
1

2
National Cancer Database
Participant User File
2020 Data Dictionary
Includes patients diagnosed in 2004-2020
Contact NCDB_PU[email protected] with any questions about the data items. The CoC reserves the right to
modify or update this Data Dictionary as or when the need arises.
Revised September 2022
3
Table of Contents
Layout of Data Dictionary Items ......................................................................................................... 11
Facility and Patient Demographics ......................................................................................................... 13
Case Key ............................................................................................................................................ 14
Facility Key ........................................................................................................................................ 15
Facility Type ....................................................................................................................................... 16
Facility Location ................................................................................................................................. 17
Patient Treated in More than One CoC Facility Flag............................................................................ 18
Reference Date Flag ........................................................................................................................... 19
Age at Diagnosis ................................................................................................................................ 20
Sex .................................................................................................................................................... 21
Race .................................................................................................................................................. 22
Spanish/Hispanic Origin ..................................................................................................................... 24
Primary Payor at Diagnosis ................................................................................................................ 26
Percent No High School Degree Quartiles 2000 .................................................................................. 27
Percent No High School Degree Quartiles 2008-2012 ......................................................................... 28
Percent No High School Degree Quartiles 2012-2016 ......................................................................... 29
Percent No High School Degree Quartiles 2016-2020 ......................................................................... 30
Median Income Quartiles 2000 .......................................................................................................... 31
Median Income Quartiles 2008-2012 ................................................................................................. 32
Median Income Quartiles 2012-2016 ................................................................................................. 33
Median Income Quartiles 2016-2020 ................................................................................................. 34
Urban/Rural 2003 .............................................................................................................................. 35
Urban/Rural 2013 .............................................................................................................................. 37
Medicaid Expansion Status State Group ............................................................................................. 39
Great Circle Distance ......................................................................................................................... 40
Charlson-Deyo Score.......................................................................................................................... 41
NCDB--SARSCoV2--Pos ....................................................................................................................... 43
Elapsed Days from DX to Date of First Positive COVID Test ................................................................. 44
4
NCDB--SARSCoV2--Test ...................................................................................................................... 45
Cancer Identification ............................................................................................................................. 46
Sequence Number ............................................................................................................................. 47
Class of Case ...................................................................................................................................... 49
Year of Diagnosis ................................................................................................................................ 51
Primary Site ....................................................................................................................................... 52
Laterality ........................................................................................................................................... 53
Histology ........................................................................................................................................... 56
Behavior Code ................................................................................................................................... 57
Grade/Differentiation ........................................................................................................................ 59
Grade/Differentiation 2018+ ............................................................................................................. 61
Diagnostic Confirmation .................................................................................................................... 63
Regional Lymph Nodes Examined ....................................................................................................... 67
Regional Lymph Nodes Positive .......................................................................................................... 70
Sentinel Lymph Nodes Examined ....................................................................................................... 73
Sentinel Lymph Nodes Positive .......................................................................................................... 75
Sentinel Lymph Node Biopsy, Days from Diagnosis ............................................................................ 78
Regional Lymph Node Dissection, Days from Diagnosis ...................................................................... 79
Surgical Diagnostic and Staging Procedure ......................................................................................... 80
Surgical Diagnostic and Staging Procedure at this Facility ................................................................... 82
Surgical Diagnostic and Staging Procedure, Days from Dx .................................................................. 84
Stage of Disease: Traditional AJCC Staging System ................................................................................. 85
AJCC Clinical T .................................................................................................................................... 86
AJCC Clinical N ................................................................................................................................... 88
AJCC Clinical M .................................................................................................................................. 90
AJCC Clinical Stage Group ................................................................................................................... 92
AJCC Pathologic T .............................................................................................................................. 94
AJCC Pathologic N .............................................................................................................................. 96
AJCC Pathologic M ............................................................................................................................. 99
5
AJCC Pathologic Stage Group ........................................................................................................... 101
TNM Edition Number ....................................................................................................................... 103
NCDB Analytic Stage Group .............................................................................................................. 104
Mets at Diagnosis – Bone ................................................................................................................. 105
Mets at Diagnosis – Brain................................................................................................................. 106
Mets at Diagnosis – Liver ................................................................................................................. 107
Mets at Diagnosis – Lung ................................................................................................................. 108
Mets at Diagnosis – Other ................................................................................................................ 109
Mets at Diagnosis - Distant Lymph Nodes ........................................................................................ 113
Tumor Size Summary ....................................................................................................................... 117
Stage of Disease .................................................................................................................................. 121
AJCC 8
th
Edition Staging System ........................................................................................................... 121
AJCC 8
th
Edition Clinical T ................................................................................................................. 122
AJCC TNM Clin T Suffix ..................................................................................................................... 124
AJCC 8
th
Edition Clinical N ................................................................................................................ 126
AJCC TNM Clin N Suffix .................................................................................................................... 128
AJCC 8
th
Edition Clinical M ................................................................................................................ 130
AJCC 8
th
Edition Clinical Stage Group ................................................................................................ 132
AJCC 8
th
Edition Pathologic T ............................................................................................................ 134
AJCC TNM Path T Suffix .................................................................................................................... 136
AJCC 8
th
Edition Pathologic N ........................................................................................................... 138
AJCC TNM Path N Suffix ................................................................................................................... 140
AJCC 8
th
Edition Pathologic M .......................................................................................................... 141
AJCC 8
th
Edition Pathologic Stage Group .......................................................................................... 143
AJCC TNM Post Therapy Path (yp) T ................................................................................................. 145
AJCC TNM Post Therapy Path (yp) T Suffix ........................................................................................ 147
AJCC TNM Post Therapy Path (yp) N ................................................................................................ 149
AJCC TNM Post Therapy Path (yp) N Suffix ....................................................................................... 151
AJCC Post Therapy Path (yp) M ........................................................................................................ 153
6
AJCC TNM Post Therapy Path (yp) Stage Group ................................................................................ 155
Stage of Disease: Collaborative Stage Data Collection System .............................................................. 157
CS Site-Specific Factors 1-25 ............................................................................................................ 158
CS Version Derived ........................................................................................................................... 161
Site Specific Code Definitions for Data Items from the Collaborative Stage Data Collection System 162
CS Extension .................................................................................................................................... 163
CS Tumor Size/Ext Eval..................................................................................................................... 164
Lymph-Vascular Invasion ................................................................................................................. 165
CS Mets at DX .................................................................................................................................. 167
CS Mets at DX-Bone ......................................................................................................................... 168
CS Mets at DX-Liver ......................................................................................................................... 170
CS Mets at DX-Lung ......................................................................................................................... 172
CS Mets at DX-Brain ......................................................................................................................... 174
CS Mets Eval .................................................................................................................................... 176
CS Tumor Size .................................................................................................................................. 177
Site Specific Data Items (SSDIs) ............................................................................................................ 178
Site Specific Data Items (SSDIs) ........................................................................................................ 179
Treatment ........................................................................................................................................... 180
RX Summ Treatment Status ............................................................................................................. 181
Treatment Started, Days from Dx ..................................................................................................... 182
Treatment: Surgery ............................................................................................................................. 183
First Surgical Procedure, Days from Dx ............................................................................................. 184
Definitive Surgical Procedure, Days from Dx..................................................................................... 185
Surgical Procedure of Primary Site .................................................................................................... 186
Surgical Procedure of Primary Site at This Facility ............................................................................ 188
Approach – Surgery of the Primary Site at this Facility ..................................................................... 190
Surgical Margins of the Primary Site ................................................................................................ 191
Scope of Regional Lymph Node Surgery ........................................................................................... 193
Scope of Regional Lymph Node Surgery 2012 .................................................................................. 195
Surgical Procedure Other Site .......................................................................................................... 201
7
Surgical Inpatient Stay, Days from Surgery ....................................................................................... 203
Readmission to the Same Hospital within 30 Days of Surgical Discharge .......................................... 204
Reason for No Surgery of Primary Site ............................................................................................. 205
Treatment: Radiation .......................................................................................................................... 207
Radiation, Days from Dx................................................................................................................... 208
Location of Radiation Therapy ......................................................................................................... 209
Phase I Radiation Primary Treatment Volume .................................................................................. 210
Phase I Radiation to Draining Lymph Nodes ..................................................................................... 218
Phase I Radiation Treatment Modality ............................................................................................. 220
Phase I External Beam Radiation Planning Technique....................................................................... 223
Phase I Dose per Fraction ................................................................................................................ 228
Phase I Number of Fractions ............................................................................................................ 231
Phase I Total Dose ........................................................................................................................... 233
Phase II Radiation Primary Treatment Volume ................................................................................. 236
Phase II Radiation to Draining Lymph Nodes .................................................................................... 244
Phase II Radiation Treatment Modality ............................................................................................ 246
Phase II External Beam Radiation Planning Technique...................................................................... 249
Phase II Dose per Fraction................................................................................................................ 254
Phase II Number of Fractions ........................................................................................................... 257
Phase II Total Dose .......................................................................................................................... 260
Phase III Radiation Primary Treatment Volume ................................................................................ 263
Phase III Radiation to Draining Lymph Nodes ................................................................................... 271
Phase III Radiation Treatment Modality ........................................................................................... 273
Phase III External Beam Radiation Planning Technique ..................................................................... 276
Phase III Dose per Fraction............................................................................................................... 280
Phase III Number of Fractions .......................................................................................................... 283
Phase III Total Dose ......................................................................................................................... 286
Number of Phases of Radiation Treatment to this Volume ............................................................... 289
Radiation Treatment Discontinued Early .......................................................................................... 291
8
Total Dose ....................................................................................................................................... 293
Radiation/Surgery Sequence ............................................................................................................ 295
Radiation Ended, Days from Start of Radiation ................................................................................. 298
Reason for No Radiation .................................................................................................................. 299
Treatment: Systemic............................................................................................................................ 301
Systemic, Days from Dx .................................................................................................................... 302
Chemotherapy ................................................................................................................................. 303
Chemotherapy at this Facility........................................................................................................... 306
Chemotherapy, Days from Dx ........................................................................................................... 308
Hormone Therapy ............................................................................................................................ 309
Hormone Therapy at This Facility ..................................................................................................... 311
Hormone Therapy, Days from Dx ...................................................................................................... 313
Immunotherapy ............................................................................................................................... 314
Immunotherapy at this Facility ........................................................................................................ 316
Immunotherapy, Days from Dx ........................................................................................................ 318
Hematologic Transplant and Endocrine Procedures .......................................................................... 319
Systemic/Surgery Sequence ............................................................................................................. 322
Treatment: Other Treatment ............................................................................................................... 324
Other Treatment.............................................................................................................................. 325
Other Treatment at this Facility ........................................................................................................ 327
Other Treatment, Days from Dx ........................................................................................................ 329
Palliative Care .................................................................................................................................. 330
Palliative Care at and this Facility ..................................................................................................... 332
Outcomes ............................................................................................................................................ 334
Thirty Day Mortality ......................................................................................................................... 335
Ninety Day Mortality ....................................................................................................................... 336
Last Contact or Death, Months from Dx ........................................................................................... 337
Vital Status....................................................................................................................................... 338
Appendix A: Site-Specific Surgery Codes .............................................................................................. 339
Oral Cavity ....................................................................................................................................... 340
9
Parotid and Other Unspecified Glands .............................................................................................. 342
Pharynx ........................................................................................................................................... 344
Esophagus ....................................................................................................................................... 346
Stomach .......................................................................................................................................... 348
Colon ............................................................................................................................................... 350
Rectosigmoid ................................................................................................................................... 352
Rectum ............................................................................................................................................ 354
Anus ................................................................................................................................................ 356
Liver and Intrahepatic Bile Ducts ...................................................................................................... 358
Pancreas .......................................................................................................................................... 360
Larynx .............................................................................................................................................. 361
Lung ................................................................................................................................................ 363
Hematopoietic/Reticuloendothelial/Immunoproliferative/Myeloproliferative Disease .................... 365
Bones, Joints and Articular Cartilage, Peripheral Nerves and Autonomic Nervous System, and
Connective, Subcutaneous and Other Soft Tissues ........................................................................... 366
Spleen ............................................................................................................................................. 367
Skin ................................................................................................................................................. 368
Breast .............................................................................................................................................. 370
Cervix Uteri...................................................................................................................................... 373
Corpus Uteri .................................................................................................................................... 375
Ovary ............................................................................................................................................... 377
Prostate ........................................................................................................................................... 379
Testis ............................................................................................................................................... 381
Kidney, Renal Pelvis, and Ureter ....................................................................................................... 382
Bladder ............................................................................................................................................ 384
Brain ................................................................................................................................................ 386
Thyroid Gland .................................................................................................................................. 387
Lymph Nodes ................................................................................................................................... 388
All Other Sites .................................................................................................................................. 389
11
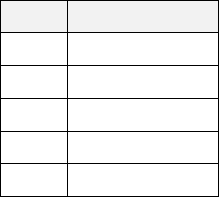
Layout of Data Dictionary Items
Each data item in the Data Dictionary includes the following elements:
Data Dictionary Category
Each item is categorized into one of ten groups: Facility and Patient Demographics, Cancer Identification,
Stage of Disease Traditional AJCC Staging System, Stage of Disease Collaborative Stage Data Collection
System, Treatment, Treatment: Surgery, Treatment: Radiation, Treatment: Systemic, Treatment: Other
Treatment, and Outcomes.
Information about the Collaborative Stage (CS) system can be accessed by the links on the PUF web
page.
PUF Data Item Name
Identifies the name applied to the data item in the distributed PUF file syntax.
NAACCR Item Number
The North American Association of Central Cancer Registries (NAACCR) facilitates standards for data
collection and transmission among and between hospital, state, regional and national cancer registries
(Standards for Cancer Registries Volume II: Data Standards and Data Dictionary). Links to the NAACR
and other registry manuals are found on the Links section on the PUF web page. Each item in the PUF is
either drawn directly from data reported from CoC-accredited cancer program registries, in which case
the NAACCR Item # is provided for investigators to identify documentation related to this item in other
coding manuals, or references that are commonly used across the cancer registry surveillance system in
the United States and Canada.
In some cases, no NAACCR item # is provided. These items have been linked from other data sources
available to the CoC/NCDB or have been derived by the NCDB from data provided from the reporting
cancer registries.
Diagnosis Years Available
Identifies the diagnosis year(s) the data item was available in the PUF.
Length
The total number of characters used by the item.
Allowable Values
The value(s) or range of values coded in the item.
12
Description
A working description of the item.
Registry Coding Instructions
A detailed account of the coding directives provided to cancer registrars in the FORDs manual. Derived
variables or variables not in the FORDs manual will have no instructions.
Analytic Note
On occasion, additional information is made available that may indicate where added information
related to the item may be located, whether the item is only available in the PUF for certain diagnosis
years, or if experience from previous analytic work with the item warrants special attention or possible
consideration by investigators.
Codes /Definitions
The list of code and the code labels for the data item are provided.
The information provided in this PUF Data Dictionary should be used by investigators applying for access
to the NCDB PUF, and when conducting analyses of the data. Successful candidates will receive access
to a PUF that will be issued by the American College of Surgeons’ (ACoS) Commission on Cancer (CoC) in
2020. This document represents the current set of items expected to be released. The CoC reserves the
right to modify or update this or any other resource as or when the need arises.
13
Facility and Patient Demographics
14
Case Key
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: PUF_CASE_ID
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 37
Allowable Values: Alphanumeric (uppercase and lowercase)
Description:
Unique case identification number assigned to the case in the PUF.
Registry Coding Instructions: Not applicable.
Analytic Note:
NCDB assigned value that uniquely identifies each case included in the PUF. The value
assigned to each case is selected at random, and the value assigned to each case will
change with each issued PUF. The PUF Case Keys are not the same across cancer sites,
and cases cannot be linked across cancer sites.
Note that the length of this key was expanded from 10 to 37 in January 2014.
15
Facility Key
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: PUF_FACILITY_ID
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 10
Allowable Values: Alphanumeric (uppercase)
Description:
The facility reporting the case to the NCDB. Codes are anonymized. The random Facility
Keys are assigned regardless of cancer site, so you may identify the same facilities
across cancer sites.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.

16
Facility Type
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: FACILITY_TYPE_CD
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
Each facility reporting cases to the NCDB is assigned a category classification by the
Commission on Cancer Accreditation program. This item provides a general
classification of the structural characteristics of each reporting facility.
Registry Coding Instructions: Not applicable.
Analytic Note:
For additional information about CoC accreditation categories see:
https://www.facs.org/quality-programs/cancer/coc/accreditation/categories.
See "Privacy Rule and Patient Case Records” document for a description of the handling
of some categories.
This item is suppressed for cases aged 0-39.
Code
Definition
1
Community Cancer Program
2
Comprehensive Community Cancer Program
3
Academic/Research Program (includes NCI-designated comprehensive
cancer centers)
4
Integrated Network Cancer Program
blank
Not available

17
Facility Location
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: FACILITY_LOCATION_CD
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
A
llowable Values: 1 -
9
, blank
D
escription: The US Census Division of the reporting facility.
Registry Coding Instructions: Not applicable.
Analytic Note: This item is suppressed for cases aged 0-39.
Code
Definition
State Grouping
1
New England
CT, MA, ME, NH, RI, VT
2
Middle Atlantic
NJ, NY, PA
3
South Atlantic
DC, DE, FL, GA, MD, NC, SC, VA, WV
4
East North Central
IL, IN, MI, OH, WI
5
East South Central
AL, KY, MS, TN
6
West North Central
IA, KS, MN, MO, ND, NE, SD
7
West South Central
AR, LA, OK, TX
8
Mountain
AZ, CO, ID, MT, NM, NV, UT, WY
9
Pacific
AK, CA, HI, OR, WA
blank
Not available
Not available

18
Patient Treated in More than One CoC Facility Flag
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: PUF_MULT_SOURCE
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0, 1
Description:
Identifies whether there was more than one CoC facility that submitted a report for this
case to NCDB.
Registry Coding Instructions: Not applicable.
Analytic Note:
All CoC accredited programs that initially diagnose a patient or that provide all or part of
first course treatment report the case. If more than one facility submitted a report, the
"best" is provided in the PUF file based on the recency of patient contact with the
program, completeness of coded detail, and/or edit quality, where differences exist.
The record used in the case of ties is arbitrary. If this item is coded 0, only one facility
provided a report for this cancer.
This item is used for hospital level comparisons, surgical volume, distance or other
hospital level computations in order to take into account cases treated at more than
one hospital.
If a patient received treatment in an outpatient facility or a non-CoC accredited facility,
they could still have a code of 0 for this variable, if only one record for this patient was
submitted to the NCDB. For these patients, they could have a Summary Treatment
variable indicating that they received treatment (for example Chemotherapy = 1, 2 or
3), but the hospital level treatment variable could indicate that no treatment was
received at the facility included in the PUF (for example Chemotherapy at this Facility =
0). This would occur if a patient was diagnosed and/or treated in only one CoC facility
but received treatment in an outpatient setting or in a non-CoC facility.
Code
Definition
0
Only one CoC facility reported this case to NCDB
1
Records pertaining to this case submitted to NCDB
by more than one CoC facility

19
Reference Date Flag
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: PUF_REFERENCE_DATE_FLAG
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0, 1
Description:
Identifies whether a report for a case has a diagnosis date before or after the facility's
reference date.
Registry Coding Instructions: Not applicable.
Analytic Note:
Every facility has a reference date, from which they are accountable for the
completeness of the data for cases diagnosed in that year through the present. Since a
facility may request to move their reference date forward, there are some instances
where a case’s diagnosis year falls before the facility’s reference date. This item is coded
0 in cases where this occurs. A value of 1 signifies cases where the diagnosis year is on
or after the reference date year. Reports for cases whose diagnosis date is prior to the
reference date cannot be changed or updated by the facility. For this reason, PUF
researchers may choose to omit cases where the diagnosis date precedes the reference
date, depending on the nature of the study.
Code
Definition
0
Diagnosis date before reference date
1
Diagnosis date on or after reference date

20
Age at Diagnosis
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: AGE
NAACCR Item #: 230
Diagnosis Years Available: 2004 +
Length: 3
Allowable Values: 000 - 090, 999
Description:
Records the age of the patient at his or her last birthday before diagnosis.
Registry Coding Instructions:
If the patient has multiple primaries, then the age at diagnosis may be different for
subsequent primaries.
Analytic Note:
In utero Date of Initial Diagnosis (NAACCR Item #390) was coded as equal to the Date
of Birth (NAACCR Item #240) in the past. Beginning in 2009, assignment is to the pre-
birth date on which the diagnosis occurs. Age at Diagnosis is assigned 000 for these
cases. For compliance with HIPAA privacy requirements, all patients age 90 or over at
diagnosis are shown as 090.
Code
Definition
000
Less than one year old, or diagnosed in utero
001 - 089
One to eighty nine years old
090
Ninety or older
999
Age at diagnosis unknown

21
Sex
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: SEX
NAACCR Item#: 220
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1, 2
Description:
Record the patient’s sex as indicated in the medical record.
Registry Coding Instructions: None
Analytic Note:
Due to low case counts, any sex other than male or female is suppressed
in the PUF data.
Code
Definition
1
Male
2
Female
22
Race
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: RACE
NAACCR Item #: 160
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 01 - 08, 10 - 17, 20 - 22, 25 - 28, 30 - 32, 96 - 99
Description:
Identifies the primary race of the person.
Registry Coding Instructions:
Race is analyzed with Spanish Origin (NAACCR Item #190). Both items must be
recorded. All tumors for the same patient should have the same race code.
Codes 08-13 became effective with diagnoses on or after January 1, 1988. Code 14
became effective with diagnoses on or after January 1, 1994.
Codes 15 was changed from 09 and split into 16 and 17 in 2010; converted cases are
likely to appear as 15.
Codes 20-97 became effective with diagnoses on or after January 1, 1991. SEER
participants in San Francisco, San Jose, Monterey, and Los Angeles are permitted to use
codes 14 and 20-97 for cases diagnosed after January 1, 1987.
Analytic Note:
Beginning in 2001 cancer registries recorded multiple race codes, as many as five. These
additional race codes are infrequently reported and are not provided as part of this file.

23
Race continued
Code
Definition
01
White
02 Black
03
American Indian, Aleutian, or Eskimo
04
Chinese
05
Japanese
06
Filipino
07
Hawaiian
08 Korean
10
Vietnamese
11
Laotian
12
Hmong
13
Kampuchean (including Khmer and Cambodian)
14
Thai
15
Asian Indian or Pakistani, NOS (formerly code 09)
16
Asian Indian
17 Pakistani
20
Micronesian, NOS
21
Chamorran
22
Guamanian, NOS
25
Polynesian, NOS
26
Tahitian
27 Samoan
28
Tongan
30
Melanesian, NOS
31
Fiji Islander
32
New Guinean
96
Other Asian, including Asian, NOS and Oriental, NOS
97 Pacific Islander, NOS
98
Other
99
Unknown
24
Spanish/Hispanic Origin
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name:
SPANISH_HISPANIC_ORIGIN
NAACCR Item #: 190
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 9
Description:
Identifies persons of Spanish or Hispanic origin.
Registry Coding Instructions:
Persons of Spanish or Hispanic origin may be of any race, but these
categories are
generally not used for Native Americans, Filipinos, or others
who may have Spanish
names.
Code 0 (Non Spanish, Non-Hispanic) for Portuguese and Brazilian persons.
If the patient
has multiple tumors, all records should have the same code.
Analytic Note: None.

