the option will be exercised; and
-Payments of penalties for terminating the lease, if the lease term reflects the exercise of an option to terminate the lease.
Variable rents that do not depend on an index or rate are not included in the measurement the lease liability and are recognised
as an expense in the period in which the event or condition that triggers those payments occurs.
The lease liability is subsequently measured by increasing the carrying amount for interest incurred using the effective interest
method and decreasing the carrying amount to reflect the lease payments made. The lease liability is remeasured, with a
corresponding adjustment to the right-of-use asset, to reflect any reassessment of or modification made to the lease.
The right-of-use asset is initially measured at an amount equal to the initial lease liability adjusted for any lease prepayments or
incentives, initial direct costs or an estimate of any dismantling, removal or restoring costs relating to either restoring the
location of the asset or restoring the underlying asset itself, unless costs are incurred to produce inventories.
The subsequent measurement of the right-of-use asset is consistent with the principles for subsequent measurement of
property, plant and equipment. Accordingly, right-of-use assets, that are held for their service potential and are in use, are
subsequently measured at their current value in existing use.
Right-of-use assets for leases that are low value or short term and for which current value in use is not expected to fluctuate
significantly due to changes in market prices and conditions are valued at depreciated historical cost as a proxy for current
value in existing use.
Other than leases for assets under construction and investment property, the right-of-use asset is subsequently depreciated on
a straight-line basis over the shorter of the lease term or the useful life of the underlying asset. The right-of-use asset is tested
for impairment if there are any indicators of impairment and impairment losses are accounted for as described in the
‘Depreciation, amortisation and impairments’ policy.
Peppercorn leases are defined as leases for which the consideration paid is nil or nominal (that is, significantly below market
value). Peppercorn leases are in the scope of IFRS 16 if they meet the definition of a lease in all aspects apart from containing
consideration.
For peppercorn leases a right-of-use asset is recognised and initially measured at current value in existing use. The lease
liability is measured in accordance with the above policy. Any difference between the carrying amount of the right-of-use asset
and the lease liability is recognised as income as required by IAS 20 as interpreted by the FReM.
Leases of low value assets (value when new less than £5,000) and short-term leases of 12 months or less are recognised as
an expense on a straight-line basis over the term of the lease.
1.10
Cash & Cash Equivalents
Cash is cash in hand and deposits with any financial institution repayable without penalty on notice of not more than 24 hours.
Cash equivalents are investments that mature in 3 months or less from the date of acquisition and that are readily convertible to
known amounts of cash with insignificant risk of change in value.
In the Statement of Cash Flows, cash and cash equivalents are shown net of bank overdrafts that are repayable on demand
and that form an integral part of the clinical commissioning group’s cash management.
Page 9 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1.11
Provisions
Provisions are recognised when the NHS clinical commissioning group has a present legal or constructive obligation as a result
of a past event, it is probable that the NHS clinical commissioning group will be required to settle the obligation, and a reliable
estimate can be made of the amount of the obligation. The amount recognised as a provision is the best estimate of the
expenditure required to settle the obligation at the end of the reporting period, taking into account the risks and uncertainties.
Where a provision is measured using the cash flows estimated to settle the obligation, its carrying amount is the present value
of those cash flows using HM Treasury’s discount rate as follows:
When some or all of the economic benefits required to settle a provision are expected to be recovered from a third party, the
receivable is recognised as an asset if it is virtually certain that reimbursements will be received and the amount of the
receivable can be measured reliably.
A restructuring provision is recognised when the NHS clinical commissioning group has developed a detailed formal plan for
the restructuring and has raised a valid expectation in those affected that it will carry out the restructuring by starting to
implement the plan or announcing its main features to those affected by it. The measurement of a restructuring provision
includes only the direct expenditures arising from the restructuring, which are those amounts that are both necessarily entailed
by the restructuring and not associated with on-going activities of the entity.
1.12
Clinical Negligence Costs
NHS Resolution operates a risk pooling scheme under which the NHS clinical commissioning group pays an annual
contribution to NHS Resolution, which in return settles all clinical negligence claims. The contribution is charged to expenditure.
Although NHS Resolution is administratively responsible for all clinical negligence cases, the legal liability remains with the
NHS clinical commissioning group.
1.13
Non-Clinical Risk Pooling
The NHS clinical commissioning group participates in the Property Expenses Scheme and the Liabilities to Third Parties
Scheme. Both are risk pooling schemes under which the NHS clinical commissioning group pays an annual contribution to NHS
Resolution and, in return, receives assistance with the costs of claims arising. The annual membership contributions, and any
excesses payable in respect of particular claims, are charged to operating expenses as and when they become due.
1.14
Contingent Liabilities and Contingent Assets
A contingent liability is a possible obligation that arises from past events, and whose existence will be confirmed only by the
occurrence, or non-occurrence of one or more uncertain future events not wholly within the control of the NHS clinical
commissioning group, or a present obligation that is not recognised, because it is not probable that a payment will be required
to settle the obligation, or the amount of the obligation cannot be measured sufficiently reliably. A contingent liability is disclosed
unless the possibility of a payment is remote.
A contingent asset is a possible asset that arises from past events, and whose existence will be confirmed by the occurrence,
or non-occurrence of one or more uncertain future events not wholly within the control of the NHS clinical commissioning group.
A contingent asset is disclosed where an inflow of economic benefits is probable.
Where the time value of money is material, contingent liabilities and contingent assets are disclosed at their present value.
1.15
Financial Assets
Financial assets are recognised when the clinical commissioning group becomes party to the financial instrument contract or, in
the case of trade receivables, when the goods or services have been delivered. Financial assets are derecognised when the
contractual rights have expired or the asset has been transferred.
Financial assets are classified into the following categories:
· Financial assets at amortised cost;
· Financial assets at fair value through other comprehensive income and ;
· Financial assets at fair value through profit and loss.
The classification is determined by the cash flow and business model characteristics of the financial assets, as set out in IFRS
9, and is determined at the time of initial recognition.