25
Spanish/Hispanic Origin continued
Code
Definition
0
Non-Spanish, Non-Hispanic
1
Mexican (includes Chicano)
2
Puerto Rican
3
Cuban
4
South or Central America (except Brazil)
5
Other Specified Spanish/Hispanic
Origin (includes European;
excludes Dominican Republic)
6
Spanish, NOS; Hispanic, NOS;
Latino, NOS (There is evidence
other
than surname or maiden name
that the person is Hispanic, but
he/she cannot be assigned to any
category of 1 - 5)
7
Spanish surname only (The only
evidence of the person's Hispanic
origin is surname or maiden name,
and there is no contrary evidence
that the person is not Hispanic)
8
Dominican Republic (for use with
patients who were diagnosed with
cancer on January 1, 2005, or later)
9
Unknown whether of Spanish/Hispanic origin; not stated in patient
record

26
Primary Payor at Diagnosis
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: INSURANCE_STATUS
NAACCR Item #: 630
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 0 - 4, 9
Description:
Identifies the patient's primary insurance carrier at the time of initial diagnosis and/or
treatment.
Registry Coding Instructions:
Record the type of insurance reported on the patient's admission page. If more than one
payer or insurance carrier is listed on the patient's admission page record the first. If
the patient's payer or insurance carrier changes, do not change the initially recorded
code.
Analytic Note: The category Medicare with Supplemental insurance is only reported for patients
diagnosed on or after January 1, 2006. Insurance codes are combined for some NAACCR categories.
Code Definition Corresponding NAACCR # 630 Codes
0 Not Insured 01, 02
1 Private Insurance / Managed Care 10, 20, 21
2 Medicaid 31, 35
3 Medicare 60-64
4 Other Government 65-68
9 Insurance Status Unknown 99

27
Percent No High School Degree Quartiles 2000
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: NO_HSD_QUAR_00
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
This measure of educational attainment for each patient's area of residence is
estimated by matching the zip code of the patient recorded at the time of diagnosis
against files derived from year 2000 US Census data. This item provides a measure of
the number of adults in the patient's zip code who did not graduate from high school,
and is categorized as equally proportioned quartiles among all US zip codes.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
29.0% +
2
20.0% - 28.9%
3
14.0%-19.9%
4
< 14.0%
blank
Not available

28
Percent No High School Degree Quartiles 2008-2012
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: NO_HSD_QUAR_12
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
This measure of educational attainment for each patient's area of residence is estimated
by matching the zip code of the patient recorded at the time of diagnosis against files
derived from the 2012 American Community Survey data, spanning years 2008-2012.
This item provides a measure of the number of adults in the patient's zip code who did
not graduate from high school, and is categorized as equally proportioned quartiles
among all US zip codes. Comparisons with Census 2000 education data may be done.
See https://www.census.gov/acs/ for more information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
21.0% +
2
13.0% - 20.9%
3
7.0%-12.9%
4
< 7.0%
blank
Not available

29
Percent No High School Degree Quartiles 2012-2016
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: NO_HSD_QUAR_2016
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
This measure of educational attainment for each patient's area of residence is estimated
by matching the zip code of the patient recorded at the time of diagnosis against files
derived from the 2016 American Community Survey data, spanning years 2012-2016.
This item provides a measure of the number of adults age 25 or older in the patient's zip
code who did not graduate from high school, and is categorized as equally proportioned
quartiles among all US zip codes. See https://www.census.gov/acs/ for more
information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
17.6% +
2
10.9% - 17.5%
3
6.3% - 10.8%
4
< 6.3%
blank
Not available
30
Percent No High School Degree Quartiles 2016-2020
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: NO_HSD_QUAR_2020
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
This measure of educational attainment for each patient's area of residence is estimated
by matching the zip code of the patient recorded at the time of diagnosis against files
derived from the 2020 American Community Survey data, spanning years 2016-2020.
This item provides a measure of the number of adults age 25 or older in the patient's zip
code who did not graduate from high school, and is categorized as equally proportioned
quartiles among all US zip codes. See https://www.census.gov/acs/ for more
information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
15.3% +
2
9.1% - 15.2%
3
5.0% - 9.0%
4
< 5.0%
blank
Not available

31
Median Income Quartiles 2000
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: MED_INC_QUAR_00
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
Median household income for each patient's area of residence is estimated by
matching the zip code of the patient recorded at the time of diagnosis against files
derived from year 2000 US Census data. Household income is categorized as quartiles
based on equally proportioned income ranges among all US zip codes.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
< $30,000
2
$30,000 - $34,999
3
$35,000 - $45,999
4
$46,000 +
blank
Not available

32
Median Income Quartiles 2008-2012
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: MED_INC_QUAR_12
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
Median household income for each patient's area of residence is estimated by
matching the zip code of the patient recorded at the time of diagnosis against files
derived from the 2012 American Community Survey data, spanning years 2008-2012
and adjusted for 2012 inflation. Household income is categorized as quartiles based on
equally proportioned income ranges among all US zip codes. Due to differences in
collection methodology, comparisons with Census 2000 income data should be done
with caution. See https://www.census.gov/acs/ for more information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
< $38,000
2
$38,000 - $47,999
3
$48,000 - $62,999
4
$63,000 +
blank
Not available

33
Median Income Quartiles 2012-2016
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: MED_INC_QUAR_2016
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
Median household income for each patient's area of residence is estimated by matching
the zip code of the patient recorded at the time of diagnosis against files derived from
the 2016 American Community Survey data, spanning years 2012-2016 and adjusted for
2016 inflation. Household income is categorized as quartiles based on equally
proportioned income ranges among all US zip codes. See https://www.census.gov/acs/
for more information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
< $40,227
2
$40,227 - $50,353
3
$50,354 - $63,332
4
$63,333 +
blank
Not available

34
Median Income Quartiles 2016-2020
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: MED_INC_QUAR_2020
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 4, blank
Description:
Median household income for each patient's area of residence is estimated by matching
the zip code of the patient recorded at the time of diagnosis against files derived from
the 2020 American Community Survey data, spanning years 2016-2020 and adjusted for
2020 inflation. Household income is categorized as quartiles based on equally
proportioned income ranges among all US zip codes. See https://www.census.gov/acs/
for more information.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
1
< $46,277
2
$46,277 - $57,856
3
$57,857 - $74,062
4
$74,063 +
blank
Not available
35
Urban/Rural 2003
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: UR_CD_03
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 9, blank
Description:
Area-based measure of rurality and urban influence, using the typology published by
the USDA Economic Research Service.
Registry Coding Instructions: Not applicable
Analytic Note:
This item was estimated by matching the state and county FIPS code of the patient
recorded at the time of diagnosis against 2003 files published by the United States
Department of Agriculture Economic Research Service at:
https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.
Rural-Urban continuum codes form a classification scheme that distinguishes
metropolitan (metro) counties by the population size of their metro area, and
nonmetropolitan (non-metro) counties by degree of urbanization and adjacency to a
metro area or areas. The metro and non-metro categories have been subdivided into
three metro and six non-metro groupings, resulting in a nine-part county codification.
The codes allow researchers working with data to break such data into finer residential
groups beyond a simple metro/non-metro dichotomy, particularly for the analysis of
trends in non-metro areas that may be related to degree of rurality and metro
proximity.

36
Urban/Rural 2003 continued
Code Definition
Rural Urban
Grouping
1
Counties in metro areas of 1 million population or more
Metro
2
Counties in metro areas of 250,000 to 1 million population
Metro
3
Counties in metro areas of fewer than 250,000 population
Metro
4
Urban population of 20,000 or more, adjacent to a metro area
Urban
5
Urban population of 20,000 or more, not adjacent to a metro area
Urban
6
Urban population of 2,500 to 19,999, adjacent to a metro area
Urban
7
Urban population of 2,500 to 19,999, not adjacent to a metro area.
Urban
8
Completely rural or less than 2,500 urban population, adjacent to a metro area
Rural
9
Completely rural or less than 2,500 urban population, not adjacent to a metro area
Rural
blank
Not available
Not available
37
Urban/Rural 2013
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: UR_CD_13
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 9, blank
Description:
Area-based measure of rurality and urban influence, using the typology published by the
USDA Economic Research Service.
Registry Coding Instructions: Not applicable.
Analytic Note:
This item was estimated by matching the state and county FIPS code of the patient
recorded at the time of diagnosis against 2013 files published by the United States
Department of Agriculture Economic Research Service (https://www.ers.usda.gov/data-
products/rural-urban-continuum-codes/ ).
Rural-Urban continuum codes form a classification scheme that distinguishes
metropolitan (metro) counties by the population size of their metro area, and
nonmetropolitan (non-metro) counties by degree of urbanization and adjacency to a
metro area or areas. The metro and non-metro categories have been subdivided into
three metro and six non-metro groupings, resulting in a nine part county codification.
The codes allow researchers working with data to break such data into finer residential
groups beyond a simple metro/non-metro dichotomy, particularly for the analysis of
trends in non-metro areas that may be related to degree of rurality and metro
proximity.
Since labels for the 2013 classification codes are the same as the 2003 labels, a direct
comparison with the 2003 Urban/Rural codes may be made.

38
Urban/Rural 2013 continued
Code Definition
Rural Urban
Grouping
1
Counties in metro areas of 1 million population or more
Metro
2
Counties in metro areas of 250,000 to 1 million population
Metro
3
Counties in metro areas of fewer than 250,000 population
Metro
4
Urban population of 20,000 or more, adjacent to a metro area
Urban
5
Urban population of 20,000 or more, not adjacent to a metro area
Urban
6
Urban population of 2,500 to 19,999, adjacent to a metro area
Urban
7
Urban population of 2,500 to 19,999, not adjacent to a metro area
Urban
8
Completely rural or less than 2,500 urban population, adjacent to a metro area
Rural
9
Completely rural or less than 2,500 urban population, not adjacent to a metro area
Rural
blank
Not available
Not available

39
Medicaid Expansion Status State Group
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: PUF_MEDICAID_EXPN_CODE
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3, 9, blank
Description:
Patient State at Diagnosis Grouped by Medicaid Expansion Status 2010 +
Registry Coding Instructions: Not applicable.
Analytic Note: This variable is suppressed for ages 0-39.
Code
Definition
State Grouping
0 Non-Expansion States
TN, NC, ID, GA, FL, MO, AL, MS, KS, TX, WI,
UT, SC, SD, VA, OK, NE, WY, ME
1 January 2014 Expansion States
KY, NV, CO, OR, NM, WV, AR, RI, AZ, MD,
MA, ND, OH, IA, IL, VT, HI, NY, DE
2
Early Expansion States (2010-2013)
WA, CA, NJ, MN, DC, CT
3
Late Expansion States (after Jan. 2014)
NH, IN, MI, PA, AK, MT, LA
9
Suppressed for Ages 0-39
Not available
blank
State Missing or Out of U.S.
Not available
Reference: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-
decisions-interactive-map/
40
Great Circle Distance
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: CROWFLY
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: Numeric (0-999999.9), blank
Description:
The "great circle" distance in miles between the patient's residence and the hospital
that reported the case.
Registry Coding Instructions: Not applicable.
Analytic Note:
Residential latitude and longitude are based on the patient's zip code centroid or on
the city if the zip code was not available. Hospital locations are based on the street
address for the facility. The great circle distance is calculated between those two
points. In some instances, the residential city is outside of the United States, so the
upper bound of distance may be quite large. A distance of 0 can result when the
patient lives in the same zip code where the facility is located.
The Haversine (half-versed-sine) formula is used to calculate the distance between the
two locations. It was published by R W Sinnott in Sky and Telescope, 1984, though
known about for much longer by navigators.

41
Charlson-Deyo Score
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: CDCC_TOTAL_BEST
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 ‐ 3
Description:
Comorbid conditions as described by Charlson-Deyo (1992)
1
are mapped from as many
as ten reported ICD‐9‐CM or ICD‐10 secondary diagnosis codes. The Charlson-Deyo
value is a weighted score derived from the sum of the scores for each of the comorbid
conditions listed in the Charlson Comorbidity Score Mapping Table.
The range for this value is between 0 and 25. Starting with the 2015 PUF released in the
Fall of 2017,
ICD‐10 codes are incorporated into the score calculation for cases
diagnosed in 2006‐2019.
Registries were able to submit ICD‐10 codes starting in 2006. However, very few ICD‐10
codes were
submitted until 2015. The 2019 Charlson‐Deyo Score is derived from the
highest score that is
calculated from using either the ICD‐9 codes or the ICD‐10 codes.
More information about the Charlson‐Deyo Comorbidity Index may be found on the
University of Manitoba’s website at:
http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1098
1
Source: Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with
ICD‐9‐CM administrative databases. Journal of Clinical Epidemiology 1992;45(6):613‐619.
Registry Coding Instructions: Not applicable
Analytic Note: Because of the small proportion of cases with a Charlson-Deyo Comorbidity score
exceeding 3, the data have
been truncated to 0, 1, 2, 3 (greater than or equal to 3). A score of 0 indicates
"no comorbid conditions
recorded", or none of the values shown below. Patients with a score of 0 could
still have comorbidities if
they are conditions that are not included in the mapping table below. Note that
the patient's cancer is
not directly reflected in the recorded score.
Two examples illustrating how the Charlson-Deyo Score is summarized for the PUF data: If a patient had a
myocardial infarction, diabetes, and renal disease, the cumulative score would be 4, and the value
shown
in the PUF would be 3. If a patient had severe liver disease, the value in the PUF would also be 3,
since
the Charlson-Deyo Score of severe liver disease is 3.

42
Charlson-Deyo Score continued
Values Reported in the PUF for Charlson-Deyo Score
Code
Definition
0
Total Charlson-Deyo Score of 0
1
Total Charlson-Deyo Score of 1
2
Total Charlson-Deyo Score of 2
3
Total Charlson-Deyo Score of 3 or more
Charlson-Deyo Comorbidity Score Mapping Table
Condition
Charlson-Deyo
Score*
Myocardial Infarction
1
Congestive Heart Failure
1
Peripheral Vascular Disease
1
Cerebrovascular Disease
1
Dementia
1
Chronic Pulmonary Disease
1
Rheumatologic Disease
1
Peptic Ulcer Disease
1
Mild Liver Disease
1
Diabetes
1
Diabetes with Chronic
Complications
2
Hemiplegia or Paraplegia
2
Renal Disease
2
Moderate or Severe Liver
Disease
3
AIDS
6
*Individual Charlson scores are not provided in the PUF. Instead,
the Charlson scores are summed for
each patient and categorized
by a value of 0, 1, 2 and 3 or more. A zero score means they had
none of
the conditions in the mapping table. They could have had
other comorbid conditions however.

43
NCDB--SARSCoV2--Pos
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: SARSCOV2_POS
NAACCR Item #: 3944
Diagnosis Years Available: 2020
Length: 1
Allowable Values: 0, 1, 9 blank
Description:
Data item is designed to track whether patient received a POSITIVE SARS-CoV-2 test or
not.
Rational: To evaluate the impact of COVID-19 diagnosis on cancer patients.
Registry Coding Instructions:
Code a confirmed diagnostic SARS-CoV-2 test was performed to diagnose the 2019 novel
coronavirus disease (COVID-19) as documented by a medical provider (i.e. lab report).
If hospital is in a SEER registry area, registrar may use the exiting SEER text fields as a source for
coding.
Diagnostic tests [reverse transcriptase-polymerase chain reaction (RT-PCR) tests] are based on
detection of viral ribonucleic acid (RNA). Serologic antibody tests (for total antibody or IgM, IgA,
and/or IgG antibodies) are not diagnostic tests for active SARS-CoV-2 infection.
Testing can be either inpatient, outpatient or emergency room visit.
This item may be left blank.
Analytic Note: Not applicable.
Code
Definition
0
Patient did not test positive for active SARS-CoV-2: No positive test
1
Patient tested positive for active SARS-CoV-2; test positive on at least one test
9
Unknown if tested; test done, results unknown

44
Elapsed Days from DX to Date of First Positive COVID Test
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: SARSCOV2_POS_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2020
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
NCDB--SARSCoV2--Pos Date [what was the date of the first positive test?] (NAACCR Item
#3945).
Rational: To evaluate the impact of COVID-19 diagnosis on cancer patients.
Registry Coding Instructions:
Record the date the patient had a positive test for SARS-CoV-2, the virus that causes the 2019
novel coronavirus disease (COVID-19), as documented by a medical provider.
When multiple interpretations are available for multiple viral tests, record the date of the first
positive diagnostic SARS-CoV-2 test. Diagnostic tests [reverse transcriptase-polymerase chain
reaction (RT-PCR) tests] are based on detection of viral ribonucleic acid (RNA). Serologic antibody
tests (for total antibody or IgM, IgA, and/or IgG antibodies) are not diagnostic tests for active
SARS-CoV-2 infection.
If both positive diagnostic tests and positive serologic tests are reported in the medical record,
code the date for the first positive diagnostic test.
Leave the field blank when a date of the test is unknown or the date of a positive (diagnostic or
serologic) test is unknown for SARS-CoV-2.
Analytic Note: Not applicable.
Code
Definition
-9999999 – 99999999
Number of elapsed days from date of initial diagnosis to date the patient had a
positive test for SARS-CoV-2, the virus that causes the 2019 novel coronavirus
(COVID-19), as documented by a medical provider
blank
Date of test is unknown or the date of a positive (diagnostic or serologic)
test is unknown for SARS-CoV-2

45
NCDB--SARSCoV2--Test
Data Dictionary Category: Facility and Patient Demographics
PUF Data Item Name: SARSCOV2_TEST
NAACCR Item #: 3943
Diagnosis Years Available: 2020
Length: 1
Allowable Values: 0, 1, 9, blank
Description: Data item is designed to track whether patient received a SARS-CoV_2 test or not.
Rational: To evaluate the impact of COVID-19 diagnosis on cancer patients.
Registry Coding Instructions:
Collection based on diagnosis years 2020 and 2021.
Code only a confirmed diagnostic test for SARS-CoV-2, the virus that causes the 2019 novel
coronavirus disease (COVID-19), as documented by a medical provider (i.e. lab report);
preadmission or hospital testing is in the record.
If hospital is in a SEER registry area, registrar may use the existing SEER text fields may be used as
a source to support the data item code selected.
Diagnostic tests [reverse transcriptase-polymerase chain reaction (RT-PCR) tests] are based on
detection of viral ribonucleic acid (RNA). Serologic antibody tests (for total antibody or IgM, IgA,
and/or IgG antibodies) are not diagnostic tests for active SARS-CoV-2 infection.
Testing can be either inpatient, outpatient or emergency room visit.
This item may be left blank.
Analytic Note: Not applicable.
Code
Definition
0
Patient not tested for SARS-CoV-2: facility records support that patient did not
undergo pre-admit or in-hospital testing.
1
Patient tested for Active SARS-CoV-2
9
Unknown if patient tested for SARS-CoV-2/No facility record of preadmit
hospital testing of SARS-CoV-2
46
Cancer Identification
47
Sequence Number
Data Dictionary Category: Cancer Identification
PUF Data Item Name: SEQUENCE_NUMBER
NAACCR Item #: 560
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 88, 99
Description:
Indicates the sequence of malignant and non-malignant neoplasms over the lifetime of
the patient.
Registry Coding Instructions:
Codes 00 - 59 and 99 indicate neoplasms of in situ or invasive malignant behavior
(Behavior equals 2 or 3). Codes 60 - 88 indicate neoplasms of benign or borderline non-
malignant behavior (Behavior equals 0 or 1).
Code 00 only if the patient has a single malignant primary. If the patient develops a
subsequent malignant invasive or in situ primary tumor, change the code for the first
tumor from 00 to 01, and number subsequent tumors sequentially.
Code 99 is used in the rare situation for which the sequence of a malignant invasive or in
situ tumor is unknown.
Code 60 only if the patient has a single non-malignant primary. If the patient develops a
subsequent non-malignant primary, change the code for the first tumor from 60 to 61,
and assign codes to subsequent non-malignant primaries sequentially.
Code 88 is used in the rare situation for which the sequence of a benign or borderline
tumor is unknown,
If two or more malignant invasive or in situ neoplasms are diagnosed at the same
time, assign the lowest sequence number to the diagnosis with the worst
prognosis. If no difference in prognosis is evident, the decision is arbitrary.
If two or more non-malignant neoplasms are diagnosed at the same time, assign
the lowest sequence number to the diagnosis with the worst prognosis. If no
difference in prognosis is evident, the decision is arbitrary.
Any tumor in the patient's past which is reportable or reportable-by-agreement
must be taken into account when sequencing subsequently accessioned tumors.
Sequence numbers should be reassigned if the facility learns later of an
unaccessioned tumor that affects the sequence.

48
Sequence Number continued
Analytic Note: None.
Code
Definition
Type of Primaries
00
One malignant or in situ primary only in the patient’s lifetime
Malignant or In Situ
01
First of two or more independent malignant or in situ primaries
Malignant or In Situ
02
Second of two or more independent malignant or in situ primaries
Malignant or In Situ
…
Malignant or In Situ
…
(Actual sequence of this malignant or in situ primary)
Malignant or In Situ
…
Malignant or In Situ
59
Fifty-ninth of 59 or more independent malignant or in situ primaries
Malignant or In Situ
60
One nonmalignant primary only in the patient’s lifetime
Non-Malignant
61
First of two or more independent nonmalignant primaries
Non-Malignant
62
Second of two or more independent nonmalignant primaries
Non-Malignant
…
Non-Malignant
…
(Actual sequence of this nonmalignant primary)
Non-Malignant
…
Non-Malignant
87
Twenty-seventh of 27 or more independent nonmalignant
primaries
Non-Malignant
88
Unspecified number of independent nonmalignant primaries
Non-Malignant
99
Unknown number of malignant or in situ primaries
Malignant or In Situ
49
Class of Case
Data Dictionary Category: Cancer Identification
PUF Data Item Name: CLASS_OF_CASE
NAACCR Item #: 610
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 10 - 14, 20 - 22
Description:
Classifies cases recorded in the database.
Registry Coding Instructions:
Class of Case has 24 categories. Analytic cases are coded 00-22. Non-analytic cases are
coded 30-99. Abstracting for analytic cases is to be completed within six months of the
date of first contact.
Analytic Note:
The CoC Accreditation Program does not require hospitals to abstract nonanalytic cases
(30-99). Nonanalytic cases are not in the PUF data set, and are not included in the
code definitions that follow.
The CoC Accreditation Program does not require Class of Case 00 cases diagnosed in
2006 or later to be staged or followed. They are included in the PUF, but PUF users
may want to omit them from some forms of analysis.
Codes for Class of Case were expanded in 2010. For cases diagnosed prior to 2010,
conversion of analytic cases was generally to Class of Case 00, 10 and 20; the other
codes will not be well populated for earlier cases.

50
Class of Case continued
Only Analytic Class of Case codes are included in the table.
Code
Definition
00
Diagnosis at the reporting facility and all treatment or a decision not to treat was done
elsewhere
10
Initial diagnosis at the reporting facility, or in an office of a physician with admitting
privileges, and part or all of first course treatment or a decision not to treat was at the
reporting facility, NOS
11
Initial diagnosis in an office of a physician with admitting privileges, and part of first course
treatment was done at the reporting facility
12
Initial diagnosis in an office of a physician with admitting privileges, and all of first course
treatment or a decision not to treat was done at the reporting facility
13
Initial diagnosis at the reporting facility and part of first course treatment was done at the
reporting facility; part of first course treatment was done elsewhere
14
Initial diagnosis at the reporting facility and all of first course treatment or a decision not to
treat was done at the reporting facility
20
Initial diagnosis elsewhere and all or part of first course treatment or a decision not to treat
was done at the reporting facility, NOS
21
Initial diagnosis elsewhere and part of first course treatment was done at the reporting
facility; part of first course treatment was done elsewhere
22
Initial diagnosis elsewhere and all of first course treatment or a decision not to treat was
done at the reporting facility
51
Year of Diagnosis
Data Dictionary Category: Cancer Identification
PUF Data Item Name: YEAR_OF_DIAGNOSIS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 4
Allowable Values: 2004 - 2019
Description:
Records the year of initial diagnosis by a physician for the tumor being reported.
Registry Coding Instructions:
Use Date of Initial Diagnosis (NAACC Item #390) whether clinically or histologically
confirmed. If the physician states that in retrospect the patient had cancer at an
earlier date, then use the earlier date as the date of diagnosis.
Use the date therapy was started as the date of diagnosis if the patient receives a first
course of treatment before a definitive diagnosis.
Refer to the list of Ambiguous Terms in Section One of Facility Oncology Registry Data
Standards (FORDS) for language that represents a diagnosis of cancer.
Analytic Note:
Cancer registries record the full date of initial diagnosis, only the year portion of the
reported date is provided in the PUF based on Date of Initial Diagnosis (NAACC Item #390).
Cases with unknown year of diagnosis are not submitted to NCDB.

52
Primary Site
Data Dictionary Category: Cancer Identification
PUF Data Item Name: PRIMARY_SITE
NAACCR Item #: 400
Diagnosis Years Available: 2004 +
Length: 4
Allowable Values: C000 - C999, blank
Description:
Identifies the primary site, that is, the anatomic site of origin for the cancer.
Registry Coding Instructions:
Record the ICD-O-3 (International Classification of Diseases for Oncology, Third Edition)
topography code for the site of origin.
Consult the physician advisor to identify the primary site or the most definitive site
code if the medical record does not contain that information.
Primary site codes may be found in the ICD-O-3 Topography, Numerical List section
(ICD-O-3, p. 43) and in the Alphabetic Index (ICD-O-3, p. 105).
Topography codes are indicated by a "C" preceding the three-digit code number (do
not record the decimal point). Follow the coding rules outlined in ICD-O-3, pp. 20-40.
Use subcategory 8 for single tumors that overlap the boundaries of two or more sub-
sites and the point of origin is not known.
Use subcategory 9 for multiple tumors that originate in one organ.
Code a
denocarcinoma in multiple polyps as a single primary even if they involve more
than one segment of the colon.
Code leukemias to bone marrow (C42.1).
Exception: Code myeloid sarcoma to the site of origin (see ICD-O-3 for coding rules).
Analytic Note:
The most current WHO ICD-O-3 manual is publicly available at
https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf
53
Laterality
Data Dictionary Category: Cancer Identification
PUF Data Item Name: LATERALITY
NAACCR Item #: 410
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 5, 9
Description:
Identifies the side of a paired organ or the side of the body on which the reportable
tumor originated.
This applies to the primary site only.
Registry Coding Instructions:
Code laterality for all paired sites (see Analytic Note).
Code all non-paired sites 0 (see Analytic Note).
Record laterality for unknown primary site (C80.9) as 0 (not a paired site). Do not code
metastatic sites as bilateral involvement.
Code midline lesions 5 (see Analytic Note).
Analytic Note:
Beginning with cases diagnosed in 2010, code 5 is used for midline of paired sites. This
code is applicable for very few sites, because it requires that the two lateral portions be
contiguous (laterality of the skin of most parts of the body has a midline; laterality of the
breast does not). For cases diagnosed prior to 2010, the midline was coded 9. Those
cases are rare, but will be coded 9 in pre-2010 PUF cases.

54
Laterality continued
Code
Definition
0
Organ is not a paired site
1
Origin of primary is right
2
Origin of primary is left
3
Only one side involved, right or left origin not specified
4
Bilateral involvement at time of diagnosis, lateral origin unknown for a single
primary; or both ovaries involved simultaneously, single histology; bilateral
retinoblastomas; Bilateral Wilms tumors
5
Paired site: midline tumor
9
Paired site, but no information concerning laterality
The following are paired sites
The following are paired sites (Continued)
Parotid gland
Peripheral nerves and autonomic nervous system
of lower limb and hip
Submandibular gland
Sublingual gland
Connective, cutaneous and other soft tissue of
upper limb and shoulder
Tonsillar fossa
Tonsillar pillar
Connective, cutaneous and other soft tissue of
lower limb and hip
Overlapping lesion of tonsil
Tonsil, NOS
Breast
Nasal cavity (excluding nasal cartilage and nasal
septum)
Ovary
Fallopian tube
Middle ear
Testis
Maxillary sinus
Epididymis
Frontal sinus
Spermatic cord
Main bronchus (excluding carina)
Kidney, NOS
Lung
Renal pelvis
Pleura
Ureter
Long bones of upper limb and scapula
Eye and lacrimal gland
Short bones of upper limb
Cerebral meninges, NOS
Long bones of lower limb
Cerebrum
Short bones of lower limb
Frontal lobe
Rib and clavicle (excluding sterum)
Temporal lobe
Pelvic bones (excluding sacrum, coccyx, and
symphysis pubis)
Parietal lobe
Occipital lobe
Skin of eyelid
Olfactory lobe
Skin of external ear
Optic lobe
Skin of other and unspecified parts of face
Acoustic lobe

55
Laterality continued
Skin of trunk
Cranial nerve, NOS
Skin of upper limb and shoulder
Adrenal gland
Skin of lower limb and hip
Carotid body
Peripheral nerves and autonomic nervous system
of upper limb and shoulder
56
Histology
Data Dictionary Category: Cancer Identification
PUF Data Item Name: HISTOLOGY
NAACCR Item #: 522
Diagnosis Years Available: 2004 +
Length: 4
Allowable Values: See Analytic Note
Description:
See ICD-O-3 and the Hematopoeitic and Lymphoid Manual Records for the tumor
histology of all cases reported to the NCDB in International Classification of Disease for
Oncology, Third Edition (ICD-O-3) terms.
Registry Coding Instructions: None.
Analytic Note:
A list of histologies and labels may be found on the online ICD-O-3 site:
http://www.iacr.com.fr/index.php?option=com_content&view=category&layout=blog&
id=100&Itemid=577.
57
Behavior Code
Data Dictionary Category: Cancer Identification
PUF Data Item Name: BEHAVIOR
NAACCR Item #: 523
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3
Description:
Records the behavior of all cases reported to the NCDB. The fifth digit of the
morphology code is the behavior code.
Registry Coding Instructions: None.
Analytic Note:
Benign tumors or tumors of uncertain behavior (behavior codes 0, 1) are not reported
to the NCDB except for the following sites: meninges (C70._), brain (C71._), spinal cord,
cranial nerves, and other parts of central nervous system (C72._), pituitary gland
(C75.1), craniopharyngeal duct (C75.2) and pineal gland (C75.3).

58
Behavior continued
Code
Definition
Additional Definition and Examples
0
Benign
Benign
1 Borderline
Uncertain whether benign or malignant
Borderline malignancy
Low malignant potential
Uncertain malignant potential
2
In-situ and synonymous
with in-situ
Adenocarcinoma in an adenomatous polyp with no invasion of stalk
Bowen disease (not reportable for C44._)
Clark level 1 for melanoma (limited to epithelium)
Comedocarcinoma, noninfiltrating (C50.B)
Confined to epithelium
Hutchinson melanotic freckle, NOS (C44.B)
Intracystic, noninfiltrating (carcinoma)
Intraductal (carcinoma)
Intraepidermal, NOS (carcinoma)
Intraepithelial, NOS (carcinoma)
Involvement up to, but not including the basement membrane.
Lentigo maligna (C44._)
Lobular neoplasia (C50._)
Lobular, noninfiltrating (C50._) (carcinoma)
Noninfiltrating (carcinoma)
Noninvasive (carcinoma only)
No stromal involvement
Papillary, noninfiltrating or intraductal (carcinoma)
Precancerous melanosis (C44._)
Queyrat erythroplasia (C60._)
3
Invasive
Invasive or microinvasive
59
Grade/Differentiation
Data Dictionary Category: Cancer Identification
PUF Data Item Name: GRADE
NAACCR Item #: 440
Diagnosis Years Available: 2004 – 2017 (new grading system used in 2018 and later)
Length: 1
Allowable Values: 1 - 9
Description:
Describes the tumor's resemblance to normal tissue. Well differentiated (Grade I) is
the most like normal tissue, and undifferentiated (Grade IV) is the least like normal
tissue.
Registry Coding Instructions:
Code grade according to ICD-O-3 (pp. 30-31 and 67).
Code the grade or differentiation as stated in the final pathologic diagnosis. If the
differentiation is not stated in the final pathologic diagnosis, use the information from
the microscopic description or comments.
When the pathology report(s) lists more than one grade of tumor, code to the highest
grade, even if the highest grade is only a focus (Rule G, ICD-O-3, p. 21).
Code the grade or differentiation from the pathologic examination of the primary
tumor, not from metastatic sites.
When there is no tissue diagnosis, it may be possible to establish grade through
magnetic resonance imaging (MRI) or positron emission tomography (PET). When
available, code grade based on the recorded findings from these imaging reports.
If the primary site is unknown, code the grade/differentiation as 9 (Unknown).
Code the grade for in situ lesions if the information is available. If the lesion is both
invasive and in situ, code only the invasive portion. If the invasive component grade is
unknown, then code 9.
Do not use "high grade", "low grade", or "intermediate grade" descriptions for
lymphomas as a basis for differentiation. These terms are categories in the Working
Formulation of Lymphoma Diagnoses and do not relate to grade/differentiation.
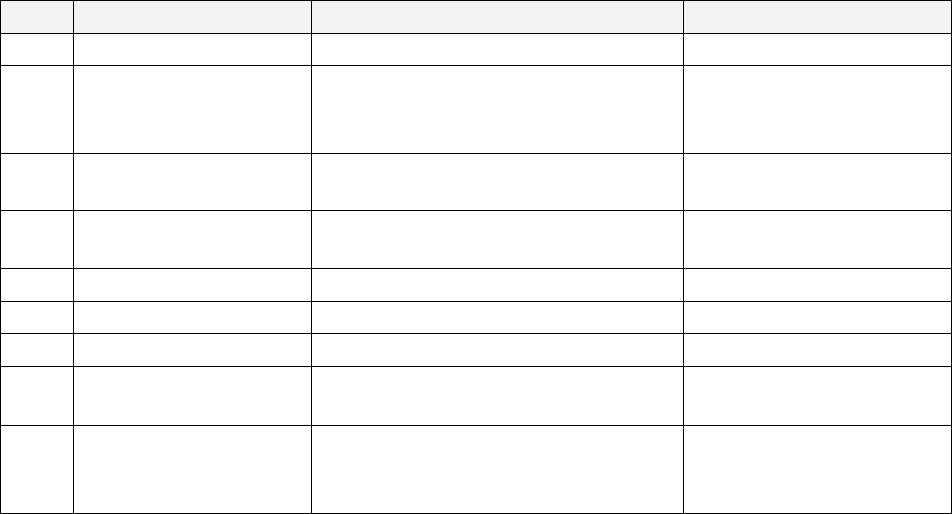
60
Grade/Differentiation continued
Codes 5-8 define T-cell or B-cell origin for leukemias and lymphomas. T-cell, B-cell, or
null cell classifications have precedence over grading or differentiation.
Do not use the WHO grade to code this data item.
If no grade is given for astrocytomas, then code 9 (Unknown).
If no grade is given for glioblastoma multiforme, then code 9 (Unknown).
Analytic Note:
Although ICD-O-2 and ICD-O-3 Grade/Differentiation are collected as separate items,
the only difference between the two editions is that code 8 (NK cells) was added after
ICD-O-2 was initially published. They are combined in the PUF, as an output to the ICD-
O-2 to ICD-O-3 conversion used for histology and behavior. In 2018 a new grading
system is used. See the description in the next section.
Code
Definition
Description
Specific Cancer Grouping
1
Grade I, 1, i
Well differentiated; differentiated, NOS
2 Grade II,2, ii I/III or 1/3
Moderately differentiated; moderately
well differentiated; intermediate
differentiation
3 Grade III,3, iii II/III or 2/3 Poorly differentiated; dedifferentiated
4 Grade IV,4, iv III/III or 3/3 Undifferentiated; anaplastic
5
T cell; T-precursor
Lymphomas and Leukemias
6
B cell; pre-B; B-precursor
Lymphomas and Leukemias
7
Null cell; non T-non B
Lymphomas and Leukemias
8
NK (natural killer) cell (effective with
diagnosis 1/1/95 and
after)
Lymphomas and Leukemias
9
Cell type not determined, not stated or
not applicable; unknown primaries; high
grade dysplasia (adenocarcinoma in situ)
All histologies
61
Grade/Differentiation 2018+
Data Dictionary Category: Cancer Identification
PUF Data Item Names: Grade_Clin, Grade_Path, Grade_Path_Post
NAACCR Items #: 3843, 3844, 3845
Diagnosis Years Available: 2018 +
Length: 1
Allowable Values: 1-5, 8, 9, A-E, L, H, M, S, blank
Description:
For solid tumors diagnosed 2018 and forward, grade will be collected in three different data
items, Grade Clinical, Grade Pathological, and Grade Post Therapy Path, and the codes and
coding instructions will depend on the type of cancer. The revised grade codes are based on the
recommended grading systems specified in the relevant chapters of the AJCC 8th edition staging
manual and/or the CAP cancer protocols (when applicable). For each AJCC chapter that has a
recommended grading system, the categories and definitions can be found in the chapter’s
grade section. The recommended AJCC grading system for a particular chapter are also used for
histologic types of tumors occurring in the relevant organs but not eligible for staging in AJCC
8th edition. For AJCC chapters for which there is no recommended grading system (for example,
chapter 47, Melanoma of the Skin) or for sites for which there is no applicable AJCC chapter (for
example, Trachea), the generic cancer registry grade categories used historically will still apply
and will be used for all three grade fields. For cases not eligible for AJCC staging within a specific
chapter (for example, a colon case with a specific histology not applicable for staging in chapter
20, Colon and Rectum), grade is still assigned. If the recommended grading system is
documented, the registrar is to use that. If a recommended grading system is not documented,
the generic cancer registry grade categories apply if they are included in the grade table for that
site. Additionally, if a case/site is eligible for TNM staging, grade is still assigned using the
recommended AJCC grade, if documented, even if grade is not necessary to determine the TNM
stage group. If the recommended grading system is not documented, then the generic cancer
registry grade categories apply if they are included in the grade table for site. The tables for
grade have been re-structured for 2018 and beyond. There may be a combination of numeric
and alphabetic codes within the same table, according to this template.

62
Grade/Differentiation 2018+ continued
Template for a Cancer-Specific Grade Table
Code
Grade Description
1
Site Specific Grade System Category
2
Site Specific Grade System Category
3
Site Specific Grade System Category
4
Site Specific Grade System Category
5
Site Specific Grade System Category
8
Not applicable (Hematopoietic neoplasms only)
9
Grade cannot be assessed; Unknown
A
Well differentiated
B
Moderately differentiated
C
Poorly differentiated
D
Undifferentiated and anaplastic
E
Site Specific Grade System Category
H
High grade
L
Low grade
M
Site Specific Grade System Category
S
Site Specific Grade System Category
Blank
(Post therapy only)
Codes 1-5, H, L, M, S, and 9 all represent AJCC recommended grading systems. Categories L and H are
applicable for the AJCC recommended grading systems of “low grade” and “high grade” for those
cancers for which these are used (e.g. urinary cancers with urothelial histologies). It also includes M for
intermediate grade to be used with L and H for breast in situ cancers. S is utilized for sarcomatous
overgrowth in corpus uteri adenosarcoma, an AJCC registry data collection variable. Codes A-E are the
generic grade categories (definitions) that have been used by the cancer surveillance community for
many years. Codes A-E are not available for all cancers since although many AJCC chapters continue to
use the traditional grade terms, many of the chapters now use a three-grade system, instead of the
four-grade system. The Grade descriptions and definitions by cancer type are found in the Grade
manual on the NAACCR website at: https://apps.naaccr.org/ssdi/list/
63
Diagnostic Confirmation
Data Dictionary Category: Cancer Identification
PUF Data Item Name: DIAGNOSTIC_CONFIRMATION
NAACCR Item #: 490
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 1 - 9
Description:
Records the most definitive method of diagnostic confirmation of the cancer being
reported at any time in the patient's history.
Registry Coding Instructions:
For solid tumors only (histologies other than 9590-9992), this is a hierarchical schema
to identify how the malignancy was determined - from histologic confirmation (1) being
most precise to unknown (9) being the least. Lower numbered codes take precedence
over higher numbered codes. The code must be changed to a lower code if a more
definitive method confirms the diagnosis at any time during the course of the disease.
Code 3 in the table below does NOT apply to solid tumors.
Separate rules were established for non-solid tumors (histology codes 9590-9992) in
2010. Prior to that, registrars were instructed to use Code 1 for positive hematologic
findings and bone marrow specimens for leukemia, including peripheral blood smears
and aspiration biopsies. Otherwise, to use Code 2 for positive brushings, washings, cell
aspiration, and hematologic findings (except for leukemia).
For non-solid tumors (histology codes 9590-9992) beginning in 2010, the table below
is NOT hierarchical, and the rules for assignment are specific to non-solid tumors.
Coding Instructions for All Tumors:
Assign Code 1 when the microscopic diagnosis is based on tissue specimens from
biopsy, frozen section, surgery, autopsy, D&C or from aspiration or biopsy of bone
marrow specimens.
Assign Code 2 when the microscopic diagnosis is based on cytologic examination
of cells such as sputum smears, bronchial brushings, bronchial washings,
prostatic secretions, breast secretions, gastric fluid, spinal fluid, pleural fluid,
urinary sediment, cervical or vaginal smears, or from paraffin block specimens
from concentrated spinal, pleural or peritoneal fluid. These methods are rarely
used for hematopoietic or lymphoid tumors.
64
Diagnostic confirmation continued
Assign Code 5 when the diagnosis of cancer is based on laboratory tests or
marker studies which are clinically diagnostic for that cancer.
Assign Code 6 when the diagnosis is based only on the surgeon's operative
report or from a surgical exploration or endoscopy or from gross autopsy
findings in the absence of tissue or cytologic findings.
Additional Coding Instructions for Hematopoietic or Lymphoid Tumors (Histologies
9590-9992):
There is no priority hierarchy for coding Diagnostic Confirmation for
hematopoietic and lymphoid tumors. Most commonly, the specific histologic
type is diagnosed by immunophenotyping or genetic testing. See the
Hematopoietic Database (DB) for information on the definitive diagnostic
confirmation for specific tumors.
For leukemia only, assign Code 1 when the diagnosis is based only on the
complete blood count (CBC), white blood count (WBC) or peripheral blood
smear. Do not use Code 1 if the diagnosis was based on immunophenotyping
or genetic testing using tissue, bone marrow, or blood.
Assign Code 3 when there is a histologic positive for cancer AND positive
immunophenotyping and/or positive genetic testing results. Do not use Code 3
for neoplasms diagnosed prior to January 1, 2010.
Assign Code 8 when the case was diagnosed by any clinical method that cannot
be coded as 6 or 7. A number of hematopoietic and lymphoid neoplasms are
diagnosed by tests of exclusion where the tests for the disease are equivocal
and the physician makes a clinical diagnosis based on the information from the
equivocal tests and the patient's clinical presentation.
Assign Code 6 when the diagnosis is based only on the surgeon's operative
report from a surgical exploration or endoscopy or from gross autopsy findings
in the absence of tissue or cytologic findings.
Assign Code 1 when microscopic diagnosis is based on tissue specimens from
biopsy, frozen section, surgery, autopsy or D&C or from aspiration of biopsy
bone marrow specimens.
Assign Code 2 when microscopic diagnosis is based on cytologic examination of
cells such as sputum smears, bronchial brushings, bronchial washings, prostatic
secretions, breast secretions, gastric fluid, peritoneal fluid, urinary sediment, or
peritoneal fluid. These methods are rarely used for hematopoietic or lymphoid
cancers.
65
Diagnostic Confirmation continued
Assign Code 5 when the diagnosis of cancer is based on laboratory tests or
marker studies which are clinically diagnostic for that specific cancer.
Analytic Note:
In 2010, cancer registries in North America adopted new rules for coding hematopoietic and
lymphoid tumors. At that time, this item was modified for cases diagnosed in 2010 or later to
better reflect the ways these tumors are diagnosed. Code 3 was defined and implemented at
that time, and the rules for coding were refined. The instructions and table presented here
represent a combination of the new instructions and the older instructions that still apply to
solid tumors.

66
Diagnostic Confirmation continued
Code
Definition
Description
1
Positive Histology
Histologic confirmation (tissue microscopically examined)
2 Positive Cytology
Cytologic confirmation (no tissue microscopically examined; fluid
cells microscopically examined)
3
Positive Histology PLUS
positive immunophenotyping
and/or positive genetic
studies
Histology is positive for cancer, and there are also
immunophenotyping and/or genetic test results. For example,
bone marrow examination is positive for acute myeloid
leukemia (9861/3). Genetic testing shows AML with inv(16)
(p13.1q22) (9871/3) Use this code only for histology range
9590-9992 where the year of diagnosis is 2010 or later
4
Positive microscopic
confirmation; method not
specified
Microscopic confirmation is all that is known. It is unknown if
cells were from histology or cytology
5
Positive laboratory
test/marker study
A clinical diagnosis of cancer is based on laboratory tests/marker
studies which are clinically diagnostic for cancer. Examples
include alpha-fetoprotein for liver primaries. Elevated PSA is
non-diagnostic of cancer. However, if the physician uses PSA as a
basis for diagnosing prostate cancer with no other workup,
record as code 5
6
Direct visualization without
microscopic confirmation
The tumor was visualized during a surgical/endoscopic procedure
only with no tissue resected for microscopic examination
7
Radiography and other
imaging techniques without
microscopic confirmation
The malignancy was reported by the physician from an imaging
technique report only
8
Clinical diagnosis only (other
than 5, 6 or 7)
The malignancy was reported by the physician in the medical
record, but there is no statement of how the cancer was
diagnosed (usually non-analytic)
9
Unknown whether or not
microscopically confirmed.
A statement of malignancy was reported in the medical record,
but there is no statement of how the cancer was diagnosed.
(usually non-analytic)
67
Regional Lymph Nodes Examined
Data Dictionary Category: Cancer Identification
PUF Data Item Name: REGIONAL_NODES_EXAMINED
NAACCR Item #: 830
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 90, 95 - 99
Description:
Records the total number of regional lymph nodes that were removed and examined by the
pathologist. Beginning with cases diagnosed on or after January 1, 2004, this item became a
component of the Collaborative Staging System (CS). In 2016, use of CS was discontinued,
however this data item continued to be required.
Rationale:
This data item serves as a quality measure of the pathologic and surgical evaluation and
treatment of the patient.
Coding Instructions:
Regional lymph nodes only. Record information about only regional lymph nodes in this field.
Distant lymph node information should not be coded in this field.
This field is based on pathologic information only. This field is to be recorded regardless of
whether the patient received preoperative treatment.
Use of Code 00. Code 00 may be used in several situations.
When the assessment of lymph nodes is clinical.
When no lymph nodes are removed and examined.
When a “dissection” of a lymph node drainage area is found to contain no lymph nodes
at the time of pathologic examination.
If Regional Nodes Examined is coded 00, Regional Nodes Positive is coded as 98.
Cumulative nodes removed and examined. Record the total number of regional lymph nodes
removed and examined by the pathologist.
The number of regional lymph nodes examined is cumulative from all procedures that
removed lymph nodes through the completion of surgeries in the first course of
treatment with the exception of aspiration or core biopsies coded to 95.
68
Do not count a positive aspiration or core biopsy of a lymph node in the same lymph
node chain removed at surgery as an additional node in Regional Nodes Examined.
If the positive aspiration or core biopsy is from a node in a different node region, include
the node in the count of Regional Nodes Examined.
If the location of the lymph node that is aspirated or core-biopsied is not known,
assume it is part of the lymph node chain surgically removed, and do not include it in
the count of Regional Nodes Examined.
When neither the type of lymph node removal procedure nor the number of lymph
nodes examined is known, use code 98.
Priority of lymph node counts. If there is a discrepancy regarding the number of lymph nodes
examined, use information in the following priority: final diagnosis, synoptic report (also known
as CAP protocol or pathology report checklist), microscopic, gross.
Use of code 95. Use code 95 when the only procedure for regional lymph nodes is a needle
aspiration (cytology) or core biopsy (tissue).
Lymph node biopsy. If a lymph node biopsy was performed, code the number of nodes
removed, if known. If the number of nodes removed by biopsy is not known, use code 96.
Definition of “sampling” (code 96). A lymph node “sampling” is removal of a limited number of
lymph nodes. Other terms for removal of a limited number of nodes include lymph node biopsy,
berry picking, sentinel lymph node procedure, sentinel node biopsy, selective dissection. Use
code 96 when a limited number of nodes are removed but the number is unknown.
Definition of “dissection” (code 97). A lymph node “dissection” is removal of most or all of the
nodes in the lymph node chain(s) that drain the area around the primary tumor. Other terms
include lymphadenectomy, radical node dissection, lymph node stripping. Use code 97 when
more than a limited number of lymph nodes are removed and the number is unknown.
Multiple lymph node procedures. If both a lymph node sampling and a lymph node dissection
are performed and the total number of lymph nodes examined is unknown, use code 97.
Use of Code 99. If it is unknown whether nodes were removed or examined, code as 99.
Primary sites always coded 99. For the following schemas, the Regional Nodes Examined field is
always coded as 99. Placenta, Brain and Cerebral Meninges, Other Parts of Central Nervous
System, Intracranial Gland Hematopoietic, Reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms Hodgkin and non-Hodgkin Lymphoma Myeloma and Plasma Cell
Disorders Other and Ill-Defined Primary Sites, Unknown Primary Site
When definition of regional nodes differs between the AJCC Cancer Staging Manual and the
SEER Program Coding and Staging Manual, use the AJCC definition.