1.15.1
Financial Assets at Amortised cost
Financial assets measured at amortised cost are those held within a business model whose objective is achieved by collecting
contractual cash flows and where the cash flows are solely payments of principal and interest. This includes most trade
receivables and other simple debt instruments. After initial recognition these financial assets are measured at amortised cost
using the effective interest method less any impairment. The effective interest rate is the rate that exactly discounts estimated
future cash receipts through the life of the financial asset to the gross carrying amount of the financial asset.
Page 10 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1.15.2
Financial Assets at Fair Value Through Other Comprehensive Income
Financial assets held at fair value through other comprehensive income are those held within a business model, whose
objective is achieved by both collecting contractual cash flows and selling financial assets, and where the cash flows are solely
payments of principal and interest.
1.15.3
Financial Assets at Fair Value Through Profit and Loss
Financial assets measure at fair value through profit and loss are those that are not otherwise measured at amortised cost or
fair value through other comprehensive income. This includes derivatives and financial assets acquired principally for the
purpose of selling in the short term.
1.16
Financial Liabilities
Financial liabilities are recognised on the statement of financial position when the NHS clinical commissioning group becomes
party to the contractual provisions of the financial instrument or, in the case of trade payables, when the goods or services have
been received. Financial liabilities are de-recognised when the liability has been discharged, that is, the liability has been paid
or has expired.
1.16.1
Other Financial Liabilities
After initial recognition, all other financial liabilities are measured at amortised cost using the effective interest method, except
for loans from Department of Health and Social Care, which are carried at historic cost. The effective interest rate is the rate
that exactly discounts estimated future cash payments through the life of the asset, to the net carrying amount of the financial
liability. Interest is recognised using the effective interest method.
1.17
Value Added Tax
Most of the activities of the NHS clinical commissioning group are outside the scope of VAT and, in general, output tax does not
apply and input tax on purchases is not recoverable. Irrecoverable VAT is charged to the relevant expenditure category or
included in the capitalised purchase cost of fixed assets. Where output tax is charged or input VAT is recoverable, the amounts
are stated net of VAT.
1.18
Foreign Currencies
The NHS clinical commissioning group’s functional currency and presentational currency is pounds sterling and amounts are
presented in thousands of pounds unless expressly stated otherwise. Transactions denominated in a foreign currency are
translated into sterling at the exchange rate ruling on the dates of the transactions. At the end of the reporting period, monetary
items denominated in foreign currencies are retranslated at the spot exchange rate on 30 June 2022. Resulting exchange gains
and losses for either of these are recognised in the NHS clinical commissioning group’s surplus in the period in which they
arise.
1.19
Critical Accounting Judgements and Key Sources of Estimation Uncertainty
In the application of the NHS clinical commissioning group's accounting policies, management is required to make various
judgements, estimates and assumptions. These are regularly reviewed.
1.19.1
Critical Accounting Judgements in Applying Accounting Policies
The following are the judgements, apart from those involving estimations, that management has made in the process of
applying the clinical commissioning group's accounting policies and that have the most significant effect on the amounts
recognised in the financial statements.
The NHS clinical Commissioning group has operated a Better Care Fund with Essex County Council during 2022-23, under a
section 75 agreement. This arrangement has been reviewed and all parties have agreed that it does not constitute a pooled
budget, as the risks of each scheme have remained with the respective commissioner. See Note 15 for furthur information.
1.19.2
Sources of Estimation Uncertainty
The following are assumptions about the future and other major sources of estimation uncertainty that have a significant risk of
resulting in a material adjustment to the carrying amounts of assets and liabilities within the next financial year.
The CCG does not consider there to be any assumptions about the future and other major sources of estimation uncertainty
that have a significant risk of resulting in a material adjustment to the carrying amounts of assets and liabilities within the next
financial year.
1.20
Adoption of New Standards
On 1 April 2022, the NHS clinical commissioning group adopted IFRS 16 ‘Leases’. The new standard introduces a single, on
statement of financial position lease accounting model for lessees and removes the distinction between operating and finance
leases.
Under IFRS 16 the NHS clinical commissioning group recognise a right-of-use asset representing the NHS clinical
commissioning group’s right to use the underlying asset, and a lease liability representing its obligation to make lease payments
for any operating leases assessed to fall under IFRS 16. There are recognition exemptions for short term leases and leases of
low value items.
In addition, the group will no longer charge provisions for operating leases that it assesses to be onerous to the statement of
comprehensive net expenditure. Instead, the group will include the payments due under the lease with any appropriate
assessment for impairments in the right-of-use asset.
Page 11 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
Notes to the financial statements
1.20.1
Impact Assessment
The NHS clinical commissioning group has applied the modified retrospective approach, and recognise the cumulative effect of
adopting the standard at the date of initial application, as an adjustment to the opening retained earnings with no restatement of
comparative balances.
IFRS 16 does not require entities to reassess whether a contract is, or contains, a lease at the date of initial application. HM
Treasury has interpreted this to mandate this practical expedient and, therefore, the group has applied IFRS 16 to contracts
identified as a lease under IAS 17 or IFRIC 4 at 1 April 2022.
The NHS clinical commissioning group has utilised three further practical expedients under the transition approach adopted:
a) The election to not make an adjustment for leases for which the underlying asset is of low value.
b) The election to not make an adjustment to leases where the lease terms ends within 12 months of the date of application.
c) The election to use hindsight in determining the lease term if the contract contains options to extend or terminate the lease.
The most significant impact of the adoption of IFRS 16 has been the need to recognise right-of-use assets and lease liabilities
for any buildings previously treated as operating leases that meet the recognition criteria in IFRS 16. Expenditure on operating
leases has been replaced by interest on lease liabilities and depreciation on right-of-use assets in the statement of
comprehensive net expenditure.
As of 1 April 2022, the group recognised £221k of right-of-use assets and lease liabilities of £221k. The weighted average
incremental borrowing rate applied at 1 April 2022 is 0.95% and on adoption of IFRS 16 there was an [£Xm] impact to tax
payers’ equity.
The NHS clinical commissioning group has assessed that there is no significant impact on its current finance leases due to the
immaterial value on the statement of financial position, and no significant impact on the limited transactions it undertakes as a
lessor because IFRS 16 has not substantially changed the accounting arrangements for lessors.
The following table reconciles the group’s operating lease obligations at 31 March 2022, disclosed in the group’s 2021/22
financial statements, to the lease liabilities recognised on initial application of IFRS 16 at 1 April 2022.
Total
£000
Operating lease commitments at 31 Mar 22 1,089
Impact of discounting at 1 Apr 22 using the weighted average incremental borrowing rate of 0.95% 10
Operating lease commitments discounted used weighted average IBR 1,079
Less: Low value leases 858-
Lease liability at 1 Apr 22 221
1.21
New and revised IFRS Standards in issue but not yet effective
● IFRS 17 Insurance Contracts – Application required for accounting periods beginning on or after 1 January 21. Standard is
not yet adopted by the FReM which is expected to be April 23: early adoption is not therefore permitted.
The NHS clinical commissioning group does not anticipate any significant impact from Standards that have not yet been
adopted.
Page 12 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
2 Operating Revenue
1-Apr-22 to
30-Jun-22
2021-22
Total Total
£'000 £'000
Income from sale of goods and services
Non-patient care services to other bodies
177 710
Other contract income
0 10
Total Income from sale of goods and services 177 720
Total operating income 177 720
3 Disaggregation of Income - Income from sale of good and services
Non-patient care
services to other
bodies
£'000
Source of Revenue
NHS
72
Non NHS
105
Total
177
Non-patient care
services to other
bodies
£'000
Timing of Revenue
Point in time
-
Over time
177
Total
177
Page 13 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
4. Employee Benefits and Staff Numbers
4.1.1 Employee benefits / Staff costs
Permanent
employees
Other Total
£'000 £'000 £'000
Employee benefits
Salaries and wages 2,321 51 2,372
Social security costs 268 (0) 268
Employer contributions to NHS pension scheme 403 - 403
Other pension costs 13 - 13
Apprenticeship levy 8 - 8
Gross employee benefits expenditure 3,013 51 3,064
Net employee benefits 3,013 51 3,064
No Exit Packages were paid in 1-Apr-22 to 30-Jun-22 or 2021-22
4.1.1 Employee benefits / Staff costs
Permanent
employees
Other Total
£'000 £'000 £'000
Employee benefits
Salaries and wages 6,669 800 7,469
Social security costs 722 2 724
Employer contributions to NHS pension scheme 1,213 - 1,213
Other pension costs 9 - 9
Apprenticeship levy 28 - 28
Gross employee benefits expenditure
8,641 802 9,443
Net employee benefits 8,641 802 9,443
4.2 Average number of people employed (WTE)
Permanently
employed
Other Total
Number Number Number
Total number of people employed (WTE) 185.4 1.7 187.0
Permanently
employed
Other Total
Number Number Number
Total number of people employed (WTE) 136.09 7.39 143.48
1-Apr-22 to 30-Jun-22
2021-22
1-Apr-22 to 30-Jun-22
2021-22
Page 14 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
4.3 Pension Costs
Past and present employees are covered by the provisions of the two NHS Pension Schemes. Details of the benefits
payable and rules of the Schemes can be found on the NHS Pensions website at www.nhsbsa.nhs.uk/pensions. Both
are unfunded defined benefit schemes that cover NHS employers, GP practices and other bodies, allowed under the
direction of the Secretary of State for Health and Social Care in England and Wales. They are not designed to be run in
a way that would enable NHS bodies to identify their share of the underlying scheme assets and liabilities. Therefore,
each scheme is accounted for as if it were a defined contribution scheme: the cost to the NHS body of participating in
each scheme is taken as equal to the contributions payable to that scheme for the accounting period.
In order that the defined benefit obligations recognised in the financial statements do not differ materially from those that
would be determined at the reporting date by a formal actuarial valuation, the FReM requires that “the period between
formal valuations shall be four years, with approximate assessments in intervening years”. An outline of these follows:
4.3.1 Accounting valuation
A valuation of scheme liability is carried out annually by the scheme actuary (currently the Government Actuary’s
Department) as at the end of the reporting period. This utilises an actuarial assessment for the previous accounting
period in conjunction with updated membership and financial data for the current reporting period, and is accepted as
providing suitably robust figures for financial reporting purposes. The valuation of the scheme liability as at 31 March 22,
is based on valuation data as 31 March 21, updated to 31 March 22 with summary global member and accounting data.
In undertaking this actuarial assessment, the methodology prescribed in IAS 19, relevant FReM interpretations, and the
discount rate prescribed by HM Treasury have also been used.
The latest assessment of the liabilities of the scheme is contained in the report of the scheme actuary, which forms part
of the annual NHS Pension Scheme Accounts. These accounts can be viewed on the NHS Pensions website and are
published annually. Copies can also be obtained from The Stationery Office.
4.3.2 Full actuarial (funding) valuation
The purpose of this valuation is to assess the level of liability in respect of the benefits due under the schemes (taking
into account recent demographic experience), and to recommend contribution rates payable by employees and
employers.
The latest actuarial valuation undertaken for the NHS Pension Scheme was completed as at 31 March 2016. The
results of this valuation set the employer contribution rate payable from April 2019 to 20.6% of pensionable pay.
The 2016 funding valuation also tested the cost of the Scheme relative to the employer cost cap that was set following
the 2012 valuation. There was initially a pause to the cost control element of the 2016 valuations, due to the uncertainty
around member benefits caused by the discrimination ruling relating to the McCloud case.
HMT published valuation directions dated 7 October 2021 (see Amending Directions 2021) that set out the technical
detail of how the costs of remedy are included in the 2016 valuation process. Following these directions, the scheme
actuary has completed the cost control element of the 2016 valuation for the NHS Pension Scheme, which concludes no
changes to benefits or member contributions are required. The 2016 valuation reports can be found on the NHS
Pensions website at https://www.nhsbsa.nhs.uk/nhs-pension-scheme-accounts-and-valuation-reports.