69
Regional Lymph Nodes Examined continued
Analytic Note: None.
Code
Definition
00
No nodes were examined
01-89
1-89 nodes were examined. (Code the exact number of regional lymph nodes
examined)
90
90 or more nodes examined
95
No regional nodes removed, but aspiration or core biopsy of regional nodes was
performed
96
Regional lymph node removal was documented as sampling, and the number of
nodes is unknown/not stated
97
Regional lymph node removal was documented as dissection, and the number of
nodes is unknown/not stated
98
Regional lymph nodes surgically removed but number of lymph nodes unknown
or not stated, and not documented as sampling or dissection; nodes were
examined, but the number is unknown
99
Unknown if regional nodes examined. Not applicable or negative. Not stated in
patient record.
70
Regional Lymph Nodes Positive
Data Dictionary Category: Cancer Identification
PUF Data Item Name: REGIONAL_NODES_POSITIVE
NAACCR Item #: 820
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 – 99
Description:
Records the exact number of regional lymph nodes examined by the pathologist and found to
contain metastases. Beginning with cases diagnosed on or after January 1, 2004, this item
became a component of the Collaborative Staging System (CS). In 2016, use of CS was
discontinued, however this data item continued to be required. Rationale This data item is
necessary for pathological staging, and it serves as a quality measure for pathology reports and
the extent of the surgical evaluation and treatment of the patient.
Coding Instructions:
Regional lymph nodes only. Record information about only regional lymph nodes in this field.
Involved distant lymph nodes should not be coded in this field.
This field is based on pathologic information only. This field is to be recorded regardless of
whether the patient received preoperative treatment.
Cumulative nodes positive. Record the total number of regional lymph nodes removed and
found to be positive by pathologic examination.
The number of regional lymph nodes positive is cumulative from all procedures that
remove lymph nodes through the completion of surgeries in the first course of
treatment.
Do not count a positive aspiration or core biopsy of a lymph node in the same lymph
node chain removed at surgery as an additional node in Regional Nodes Positive when
there are positive nodes in the resection. In other words, if there are positive regional
lymph nodes in a lymph node dissection, do not count the core needle biopsy or the fine
needle aspiration if it is in the same chain. See also Use of Code 95 below.
If the positive aspiration or core biopsy is from a node in a different node region, include
the node in the count of Regional Nodes Positive.
71
If the location of the lymph node that is core-biopsied or aspirated is not known,
assume it is part of the lymph node chain surgically removed, and do not include it in
the count of Regional Nodes Positive.
Priority of lymph node counts. If there is a discrepancy regarding the number of positive lymph
nodes, use information in the following priority: final diagnosis, synoptic report (also known as
CAP protocol or pathology report checklist), microscopic, gross.
Positive Nodes in Multiple Primaries in Same Organ. If there are multiple primary cancers with
different histologic types in the same organ and the pathology report just states the number of
nodes positive, the registrar should first try to determine the histology of the metastases in the
nodes and code the nodes as positive for the primary with that histology. If no further
information is available, code the nodes as positive for all primaries.
Isolated tumor cells (ITCs) in lymph nodes. For all primary sites except cutaneous melanoma and
Merkel cell carcinoma of skin, count only lymph nodes that contain micrometastases or larger
(metastases greater than 0.2 millimeters in size). Do not include in the count of lymph nodes
positive any nodes that are identified as containing isolated tumor cells (ITCs). If the path report
indicates that nodes are positive but the size of metastasis is not stated, assume the metastases
are larger than 0.2 mm and count the lymph node(s) as positive.
For cutaneous melanoma and Merkel cell carcinoma, count nodes with ITCs as positive
lymph nodes.
Use of Code 95. Use code 95 when the only procedure for regional lymph nodes is a needle
aspiration (cytology) or core biopsy (tissue).
Use code 95 when a positive lymph node is aspirated and there are no surgically
resected lymph nodes.
Use code 95 when a positive lymph node is aspirated and surgically resected lymph
nodes are negative.
Definition of Code 97. Use code 97 for any combination of positive aspirated, biopsied, sampled
or dissected lymph nodes if the number of involved nodes cannot be determined on the basis of
cytology or histology. Code 97 includes positive lymph nodes diagnosed by either cytology or
histology. o Note: If the aspirated node is the only one that is microscopically positive, use code
95.
Use of Code 98. Code 98 may be used in several situations.
When the assessment of lymph nodes is clinical only.
When no lymph nodes are removed and examined.
When a “dissection” of a lymph node drainage area is found to contain no lymph nodes
at the time of pathologic examination.
If Regional Nodes Positive is coded as 98, Regional Nodes Examined is usually coded 00.

72
Use of code 99. Use code 99 if it is unknown whether regional lymph nodes are positive.
Primary sites always coded 99. For the following primary sites and histologies, the Regional
Nodes Positive field is always coded as 99: Placenta, Brain and Cerebral Meninges, Other Parts
of Central Nervous System, Intracranial Gland, Hodgkin and non-Hodgkin’s Lymphoma,
Hematopoietic, Reticuloendothelial, Immunoproliferative and Myeloproliferative Neoplasms
Myeloma and Plasma Cell Disorders, Other and Ill-Defined Primary Sites, Unknown Primary Site
When definition of regional nodes differs between the AJCC Cancer Staging Manual and the
SEER Program Coding and Staging Manual use the AJCC definition.
Analytic Note: None.
Code
Definition
00
All nodes examined are negative
01-89
1-89 nodes are positive. (Code exact number of nodes positive)
90
90 or more nodes are positive
95
Positive aspiration or core biopsy of lymph node(s)
97
Positive nodes are documented, but the number are unspecified
98
No nodes examined
99
It is unknown whether nodes are positive; not applicable; not stated in patient
record
73
Sentinel Lymph Nodes Examined
Data Dictionary Category: Cancer Identification
PUF Data Item Name: SLN_EXAM
NAACCR Item #: 834
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00-90, 95, 98, 99, Blank
Description:
Records the total number of lymph nodes sampled during the sentinel node biopsy and
examined by the pathologist. This data item is required for CoC-accredited facilities as of cases
diagnosed 01/01/2018 and later. This data item is required for breast and cutaneous
melanoma cases only.
Rationale:
It is a known fact that sentinel lymph node biopsies have been under-reported. Additionally, the
timing and results of sentinel lymph node biopsy procedures are used in quality of care
measures. This data item can be used to more accurately assess the number of lymph nodes
biopsied during the sentinel node biopsy procedure separate from the number of lymph nodes
dissected during additional subsequent regional node procedures.
Coding Instructions:
If, during a sentinel node biopsy procedure, a few non-sentinel nodes happen to be sampled,
document the total number of nodes sampled during the sentinel node procedure in this data
item. I.e., record the total number of nodes from the sentinel node biopsy procedure regardless
of sentinel node status.
If a sentinel node biopsy procedure and then a subsequent, separate regional node dissection
procedure are performed, record the total number of nodes biopsied during the sentinel node
procedure in this data item, and record the total number of regional lymph nodes
biopsied/dissected (which includes the number of nodes documented in this data item) in
Regional Lymph Nodes Examined [830].
If a sentinel lymph node biopsy is performed during the same procedure as the regional node
dissection, record the total number of nodes biopsied during the sentinel node procedure in this
data item, and record the total number of regional lymph nodes biopsied/dissected (which
includes the number of nodes documented in this data item) in Regional Lymph Nodes
Examined [830].

74
Sentinel Lymph Nodes Examined, continued
If aspiration of sentinel lymph node(s) AND a sentinel node biopsy procedure were performed
for same patient, record the results for the sentinel node biopsy.
The number of sentinel lymph nodes examined will typically be found in the pathology report;
radiology reports, or documented by the physician. Determination of the exact number of
sentinel lymph nodes examined may require assistance from the managing physician for
consistent coding.
Sentinel node procedures are common for other sites, but data is only collected in these fields
for breast and cutaneous melanoma. Use the AJCC N suffix to designate sentinel node
procedures for ALL sites.
The number of sentinel nodes should be equal to or less than the number of regional nodes
examined recorded in the Regional Lymph Nodes Examined [830] data item.
Code
Label
00
No sentinel nodes were examined
01-90
Sentinel nodes were examined
(code the exact number of sentinel lymph nodes examined)
95
No sentinel nodes were removed,
but aspiration of sentinel node(s) was performed
98
Sentinel lymph nodes were biopsied, but the number is unknown
99
It is unknown whether sentinel nodes were examined;
not applicable or negative; not stated in patient record
75
Sentinel Lymph Nodes Positive
Data Dictionary Category: Cancer Identification
PUF Data Item Name: SLN_POS
NAACCR Item #: 835
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00-90, 95, 97-99, Blank
Description:
Records the exact number of sentinel lymph nodes biopsied by the pathologist and found to
contain metastases. This data item is required for CoC-accredited facilities as of cases diagnosed
01/01/2018 and later. This data item is required for breast and cutaneous melanoma cases
only.
Rationale:
It is a known fact that sentinel lymph node biopsies have been under-reported. Additionally, the
timing and results of sentinel lymph node biopsy procedures are used in quality of care
measures. This data item can be used to more accurately assess the number of positive sentinel
lymph nodes biopsied separate from the number of positive lymph nodes identified during
additional subsequent regional node dissection procedures, if performed.
Coding Instructions:
If, during a sentinel node biopsy procedure, a few non-sentinel nodes happen to be sampled and
are positive, document the total number of positive nodes identified during the sentinel node
procedure in this data item. I.e., record the total number of positive nodes from the sentinel
node biopsy procedure regardless of whether the nodes contain dye or colloidal material (tracer
or radiotracer).
If both a sentinel node biopsy procedure and then a subsequent, separate regional node
dissection procedure are performed, record the total number of positive sentinel nodes
identified during the sentinel node procedure in this data item, and record the total number of
positive regional lymph nodes biopsied/dissected (which includes the number of sentinel nodes
documented in this data item) in Regional Lymph Nodes Positive [820].
If a positive aspiration of sentinel lymph node(s) AND a positive sentinel node biopsy procedure
were performed for same patient, record the results for the positive sentinel node biopsy
procedure.
76
Sentinel Lymph Nodes Positive, continued
Sentinel node procedures are common for other sites, but data is only collected in these fields
for breast and cutaneous melanoma. Use the AJCC N suffix to designate sentinel node
procedures for ALL sites.
FOR BREAST ONLY: If a sentinel lymph node biopsy is performed during the same procedure as
the regional node dissection, use code 97 in this data item, and record the total number of
positive regional lymph nodes biopsied/dissected (both sentinel and regional) in Regional Lymph
Nodes Positive [820]. • The CAP Protocol for Breast is designed to capture information from the
resection (there is no diagnostic protocol for breast). As a result, when the sentinel lymph node
biopsy is performed during the same procedure as the regional node dissection, only the overall
total number of positive regional nodes (both sentinel and regional) is recorded; the number of
positive sentinel nodes is not captured. STORE 2018 Sentinel Lymph Nodes Positive Page 164
FOR MELANOMA ONLY: If a sentinel lymph node biopsy is performed during the same
procedure as the regional node dissection, record the total number of positive sentinel nodes
identified in this data item, and record the total number of positive regional lymph nodes
identified (which includes the number of positive sentinel nodes documented in this data item)
in Regional Lymph Nodes Positive [820].
When the sentinel lymph node biopsy is performed during the same procedure as the regional
node dissection the CAP Protocol for Melanoma captures both the number of positive sentinel
nodes as well as the number of positive regional nodes (i.e., the number of positive sentinel
nodes is captured).
The number of sentinel lymph nodes biopsied and found positive will typically be found in the
pathology report; radiology reports, or documented by the physician. Determination of the
exact number of sentinel lymph nodes positive may require assistance from the managing
physician for consistent coding.
The number of sentinel nodes positive should be less than or equal to than the total number of
Regional Nodes Positive [820].
For carcinoma of the breast, if only positive Isolated Tumor Cells (ITC) are identified the sentinel
lymph nodes are considered negative.
For melanoma, if only positive Isolated Tumor Cells (ITC) are identified the sentinel lymph nodes
are considered positive.
mi (microscopic or micro mets) sentinel lymph nodes are considered positive.

77
Sentinel Lymph Nodes Positive, continued
Code
Label
00
All sentinel nodes examined are negative
01-90
Sentinel nodes are positive (code exact number of nodes positive)
95
Positive aspiration of sentinel lymph node(s) was performed
97
Positive sentinel nodes are documented, but the number is unspecified; For breast ONLY:
SLN and RLND occurred during the same procedure
98
No sentinel nodes were biopsied
99
It is unknown whether sentinel nodes are positive; not applicable; not stated in patient
record

78
Sentinel Lymph Node Biopsy, Days from Diagnosis
Data Dictionary Category: Cancer Identification
PUF Data Item Name: SENTINEL_LNBX_STARTED_DAY
NAACCR Item #: Not applicable
Diagnosis Years Available: 2018 +
Length: 8
Allowable Values: 0000-9999, blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date of Sentinel Node Biopsy (NAACCR Item #832).
This is a new variable collected in 2018 and later. This item is only collected for breast and
cutaneous melanoma. The AJCC N suffix to designate sentinel node procedures for ALL sites.
For more information, see NAACCR Item 832, Date of Sentinel Node Biopsy in the STORE manual
at:
https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx

79
Regional Lymph Node Dissection, Days from Diagnosis
Data Dictionary Category: Cancer Identification
PUF Data Item Name: REG_LN_DISS_STARTED_DAY
NAACCR Item #: Not applicable
Diagnosis Years Available: 2018 +
Length: 8
Allowable Values: 0000-9999, blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date of Regional Lymph Node Dissection (NAACCR Item #682).
This is a new variable collected in 2018 and later.
For more information, see NAACCR Item 682, Date of Regional Lymph Node Dissection in the
STORE manual at
https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx
80
Surgical Diagnostic and Staging Procedure
Data Dictionary Category: Cancer Identification
PUF Data Item Name: RX_SUMM_DXSTG_PROC
NAACCR Item #: 1350
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 07, 09
Description:
Records the type of surgical diagnostic and/or staging procedure performed.
Registry Coding Instructions:
Code the type of procedure performed as part of the initial diagnosis and workup,
whether
this is done at the reporting institution or another facility.
Code 02 is used if both an incisional biopsy of the primary site and an incisional
biopsy of a
metastatic site are done.
Surgical procedures which aspirate, biopsy, or remove regional lymph nodes in an
effort to
diagnose and/or stage disease are not coded in this item. The
item Scope of Regional Lymph
Node Surgery (NAACCR Item #1292) is used
to code these procedures.
Brushings, washings, cell aspiration, and hematologic findings (peripheral blood
smears) as
positive cytologic diagnostic confirmation are coded in the data
item Diagnostic
Confirmation (NAACCR Item #490). These are not considered
surgical procedures and are
not be coded in this item.
Excisional biopsies with clear or microscopic margins are not coded in this data
item. Item
Surgical Procedure of Primary Site (NAACCR Item #1290) is used
to code these procedures.
Palliative surgical procedures are not coded in this data item. The item Palliative
Care
(NAACCR Item #3270) is used to code these procedures.
Analytic Note: None.

81
Surgical Diagnostic and Staging Procedure continued
Code
Definition
00
No surgical diagnostic or staging procedure was performed
01
A biopsy (incisional, needle, or aspiration) was done to a site other than the primary.
No exploratory procedure was done
02
A biopsy (incisional, needle, or aspiration) was done to the primary site; or biopsy or
removal of a lymph node to diagnose or stage lymphoma
03
A surgical exploration only. The patient was not biopsied or treated
04
A surgical procedure with a bypass was performed, but no biopsy was done
05
An exploratory procedure was performed, and a biopsy of either the primary site or
another site was done
06
A bypass procedure was performed, and a biopsy of either the primary site or another
site was done
07
A procedure was done, but the type of procedure is unknown
09
No information on whether a diagnostic or staging procedure was performed
82
Surgical Diagnostic and Staging Procedure at this Facility
Data Dictionary Category: Cancer Identification
PUF Data Item Name: RX_HOSP_DXSTG_PROC
NAACCR Item #: 740
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 07, 09
Description:
Records the type of surgical diagnostic and/or staging procedure performed at the
reporting facility This data item was added to the 2015 PUF (data released in Fall
2017), and does not appear in prior versions of the PUF data.
Registry Coding Instructions:
Code the type of procedure performed as part of the initial diagnosis and workup,
whether
this is done at the reporting institution or another facility.
Code 02 is used if both an incisional biopsy of the primary site and an incisional
biopsy of a
metastatic site are done.
Surgical procedures which aspirate, biopsy, or remove regional lymph nodes in an
effort to
diagnose and/or stage disease are not coded in this item. The
item Scope of Regional Lymph
Node Surgery (NAACCR Item #1292) is used
to code these procedures.
Brushings, washings, cell aspiration, and hematologic findings (peripheral blood
smears) as
positive cytologic diagnostic confirmation are coded in the data
item Diagnostic
Confirmation (NAACCR Item #490). These are not considered
surgical procedures and are
not be coded in this item.
Excisional biopsies with clear or microscopic margins are not coded in this data
item. Item
Surgical Procedure of Primary Site (NAACCR Item #1290) is used
to code these procedures.
Palliative surgical procedures are not coded in this data item. The item Palliative
Procedure
(NAACCR Item #3270) is used to code these procedures.
Analytic Note: None.

83
Surgical Diagnostic and Staging Procedure at this Facility continued
Code
Definition
00
No surgical diagnostic or staging procedure was performed
01
A biopsy (incisional, needle, or aspiration) was done to a site other than the primary.
No exploratory procedure was done
02
A biopsy (incisional, needle, or aspiration) was done to the primary site; or biopsy or
removal of a lymph node to diagnose or stage lymphoma
03
A surgical exploration only. The patient was not biopsied or treated
04
A surgical procedure with a bypass was performed, but no biopsy was done
05
An exploratory procedure was performed, and a biopsy of either the primary site or
another site was done
06
A bypass procedure was performed, and a biopsy of either the primary site or another
site was done
07
A procedure was done, but the type of procedure is unknown
09
No information on whether a diagnostic or staging procedure was performed

84
Surgical Diagnostic and Staging Procedure, Days from Dx
Data Dictionary Category: Cancer Identification
PUF Data Item Name: DX_STAGING_PROC_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: 0 - 9999, blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date of Surgical Diagnostic and Staging Procedure (NAACCR Item #1280).
Registry Coding Instructions: None.
Analytic Note: None.
Code
Definition
0 - 9999
Number of elapsed days
blank
No surgical diagnostic and staging procedure,
procedure unknown, elapsed days cannot be
computed, or not available for these diagnosis
85
Stage of Disease: Traditional AJCC Staging
System
86
AJCC Clinical T
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_CLIN_T
NAACCR Item #: 940
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the clinically-determined size and/or extension of the primary tumor (cT) as
defined by the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be
completed by an attending physician, though registry staff were frequently involved in
the determination of the information coded in this item though the review of full
range of clinical and patient notes available to registry staff. For cases diagnosed
January 1, 2004, through December 31, 2007, the CoC required registries to copy the
staging elements from a standardized document found in the patient record, as
recorded by the managing physician. PUF users may notice an increase in the
proportion of cases with cT reported as X as a consequence of the CoC restriction on
the allowable range of registry coding of information beyond that documented by the
managing physician.
The rules changed again with cases diagnosed in 2008. Beginning with 2008 diagnoses,
registrars were required to record clinical stage. If it was not available from a physician,
it was to be coded from information available in the patient record.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in
which the case was diagnosed. Consult the appropriate edition of this manual for organ
or site specific codes and their definitions. See AJCC TNM Edition Number (NAACCR
Item #1060). Prior to implementation of the 5th edition of the manual, some
"slippage" in version occurred, and edition numbers are not included in the PUF for
those older cases.

87
AJCC Clinical T continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition
and for any chapter. Please consult the applicable manual and chapter for codes that
are valid for specific site, histology and AJCC edition combinations.
There is no standard mechanism to recode AJCC items from one edition to another.
Careful review of the individual definitions in the respective AJCC manuals is necessary
before combining or comparing data across two or more AJCC editions.
Code
Definition
Code
Definition
Blank Not available in patient record
2A, c2A
cT2a
2A1, c2A1
cT2a1
X, cX
cTX
2A2, c2A2
cT2a2
0, c0
cT0
2B, c2B
cT2b
A, pA
pTa
2C, c2C
cT2c
IS, pIS
pTis
2D, c2D
cT2d
ISPU, pISPU
pTispu
3, c3
cT3
ISPD, pISPD
pTispd
3A, c3A
cT3a
1MI, c1MI
cT1mic
3B, c3B
cT3b
1, c1
cT1
3C, c3C
cT3c
1A, c1A
cT1a
3D, c3D
cT3d
1A1, c1A1
cT1a1
4, c4
cT4
1A2, c1A2
cT1a2
4A, c4A
cT4a
1B, c1B
cT1b
4B, c4B
cT4b
1B1, c1B1
cT1b1
4C, c4C
cT4c
1B2, c1B2
cT1b2
4D, c4D
cT4d
1C, c1C
cT1c
4E, c4E
cT4e
1D, c1D
cT1d
88
Not applicable
2, c2
cT2
88
AJCC Clinical N
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_CLIN_N
NAACCR Item #: 950
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the clinically-determined absence or presence of regional lymph node (cN)
metastasis and describes the extent of the regional lymph node metastasis as defined
by the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination of
the information coded in this item though the review of full range of clinical and patient notes
available to registry staff. For cases diagnosed January 1, 2004, through December 31, 2007, the
CoC required registries to copy the staging elements from a standardized document found in the
patient record, as recorded by the managing physician. PUF users may notice an increase in the
proportion of cases with cN reported as X as a consequence of the CoC restriction on the
allowable range of registry coding of information beyond that documented by the managing
physician.
The rules changed again with cases diagnosed in 2008. Beginning with 2008 diagnoses,
registrars were required to record clinical stage. If it was not available from a physician, it was
to be coded from information available in the medical record.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version occurred, and
edition numbers are not included in the PUF for those older cases.
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations.

89
AJCC Clinical N continued
There is no standard mechanism to recode AJCC items from one edition to another. Careful review of
the individual definitions in the respective AJCC manuals is necessary before combining or comparing
data across two or more AJCC editions.
Code
Definition
blank
Not available in patient record
X
cNX
0, c0
cN0
0I-, c0I-
cN0i-
0I+, c0I+
cN0i+
0M-, c0M-
cN0m-
0M+, c0M+
cN0m+
1MI, c1MI
cN1mi
0A, c0A
cN0a
0B, c0B
cN0b
1, c1
cN1
1A, c1A
cN1a
1B, c1B
cN1b
1C, c1C
cN1c
2, C2
cN2
2A, c2A
cN2a
2B. c2B
cN2b
2C, c2C
cN2c
3, c3
cN3
3A, c3A
cN3a
3B, c3B
cN3b
3C, c3C
cN3c
4, c4
cN4
88
Not applicable
90
AJCC Clinical M
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_CLIN_M
NAACCR Item #: 960
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the clinically-determined absence or presence of distant metastasis (cM) as
defined by the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules in force for the
particular edition.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination of
the information coded in this item though the review of full range of clinical and patient notes
available to registry staff. For cases diagnosed January 1, 2004, through December 31, 2007,
the CoC required registries to copy the staging elements from a standardized document found in
the patient record, as recorded by the managing physician. PUF users may notice an increase in
the proportion of cases with cM reported as X as a consequence of the CoC restriction on the
allowable range of registry coding of information beyond that documented by the managing
physician.
The rules changed again with cases diagnosed in 2008. Beginning with 2008 diagnoses,
registrars were required to record clinical stage. If it was not available from a physician, it was
to be coded from information available in the medical record.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site-specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version occurred, and
edition numbers are not included in the PUF for those older cases.