Page 15 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
5 Operating expenses
1-Apr-22 to 30-
Jun-22
2021-22
Total Total
£'000 £'000
Purchase of goods and services
Services from other CCGs and NHS England 620 1,686
Services from foundation trusts 132,995 605,211
Services from other NHS trusts 7,058 25,771
Services from other WGA bodies - 1
Purchase of healthcare from non-NHS bodies 21,862 152,882
Prescribing costs 13,638 58,098
General Ophthalmic services 1 8
GPMS/APMS and PCTMS 13,097 64,395
Supplies and services – clinical 7 30
Supplies and services – general (1,780) 3,836
Consultancy services 79 542
Establishment 280 836
Transport 812 2,864
Premises 191 1,368
Audit fees 71 78
Other professional fees 43 239
Legal fees 5 56
Education, training and conferences 57 25
Total purchase of goods and services 189,036 917,926
Depreciation and impairment charges
Depreciation 47 -
Total depreciation and impairment charges 47 -
Provision expense
Provisions - 973
Total provision expense - 973
Other operating expenditure
Chair and non-executive members 40 104
Grants to Other bodies 14 566
Expected credit loss on receivables 1 -
Other expenditure (0) 5
Total other operating expenditure 55 675
Total operating expenditure 189,138 919,574
There were no Losses or special payments in 1-Apr-22 to 30-Jun-22 or 2021-22
Page 16 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
8 Leases
8.1 Right-of-use assets
1-Apr-22 to 30-Jun-22
Buildings
excluding
dwellings
Total
£'000 £'000
Cost/valuation at 1-Apr-22 - -
IFRS 16 transition adjustment 222 222
Cost/valuation at 30-Jun-22 222 222
Depreciation 1-Apr-22 - -
Charged during the period 47 47
Depreciation at 30-Jun-22 47 47
Net book value at 30-Jun-22 175 175
8.2 Lease liabilities
1-Apr-22 to 30-Jun-22
1-Apr-22 to
30-Jun-22
£'000
Lease liabilities at 1-Apr-22
-
IFRS 16 transition adjustment 221
Repayment of lease liabilities (including interest) (37)
Lease liabilities at 30-Jun-22 184
8.3 Lease liabilities - maturity analysis of undiscounted future lease payments
1-Apr-22 to
30-Jun-22
£'000
Within one year (148)
Between one and five years (37)
Balance at 30-Jun-22 (185)
Effect of discounting
(0)
Included in:
Current lease liabilities (185)
Balance at 30-Jun-22 (185)
Page 17 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
6 Better Payment Practice Code
Measure of compliance
1-Apr-22 to
30-Jun-22
1-Apr-22 to
30-Jun-22
2021-22 2021-22
Number £'000 Number £'000
Non-NHS payables
Total non-NHS trade invoices paid in the period 4,068 58,672 12,247 229,306
Total non-NHS trade Invoices paid within target 4,000 57,806 11,747 222,252
Percentage of non-NHS trade invoices paid within target 98.33% 98.52% 95.92% 96.92%
NHS payables
Total NHS trade invoices paid in the period 160 110,881 668 662,643
Total NHS trade invoices paid within target 143 106,360 642 657,668
Percentage of NHS trade Invoices paid within target 89.38% 95.92% 96.11% 99.25%
7 Finance Costs
1-Apr-22 to
30-Jun-22
2021-22
£'000
£'000
Interest
Interest on lease liabilities 0 -
Total interest 0 -
Total finance costs 0 -
Page 18 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
8 Leases continued
8.4 Amounts recognised in statement of comprehensive net expenditure
1-Apr-22 to
30-Jun-22
2021-22
£'000
£'000
Depreciation expense on right-of-use assets 47 -
Interest expense on lease liabilities 0 -
8.5 Amounts recognised in statement of cash flows
1-Apr-22 to
30-Jun-22
2021-22
£'000
£'000
Total cash outflow on leases under IFRS 16 (37) -
8.6 Leases narrative
We receive an annual charging schedule from NHS Property Services in relation to the costs.
The leasing activities falling under IFRS 16 relate to the administration premises at Hedgerows
Business Park, Chelmsford for the NHS clinical commissioning group.
Page 19 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
9 Trade and other receivables
30-Jun-22 31-Mar-22
£'000 £'000
NHS receivables: revenue
141 191
NHS/WGA accrued income
30 739
Non-NHS and other WGA receivables:
revenue
36 380
Non-NHS and other WGA prepayments
266 255
Non-NHS and other WGA accrued income
3,365 40
VAT
590 48
Total trade & other receivables - current 4,428 1,653
9.1 Receivables past their due date but not impaired
30-Jun-22 30-Jun-22 31-Mar-22 31-Mar-22
DHSC group
bodies
Non DHSC
group bodies
DHSC group
bodies
Non DHSC
group bodies
£'000 £'000
£'000 £'000
By up to three months
124 26 18 159
By three to six months
- - 21 -
By more than six months
17 - - -
Total 141 26 39 159
Page 20 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
10 Cash and cash equivalents
1-Apr-22 to
30-Jun-22
2021-22
£'000
£'000
Opening Balance (4,299) (548)
Net change in period 1,711 (3,752)
Closing Balance (2,588) (4,300)
Made up of:
Cash with the government banking service 0 -
Cash in hand - 0
Cash and cash equivalents as in Statement of Financial Position 0 0
Bank overdraft: Government Banking Service (2,588) (4,300)
Closing Balance (2,588) (4,300)
11 Trade and other payables
30-Jun-22 31-Mar-22
£'000 £'000
NHS payables: revenue 298 4,318
NHS accruals 2,724 1,650
Non-NHS and other WGA payables: revenue 2,116 2,148
Non-NHS and other WGA accruals 15,316 37,120
Non-NHS and Other WGA deferred income 38 75
Social security costs 162 149
Tax 127 132
Other payables and accruals 720 828
Total trade & other payables - current 21,501 46,420
Other payables include £335k outstanding pension contributions at 30-Jun-22 (31-Mar-22 £394k)
The NHS clinical commissioning group's cash position is reported in the financial statements as a negative
balance of £2,588k at 30 Jun 22, due to outstanding payments due to clear after year-end. As at 30 Jun 22,
the NHS clinical commissioning group had a net positive balance deposited in its Government Banking
Service bank account of £110k.
Page 21 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
12 Provisions
Current Non-current Current Non-current
30-Jun-22 30-Jun-22 31-Mar-22 31-Mar-22
£'000 £'000 £'000 £'000
Restructuring 919 - 919 -
Continuing care 1,030 2,351 494 2,351
Other 144 198 155 198
Total provisions 2,093 2,549 1,568 2,549
Total current and non-current 4,642 4,117
Restructuring
Continuing
Care
Other Total
£'000 £'000 £'000 £'000
Balance at 1-Apr-22 919 2,844 354 4,117
Utilised during the period - 536 (11)
525
Balance at 30-Jun-22 919 3,380 343 4,642
Expected timing of cash flows:
Within one year 919 1,030 144
2,093
Between one and five years - 2,350 199
2,549
Balance at 30-Jun-22 919 3,380 343 4,642
Restructuring provision
CHC (Continuing Care) provision
Other provision
A restructuring provision has been calculated across all CCGs and shared proportionately to the size of each CCG. The provision
has been made as the CCGs are in the process of restructuring resources for transition. Engagement on the restructure began
during March 22, with the information available the CCG has estimated potential one-off costs which could come to bear, throughout
2022-23 as a result of decisions made during 2021-22. These costs are associated with displacement of staff, retraining or
redeployment on the basis of the new organisational form.
This provision is to cover the cost of reimbursing residents for CHC amenity top ups back to 2012 as per the national CHC guidance.
The provision has been calculated based on a full years anticipated cost extrapolated back to 2012.
This provision which covered dilapidation costs; based on 7.5% of the annual lease value, from the commencement of the lease,
has been released following the council relocating the CCG to a new part of the building, as part of changes to the council building.
Page 22 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
13 Financial Instruments
13.1 Financial risk management
13.1.1 Currency risk
13.1.2 Interest rate risk
13.1.3 Credit risk
13.1.4 Liquidity risk
13.1.5 Financial Instruments
As the cash requirements of NHS England are met through the estimate process, financial instruments play a more limited role in
creating and managing risk than would apply to a non-public sector body. The majority of financial instruments relate to contracts to buy
non-financial items in line with NHS England's expected purchase and usage requirements and NHS England is therefore exposed to
little credit, liquidity or market risk.
The NHS clinical commissioning group borrows from government for capital expenditure, subject to affordability as confirmed by NHS
England. The borrowings are for 1 to 25 years, in line with the life of the associated assets, and interest is charged at the National Loans
Fund rate, fixed for the life of the loan. The clinical commissioning group therefore has low exposure to interest rate fluctuations.
Because the majority of the NHS clinical commissioning group and revenue comes parliamentary funding, NHS clinical commissioning
group has low exposure to credit risk. The maximum exposures as at the end of the financial year are in receivables from customers, as
disclosed in the trade and other receivables note.
NHS clinical commissioning group is required to operate within revenue and capital resource limits, which are financed from resources
voted annually by Parliament. The NHS clinical commissioning group draws down cash to cover expenditure, as the need arises. The
NHS clinical commissioning group is not, therefore, exposed to significant liquidity risks.
Financial reporting standard IFRS 7 requires disclosure of the role that financial instruments have had during the period in creating or
changing the risks a body faces in undertaking its activities.
Because NHS clinical commissioning group is financed through parliamentary funding, it is not exposed to the degree of financial risk
faced by business entities. Also, financial instruments play a much more limited role in creating or changing risk than would be typical of
listed companies, to which the financial reporting standards mainly apply. The clinical commissioning group has limited powers to borrow
or invest surplus funds and financial assets and liabilities are generated by day-to-day operational activities rather than being held to
change the risks facing the clinical commissioning group in undertaking its activities.
Treasury management operations are carried out by the finance department, within parameters defined formally within the NHS clinical
commissioning group standing financial instructions and policies agreed by the governing body. Treasury activity is subject to review by
the NHS clinical commissioning group and internal auditors.
The NHS clinical commissioning group is principally a domestic organisation with the great majority of transactions, assets and liabilities
being in the UK and sterling based. The NHS clinical commissioning group has no overseas operations. The NHS clinical commissioning
group and therefore has low exposure to currency rate fluctuations.
Page 23 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
13 Financial instruments continued.
13.2 Financial assets
Financial assets
measured at
amortised cost
Total
30-Jun-22 30-Jun-22
£'000 £'000
Trade and other receivables with NHSE bodies 154 154
Trade and other receivables with other DHSC / WGA group bodies 3,382 3,382
Trade and other receivables with external bodies 36 36
Cash and cash equivalents 0 0
Total at 30-Jun-22 3,572 3,572
13.3 Financial liabilities
Financial liabilities
measured at
amortised cost
Total
30-Jun-22 30-Jun-22
£'000
£'000
Loans with external bodies 2,588
2,588
Trade and other payables with NHSE bodies 100
100
Trade and other payables with other DHSC group bodies 3,308
3,308
Trade and other payables with external bodies (Incl. IFRS 16 Lease Liability). 17,950
17,950
Total at 30-Jun-22 23,946 23,946
Page 24 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
14 Operating Segments
15 Joint Arrangements - Interests in Joint Operations
1-Apr-22 to
30-Jun-22
2021-22
£'000 £'000
Income 6,722 26,888
Expenditure (6,722) (26,888)
There are five NHS clinical commissioning group (CCGs), within Essex Better Care Fund:
NHS Basildon and Brentwood Clinical Commissioning Group (BBCCG)
NHS Castle Point and Rochford Clinical Commissioning Group (CPRCCG)
NHS Mid Essex Clinical Commissioning Group (MECCG)
NHS North East Essex Clinical Commissioning Group (NECCG)
NHS West Essex Clinical Commissioning Group (WECCG)
The NHS clinical commissioning group has only one segment, commissioning of healthcare services (2021-22 one
segment).