91
AJCC Clinical M continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations.
There is no standard mechanism to recode AJCC items from one edition to another. Careful
review of the individual definitions in the respective AJCC manuals is necessary before combining
or comparing data across two or more AJCC editions.
Code
Definition*
blank
Not available in patient record
X, cX
cMX
0, c0
cM0
0I+, c0I+
cM0(i+)
1, c1, p1
cM1, pM1
1A, c1A, p1A
cM1a, pM1a
1B, c1B, p1B
cM1b, pM1b
1C, c1C, p1C
cM1c, pM1c
1D, c1D, p1D
cM1d, pM1d
88
Not applicable (not defined)
*P prefixes were allowed starting in 2016 but can occur
before 2016 for resubmitted cases
92
AJCC Clinical Stage Group
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_CLIN_STAGE_GROUP
NAACCR Item #: 970
Diagnosis Years Available: 2004 - 2017
Length: 4
Allowable Values: Alphanumeric (uppercase), blank
Description:
Identifies the applicable stage group based on the T, N, and M elements as defined by
the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the current AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination of
the information coded in this item through the review of the full range of clinical and patient
notes available to registry staff.
For cases diagnosed January 1, 2004, through December 31, 2007, the CoC required registries to
copy the staging items from a standardized document found in the patient record, as recorded
by the managing physician. PUF users may notice an increase in the proportion of 99s as a
consequence of the CoC restriction on the allowable range of registry coding of information
beyond that documented by the managing physician.
The rules changed again with cases diagnosed in 2008. Beginning with 2008 diagnoses,
registrars were required to record clinical stage. If it was not available from a physician, it was
to be coded from information available in the patient record.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version occurred, and
edition numbers are not included in the PUF for those older cases.
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations.

93
AJCC Clinical Stage Group continued
There is no standard mechanism to recode AJCC items from one edition to another. Careful
review of the individual definitions in the respective AJCC manuals is necessary before
combining or comparing data across two or more AJCC editions.
Code
Definition
Code
Definition
0
cStage 0
2C
cStage IIC
0A
cStage 0A
3
cStage III
0IS
cStage 0is
3A
cStage IIIA
1
cStage I
3B
cStage IIIB
1A
cStage IA
3C
cStage IIIC
1A1
cStage IA1
3C1
cStage IIIC1
1A2
cStage IA2
3C2
cStage IIIC2
1B
cStage IB
4
cStage IV
1B1
cStage IB1
4A
cStage IVA
1B2
cStage IB2
4A1
cStage IVA1
1C
cStage IC
4A2
cStage IVA2
1S
cStage IS
4B
cStage 4B
2
cStage II
4C
cStage IVC
2A
cStage IIA
OC
Occult
2A1
cStage IIA1
88
Not applicable
2A2
cStage IIA2
99
Unknown
2B
cStage IIB
blank
Not available
94
AJCC Pathologic T
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_PATH_T
NAACCR Item #: 880
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the pathologically determined tumor size and/or extension (pT) as defined by
the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination
of the information coded in this item through the review of clinical and patient notes available
to registry staff. For cases diagnosed January 1, 2004, through December 31, 2007, the CoC
required registries to copy the staging elements from a standardized document found in the
patient record, as recorded by the managing physician.
Beginning with 2008 diagnoses, the rules changed again. Physicians were no longer required to
stage, but cancer committees in CoC programs were required to devise plans to ascertain that
staging was used appropriately to make treatment decisions. Registries were encouraged to
record physician staging when it was available, but were not required to do so. The CoC
determined that the stage groups derived from the Collaborative Stage Data Collection System
met the criteria expected of pathologic staging, in providing an AJCC "final stage". PUF users are
likely to see a decrease in the completeness of pathologic staging recorded in the "AJCC" staging
items in the years following 2008.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version occurred, and
edition numbers are not included in the PUF for those older cases.

95
AJCC Pathologic T continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations.
There is no standard mechanism to recode AJCC items from one edition to another. Careful
review of the individual definitions in the respective AJCC manuals is necessary before
combining or comparing data across two or more AJCC editions.
Code
Definition
Code
Definition
blank
Not available in patient record.
Not collected (2008+)
2, p2
pT2
2A, p2A
pT2a
2A1, p2A1
pT2a1
X, px
pTX
2A2, p2A2
pT2a2
0, p0
pT0
2B, p2B
pT2b
A, pA
pTa
2C, p2C
pT2c
IS, pIS
pTis
2D, p2D
pT2d
ISPU, pISPU
pTispu
3, p3
pT3
ISPD, pISPD
pTispd
3A, p3A
pT3a
1MI, p1MI
pT1mic
3B, p3B
pT3b
1, p1
pT1
3C, p3C
pT3c
1A, p1A
pT1a
3D, p3D
pT3d
1A1, p1A1
pT1a1
4, p4
pT4
1A2, p1A2
pT1a2
4A, p4A
pT4a
1B, p1B
pT1b
4B, p4B
pT4b
1B1, p1B1
pT1b1
4C, p4C
pT4c
1B2, p1B2
pT1b2
4D, p4D
pT4d
1C, p1C
pT1c
4E, p4E
pT4e
1D, p1D
pT1d
88
Not applicable
96
AJCC Pathologic N
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_PATH_N
NAACCR Item #: 890
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the pathologically determined absence or presence or extent of regional
lymph node (pN) metastasis as defined by the American Joint Committee on Cancer
(AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination of
the information coded in this item though the review of full range of clinical and patient notes
available to registry staff. For cases diagnosed January 1, 2004, through December 31, 2007, the
CoC required registries to copy the staging elements from a standardized document found in the
patient record, as recorded by the managing physician.
Beginning with 2008 diagnoses, the rules changed again. Physicians were no longer required to
stage, but cancer committees in CoC programs were required to devise plans to ascertain that
staging was used appropriately to make treatment decisions. Registries were encouraged to
record physician staging when it was available, but were not required to do so. The CoC
determined that the stage groups derived from the Collaborative Stage Data Collection System
met the criteria expected of pathologic staging, in providing a AJCC "final stage". PUF users are
likely to see a decrease in the completeness of pathologic staging recorded in the "AJCC" staging
items in the years following 2008.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version was allowed, such
that some codes for cases diagnosed the year prior to implementation of a given edition and the
year following its replacement may also have codes from the edition.

97
AJCC Pathologic N continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations.
There is no standard mechanism to recode AJCC items from one edition to another. Careful
review of the individual definitions in the respective AJCC manuals is necessary before
combining or comparing data across two or more AJCC editions.
For pathologic N, some cancer sites in which lymph node involvement is rare, patients whose
nodal status is not determined to be positive for tumor should be designated as cN0, not pN0.
See the AJCC 8th edition Chapter 1 Principles of Cancer Staging: Node Status Not Required in
Rare Circumstances, at
https://www.facs.org/-/media/files/quality-
programs/cancer/ajcc/principles_cancer_staging.ashx

98
AJCC Pathologic N continued
Code
Definition
blank
Not available in patient record.
Not collected (2008+)
X
pNX
0, p0, c0
pN0, cN0
0I-, p0I-
pN0i-
0I+, p0I+
pN0i+
0M-, p0M-
pN0m-
0M+, p0M+
pN0m+
1MI, p1MI
pN1mi
0A, p0A
pN0a
0B, p0B
pN0b
1, p1
pN1
1A, p1A
pN1a
1B, p1B
pN1b
1C, p1C
pN1c
2, p2
pN2
2A, p2A
pN2a
2B, p2B
pN2b
2C, p2C
pN2c
3, p3
pN3
3A, p3A
pN3a
3B,p3B
pN3b
3C, p3C
pN3c
4, p4
pN4
88
Not applicable
99
AJCC Pathologic M
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_PATH_M
NAACCR Item #: 900
Diagnosis Years Available: 2004 - 2017
Length: 5
Allowable Values: Alphanumeric (uppercase and lowercase), blank
Description:
Identifies the pathologically determined absence or presence of distant metastasis
(pM) as defined by the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed on or prior to December 31, 2003, this item was expected to be completed
by an attending physician, though registry staff were frequently involved in the determination of
the information coded in this item though the review of full range of clinical and patient notes
available to registry staff. For cases diagnosed January 1, 2004, through December 31, 2007, the
CoC required registries to copy the staging elements from a standardized document found in the
patient record, as recorded by the managing physician.
Beginning with 2008 diagnoses, the rules changed again. Physicians were no longer required to
stage, but cancer committees in CoC programs were required to devise plans to ascertain that
staging was used appropriately to make treatment decisions. Registries were encouraged to
record physician staging when it was available, but were not required to do so. The CoC
determined that the stage groups derived from the Collaborative Stage Data Collection System
met the criteria expected of pathologic staging, in providing an AJCC "final stage". PUF users are
likely to see a decrease in the completeness of pathologic staging recorded in the "AJCC" staging
items in the years following 2008.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which
the case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version was allowed, such
that some codes for cases diagnosed the year prior to implementation of a given edition and the
year following its replacement may also have codes from the edition.

100
AJCC Pathologic M continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for
any chapter. Please consult the applicable manual and chapter for codes that are valid for
specific site, histology and AJCC edition combinations. There is no standard mechanism to recode
AJCC items from one edition to another. Careful review of the individual definitions in the
respective AJCC manuals is necessary before combining or comparing data across two or more
AJCC editions.
Code
Definition*
blank
Not available in patient record.
No positive pM. Not collected (2008+)
X, px, cx
pMX, cMX
0, p0, c0
pM0, cM0
0I+, p0I+, c0I+
pM0(i+), cM0(i+)
1, p1, c1
pM1, cM1
1A, p1A, c1A
pM1a, cM1a
1B, p1B, c1B
pM1b, cM1b
1C. p1C, c1C
pM1c, cM1c
1D, p1D, c1D
pM1d, cM1d
88
Not applicable (not defined)
*C prefixes were allowed starting in 2016 but can occur before
2016 for resubmitted cases
101
AJCC Pathologic Stage Group
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_PATH_STAGE_GROUP
NAACCR Item #: 910
Diagnosis Years Available: 2004 - 2017
Length: 4
Allowable Values: Alphanumeric (uppercase), blank
Description:
Identifies the pathologically-determined anatomic extent of disease based on the
T, N, and M elements as defined by the American Joint Committee on Cancer (AJCC).
Registry Coding Instructions:
Refer to the applicable AJCC Cancer Staging Manual for coding rules.
Analytic Note:
For cases diagnosed prior to December 31, 2003, this item was expected to be completed by an
attending physician, though registry staff were frequently involved in the determination of the
information coded in this item through the review of clinical and patient notes available to
registry staff. For cases diagnosed January 1, 2004, through December 31, 2007, the CoC
required registries to copy the staging elements from a standardized document, as recorded by
the managing physician.
Beginning with 2008 diagnoses, the rules changed again. Physicians were no longer required to
stage, but cancer committees in CoC cancer programs were required to devise plans to ascertain
that staging was used appropriately to make treatment decisions. Registries were encouraged to
record physician staging when it was available, but were not required to do so.
The CoC determined that the stage groups derived from the Collaborative Stage Data Collection
System met the criteria expected of pathologic staging, in providing an AJCC "final stage". PUF
users are likely to see a decrease in the completeness of pathologic staging in the "AJCC' staging
items in the years following 2008.
Cases are coded using the AJCC Cancer Staging Manual edition in use during the year in which the
case was diagnosed. Consult the appropriate edition of this manual for organ or site specific
codes and their definitions. See AJCC TNM Edition Number (NAACCR Item #1060). Prior to
implementation of the 5th edition of the manual, some "slippage" in version was allowed, such
that some codes for cases diagnosed the year prior to implementation of a given edition and the
year following its replacement may also have codes from the edition.

102
AJCC Pathologic Stage Group continued
Codes on this list comprise all codes valid for any AJCC manual through the 7th edition and for any
chapter. Please consult the applicable manual and chapter for codes that are valid for specific
site, histology and AJCC edition combinations. There is no standard mechanism to recode AJCC
items from one edition to another. Careful review of the individual definitions in the respective
AJCC manuals is necessary before combining or comparing data across two or more AJCC editions.
Code
Definition
Code
Definition
0
pStage 0
3
pStage III
0A
pStage 0A
3A
pStage IIIA
0IS
pStage 0is
3B
pStage IIIB
1
pStage I
3C
pStage IIIC
1A
pStage IA
3C1
pStage IIIC1
1A1
pStage IA1
3C2
pStage IIIC2
1A2
pStage IA2
4
pStage IV
1B
pStage IB
4A
pStage IVA
1B1
pStage IB1
4A1
pStage IVA1
1B2
pStage IB2
4A2
pStage IVA2
1C
pStage IC
4B
pStage 4B
1S
pStage IS
4C
pStage IVC
2
pStage II
OC
Occult
2A
pStage IIA
88
Not applicable
2A1
pStage IIA1
99
Unknown
2A2
pStage IIA2
blank
No pathologic
staging for this
case (2008+ only)
2B
pStage IIB
2C
pStage IIC

103
TNM Edition Number
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TNM_EDITION_NUMBER
NAACCR Item #: 1060
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 06-08, 88, 99
Description:
Identifies the edition number of the AJCC Cancer Staging Manual used to stage the case.
Registry Coding Instructions:
None; this item may be auto-coded by cancer registry software.
Analytic Note:
AJCC staging is coded according to the version of the AJCC Cancer Staging Manual in use
at the time the case was diagnosed. Prior to implementation of the 5th edition of the
manual, some "slippage" in version occurred, and edition numbers are not included in
the PUF for those older cases.
Code
Definition
00
Not staged (cases that have AJCC staging scheme and staging was not done)
06
Sixth Edition
07
Seventh Edition
08
Eighth Edition
88
Not applicable (cases that do not have an AJCC staging scheme)
99
Staged, but the edition is unknown

104
NCDB Analytic Stage Group
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: ANALYTIC_STAGE_GROUP
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 5, 8, 9
Description:
Analytic Stage Group is assigned the value of reported Pathologic Stage Group (NAACCR
Item #910). Clinical Stage Group (NAACCR Item #970) is used if Pathologic Stage Group
(NAACCR Item #910) is not reported. Sub-stage groups are collapsed into the
corresponding general stage designation. The alphanumeric representation of stage
group is provided for ease of display.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
0
Stage 0
1
Stage I
2
Stage II
3
Stage III
4
Stage IV
5
Occult (lung only)
8
AJCC staging not applicable
9
AJCC stage group unknown
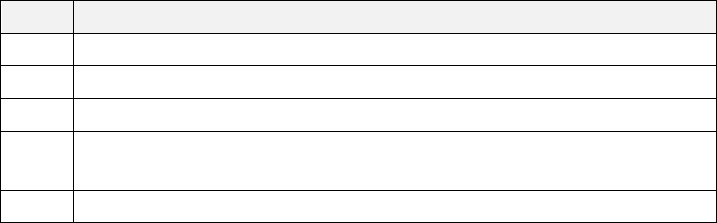
105
Mets at Diagnosis – Bone
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_BONE
NAACCR Item #: 1112
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description: This data item identifies whether bone is an involved metastatic site.
Registry Coding Instructions:
Code information about bone metastases only (discontinuous or distant metastases to
bone) identified at the time of diagnosis. This field should not be coded for bone
marrow involvement. Bone involvement may be single or multiple. Information about
bone involvement may be clinical or pathologic.
Code this field regardless of whether the patient had any preoperative systemic
therapy. This field should be coded for all solid tumors, Kaposi sarcoma, Unknown
Primary Site, and Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin’s and non-Hodgkin’s Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had bone metastases; for example, when there is documentation of
carcinomatosis but bone is not specifically mentioned as a metastatic site.
Analytic Note: This is a new item in 2016, replacing the CS Mets at DX-Bone (NAACCR Item #2851) item.
Code
Definition
0
None; no bone metastases
1
Yes, distant bone metastases
8
Not applicable
9
Unknown whether bone is involved metastatic site; Not documented
in patient record
blank
Not available

106
Mets at Diagnosis – Brain
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_BRAIN
NAACCR Item #: 1113
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description: This data item identifies whether brain is an involved metastatic site.
Registry Coding Instructions:
Code information about brain metastases only (discontinuous or distant metastases to
brain) identified at the time of diagnosis. This field should not be coded for
involvement of spinal cord or other parts of the central nervous system. Brain
involvement may be single or multiple. Information about brain involvement may be
clinical or pathologic. Code this field regardless of whether the patient had any
preoperative systemic therapy. This field should be coded for all solid tumors, Kaposi
sarcoma, Unknown Primary Site, and Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin and non-Hodgkin’s Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had brain metastases; for example, when there is documentation of
carcinomatosis but brain is not specifically mentioned as a metastatic site.
A
nalytic Note: This is a new item in 2016, replacing the CS Mets at DX-Brain (NAACCR
Item #2852) item.
Code
Definition
0
None; no brain metastases
1
Yes, distant brain metastases
8
Not applicable
9
Unknown whether brain is involved metastatic site; Not documented
in patient record
blank
Not available

107
Mets at Diagnosis – Liver
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_LIVER
NAACCR Item #: 1115
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description: This data item identifies whether liver is an involved metastatic site.
Registry Coding Instructions:
Code information about liver metastases only (discontinuous or distant metastases to
brain) identified at the time of diagnosis. Liver involvement may be single or multiple.
Information about liver involvement may be clinical or pathologic. Code this field
regardless of whether the patient had any preoperative systemic therapy.
This field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site,
and Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin’s and non-Hodgkin’s Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had liver metastases; for example, when there is documentation of
carcinomatosis but liver is not specifically mentioned as a metastatic site.
Analytic Note: This is a new item in 2016, replacing the CS Mets at DX-Liver (NAACCR Item #2853) item.
Code
Definition
0
None; no liver metastases
1
Yes, distant liver metastases
8
Not applicable
9
Unknown whether liver is involved metastatic site; Not documented
in patient record
blank
Not available

108
Mets at Diagnosis – Lung
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_LUNG
NAACCR Item #: 1116
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description: This data item identifies whether lung is an involved metastatic site.
Registry Coding Instructions:
Code information about lung metastases only (discontinuous or distant metastases to
brain) identified at the time of diagnosis. Lung involvement may be single or multiple.
Information about lung involvement may be clinical or pathologic.
Code this field whether or not the patient had any preoperative systemic therapy.
This field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site,
and Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin’s and non-Hodgkin’s Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had lung metastases; for example, when there is documentation of
carcinomatosis but lung is not specifically mentioned as a metastatic site.
Analytic Note: This is a new item in 2016, replacing the CS Mets at DX-Lung (NAACCR Item #2854) item.
Code
Definition
0
None; no lung metastases
1
Yes, distant lung metastases
8
Not applicable
9
Unknown whether lung is involved metastatic site; Not documented
in patient record
blank
Not available
109
Mets at Diagnosis – Other
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_OTHER
NAACCR Item #: 1117
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0 - 2, 8, 9, blank
Description:
This data item identifies whether other metastatic involvement, other than bone, brain, liver,
lung or distant lymph nodes exists. Some examples include but are not limited to the adrenal
gland, bone marrow, pleura, peritoneum, and skin. The five Mets at Dx Metastatic Sites
variables provide information on specific metastatic sites for data analysis.
Rationale:
Information on site of metastatic disease at diagnosis has prognostic implications to
survival among patients with initial late stage disease. Capturing data on where the
patient’s metastatic lesions (including the number of locations) will be an important
variable to look at when looking a survival. Survival among metastatic patients is
becoming increasingly important for cancer survivors. CoC requires this data item be
recorded in its accredited cancer program registries beginning with cases diagnosed
January 1, 2016.
Registry coding instructions:
1. Code information about other metastases only (discontinuous or distant metastases) identified at
the time of diagnosis. This data item should not be recorded for bone, brain, liver, lung or distant
lymph node metastases.
a. Other involvement may be single or multiple.
b. Information about other involvement may be clinical or pathological.
c. Code this data item whether or not the patient had any preoperative systemic therapy.
d. This data item should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site, and
Other and Ill-Defined Primary Sites.
2. Use of codes. Assign the code that best describes whether the case has other metastases at
diagnosis.
a. Use code 0 when the medical record
i. indicates that there are no distant (discontinuous) metastases at all
ii. includes a clinical or pathologic statement that there are no other metastases
iii. includes imaging reports that are negative for other metastases
110
iv. indicates that the patient had distant (discontinuous) metastases but other sites are not
mentioned as involved.
Example: Use code 0 when the patient has lung and liver metastases only.

111
Mets at Diagnosis Other continued
b. Use code 1 when the medical record
i. indicates that the patient has distant (discontinuous) metastases in any site(s) other than
bone, brain, liver, lung or distant lymph node(s).
c. Use code 8 (Not applicable) for the following site/histology combinations for which a code for
distant metastases is not clinically relevant.
ICD-0-3 Site
ICD-0-3 Histology
C000-C809
9740-9809, 9840-9992
Mast cell, histiocytosis,
immunoproliferative,
leukemias coded to any site
C420, C421, C424
9811-9818, 9823,9827,9837
Specific leukemia/lymphoma
histologies coded to blood,
bone, bone marrow,
hematopoietic
C000-C440, C442-C689,
C691-C694, C698-C809
9820, 9826, 9831-9834
Mostly lymphoid leukemias
coded to any site except
eyelid, conjunctiva, lacrimal
gland, orbit, and eye
overlapping and NOS
C000-C440, C442-C689,
C691-C694, C698-C809
9731, 9732, 9734
Plasma cell tumors coded to
any site except eyelid,
conjunctiva, lacrimal gland,
orbit, and eye overlapping and
NOS
d. Use code 9 when it cannot be determined from the medical record whether the patient has
metastases other than bone, brain, liver, lung, and distant lymph node(s); for example, when
there is documentation of carcinomatosis but a specified site is not mentioned as a metastatic
site. In other words, use code 9 when there are known distant metastases but is not known
specifically what they are.
Analytic note: This variable was added as a FORDS item in 2016.

112
Mets at Diagnosis Other continued
Code
Definition
0
None; no other metastases
1
Yes; distant metastases in known site(s) other than bone, brain, liver,
lung or distant lymph nodes
2
Generalized metastases such as carcinomatosis
8
Not applicable
9
Unknown whether any other metastatic site. Not documented in
patient record
blank
Not available
113
Mets at Diagnosis - Distant Lymph Nodes
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: METS_AT_DX_DISTANT_LN
NAACCR Item #: 1114
Diagnosis Years Available: 2016 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
This data item identifies whether distant lymph node(s) are an involved metastatic site. The five
Mets at Dx Metastatic Site variables provide information on specific metastatic sites for data
analysis.
Rationale:
Information on site of metastatic disease at diagnosis has prognostic implications to
survival among patients with initial late stage disease. Capturing data on where the
patient’s metastatic lesions (including the number of locations) will be an important
variable to look at when looking a survival. Survival among metastatic patients is
becoming increasingly important for cancer survivors. CoC requires this data item be
recorded in its accredited cancer program registries beginning with cases diagnosed
January 1, 2016.
Registry coding instructions:
1. Code information about distant lymph node(s) metastases only (metastases to distant lymph
nodes) identified at the time of diagnosis.
a. Distant lymph node metastases may be single or multiple.
b. Information about distant lymph node involvement may be clinical or pathologic
c. Code this data item whether or not the patient had any preoperative systemic therapy.
d. This data item should not be coded for regional lymph node involvement with the exception of
lymph nodes for placenta which are M1.
e. This data item should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site, and
Other and Ill-defined primary sites.
2. Use of codes. Assign the code that best describes whether the case has distant lymph node
metastases at diagnosis.
a. Use code 0 when the medical record
i. indicates that there are no distant (discontinuous) metastases at all
ii. includes a clinical or pathologic statement that there are no distant lymph node metastases
iii. includes imaging reports that are negative for distant lymph node metastases
114
iv. indicates that the patient had distant (discontinuous) metastases but distant lymph node(s)
are not mentioned as an involved site.
Example: Use code 0 when the patient has lung and liver metastases but not distant lymph
node(s)

115
Mets at Diagnosis Distant Lymph Nodes continued
b. Use code 1 when the medical record
i. indicates that the patient has distant (discontinuous) metastases and distant lymph node(s)
are mentioned as an involved site.
ii. indicates that the patient is diagnosed as an unknown primary (C80.9) and distant lymph
node(s) are mentioned as a metastatic site.
c. Use code 8 (Not applicable) for the following site/histology combinations for which a code for
distant metastases is not clinically relevant.
ICD-0-3 Site
ICD-0-3 Histology
C000-C809
9740-9809, 9840-9992
Mast cell, histiocytosis,
immunoproliferative,
leukemias coded to any site
C420, C421, C424
9811-9818, 9823,9827,9837
Specific leukemia/lymphoma
histologies coded to blood,
bone, bone marrow,
hematopoietic
C000-C440, C442-C689,
C691-C694, C698-C809
9820, 9826, 9831-9834
Mostly lymphoid leukemias
coded to any site except
eyelid, conjunctiva, lacrimal
gland, orbit, and eye
overlapping and NOS
C000-C440, C442-C689,
C691-C694, C698-C809
9731, 9732, 9734
Plasma cell tumors coded to
any site except eyelid,
conjunctiva, lacrimal gland,
orbit, and eye overlapping and
NOS
d. Use code 9 when it cannot be determined from the medical record whether the patient
specifically has lymph node metastases; for example, when there is documentation of
carcinomatosis but distant lymph node(s) are not mentioned as a metastatic site. In other words,
use code 9 when there are known distant metastases but is not known whether the distant
metastases include distant lymph node(s).
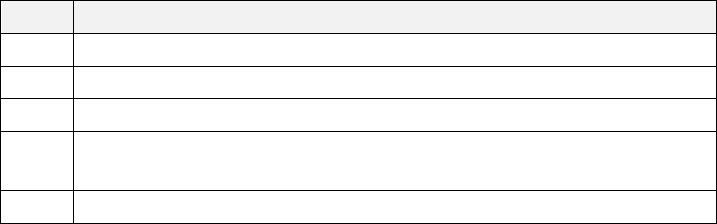
116
Mets at Diagnosis Distant Lymph Nodes continued
Analytic note: This variable was added as a FORDS item in 2016.
Code
Definition
0
None; no distant lymph node metastases
1
Yes; distant lymph node metastases
8
Not applicable
9
Unknown whether distant lymph node(s) are an involved metastatic
site. Not documented in patient record
blank
Not available
117
Tumor Size Summary
Data Dictionary Category: Stage of Disease Traditional AJCC Staging System
PUF Data Item Name: TUMOR_SIZE_SUMMARY_2016
NAACCR Item #: 756
Diagnosis Years Available: 2016 +
Length: 3
Allowable Values: 000 - 990, 998, 999, blank
Description:
Describes the most accurate measurement of a solid primary tumor, usually measured
on the surgical resection specimen. Describes the largest dimension of the diameter of
the primary tumor in millimeters.
Rationale:
Tumor size is one indication of the extent of the disease. As such, it is used by both
clinicians and researchers. Tumor size that is independent of stage is also useful for quality
assurance efforts.
Registry coding instructions:
Note: All measurements should be in millimeters (mm).
Record size in specified order:
1. Size measured on the surgical resection specimen, when surgery is administered as the first
definitive treatment, i.e. no pre-surgical treatment administered.
a. If there is a discrepancy among tumor size measurements in the various sections of the
pathology report, code the size from the synoptic report (also known as CAP protocol or
pathology report checklist.) If only a text report is available, use: final diagnosis, microscopic, or
gross examination, in that order.
Example: Chest x-ray shows 3.5 cm mass; the pathology report from the surgery states that the
same mass is malignant and measures 2.8 cm. Record tumor size as 028 (28 mm).
Example: Pathology report states lung carcinoma is 2.1 cm x 3.2 cm x 1.4 cm. Record tumor size
as 032 (32 mm).
2. If neoadjuvant therapy followed by surgery, do not record the size of the pathologic specimen. Code
the largest size of tumor prior to neoadjuvant treatment; if unknown code size as 999.
118
Tumor Size Summary continued
Example: Patient has a 2.2 cm mass in the oropharynx; fine needle aspiration of mass confirms
squamous cell carcinoma. Patient receives a course of neoadjuvant combination chemotherapy.
Pathologic size after total resection is 2.8 cm. Record tumor size as 022 (22 mm).
3. If no surgical resection, then largest measurement of the tumor from physical exam, imaging, or other
diagnostic procedures prior to any other form of treatment. (See Coding Rules below).
4. If 1,2 and 3 do not apply, the largest size from all information available within four months of the date
of diagnosis, in the absence of disease progression.
Coding Rules:
1. Tumor size is the diameter of the tumor, not the depth or thickness of the tumor.
2. Recording less than/greater than Tumor Size:
a. If tumor size is reported as less than x mm or less than x cm, the reported tumor size should
be 1 mm less; for example, if size is <10mm, code size as 009. Often these are given in cm
such as < 1 cm which is coded as 009, < 2 cm is coded as 019, < 3 cm is coded as 029, < 4 cm is
coded as 039, < 5 cm is coded as 049. If stated as less than 1 mm, use code 001.
b. If tumor size is reported as more than x mm or more than x cm, code size as 1 mm more; for
example, if size is > 10 mm, size should be coded as 011. Often these are given in cm such as >
1 cm, which coded as 011, > 2 cm coded as 021, > 3 cm is coded as 031, > 4 cm is coded as
041, > 5 cm is coded as 051. If described as anything greater than 989 mm (98.9 cm) code as
989.
c. If tumor size is reported to be between two sizes, record tumor size as the midpoint between
the two; i.e., add the two sizes together and then divide by two (“between 2 and 3 cm is
coded as 025).
3. Rounding: Round the tumor size only if it is described in fractions of millimeters. If the largest
dimension of a tumor is less than 1 millimeter (between 0.1 and 0.9 mm), record size as 001 (do
not round down to 000). If tumor size is greater than 1 millimeter, round tenths of millimeters in
the 1-4 range down to the nearest whole millimeter, round tenths of millimeters in the 5-9 range
up to the nearest whole millimeter. Do not round tumor size expressed in centimeters to the
nearest whole centimeter (rather, move the decimal point one space to the right, converting the
measurement to millimeters.
Examples:
Breast cancer described as 6.5 millimeters in size. Round up Tumor Size as 007.
Cancer in polyp described as 2.3 millimeters in size. Round down Tumor Size as 002.
Focus of cancer described as 1.4 mm in size. Round down as 001.
5.2 mm breast cancer. Round down to 5 mm and code as 005.
4. Priority of imaging/radiographic techniques: Information on size from imaging/radiographic
techniques can be used to code size when there is no more specific size information from a
pathology or operative report, but is should be taken as low priority, over a physical exam.
119
Tumor Size Summary continued
5. Tumor size discrepancies among imaging and radiographic techniques. If there is a difference in
reported tumor size among imaging and radiographic techniques, unless the physician specifies
which imaging is most accurate, record the largest size in the record, regardless of which imaging
technique reports it.
6. Always code the size of the primary tumor, not the size of the polyp, ulcer, cyst, or distant
metastases. However, if the tumor is described as a “cystic mass,” and only the size of the entire
mass is given, code the size of the entire mass, since the cysts are part of the tumor itself.
7. Record the size of the invasive component, if given.
a. If both an in situ and invasive component are present and the invasive component is
measured, record the size of the invasive component, even if it is smaller.
Example: Tumor is mixed in situ and invasive adenocarcinoma, total 3.7 cm in size, of which
1.4 cm is invasive. Record tumor size as 014 (14 mm).
b. If the size of the invasive component is not given, record the size of the entire tumor from the
surgical report, pathology report, radiology report or clinical examination.
Example: A breast tumor with infiltrating duct carcinoma with extensive in situ component;
total size 2.3 cm. Record tumor size as 023 (23 mm).
Example: Duct carcinoma in situ measuring 1.9 cm with an area of invasive ductal carcinoma.
Record tumor size as 019 (19 mm).
8. Record the largest dimension or diameter of the tumor, whether it is from an excisional biopsy
specimen or the complete resection of the primary tumor.
Example: Tumor is described as 2.4 x 5.1 x 1.8 cm in size. Record tumor size as 051 (51 mm).
9. Record the size as stated for purely in situ lesions.
10. Disregard microscopic residual or positive surgical margins when coding tumor size. Microscopic
residual tumor does not affect overall tumor size. The status of primary tumor margins may be
recorded in a separate data item.
11. Do not add the size of pieces or chips together to create a whole; they may not be from the same
location, or they may represent only a very small portion of a large tumor. However, if the
pathologist states an aggregate or composite size (determined by fitting the tumor pieces together
and measuring the total size), record that size. If the only measurement describes pieces or chips,
record tumor size as 999.
12. Multifocal/multcentric tumors: If the tumor is mult-focal or if multiple tumors are reported as a
single primary, code the size of the largest invasive tumor or if all of the tumors are in situ, code
the size of the largest in situ tumor.
13. Tumor size code 999 is used when size is unknown or not applicable. Sites/morphologies where
tumor size is not applicable are listed here: Hematopoietic, Reticuloendothelial, and
Myeloproliferative neoplasms: histology codes: 9590-9992; Kaposi’s sarcoma, Melanoma Choriod,
Melanoma Ciliary Body, Melanoma Iris.
14. Document the information to support coded tumor size in the appropriate text data item of the
abstract.

120
Tumor Size Summary continued
Analytic note:
This variable was added as a FORDS item in 2016, replacing the CS Tumor Size (NAACCR
Item #2800) variable collected in 2004 - 2015. Use the CS Tumor Size (NAACCR Item
#2800) variable for 2004 - 2015 diagnosis years, and the Tumor Size Summary (NAACCR
Item #756) for cases diagnosed in 2016 and later. This field is blank for melanoma of
the skin. Use CS Site-Specific Factor 1 (NAACCR Item #2880) to obtain Breslow’s depth
for melanoma of the skin. The codes for Tumor Size Summary (NAACCR Item #756) are
slightly different from those in the CS Tumor Size (NAACCR Item #2800) variable.
Code
Definition
000
No mass/tumor found
001
1 mm or described as less than 1 mm
002-988
Exact size in millimeters (2 mm to 988 mm)
989
989 millimeters or larger
990
Microscopic focus or foci only and no size of focus is given
998
SITE SPECIFIC CODES
Alternate descriptions of tumor size for specific sites:
Familial/multiple polyposis: Rectosigmoid and rectum (C19.9,
C20.9) and Colon (C18.0, C18.2-C18.9)
If no size is documented:
Circumferential: Esophagus (C15.0-C15.5, C15.8-C15.9)
Diffuse; widespread: 3/4s or more; linitis plastica: Stomach
and Esophagus GE Junction (C16.0-C16.6, C16.8-C16.9)
Diffuse, entire lung or NOS: Lung and main stem bronchus
(C34.0-C34.3, C34.8-C34.9)
Diffuse: Breast (C50.0-C50.6, C50.9-C50.9)
999
Unknown; size not stated. Not documented in patient
record. Size of tumor cannot be assessed. Not applicable
blank
Not available
121
Stage of Disease
AJCC 8
th
Edition Staging System
122
AJCC 8
th
Edition Clinical T
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_CLIN_T
NAACCR Item #: 1001
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description: Evaluates the primary tumor (T) and reflects the tumor size and/or extension of the tumor
known prior to the start of any therapy. Detailed site-specific values for the clinical T category as defined
by the current AJCC edition.
Rationale: The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective
January 1, 2018, the CoC requires use of the AJCC 8th Edition Staging System in its accredited program
cancer registries. The AJCC developed this staging system for evaluating trends in the treatment and
control of cancer. This staging system is used by physicians to estimate prognosis, plan treatment,
evaluate new types of therapy, analyze outcomes, design follow-up strategies, and to assess early
detection results. With the implementation of the 8th Edition, storage codes are no longer utilized.
Codes and Labels for the different categories are exact matches to what is listed in the 8th Edition
Manual (except for code 88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions
• The clinical T category staging data item must be recorded for Class of Case 10-22.
• It is strongly recommended that the clinical T category staging data item be recorded for Class of Case
00 cases if the patient’s workup at the facility allows assigning of clinical T.
• Assign clinical T category as documented by the first treating physician or the managing physician in
the medical record.
• If the managing physician has not recorded clinical T, registrars will assign this item based on the best
available information, without necessarily requiring additional contact with the physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Refer to the current AJCC Cancer Staging Manual, Eighth Edition for detailed staging rules.
124
AJCC TNM Clin T Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_CLIN_T_SFX
NAACCR Item #: 1031
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (m), (s), Blank
Description:
Identifies the AJCC TNM clinical T category suffix for the tumor prior to the start of any therapy. Stage
suffixes identify special cases that need separate analysis. Suffixes are adjuncts to and do not change the
stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Codes and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• Record the clinical T category suffix as documented by the first treating physician or the managing
physician in the medical record.
• If the managing physician has not recorded the suffix when applicable, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

125
AJCC TNM Clin T Suffix, continued
Code
Label
(blank)
No information available; not recorded
(m)
Multiple synchronous tumors OR Multifocal tumor (differentiated and anaplastic thyroid
only)
(s)
Solitary tumor (differentiated and anaplastic thyroid only)
126
AJCC 8
th
Edition Clinical N
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_CLIN_N
NAACCR Item #: 1002
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description: Identifies the absence or presence of regional lymph node (N) metastasis and describes the
extent of regional lymph node metastasis of the tumor known prior to the start of any therapy. Detailed
site specific values for the clinical N category as defined by the current AJCC edition.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Codes and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions
• The clinical N category staging data item must be assigned for Class of Case 10-22.
• It is strongly recommended that the clinical N category staging data item be recorded for Class of Case
00 cases if the patient’s workup at the facility allows assigned of clinical N category.
• Record clinical N category as documented by the first treating physician or the managing physician in
the medical record.
• If the managing physician has not recorded clinical N, registrars will assign this item based on the best
available information, without necessarily requiring additional contact with the physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

127
AJCC 8
th
Edition Clinical N, continued
The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded and
are now consistent for clarity. Refer to the STORE manual for the list of codes, p. 198.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
128
AJCC TNM Clin N Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_CLIN_N_SFX
NAACCR Item #: 1034
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (sn), (f), Blank
Description:
Identifies the AJCC TNM clinical N category suffix for the tumor prior to the start of any therapy. Stage
suffices identify special cases that need separate analysis. Suffices are adjuncts to and do not change the
stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions
• Record the clinical N category suffix as documented by the first treating physician or the managing
physician in the medical record.
• If the managing physician has not recorded the suffix when applicable, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules

129
AJCC TNM Clin M Suffix, continued
Code
Label
(blank)
No information available; not recorded
(sn)
Sentinel node procedure with or without FNA or core needle biopsy
(f)
FNA or core needle biopsy only
130
AJCC 8
th
Edition Clinical M
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_CLIN_M
NAACCR Item #: 1003
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the presence or absence of distant metastasis (M) of the tumor known prior to the start of any
therapy. Detailed site-specific values for the clinical T category suffix as defined by the current AJCC
edition.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions
• The clinical M category staging data item must be assigned for Class of Case 10-22. • It is strongly
recommended that the clinical M category staging data item be recorded for Class of Case 00 cases if
the patient’s workup at the facility allows assigning of clinical M.
• Record clinical M category as documented by the first treating physician or managing physician in the
medical record.
• If the managing physician has not recorded clinical M category, registrars will assign this item based
on the best available information, without necessarily requiring additional contact with the physician. •
Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a site/histology
combination is not defined in the current AJCC edition and for in situ tumors that are not staged
according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.

131
AJCC 8
th
Edition Clinical M continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 202 for the valid list of codes at
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
132
AJCC 8
th
Edition Clinical Stage Group
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_CLIN_STG_GRP
NAACCR Item #: 1004
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the anatomic extent of disease based on the T, N, and M category data items known prior to
the start of any therapy. Detailed site-specific values for the clinical stage group as defined by the
current AJCC edition.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are still utilized for the stage groups only due
to the decision to maintain Arabic numerals in the stage groups. New groups will be used for cases
diagnosed in 2018 and later.
Coding Instructions
• Record the clinical stage group as documented by the first treating physician or the managing
physician in the medical record.
• If the managing physician has not recorded the clinical stage, registrars will assign this item based on
the best available information, without necessarily requiring additional contact with the physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Convert all Roman numerals to Arabic numerals and use upper-case (capital letters) only. • Refer to
the current AJCC Cancer Staging Manual for staging rules.

133
AJCC 8
th
Edition Clinical Stage Group, continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 204 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
134
AJCC 8
th
Edition Pathologic T
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_T
NAACCR Item #: 1011
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Evaluates the primary tumor (T) and reflects the tumor size and/or extension of the tumor known
following the completion of surgical therapy. Detailed site-specific values for the pathological tumor (T)
as defined by the current AJCC edition.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The pathological T category staging data item must be assigned for Class of Case 10-22.
• Assign pathological T as documented by the treating physician(s) or the managing physician in the
medical record.
• If the managing physician has not recorded pathological T category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• For lung, occult carcinoma is assigned TX.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.

135
AJCC 8
th
Edition Pathologic T continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual pages 207-208 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
136
AJCC TNM Path T Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_T_SFX
NAACCR Item #: 1032
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (m), (s), blank
Description:
Identifies the AJCC TMN pathological T category suffix for the tumor following the completion of surgical
therapy. Stage suffices identify special cases that need separate analysis. Suffices are adjuncts to and do
not change the stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2008 the CoC requires that AJCC clinical TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions
• Record the pathological stage T category suffix as documented by the first treating physician or the
managing physician in the medical record.
• If the managing physician has not recorded the descriptor, registrars will assign this item based on the
best available information, without necessarily requiring additional contact with the physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

137
AJCC TNM Path T Suffix, continued
Code
Label
(blank)
No information available; not recorded
(m)
Multiple synchronous tumors OR
Multifocal tumor (differentiated and anaplastic thyroid only)
(s)
Solitary tumor (differentiated and anaplastic thyroid only)
138
AJCC 8
th
Edition Pathologic N
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_N
NAACCR Item #: 1012
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the absence or presence of regional lymph node (N) metastasis and describes the extent of
regional lymph node metastasis of the tumor known following the completion of surgical therapy.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The pathological N category staging data item must be assigned for Class of Case 10-22.
• Assign pathological N category as documented by the treating physician(s) or managing physician in
the medical record.
• If the managing physician has not recorded pathological N category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.

139
AJCC 8
th
Edition Pathologic N, continued
• Refer to the current AJCC Cancer Staging Manual for staging rules.
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 211 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx

140
AJCC TNM Path N Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_N_SFX
NAACCR Item #: 1035
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (sn), (f), blank
Description:
Identifies the AJCC TNM pathological N suffix for the tumor following the completion of surgical therapy.
Stage suffices identify special cases that need separate analysis. Suffices are adjuncts to and do not
change the stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2008 the CoC requires that AJCC pathological TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions:
• Record the pathological N category suffix as documented by the first treating physician or the
managing physician in the medical record.
• If the managing physician has not recorded the descriptor, registrars will assign this item based on the
best available information, without necessarily requiring additional contact with the physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.
Code
Label
(blank)
No information available; not recorded
(sn)
Sentinel node procedure with or without FNA or core needle biopsy
(f)
FNA or core needle biopsy only
141
AJCC 8
th
Edition Pathologic M
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_M
NAACCR Item #: 1013
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the presence or absence of distant metastasis (M) of the tumor known following the
completion of surgical therapy.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The pathological M category staging data item must be assigned for Class of Case 10-22.
• Assign pathological M category as documented by the treating physician(s) or the managing physician
in the medical record.
• If the managing physician has not recorded pathological M category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

142
AJCC 8
th
Edition Pathologic M, continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 214 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
143
AJCC 8
th
Edition Pathologic Stage Group
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_ TNM_PATH_STG_GRP
NAACCR Item #: 1014
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the anatomic extent of disease based on the T, N, and M category data items known following
the completion of surgical therapy.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2015 the CoC requires that AJCC pathological TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions:
• Record the pathological stage group as documented by the treating physician(s) or the managing
physician in the medical record.
• If the managing physician has not recorded the pathological stage, registrars will assign this item based
on the best available information, without necessarily requiring additional contact with the physician(s).
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Convert all Roman numerals to Arabic numerals and use upper-case (capital letters) only.
• Refer to the current AJCC Cancer Staging Manual for staging rules.
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
145
AJCC TNM Post Therapy Path (yp) T
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_T
NAACCR Item #: 1021
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Evaluates the primary tumor (T) and reflects the tumor size and/or extension of the tumor known
following the completion of neoadjuvant therapy (satisfying the definition for that disease site) and
planned post-neoadjuvant therapy surgical resection.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The post therapy T category staging data item must be assigned for Class of Case 10-22.
• Assign post therapy T category as documented by the treating physician(s) or the managing physician
in the medical record.
• If the managing physician has not recorded post therapy T category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• For lung, occult carcinoma is assigned TX.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.

146
AJCC TNM Post Therapy T continued
• Refer to the current AJCC Cancer Staging Manual for staging rules.
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 219 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
147
AJCC TNM Post Therapy Path (yp) T Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_T_SFX
NAACCR Item #: 1033
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (m), (s), blank
Description:
Identifies the AJCC TNM post therapy T category suffix for the tumor following the completion of
neoadjuvant therapy (satisfying the definition for that disease site) and planned post-neoadjuvant
therapy surgical resection. Stage suffices identify special cases that need separate analysis. Suffices are
adjuncts to and do not change the stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2008 the CoC requires that AJCC clinical TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions
• Record the post therapy T category suffix as documented by the first treating physician or the
managing physician in the medical record.
• If the managing physician has not recorded the post therapy T category suffix, registrars will assign this
item based on the best available information, without necessarily requiring additional contact with the
physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.
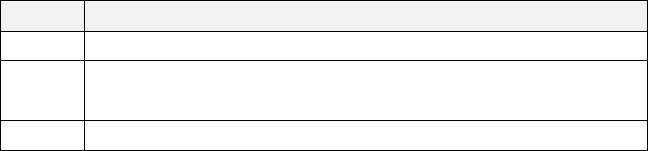
148
AJCC TNM Post Therapy T Suffix, continued
Code
Label
(blank)
No information available; not recorded
(m)
Multiple synchronous tumors OR
Multifocal tumor (differentiated and anaplastic thyroid only)
(s)
Solitary tumor (differentiated and anaplastic thyroid only)
149
AJCC TNM Post Therapy Path (yp) N
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_N_SFX
NAACCR Item #: 1022
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the absence or presence of regional lymph node (N) metastasis and describes the extent of
lymph node metastasis for the tumor following the completion of neoadjuvant therapy (satisfying the
definition for that disease site) and planned post-neoadjuvant therapy surgical resection.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The post therapy N category staging data item must be assigned for Class of Case 10-22.
• Assign post therapy N category as documented by the treating physician(s) or managing physician in
the medical record.
• If the managing physician has not recorded post therapy N category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

150
AJCC TNM Post Therapy N, continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 222 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
151
AJCC TNM Post Therapy Path (yp) N Suffix
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_N_SFX
NAACCR Item #: 1036
Diagnosis Years Available: 2018 +
Length: 4
Allowable Values: (sn), (f), blank
Description:
Identifies the AJCC TNM post therapy N suffix for the tumor known following the completion of
neoadjuvant therapy (satisfying the definition for that disease site) and planned post-neoadjuvant
therapy surgical resection. Stage suffices identify special cases that need separate analysis. Suffices are
adjuncts to and do not change the stage group.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2008 the CoC requires that AJCC clinical TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions
• Record the post therapy N category suffix as documented by the first treating physician or the
managing physician in the medical record.
• If the managing physician has not recorded the post therapy N category suffix, registrars will assign
this item based on the best available information, without necessarily requiring additional contact with
the physician.
• If the tumor is not staged according to the AJCC manual, leave this data item blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

152
AJCC TNM Post Therapy N Suffix, continued
Code
Label
(blank)
No information available; not recorded
(sn)
Sentinel node procedure with or without FNA or core needle biopsy
(f)
FNA or core needle biopsy only
153
AJCC Post Therapy Path (yp) M
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_M
NAACCR Item #: 1023
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the presence or absence of distant metastasis (M) of the tumor known following the
completion of neoadjuvant therapy (satisfying the definition for that disease site) and planned post-
neoadjuvant therapy surgical resection.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2018 the CoC requires use of the AJCC 8th Edition Staging System in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
With the implementation of the 8th Edition, storage codes are no longer utilized. Values and Labels for
the different categories are exact matches to what is listed in the 8th Edition Manual (except for code
88). The new categories will be used for cases diagnosed in 2018 and later.
Coding Instructions:
• The post therapy M category staging data item must be assigned for Class of Case 10-22.
• Assign post therapy M category as documented by the treating physician(s) or the managing physician
in the medical record.
• If the managing physician has not recorded post therapy M category, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician.
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Refer to the current AJCC Cancer Staging Manual for staging rules.