The s75 agreement sets out the terms on which the partners have agreed to collaborate and to establish a framework
through which the partners can secure the future position of health and social care services through lead
commissioning arrangements. It is also the means through which the partners pool funds and align budgets as agreed
between the partners.
The Essex Better Care Fund therefore comprises five pooled funds (i.e. one for each CCG), each governed by a
Section 75 Agreement, with an overarching collaboration agreement signed by Essex County Council and each of the
CCGs.
The NHS clinical commissioning group shares of the income and expenditure handled by the Better Care Fund in the
financial period were:
Page 25 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
16 Related Party Transactions
Details of related party transactions are as follows:
Payments
to Related
Party
Receipts
from
Related
Party
Amounts
owed to
Related
Party
Amounts
due from
Related
Party
£'000 £'000 £'000 £'000
Part one - Transactions with board members and those with significant influence over the CCG
Part two - Transactions in relation to interests declared by Governing Board Members
Nursing for NHS Thurrock CCG - Rachel Hearn (Executive Director of Nursing), Anthony
McKeever (Joint Accountable Officer), Mark Barker (Joint Chief Finance Officer)
18 - - -
Dr Julie McGeachy (GP Board Member) - spouse is employed as Chief Medical Officer at
Provide
9,742 - 994 -
Part Three - Transactions in relation to practices where the GP has served during the period of the Governing Body
Dr Julie McGeachy (GP Board Member) - a GP partner at Dengie Medical Partnership 429 - 26 -
Dr Fatai Salau (GP Board Member) - Douglas Grove Surgery partner 459 - 28 -
Dr Anna Davey (Chair of Mid Essex CCG and Partner at Coggeshall Surgery) 467 - 33 -
Part Four - Material transactions in relation to Department of Health and Social Care Bodies
Cambridge University Hospitals NHS Foundation Trust
East of England Ambulance Service NHS Trust
East Suffolk and North Essex NHS Foundation Trust
Essex Partnership University NHS Foundation Trust
Hertfordshire Partnership University NHS Foundation Trust
Mid and South Essex NHS Foundation Trust
NHS Arden & GEM Commissioning Support Unit
NHS Business Services Authority
North East London NHS Foundation Trust
Princess Alexandra Hospital NHS Trust
Specialist acute London hospitals
Part Five - Department of Health and Social Care
The individuals and entities that the Department of Health and Social Care identifies as meeting the definition of Related Parties set out in IAS 24
(Related Party Transactions) are also deemed to be related parties of entities within the Departmental Group. We have reviewed the list of individuals
and entities and the CCG does not have any material disclosable transaction with any of the entities.
In addition, the NHS clinical commissioning group has had a number of material transactions with other government departments and other central
and local government bodies. Most of these transactions have been with Essex County Council (ECC).
Transactions with the chair, chief executive or members of the board of directors are shown in the remuneration report.
There are no other individuals who are considered to meet the definition of related parties under IAS24 as interpreted by the GAM 2022-23.
The Department of Health and Social Care is regarded as a related party. During the period the NHS clinical commissioning group has had a
significant number of material transactions with entities for which the Department is regarded as the parent Department:
The NHS clinical commissioning group has had a number of joint working arrangements and transactions with Essex clinical commissioning groups
such as Basildon and Brentwood CCG, Castle Point and Rochford CCG, Thurrock CCG, Southend CCG, North East Essex CCG and West Essex
CCG.
Page 26 of 32

NHS Mid Essex CCG - Statutory Accounts - 1-Apr-22 to 30-Jun-22
17 Events After the End of the Reporting Period
18 Financial Performance Targets
NHS clinical commissioning group have a number of financial duties under the NHS Act 2006 (as amended).
NHS clinical commissioning group performance against those duties was as follows:
1-Apr-22 to
30-Jun-22
1-Apr-22 to 30-
Jun-22
1-Apr-22 to
30-Jun-22
Target Performance Duty
£'000 £'000 achieved?
Expenditure not to exceed income 192,203 192,202 Yes
Revenue resource use does not exceed the amount specified in
Directions
192,026 192,025 Yes
Revenue administration resource use does not exceed the amount
specified in Directions
924 923 Yes
2021-22 2021-22 2021-22
Target Performance Duty
£'000 £'000 achieved?
Expenditure not to exceed income 929,272 929,017 Yes
Revenue resource use does not exceed the amount specified in
Directions
928,552 928,297 Yes
Revenue administration resource use does not exceed the amount
specified in Directions
7,808 7,789 Yes
The Health and Care Bill, as approved by Parliament on 28 April 22, approved the formation of Integrated Care
Boards and for them to take over the functions of Clinical Commissioning Groups. As a result, NHS Mid Essex CCG
dissolved on 30 June 22 and the Mid and South Essex Integrated Health and Care Board was formed from the
following day. In line with the provisions of the Group Accounting Manual the assets and liabilities of the CCG
transfered to the newly formed Integrated Care Board at book value. Further details are provided in the annual report
and in the accounting policies.
Page 27 of 32
INDEPENDENT AUDITOR’S REPORT TO THE MEMBERS OF THE
BOARD OF NHS MID & SOUTH ESSEX INTEGRATED CARE BOARD IN
RESPECT OF NHS MID ESSEX CLINICAL COMMISSIONING GROUP
REPORT ON THE AUDIT OF THE FINANCIAL STATEMENTS
Opinion
We have audited the financial statements of NHS Mid Essex Clinical Commissioning Group
(“the CCG”) for the three month period ended 30 June 2022 which comprise the Statement of
Comprehensive Net Expenditure, Statement of Financial Position, Statement of Changes in
Taxpayers’ Equity and Statement of Cash Flows, and the related notes, including the
accounting policies in note 1.