154
AJCC Post Therapy M, continued
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
Refer to the STORE manual page 225 for the valid list of codes.
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
155
AJCC TNM Post Therapy Path (yp) Stage Group
Data Dictionary Category: Stage of Disease: AJCC 8
th
Edition
PUF Data Item Name: AJCC_TNM_POST_PATH_STG_GRP
NAACCR Item #: 1024
Diagnosis Years Available: 2018 +
Length: 15
Allowable Values: Alphanumeric, blank
Description:
Identifies the anatomic extent of disease based on the T, N, and M category data items of the tumor
known following the completion of neoadjuvant therapy (satisfying the definition for that disease site)
and planned post-neoadjuvant therapy surgical resection.
Rationale:
The CoC requires that AJCC TNM staging be used in its accredited cancer programs. Effective January 1,
2015 the CoC requires that AJCC pathological TNM staging be recorded in its accredited program cancer
registries. The AJCC developed this staging system for evaluating trends in the treatment and control of
cancer. This staging system is used by physicians to estimate prognosis, plan treatment, evaluate new
types of therapy, analyze outcomes, design follow-up strategies, and to assess early detection results.
Coding Instructions:
• Record the post therapy stage group as documented by the treating physician(s) or the managing
physician in the medical record.
• If the managing physician has not recorded the post therapy stage, registrars will assign this item
based on the best available information, without necessarily requiring additional contact with the
physician(s).
• Code 88 for clinical and pathological or post therapy T, N, and M as well as stage group if a
site/histology combination is not defined in the current AJCC edition and for in situ tumors that are not
staged according to the current AJCC edition.
• If the value does not fill all 15 characters, then record the value to the left and leave the remaining
spaces blank.
• Convert all Roman numerals to Arabic numerals and use upper-case (capital letters) only. • Refer to
the current AJCC Cancer Staging Manual for staging rules.
• The valid codes and labels for the AJCC Cancer Staging Manual, Eighth Edition have been expanded
and are now consistent for clarity.
157
Stage of Disease: Collaborative Stage Data
Collection System
158
CS Site-Specific Factors 1-25
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_SITESPECIFIC_FACTOR_1 through CS_SITESPECIFIC_FACTOR_25
NAACCR Item #: 2861- 2880, 2890, 2900, 2910, 2920, 2930
Diagnosis Years Available: Version 1: 2004-2009, Version 2: 2010-2017
Length: 3
Allowable Values: 000 - 999, blank Site-specific (see variable Site Specific Code Definitions for Data
Items from the Collaborative Stage Data Collection System)
Note: These were no longer collected starting in 2018. These were replaced by Site Specific Data Items
(SSDIs) in 2018.
Description:
The CS Site-Specific Factors are part of the Collaborative Stage Data Collection System,
which was implemented in 2004 and expanded in 2010. CS Site-Specific Factors 1-24,
when used for a particular site, contain information that is used to assign AJCC 6th
and/or 7th edition T, N, M and stage group, or prognostic information identified in the
AJCC Cancer Staging Manual, 7th edition. CS Site- Specific Factor 25 is used to
distinguish between or among staging schema when site and histology codes are not
sufficient, for consistency with the AJCC 7
th
edition for the following: Nasopharynx/
Pharyngeal Tonsil; Esophagus GE Junction / Stomach; Bile Ducts Distal / Bile Ducts
Perihilar / Cystic Duct; Peritoneum / Peritoneum Female Genital; Melanoma Ciliary
Body / Melanoma Iris; Lacrimal Gland / Lacrimal Sac.
Registry coding instructions: Instructions are found on the Collaborative Stage website for each
Site Specific Factor. See below for more information.
Analytic Note:
Using the Site Specific Factors (SSF) from the Collaborative Stage Data Collection
System (CS)
PUF projects may examine one or more laboratory prognostic indicators. These are
available as SSF collected as part of the CS. The term “collaborative” means that the
data collection tool was devised to meet the various needs of cancer registry data
standard setters such as the Commission on Cancer (CoC), Surveillance Epidemiology
and End Results (SEER), and the National Program of Cancer Registries (NPCR).
Up to 25 data fields are used to collect SSFs. Being site specific, they contain different
information depending on the type of cancer in the report. For example, for breast
159
CS Site Specific Factors 1-25 continued
cancer reports SSF1 contains “Estrogen Receptor (ER) Assay” results, but for colon
cancer reports SSF1 contains “Carcinoembryonic Antigen (CEA)” results.
SSFs also may convey non-laboratory site specific information that is relevant to
prognosis for some cases. For example, SSF1 for gastric cancers is “Clinical Assessment
of Regional Lymph Nodes”, and for melanoma of skin it is “Measured Thickness
(Depth), Breslow Measurement”.
Some detective work is required to identify the data fields of interest, the applicable
codes, and the adequacy of the data for the particular study.
The codes, and occasionally the fields used, for a particular prognostic factor changed
over time. In the PUF the SSF data are retained in the form in which they were
submitted. That means that it will be necessary to identify the CS Version Numbers that
are used in the PUF file, and use those to identify whether the data contents for the
desired SSF may have changed or moved over time. Links to the site-specific codes can
be found within the variable Site Specific Code Definitions for Data Items from the
Collaborative System.
The quality of the SSF data items has undergone minimal review by NCDB, and PUF
users are advised to examine the data consistency and completeness of these items
carefully before proceeding with the study.
All SSF data items are edited for validity and internal consistency before the case
report is submitted, and the submitter is required to correct any edit errors. However,
some coding errors remain.
Case coverage of the SSFs is limited for a variety of reasons, potentially seriously
affecting their applicability for some studies.
The availability of the measures to hospital registrars at the time of data entry is
sparse for many prognostic measures. The source of information is usually the
laboratory report as it appears in the hospital patient record. The information
may not be available in the hospital if it was requested by a physician and the
report was sent to the physician’s office. Or it may be delayed and not picked up
later.
The individual tests are not run at all locations or for all patients, even if the test
is part of an acknowledged treatment protocol.
Finally, many hospital registries began abstracting data for the years the
measures were introduced prior to the hospital’s upgrade of the software
necessary to collect those items, and they did not necessarily return to the cases
to abstract the missed data.
160
CS Site Specific Factors 1-25 continued
Some SSFs were first introduced in 2004, and are underrepresented for cases
diagnosed that year compared to later years. Most prognostic SSFs were
introduced in 2010, and are certainly underrepresented for 2010 diagnoses;
they are not available at all for earlier years.
The SSFs in use in for Versions 2.02 through 2.05, and whether the field was required
for CoC registries are described in http://seer.cancer.gov/csreqstatus/index.html. To
access the list of Site-Specific Factors required by the Commission on Cancer, click the
Get Started button in the Collaborative Stage Requirements Status box on the right-
hand side of the page. Then, press the plus sign in the middle of the page, select
Required Factors as Report, CoC as the Standard Setter, and the applicable version
under Version. As noted above, the fields in which these items were stored and the
codes used may have changed over time.

161
CS Version Derived
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: C S_VERSION_LATEST
NAACCR Item #: 2936
Diagnosis Years Available: 2004 - 2015
Length: 6
Allowable Values: 000900 - 020599, blank
Description: This is the version number of the most recent derivation of CS data items in the record.
Registry coding instructions: None.
Analytic Note: This item is a 6-digit code. The first two digits represent the major version number;
the second two digits represent minor version changes; and the last two digits represent even less
significant changes (from correction of spelling errors to tracking of conversion processes). Use the
codes listed above to interpret contents of CS Site-
S
pecific items. See data item Site Specific Code
Definitions for Data Items from the Collaborative Stage Data Collection System for the links to respective
site
-sp
ecific schema. As of 2016, this item was no longer required.
The following are the allowable codes (XX stands for "any two digits"):
Code
Definition
CS Version
0009XX
This was a trial version, consider the same as 0101XX
CSv01
0101XX
CSv01
0102XX
CSv01
0103XX
CSv01
0104XX
CSv01
0200XX
CSv02
0201XX
CSv02
0202XX
CSv02
0203XX
CSv02
0204XX
CSv02
0205XX
CSv02

162
Site Specific Code Definitions for Data Items from the Collaborative
Stage Data Collection System
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: Not applicable
NAACCR Item #: Not Applicable
Diagnosis Years Available: Version 1: 2004-2009, Version 2: 2010:2017
Length: Varies
Allowable Values: Varies
Description:
The most recent version of CS is located at
https://www.facs.org/quality-
programs/cancer/ajcc/cs-schema. You may search the primary site by natural order or
alphabetically. Select the primary site of interest and the CS variables for the primary
site will appear. To see the associated codes with each variable, click on the variable
name.
Registry coding instructions: See CS manuals referenced below
Analytic note: None
163
CS Extension
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: C S_EXTENSION
NAACCR Item #: 2810
Diagnosis Years Available: 2004 - 2015
Length: 3
Allowable Values: 00 - 80, 95, 99 Site-specific (see variable Site-Specific Code Definitions for data items
from the Collaborative Stage Data Collection System)
Description:
Identifies contiguous growth (extension) of the primary tumor within the organ or origin
or its direct extension into neighboring organs. For some sites such as ovary,
discontinuous metastasis is coded in CS Extension (NAACCR Item # 2810).
Registry coding instructions:
None.
Analytic Note:
CS Extension (NAACCR Item #2810) is used to derive some AJCC T-values and some SEER
Summary Stage codes. This item was discontinued in 2016.
Some detective work is required to interpret codes in the CS Extension (NAACCR Item
#2810) field. The codes differ by type of cancer and by the version of CS in which the
case was coded. In the PUF, CS fields are retained in the form in which they were
submitted. That means that it will be necessary to identify the CS Version Derived
(NAACCR Item #2936) that are used in the PUF file, and use those to identify whether
the contents of the CS Extension (NAACCR Item #2810) field may have changed over
time. Links to the site specific codes can be found within the variable Site Specific
Code Definitions for Data Items from the Collaborative Stage Data Collection System.
164
CS Tumor Size/Ext Eval
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_TUMOR_SIZEEXT_EVAL
NAACCR Item #: 2820
Diagnosis Years Available: 2004 - 2015
Length: 1
Allowable Values: 0 - 3, 5, 6, 8, 9, blank Site-specific (see variable Site Specific Code Definitions for Data
Items from the Collaborative Stage Data Collection System)
Description:
Records how the codes for the two items, CS Tumor Size (NAACCR Item #2800) and CS
Extension (NAACCR Item #2810) were determined, based on the diagnostic methods
employed.
Registry coding instructions: See CS manual
Analytic Note:
CS Tumor Size/Ext Eval (NAACCR Item #2820) is used to describe whether the staging
basis for the AJCC T value is clinical or pathologic to record whether systemic
treatment was performed prior to assignment of either CS Tumor Size (NAACCR Item
#2800) or CS Extension (NAACCR Item #2810) codes. This item was discontinued in 2016.
Some detective work is required to interpret codes in the CS Tumor Size/Ext (NAACCR
Item #2820) field. The codes differ by type of cancer and occasionally by the version of
CS in which the case was coded. In the PUF, CS fields are retained in the form in which
they were submitted. That means that it will be necessary to identify the CS Version
Derived (NAACCR Item #2936) that are used in the PUF file, and to use those to identify
whether the contents of the CS Tumor Size/Ext Eval (NAACCR Item #2820) fields may
have changed over time. Links to the site-specific codes can be found within the
variable Site Specific Code Definitions for Data Items from the Collaborative Stage Data
Collection System.
165
Lymph-Vascular Invasion
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: LYMPH_VASCULAR_INVASION
NAACCR Item #: 1182
Diagnosis Years Available: 2010 +
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
Indicates the presence or absence of tumor cells in lymphatic channels (not lymph
nodes) or blood vessels within the primary tumor as noted microscopically by the
pathologist.
This data item is separate from the CS data items but is included in this manual because
of its relationship to the Collaborative Stage Data Collection System. Lymph-vascular
invasion is an item of interest to both pathologists and clinicians and is mentioned in
many chapters of the AJCC Cancer Staging Manual, seventh edition. This field is required
for mapping of T in some sites, such as testis and penis.
Registry Coding Instructions:
Code from pathology report(s). Code the absence or presence of lymph-vascular
invasion as described in the medical record.
The primary sources of information about lymph-vascular invasion are the
pathology check lists (synoptic reports) developed by the College of American
Pathologists. If the case does not have a checklist or synoptic report, code
from the pathology report or a physician’s statement, in that order.
Do not code perineural invasion in this field.
Information to code this field can be taken from any specimen from the
primary tumor.
If lymph-vascular invasion is identified anywhere in the resected specimen, it
should be coded as present/identified.

166
Lymph Vascular Invasion continued
Use of codes.
Use code 0 when the pathology report indicates that there is no lymph-vascular
invasion. This includes cases of purely in situ carcinoma, which biologically
have no access to lymphatic or vascular channels below the basement
membrane.
Use code 1 when the pathology report or a physician’s statement indicates that
lymph-vascular invasion (or one of its synonyms) is present in the specimen.
Use code 8 for the following primary sites: Hodgkin and Non-Hodgkin
lymphoma, Leukemias, Hematopoietic and reticuloendothelial disorders,
Myelodysplastic syndromes including refractory anemias and refractory
cytopenias, Myeloproliferative disorders.
Use code 9 when:
There is no microscopic examination of a primary tissue specimen.
The primary site specimen is cytology only or a fine needle aspiration.
The biopsy is only a very small tissue sample.
It is not possible to determine whether lymph-vascular invasion is
present.
The pathologist indicates the specimen is insufficient to determine
lymph- vascular invasion.
Lymph-vascular invasion is not mentioned in the pathology report.
Analytic Note: This data item was not collected for cases diagnosed prior to 2010. Due to delays in
some hospitals for implementing registry data updates, it may be incomplete for 2010 cases.
Code
Definition
0
Lymph-vascular invasion is not present (absent) or not
identified
1
Lymph-vascular invasion is present or identified
8
Not applicable
9
Unknown if lymph-vascular invasion is present, or
indeterminate
blank
Not available
167
CS Mets at DX
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_METS_AT_DX
NAACCR Item #: 2850
Diagnosis Years Available: 2004 - 2015
Length: 2
Allowable Values: Site-specific (see variable Site Specific Code Definitions for Data Items from the
Collaborative Stage Data Collection System)
Description:
Identifies whether there is metastatic involvement of distant site(s) at the time of
diagnosis.
Registry coding instructions: None.
Analytic Note:
CS Mets at DX (NAACCR Item #2850) is used to derive some AJCC M values and SEER
Summary Stage codes. This item was discontinued in 2016.
Some detective work is required to interpret codes in the CS Mets at DX (NAACCR Item
#2850) field. The codes differ by type of cancer and by the version of CS in which the
case was coded. In the PUF, CS fields are retained in the form in which they were
submitted. That means that it will be necessary to identify the CS Version Derived
(NAACCR Item #2936) that are used in the PUF file, and use those to identify whether
the contents of the CS Mets at DX (NAACCR Item #2850) filed may have changed over
time. Links to the site-specific codes can be found within the variable Site Specific
Code Definitions for Data Items from the Collaborative Stage Data Collection System.
168
CS Mets at DX-Bone
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_METS_DX_BONE
Diagnosis Years Available: 2010 - 2015
NAACCR Item #: 2851
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
Identifies the presence of distant metastatic involvement of bone at the time of
diagnosis.
Registry Coding Instructions:
Code information about bone metastases only (discontinuous or distant metastases to
bone) identified at the time of diagnosis. This field should not be coded for bone
marrow involvement. Bone involvement may be single or multiple. Information about
bone involvement may be clinical or pathologic.
Code this field whether or not the patient had any preoperative systemic therapy. This
field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site, and
Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, reticuloendothelial, Immunopolifereative and
Myeloproliferative Neoplasms, and Hodgkin’s and non-Hodgkin’s Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the patient
specifically had bone metastases; for example, when CS Mets at DX (NAACCR Item
#2850) is coded as carcinomatosis but bone is not specifically mentioned as a metastatic
site. Also use code 9 when it is not known whether the patient had any distant
metastases.
Analytic Note:
This item was first collected in 2010. Because of delays in some hospitals in
implementing registry software updates, data may be incomplete for 2010 diagnoses.
This item was discontinued in 2016, and replaced by the FORDS manual variable, Mets
at Diagnosis – Bone (NAACCR Item #1112). Links to the site-specific codes can be found
within the variable Site Specific Code Definitions for Data Items from the Collaborative
Stage Data Collection System.

169
CS Mets at Dx- Bone continued
Code
Definition
0
None; no bone metastases
1
Yes
8
Not applicable
9
Unknown whether bone is involved metastatic site; Not documented
in patient record
blank
Not available
170
CS Mets at DX-Liver
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_METS_DX_LIVER
NAACCR Item #: 2853
Diagnosis Years Available: 2010 - 2015
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
Identifies the presence of distant metastatic involvement of the liver at the time of
diagnosis.
Registry Coding Instructions:
Code information about liver metastases only (discontinuous or distant metastases to
the liver) identified at the time of diagnosis.
Liver involvement may be single or multiple. Information about liver involvement may
be clinical or pathologic. Code this field whether or not the patient had any
preoperative systemic therapy.
This field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site,
and Other and Ill-Defined Sites.
Use code 8 for Hematopoietic, Reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin and non-Hodgkin Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient had liver metastases; for example, when CS Mets at DX (NAACCR Item #2850) is
coded as carcinomatosis but the liver is not specifically mentioned as a metastatic site.
Also use code 9 when it is not known whether the patient had any distant metastases.
Analytic Note:
This item was first collected in 2010. Because of delays in some hospitals in
implementing registry software updates, data may be incomplete for 2010 diagnoses.
This item was discontinued in 2016 and replaced by the FORDS manual variable Mets
at Diagnosis – Liver (NAACCR Item #1115). Links to the site-specific codes can be found
within the variable Site Specific Code Definitions for Data Items from the Collaborative
Stage Data Collection System.

171
CS Mets at Dx-Liver continued
Code
Definition
0
None; no liver metastases
1
Yes
8
Not applicable
9
Unknown whether bone is involved metastatic site; Not documented
in patient record
blank
Not available
172
CS Mets at DX-Lung
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_METS_DX_LUNG
NAACCR Item #: 2854
Diagnosis Years Available: 2010 - 2015
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
Identifies the presence of distant metastatic involvement of the lung at the time of
diagnosis.
Registry Coding Instructions:
Code information about lung metastases only (discontinuous or distant metastases to
the lung) identified at the time of diagnosis. This field should not be coded for pleural
or pleural fluid involvement.
Lung involvement may be single or multiple. Information about lung involvement may
be clinical or pathologic. Code this field whether or not the patient had any
preoperative systemic therapy.
This field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site,
and Other and Ill-Defined Primary Sites.
Use code 8 for Hematopoietic, Reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin and non-Hodgkin Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had lung metastases; for example, when CS Mets at Dx (NAACCR
Item #2850) is coded as carcinomatosis but the lung is not specifically mentioned as a
metastatic site.
Also use code 9 when it is not known whether the patient had any distant metastases.
Analytic Note:
This item was first collected in 2010. Because of delays in some hospitals in
implementing registry software updates, data may be incomplete for 2010. This item
was discontinued in 2016 and replaced by the FORDS manual variable Mets at
Diagnosis – Lung (NAACCR Item #1116). Links to the site-specific codes can be found
within the variable Site Specific Code Definitions for Data Items from the Collaborative
Stage Data Collection System.

173
CS Mets at Dx-Lung continued
Code
Definition
0
None; no lung metastases
1
Yes
8
Not applicable
9
Unknown whether bone is involved metastatic site; Not documented
in patient record
blank
Not available
174
CS Mets at DX-Brain
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: CS_METS_DX_BRAIN
NAACCR Item #: 2852
Diagnosis Years Available: 2010 - 2015
Length: 1
Allowable Values: 0, 1, 8, 9, blank
Description:
Identifies the presence of distant metastatic involvement of the brain at the time of
diagnosis.
Registry Coding Instructions:
Code information about brain metastases only (discontinuous or distant metastases to
brain) known at the time of diagnosis. This field should not be coded for involvement
of the spinal cord or other parts of the central nervous system.
Brain involvement may be single or multiple. Information about brain involvement may
be clinical or pathologic. Code this field whether or not the patient had any
preoperative systemic therapy.
This field should be coded for all solid tumors, Kaposi sarcoma, Unknown Primary Site,
and Other and Ill-Defined Primary Sites.
Use code 8 for Hematopoietic, Reticuloendothelial, Immunoproliferative and
Myeloproliferative Neoplasms, and Hodgkin and non-Hodgkin Lymphoma.
Use code 9 when it cannot be determined from the medical record whether the
patient specifically had brain metastases; for example, when CS Mets at DX (NAACCR
Item #2850) is coded as carcinomatosis but the brain is not specifically mentioned as a
metastatic site. Also use code 9 when it is not known whether the patient had any
distant metastases.
Analytic Note:
This item was first collected in 2010. Because of delays in some hospitals in
implementing registry software updates, data may be incomplete for 2010 diagnoses.
This item was discontinued in 2016. It was replaced by the FORDS manual variable Mets
at Diagnosis – Brain (NAACCR Item #1113) in 2016.
Links to the site-specific codes can be found within the variable Site Specific Code
Definitions for Data Items from the Collaborative Stage Data Collection System.

175
CX Mets at Dx-Brain continued
Code
Definition
0
None; no brain metastases
1
Yes
8
Not applicable
9
Unknown whether bone is involved metastatic site; Not documented
in patient record
blank
Not available
176
CS Mets Eval
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: C S_METS_EVAL
NAACCR Item #: 2860
Diagnosis Years Available: 2004 - 2015
Length: 1
Allowable Values: 0 - 3, 5, 6, 8, 9, blank Site-specific (see variable Site Specific Code Definitions for Data
Items from the Collaborative Stage Data Collection System)
Description:
Records how the code for CS Mets at DX (NAACCR Item #2850) was determined based
on the diagnostic methods employed.
Registry coding instructions:
None.
Analytic Note:
CS Mets Eval (NAACCR Item #2860) describes whether the staging basis for CS Mets at
DX (NAACCR Item #2850) was clinical or pathologic, and whether any systemic
treatment was given prior to that code assignment. This item was discontinued in 2016.
Some detective work is required to interpret codes in CS Mets Eval (NAACCR Item
#2860). The codes may differ by type of cancer and by the version of CS in which the
case was coded. In the PUF, CS fields are retained in the form in which they are
submitted.
That means that it will be necessary to identify the CS Version Derived (NAACCR Item #
2936) that are used in the PUF file, and use those to identify whether the contents of
the CS Mets Eval (NAACCR Item #2860) field may have changed over time. Links to the
site-specific codes can be found within the variable Site Specific Code Definitions for
Data Items from the Collaborative Stage Data Collection System.