In our opinion the financial statements:
• give a true and fair view of the state of the CCG’s affairs as at 30 June 2022 and of its
income and expenditure for the three month period then ended; and
• have been properly prepared in accordance with the accounting policies directed by NHS
England with the consent of the Secretary of State on 22 June 2022 as being relevant to
CCGs in England and included in the Department of Health and Social Care Group
Accounting Manual 2022/23; and
• have been prepared in accordance with the requirements of the National Health Service
Act 2006 (as amended).
Basis for opinion
We conducted our audit in accordance with International Standards on Auditing (UK) (“ISAs
(UK)”) and applicable law. Our responsibilities are described below. We have fulfilled our
ethical responsibilities under and are independent of the CCG and NHS Mid & South Essex
Integrated Care Board (“the ICB”) in accordance with, UK ethical requirements including the
FRC Ethical Standard. We believe that the audit evidence we have obtained is a sufficient
and appropriate basis for our opinion.
Emphasis of matter – going concern
We draw attention to the disclosure made in note 1.1 to the financial statements which
explains that on 1 July 2022, NHS Mid Essex CCG was dissolved, and its services
transferred to NHS
Mid & South Essex Integrated Care Board. Under the continuation of
service principle the financial statements of the CCG have been prepared on a going concern
basis because its services will continue to be provided by the successor public sector entity.
Our opinion is not modified in respect of this matter.
Going concern
The Accountable Officer of the ICB (“the Accountable Officer”) has prepared the financial
statements on the going concern basis as the CCG has been dissolved and its services
transferred to another public sector entity, the ICB, and the Accountable Officer has not been
informed by the relevant national body of the intention to cease the services previously
provided by the CCG. They have also concluded that there are no material uncertainties that
could have cast significant doubt over its ability to continue as a going concern for at least a
year from the date of approval of the financial statements (“the going concern period”).
In our evaluation of the Accountable Officer’s conclusions, we considered the inherent risks
associated with the continuity of services provided by the CCG and transferred to the ICB
over the going concern period.
Our conclusions based on this work:
• we consider that the Accountable Officer’s use of the going concern basis of accounting
in the preparation of the financial statements is appropriate; and
Page 28 of 32
• we have not identified and concur with the Accountable Officer’s assessment that there is
not, a material uncertainty related to events or conditions that, individually or collectively,
may cast significant doubt on the CCG’s ability to continue as a going concern for the
going concern period.
However, as we cannot predict all future events or conditions and as subsequent events may
result in outcomes that are inconsistent with judgements that were reasonable at the time
they were made, the above conclusions are not a guarantee that the services provided by the
CCG will continue to be provided by the successor body.
Fraud a
nd breaches of laws and regulations – ability to detect
Identifying and responding to risks of material misstatement due to fraud
To identify risks of material misstatement due to fraud (“fraud risks”) we assessed events or
conditions that could indicate an incentive or pressure to commit fraud or provide an
opportunity to commit fraud. Our risk assessment procedures included:
• Enquiring of management, the Audit Committee of the successor ICB and internal audit
as to the CCG’s high-level policies and procedures to prevent and detect fraud, including
the internal audit function, , as well as whether they have knowledge of any actual,
suspected or alleged fraud.
• Reading Governing Body and Audit Committee minutes of the CCG.
• Using analytical procedures to identify any unusual or unexpected relationships.
We communicated identified fraud risks throughout the audit team and remained alert to any
indications of fraud throughout the audit.
As required by auditing standards, we performed procedures to address the risk of
management override of controls, in particular the risk that CCG management may be in a
position to make inappropriate accounting entries.
On this audit we did not identify a fraud risk related to revenue recognition because of the
nature of funding provided to the CCG, which is transferred from NHS England and
recognised through the Statement of Changes in Taxpayers’ Equity.
We did not i
dentify any additional fraud risks.
We performed procedures including:
• Identifying journal entries and other adjustments to test based on risk criteria and
comparing the identified entries to supporting documentation. These included unusual
doubl
e entries where one side included either Cash & Borrowings, or Revenue
Ident
ifying and responding to risks of material misstatement related to compliance with laws
and regulations
We identified areas of laws and regulations that could reasonably be expected to have a
material effect on the financial statements from our general sector experience and through
discussion with the Board of the CCG and ICB (as required by auditing standards), and from
inspection of the CCG’s regulatory and legal correspondence and discussed with the directors
and other management the policies and procedures regarding compliance with laws and
regulations.
We communic
ated identified laws and regulations throughout our team and remained alert to
any indications of non-compliance throughout the audit.
Page 29 of 32
The potential effect of these laws and regulations on the financial statements varies
considerably.
First
ly, the CCG is subject to laws and regulations that directly affect the financial statements
including the financial reporting aspects of NHS legislation We assessed the extent of
compliance with these laws and regulations as part of our procedures on the related financial
statement items.
Secondly, the CCG is subject to many other laws and regulations where the consequences of
non-compliance could have a material effect on amounts or disclosures in the financial
statements, for instance through the imposition of fines or litigation. We identified the
following areas as those most likely to have such an effect: health and safety, data protection
laws, anti-bribery, employment law recognising the regulated nature of the CCG’s activities.
Auditing standards limit the required audit procedures to identify non-compliance with these
laws and regulations to enquiry of the directors and inspection of regulatory and legal
correspondence, if any.
Therefore, if a breach of operational regulations is not disclosed to us
or evident from relevant correspondence, an audit will not detect that breach.
Context
of the ability of the audit to detect fraud or breaches of law or regulation
Owing to the inherent limitations of an audit, there is an unavoidable risk that we may not
have detected some material misstatements in the financial statements, even though we have
properly planned and performed our audit in accordance with auditing standards. For
example, the further removed non-compliance with laws and regulations is from the events
and transactions reflected in the financial statements, the less likely the inherently limited
procedures required by auditing standards would identify it.
In addition, as with any audit, there remained a higher risk of non-detection of fraud, as these
may involve collusion, forgery, intentional omissions, misrepresentations, or the override of
internal controls. Our audit procedures are designed to detect material misstatement. We are
not responsible for preventing non-compliance or fraud and cannot be expected to detect
non-compliance with all laws and regulations.
Other information in the Annual Report
The Accountable Officer is responsible for the other information, which comprises the
information included in the Annual Report, other than the financial statements and our
auditor’s report thereon. Our opinion on the financial statements does not cover the other
information and, accordingly, we do not express an audit opinion or, except as explicitly
stated below, any form of assurance conclusion thereon.
Our responsibility is to read the other information and, in doing so, consider whether, based
on our financial statements audit work, the information therein is materially misstated or
inconsistent with the financial statements or our audit knowledge. Based solely on that work:
• we have not identified material misstatements in the other information; and
• in our opinion the other information included in the Annual Report for the financial year is
consistent with the financial statements.
Annual Governance Statement
We are r
equired by the Code of Audit Practice published by the National Audit Office in April
2020 on behalf of the Comptroller and Auditor General (the “Code of Audit Practice”) to report
to you if the Annual Governance Statement has not been prepared in accordance with the
requirements of the Department of Health and Social Care Group Accounting Manual
2022/23. We have nothing to report in this respect.
Remuneration and Staff Reports
In our opinion the parts of the Remuneration and Staff Reports subject to audit have been
properly prepared, in all material respects, in accordance with the Department of Health and
Social Care Group Accounting Manual 2022/23.
Page 30 of 32

Accountable Officer’s responsibilities
As explained more fully in the statement set out on page 36, the Accountable Officer of the
ICB is responsible for the preparation of financial statements that give a true and fair view.
They are also responsible for such internal control as they determine is necessary to enable
the preparation of financial statements that are free from material misstatement, whether due
to fraud or error; assessing the CCG’s ability to continue as a going concern, disclosing, as
applicable, matters related to going concern; and using the going concern basis of accounting
unless they have been informed by the relevant national body of the intention to either cease
the services provided by the CCG or dissolve the CCG without the transfer of its services to
another public sector entity.
Auditor’s responsibilities
Our objectives are to obtain reasonable assurance about whether the financial statements as
a whole are free from material misstatement, whether due to fraud or error, and to issue our
opinion in an auditor’s report. Reasonable assurance is a high level of assurance, but does
not guarantee that an audit conducted in accordance with ISAs (UK) will always detect a
material misstatement when it exists. Misstatements can arise from fraud or error and are
considered material if, individually or in aggregate, they could reasonably be expected to
influence the economic decisions of users taken on the basis of the financial statements.
A fuller description of our responsibilities is provided on the FRC’s website at
www.frc.org.uk/auditorsresponsibilities
.
REPORT ON OTHER LEGAL AND REGULATORY MATTERS
Opinion on regularity
We are required to report on the following matters under Section 21(4) and (5) of the Local
Audit and Accountability Act 2014.
In our opinion, in all material respects, the expenditure and income recorded in the financial
statements have been applied to the purposes intended by Parliament and the financial
transactions conform to the authorities which govern them.
Report on the CCG’s arrangements for securing economy, efficiency and effectiveness
in its use of resources
Under the Code of Audit Practice, we are required to report if we identify any significant
weaknesses in the arrangements that have been made by the CCG to secure economy,
efficiency and effectiveness in its use of resources.
We have nothing to report in this respect.
Respective responsibilities in respect of our review of arrangements for securing
economy, efficiency and effectiveness in the use of resources
As explained more fully in the statement set out on page 36, the Accountable Officer is
responsible for ensuring that the CCG exercises its functions effectively, efficiently and
economically. We are required under section 21(1)(c) of the Local Audit and Accountability
Act 2014 to be satisfied that the CCG has made proper arrangements for securing economy,
efficiency and effectiveness in its use of resources.
We are not required to consider, nor have we considered, whether all aspects of the CCG’s
arrangements for securing economy, efficiency and effectiveness in the use of resources are
operating effectively.
We planned our work and undertook our review in accordance with the Code of Audit Practice
and related statutory guidance, having regard to whether the CCG had proper arrangements
in place to ensure financial sustainability, proper governance and to use information about
costs and performance to improve the way it manages and delivers its services. Based on our
risk assessment, we undertook such work as we considered necessary.
Page 31 of 32
Statutory reporting matters
We are required by Schedule 2 to the Code of Audit Practice to report to you if we refer a
matter to the Secretary of State and NHS England under section 30 of the Local Audit and
Accountability Act 2014 because we have reason to believe that the CCG, or an officer of the
CCG, is about to make, or has made, a decision which involves or would involve the body
incurring unlawful expenditure, or is about to take, or has begun to take a course of action
which, if followed to its conclusion, would be unlawful and likely to cause a loss or deficiency.
We have nothing to report in this respect.
THE PURPOSE OF OUR AUDIT WORK AND TO WHOM WE OWE OUR
RESPONSIBILITIES
This report is made solely to the Members of the Board of NHS Mid and South Essex
Integrated Care Board in respect of NHS Mid Essex CCG, as a body, in accordance with Part
5 of the Local Audit and Accountability Act 2014. Our audit work has been undertaken so
that we might state to the Members of the Board of the ICB, as a body, those matters we are
required to state to them in an auditor’s report and for no other purpose. To the fullest extent
permitted by law, we do not accept or assume responsibility to anyone other than the
Members of the Board of the ICB, as a body, for our audit work, for this report or for the
opinions we have formed.
CERTIFICATE OF COMPLETION OF THE AUDIT
We certify that we have completed the audit of the accounts of NHS Mid Essex CCG for the
three month period ended 30 June 2022 in accordance with the requirements of the Local
Audit and Accountability Act 2014 and the Code of Audit Practice.
Emma Larcombe
for and on behalf of KPMG LLP
Chartered Accountants
Dragonfly House
2 Gilders Way
Norwich
NR3 1UB
28 June 2023
Page 32 of 32