177
CS Tumor Size
Data Dictionary Category: Stage of Disease Collaborative Stage Data Collection System
PUF Data Item Name: TUMOR_SIZE
NAACCR Item #: 2800
Length: 3
Diagnosis Years Available: 2004 - 2015
Allowable Values: 000 - 999
Description:
Describes the largest dimension of the diameter of the primary tumor in millimeters
(mm).
Registry Coding Instructions:
Refer to the site and histology-specific instructions in the current CS manual for coding
instructions at: https://www.facs.org/quality-programs/cancer/ajcc/cs-schema
CoC
does not require that registrars report information for this item that is not readily
available in the facility's records. However, if that information is obtained along with
other material from another source, it may be used.
Analytic Note:
This field is blank in the melanoma PUF. Use CS Site-Specific Factor 1 (NAACCR Item
#2880) to obtain Breslow’s depth. CS Tumor Size (NAACCR Item #2800) is part of the
Collaborative Stage Data Collection System (CS), and was implemented in 2004 through
2015. This item was discontinued in 2016 and replaced by a new Tumor Size Summary
(NAACCR Item #756) variable. It is used to describe tumor size at diagnosis as an
independent prognostic indicator for many tumors and it is used by Collaborative Stage
to derive some TNM-T codes.
Links to the site-specific codes can be found within the variable Site Specific Code
Definitions for Data Items from the Collaborative Stage Data Collection System.
178
Site Specific Data Items (SSDIs)

179
Site Specific Data Items (SSDIs)
Data Dictionary Category: Site Specific Data Items (SSDIs)
PUF Data Item Names: Various
NAACRR Item Number: Various
Length: Various
Diagnosis Years Available: 2018 +
Allowable Values: Various
Description:
In 2018, Site Specific Data Items replaced the Site Specific Factors. What is a SSDI? A “SSDI’” is a site-
specific data item. “Site” in this instance is based on the primary site, the AJCC chapter, Summary Stage
chapter and the EOD schema. SSDIs were preceded by Collaborative Stage Site Specific Factors (CS SSFs),
which were first introduced in 2004 with CSv1, and went through major revisions in 2010 with
Collaborative Stage v2 (CSv2). CS SSFs were discontinued as of 12/31/2017. SSDIs have their own data
item name and number and can be collected for as many sites/chapters/schemas as needed. Each Site-
Specific Data Item (SSDI) applies only to selected schemas. SSDI fields should be blank for schemas for
which they do not apply.
Number of SSDIs compared to CS SSFs
Approximately 260 unique CS SSFs in CSv0205
• 101 discontinued
• 12 obsolete
• 147 required
• Of these, 27 are not required for 1/1/2018+
• 120 SSDIs added to the NAACCR v18 layout. CS SSF data will be retained for cases diagnosed 2004-
2017.
The SSDI manuals which include descriptions and definitions of each SSDI are found on the NAACCR
Website at: https://apps.naaccr.org/ssdi/list/
See also the STORE manual pages 7-8 for a description of the SSDIs at:
https://www.facs.org/~/media/files/quality%20programs/cancer/ncdb/store_manual_2018.ashx
180
Treatment

181
RX Summ Treatment Status
Data Dictionary Category: Treatment
PUF Data Item Name: RX_SUMM_TREATMENT_STATUS
NAACCR Item #: 1285
Diagnosis Years Available: 2010 +
Length: 1
Allowable Values: 0 - 2, 9, blank
Description:
This item summarizes whether the patient received any treatment or was under active
surveillance.
Registry Coding Instructions:
Treatment after a period of active surveillance is considered subsequent treatment
and is not coded in this item.
Use code 0 when treatment is refused or the physician decides not to treat for any
reason such as the presence of comorbidities.
Analytic Note:
This item is only reported for diagnosis years 2010 and later.
Code
Definition
0
No treatment given
1
Treatment given
2
Active surveillance (watchful waiting)
9
Unknown if treatment given
blank
Not available

182
Treatment Started, Days from Dx
Data Dictionary Category: Treatment
PUF Data Item Name: DX_RX_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and
the Date of First Course of Treatment [surgery, radiation, systemic, or other therapy]
(NAACCR Item #1270) of the patient began at any facility.
Registry coding instructions:
None.
Analytic note:
The elapsed time from diagnosis to date of first treatment will be zero for some cases
due to the surgery codes consisting of a mix of both diagnostic and surgical procedures.
Registrars must interpret ambiguous terms according to registry rules, and this may
keep them from recording an imaging or physical exam date as the date of diagnosis.
Because either a diagnostic or surgical procedure will trigger a set date of first course
treatment, there is no correction that can be done. We recognize this flaw and there are
ongoing discussions to revise the coding instructions. You may elect to use the NCCN
treatment guidelines to determine which procedures listed in the FORDS surgery codes
are curative and use the Days from Diagnosis to the earliest curative treatment as the
number of days from diagnosis to First Treatment.
Code
Definition
0000 - 9999
Number of elapsed days.
blank
No first course therapy administered, first course therapy
unknown, or cannot compute days elapsed due to missing or
incomplete dates
183
Treatment: Surgery

184
First Surgical Procedure, Days from Dx
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: DX_SURG_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date of First Surgical Procedure (NAACCR Item #1200). The surgery may be Surgical
Procedure of Primary Site (NAACCR Item #1290), Scope of Regional Lymph Node
Surgery (NAACCR Item #1292) or Surgical Procedure/Other Site (NAACCR Item #1294).
Incisional biopsies are not coded as treatment surgery.
Registry Coding Instructions: Not applicable.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Surgical treatment may have occurred at any facility, or at multiple facilities,
not limited to the one whose report is included in this file. This refers to the first
surgical procedure for the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
No first course surgery, first course surgery unknown, or cannot
compute days elapsed due to missing or incomplete dates

185
Definitive Surgical Procedure, Days from Dx
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: DX_DEFSURG_STARTED_DAYS
NAACCR Item #: Not Available
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date of Most Definitive Surgical Resection of the Primary Site (NAACCR Item #3170).
Registry Coding Instructions:
None.
Analytic Note:
The Date of the Most Definitive Surgical Resection of the Primary Site (NAACCR Item
#3170) refers to the last date that first course surgery of the primary site was
performed for the patient. For example, a breast cancer patient may have been
treated with an excisional biopsy, followed by a lumpectomy, followed by a
mastectomy. This item identifies the time period between the Date of Initial Diagnosis
(NAACCR Item #390) and the date of the mastectomy (Date of the Most Definitive
Surgical Resection of the Primary Site NAACCR Item #3170). The Surgical Procedure of
Primary Site (NAACCR Item #1290) will record the mastectomy.
CoC cancer programs are required to identify treatment their patients received from
all sources. Surgical treatment may have occurred at any facility, or at multiple
facilities, not limited to the one whose report is included in this file. This refers to the
final surgery of the primary site, cumulative for all procedures, for the cancer by any
facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
No first course surgery, surgery unknown, or cannot compute days
elapsed due to incomplete or missing dates
186
Surgical Procedure of Primary Site
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_SUMM_SURG_PRIM_SITE
NAACCR Item #: 1290
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 10 - 80, 90, 98, 99
Description:
Records the surgical procedure performed to the primary site at any facility.
Registry Coding Instructions:
Site-specific codes for this data item are found in Appendix A: Site-Specific Surgery
Codes.
If registry software allows only one procedure to be collected, document the most
invasive surgical procedure for the primary site.
If registry software allows multiple procedures to be recorded, this item refers to the
most invasive surgical procedure of the primary site.
For codes 00 through 79, the response positions are hierarchical by position (not
necessarily numerically). Last-listed responses take precedence over responses written
above. Code 98 takes precedence over code 00. Use codes 80 and 90 only if more
precise information about the surgery is not available.
Biopsies that remove all of the tumor and/or leave only microscopic margins are to be
coded in this item.
Surgery to remove regional tissue or organs is coded in this item only if the
tissue/organs are removed in continuity with the primary site, except where noted in
where noted in Appendix A: Site-Specific Surgery Codes.
If a previous surgical procedure to remove a portion of the primary site is followed by
surgery to remove the remainder of the primary site, then code the total or final
results.
If the procedure coded in this item was provided to prolong a patient’s life by
controlling symptoms, to alleviate pain, or to make the patient more comfortable, then
also record this surgery in the item Palliative Care (NAACCR Item #3270).

187
Surgical Procedure of the Primary Site continued
Analytic Note:
If multiple first course surgeries are performed on the primary site, the code represents
the cumulative effect of all primary site surgeries. For example, if a breast cancer patient
is treated with an excisional biopsy, then a lumpectomy, then a mastectomy, the
mastectomy is coded in this field. The date of the mastectomy is represented in Date of
the Most Definitive Surgical Resection of the Primary Site (NAACCR Item #3170).
CoC cancer programs are required to identify treatment their patients received from all
sources. Surgical treatment may have occurred at any facility, or at multiple facilities, not
limited to the one whose report is included in this file. This refers to the final surgery of
the primary site, cumulative for all procedures, for the cancer by any facility.
Descriptions of surgical codes have been revised over time. Please refer to the versions
of FORDS corresponding to the diagnosis years covered in your analyses to find out
whether any changes have occurred in your primary site(s) of interest in your study. All
versions of FORDS may be accessed via the following:
https://www.facs.org/quality-programs/cancer/ncdb/call-for-data/fordsolder.
The site-specific surgical codes may also be found in the Surgical Procedure of Primary
Site (NAACCR Item #1290) codes in Appendix A: Site-Specific Surgery Codes of this
document.
Code
Definition
Description
00
None
No surgical procedure of primary site
10-19
Site-specific
codes; tumor
destruction
Tumor destruction, no pathologic specimen produced. Refer
to Appendix A: Site-Specific Surgery Codes for the correct
site-specific code for the procedure
20-80
Site-specific
codes; resection
Refer to Appendix A: Site-Specific Surgery Codes for the
correct site-specific code for the procedure
90 Surgery, NOS
A surgical procedure to the primary site was done, but no
information on the type of surgical procedure is provided
98
Site-specific
codes; special
Special code. Refer to Appendix A: Site-Specific Surgery
Codes for the correct site-specific code for the procedure
99 Unknown
Patient record does not state whether a surgical procedure of
the primary site was performed and no information is
available
188
Surgical Procedure of Primary Site at This Facility
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_HOSP_SURG_PRIM_SITE
NAACCR Item #: 670
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 10 - 80, 90, 98, 99
Description:
This item records the surgical procedure performed to the primary site at the facility
that submitted this record.
Registry Coding Instructions:
Site-specific codes for this data item are found in Appendix A: Site-Specific Surgery
Codes.
If registry software allows only one procedure to be collected, document the most
invasive surgical procedure for the primary site.
If registry software allows multiple procedures to be recorded, this item refers to the
most invasive surgical procedure of the primary site.
For codes 00 through 79, the response positions are hierarchical by position (not
necessarily numerically). Last-listed responses take precedence over responses written
above. Code 98 takes precedence over code 00. Use codes 80 and 90 only if more
precise information about the surgery is not available.
Biopsies that remove all of the tumor and/or leave only microscopic margins are to be
coded in this item.
Surgery to remove regional tissue or organs is coded in this item only if the
tissue/organs are removed in continuity with the primary site, except where noted in
Appendix A: Site-Specific Surgery Codes.
If a previous surgical procedure to remove a portion of the primary site is followed by
surgery to remove the remainder of the primary site, then code the total or final
results.

189
Surgical Procedure of the Primary Site at this Facility-continued
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all
sources. Surgical treatment may have occurred at any facility, or at multiple facilities,
not limited to the one whose report is included in this file. This refers to the final
surgery of the primary site, cumulative for all procedures, for the cancer by the
reporting facility. Additional surgery, or prior surgery, may have been performed
elsewhere. The item Surgical Procedure of Primary Site (NAACCR Item #1290) describes
the cumulative primary site surgery performed on the patient at any facility.
The site-specific surgical codes may be found in Appendix A: Site-Specific Surgery Codes.
Code
Definition
Description
00 None No surgical procedure of primary site
10-19
Site-specific
codes; Tumor
destruction
Tumor destruction; no pathologic specimen produced.
Refer to Appendix A: Site-Specific Surgery Codes for the
correct site-specific code for the procedure
20-80
Site-specific
codes; Resection
Refer to Appendix A: Site-Specific Surgery Codes for the
correct site-specific code for the procedure
90 Surgery, NOS
A surgical procedure to the primary site was done, but
no information on the type of surgical procedure is
provided
98
Site specific
codes; special
Special code. Refer to Appendix A: Site-Specific Surgery
Codes for the correct site-specific code for the
procedure
99 Unknown
Patient record does not state whether a surgical
procedure of the primary site was performed and no
information is available

190
Approach – Surgery of the Primary Site at this Facility
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_HOSP_SURG_APPR_2010
NAACCR Item #: 668
Diagnosis Years Available: 2010 +
Length: 1
Allowable Values: 0 - 5, 9, blank
Description: This item is used to monitor patterns and trends in the adoption and utilization of
minimally-invasive surgical techniques.
Registry Coding Instructions:
This item may be left blank for cases diagnosed prior to 2010.
If the patient has multiple surgeries of the primary site, this item describes the
approach used for the most invasive, definitive surgery.
For ablation of skin tumors, assign code 3.
Assign code 2 or 4 if the surgery began as robotic assisted or endoscopic and was
converted to open.
If both robotic and endoscopic or laparoscopic surgery are used, code to robotic
(codes 1 or 2).
Analytic Note: This item was first used for 2010 diagnoses.
Code
Definition
0
No surgical procedure of primary site at this facility
1
Robotic assisted
2
Robotic converted to open
3
Minimally invasive (such as endoscopic or laparoscopic)
4
Minimally invasive (endoscopic or laparoscopic)
converted to open
5
Open or approach unspecified
9
Unknown whether surgery was performed at this
facility
blank
Not available
191
Surgical Margins of the Primary Site
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_SUMM_SURGICAL_MARGINS
NAACCR Item #: 1320
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3, 7 - 9
Description:
Records the final status of the surgical margins after resection of the primary tumor
Registry Coding Instructions:
Record the margin status as it appears in the pathology report.
Codes 0-3 are hierarchical; if two codes describe the margin status, use the numerically
higher code.
If no surgery of the primary site was performed, code 8.
For lymphomas with a lymph node primary site (C77.0-C77.9), code 9.
For an unknown or ill-defined primary (C76.0-C76.8, C80.9) or for hematopoietic,
reticuloendothelial, immunoproliferative, or myeloproliferative disease, code 9.
For Brain and CNS sites, the NCDB converts codes 0, 1, 2, 3, and 7 to code 9 for this item
due to unreliability.
Analytic note: None.

192
Surgical Margins of the Primary Site continued
Code
Definition
Description
0
No residual tumor
All margins are grossly and microscopically negative
1
Residual tumor, NOS
Involvement is indicated, but not otherwise specified
2
Microscopic residual tumor
Cannot be seen by the naked eye
3
Macroscopic residual tumor
Gross tumor of the primary site which is visible to the naked eye
7
Margins not evaluable
Cannot be assessed (indeterminate)
8
No primary site surgery
No surgical procedure of the primary site
9 Unknown or not applicable
It is unknown whether a surgical procedure to the primary site was
performed; for lymphomas with a lymph node primary site; an
unknown or ill-defined primary; or for hematopoietic,
reticuloendothelial, immunoproliferative, or myeloproliferative disease
193
Scope of Regional Lymph Node Surgery
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_SUMM_SCOPE_REG_LN_SUR
NAACCR Item #: 1292
Diagnosis Years Available: 2004 - 2011
Length: 1
Allowable Values: 0, 1, 9
Description:
Identifies the removal, biopsy, or aspiration of regional lymph node(s) at the time of
surgery of the primary site or during a separate surgical event.
Registry Coding Instructions:
The scope of regional lymph node surgery is collected for each surgical event even if
surgery of the primary site was not performed.
Record surgical procedures which aspirate, biopsy, or remove regional lymph nodes in
an effort to diagnose or stage disease in this data item.
Record the date of this surgical procedure in data item Date of First Course of Treatment
(NAACCR Item #1270) and/or Date of First Surgical Procedure (NAACCR Item #1200) as
appropriate.
For primaries of the meninges, brain, spinal cord, cranial nerves, and other parts of the
central nervous system (C70.0-C70.9, C71.0-C71.9, C72.0-C72.9), code 9.
For lymphomas with a lymph node primary site (C77.0-C77.9), code 9.
For an unknown or ill-defined primary (C76.0-C76.8, C80.9) or for hematopoietic,
reticuloendothelial, immunoproliferative, or myeloproliferative disease regardless of site,
code 9.
Do not code distant lymph nodes removed during surgery to the primary site for this
data item. Distant nodes are coded in the data field Surgical Procedure/Other Site
(NAACCR Item #1294).
Refer to the applicable AJCC Cancer Staging Manual for site-specific identification of
regional lymph nodes.
If the procedure coded in this item was provided to prolong a patient’s life by controlling
symptoms, to alleviate pain, or to make the patient more comfortable, then also record
this surgery in the item Palliative Care (NAACCR Item #3270).
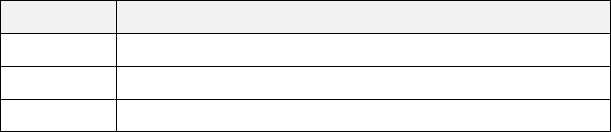
194
Scope of Regional Lymph Node Surgery continued
Analytic note: None.
Code
Definition
0
No regional lymph node surgery
1
Regional lymph node surgery
9
Unknown if there was any regional lymph node surgery
195
Scope of Regional Lymph Node Surgery 2012
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_SUMM_SCOPE_REG_LN_2012
NAACCR Item #: 1292
Diagnosis Years Available: 2012 +
Length: 1
Allowable Values: 0 - 7, 9, blank
Description:
The revised Scope of Regional Lymph Node Surgery 2012 (NAACCR Item #1292) field is
for cases diagnosed on and after January 1, 2012. Scope of Regional Lymph Node
Surgery (NAACCR Item #1292) was found to under-report Sentinel Lymph Node Biopsy
(SLNBx) procedures, either alone or with Axillary Dissection (ALND). Reviews by the
Commission on Cancer (CoC), the Centers for Disease Control and Prevention’s National
Program of Cancer Registries (CDC/NPCR), and the National Cancer Institute’s
Surveillance, Epidemiology, and End Results (SEER) Program confirmed miscoding of this
data element. Revised coding rules and associated instructions have been developed
that put emphasis on securing information from the operative report in contrast to the
pathology report. CoC use of the item Scope of Regional Lymph Node Surgery (NAACCR
Item #1292) remains curtailed in all pre-2012 data years contained in the PUF. The item
is used only to identify whether or not a patient underwent regional lymph node
surgery, effectively removing any distinction between the type or extent of surgical
intervention.
Note that this item is primarily of interest for researchers who received Breast and
Melanoma PUF files.
Registry coding instructions: None.
Analytic note: None.

196
Scope of the Regional Lymph Node Surgery 2012 continued
Code Label
General Instructions Applying to All
Sites
Additional Notes to Breast (C50.X)
Use the operative report as the primary
source document to determine whether
the operative procedure was a sentinel
lymph node biopsy (SLNBx), or a more
extensive dissection of regional lymph
nodes, or a combination of both SLNBx
and regional lymph node dissection. The
operative report will designate the
surgeon's planned procedure as well as a
description of the procedure that was
actually performed. The pathology report
may be used to complement the
information appearing in the operative
report, but the operative report takes
precedence when attempting to
distinguish between SLNBx and regional
lymph node dissection or a combination
of these two procedures. Do not use the
number of lymph nodes removed and
pathologically examined as the sole
means of distinguishing between a SLNBx
and a regional lymph node dissection
Use the operative report as the
primary source document to
determine whether the operative
procedure was a sentinel lymph node
biopsy (SLNBx), an axillary node
dissection (ALND), or a combination
of both SLNBx and ALND. The
operative report will designate the
surgeon's planned procedure as well
as a description of the procedure that
was actually performed. The
pathology report may be used to
complement the information
appearing in the operative report, but
the operative report takes
precedence when attempting to
distinguish between SLNBx and ALND,
or a combination of these two
procedures. Do not use the number
of lymph nodes removed and
pathologically examined as the sole
means of distinguishing between a
SLNBx and a ALND
0
No Regional Lymph
Node Surgery
1
Biopsy or aspiration
of regional lymph
node(s)
Review the operative report to confirm
whether an excisional biopsy or
aspiration of regional lymph nodes was
actually performed. If additional
procedures were performed on the
lymph nodes, use the appropriate code
2-7
Excisional biopsy or aspiration of
regional lymph nodes for breast
cancer is uncommon. Review the
operative report of to confirm
whether an excisional biopsy or
aspiration of regional lymph nodes
was actually performed; it is highly
possible that the procedure is a SLNBx
(code 2) instead. If additional
procedures were performed on the
lymph nodes, such as axillary lymph
node dissection, use the appropriate
code 2-7

197
Scope of the Regional Lymph Node Surgery continued
2
Sentinel Lymph
Node Biopsy
The operative report states that a SLNBx
was performed
Code 2 SLNBx when the operative report
describes a procedure using injection of a
dye, radio label, or combination to
identify a lymph node (possibly more
than one) for removal/examination
When a SLNBx is performed, additional
non-sentinel nodes can be taken during
the same operative procedure. These
additional non-sentinel nodes may be
discovered by the pathologist or
selectively removed (or harvested) as
part of the SLNBx procedure by the
surgeon. Code this as a SLNBx (code 2). If
review of the operative report confirms
that a regional lymph node dissection
followed the SLNBx, code these cases as
6.
If a relatively large number of lymph
nodes, more than 5, are
pathologically examined, review the
operative report to confirm the
procedure was limited to a SLNBx and
did not include an axillary lymph node
dissection (ALND)
Infrequently, a SLNBx is attempted
and the patient fails to map (i.e. no
sentinel lymph nodes are identified by
the dye and/or radio label injection)
and no sentinel nodes are removed.
Review the operative report to
confirm that an axillary incision was
made and a node exploration was
conducted. Patients undergoing
SLNBx who fail to map will often
undergo ALND. Code these cases as 2
if no ALND was performed, or 6 when
ALND was performed during the same
operative event. Enter the
appropriate number of nodes
examined and positive in the data
items Regional Lymph Nodes
Examined (NAACCR Item #830) and
Regional Lymph Nodes Positive
(NAACCR Item #820).

198
Scope of the Regional Lymph Node Surgery 2012 continued
3
Number of regional
lymph nodes
removed unknown
or not stated;
regional lymph
nodes removed,
NOS
The operative report states that a
regional lymph node dissection was
performed (a SLNBx was not done during
this procedure or in a prior procedure)
Code 3 (Number of regional lymph nodes
removed unknown, not stated; regional
lymph nodes removed, NOS). Check the
operative report to ensure this
procedure is not a SLNBx only (code 2),
or a SLNBx with a regional lymph node
dissection (code 6 or 7)
Code 4 (1-3 regional lymph nodes
removed) should be used infrequently.
Review the operative report to ensure
the procedure was not a SLNBx only
Code 5 (4 or more regional lymph nodes
removed). If a relatively small number of
nodes was examined pathologically,
review the operative report to confirm
the procedure was not a SLNBx only
(code 2). If a relatively large number of
nodes was examined pathologically,
review the operative report to confirm
that there was not a SLNBx in addition to
a more extensive regional lymph node
dissection during the same, or separate,
procedure (code 6 or 7)
Infrequently, a SNLBx is attempted and
the patient fails to map (i.e. no sentinel
lymph nodes are identified by the dye
and/or radio label injection). When
mapping fails, surgeons usually perform a
more extensive dissection of regional
lymph nodes. Code these cases as 2 if no
further dissection of regional lymph
nodes was undertaken, or 6 when
regional lymph nodes were dissected
during the same operative event
Generally, ALND removes at least 7-9
nodes. However, it is possible for
these procedures to remove or
harvest fewer nodes. Review the
operative report to confirm that there
was not a SLNBx in addition to a more
extensive regional lymph node
dissection during the same procedure
(code 6 or 7)
4
1-3 regional lymph
nodes removed
5
4 or more regional
lymph nodes
removed

199
Scope of the Regional Lymph Node Surgery 2012 continued
6
Sentinel node
biopsy and code 3,
4, or 5 at same time,
or timing not stated
SNLBx and regional lymph node
dissection (code 3, 4, or 5) during the
same surgical event, or timing not known
Generally, SLNBx followed by a regional
lymph node completion will yield a
relatively large number of nodes.
However, it is possible for these
procedures to harvest only a few nodes
If relatively few nodes are pathologically
examined, review the operative report to
confirm whether the procedure was
limited to a SLNBx only
Infrequently, a SNLBx is attempted and
the patient fails to map (i.e. no sentinel
lymph nodes are identified by the dye
and/or radio label injection.) When
mapping fails, the surgeon usually
performs a more extensive dissection of
regional lymph nodes. Code these cases
as 6
Generally, SLNBx followed by ALND
will yield a minimum of 7-9 nodes.
However it is possible for these
procedures to harvest fewer (or
more) nodes
If relatively few nodes are
pathologically examined, review the
operative report to confirm whether
the procedure was limited to a SLNBx,
or whether a SLNBx plus an ALND was
performed
7
Sentinel node
biopsy and code 3,
4, or 5 at different
times
SNLBx and regional lymph node
dissection (code 3, 4, or 5) in separate
surgical events.
Generally, SLNBx followed by regional
lymph node completion will yield a
relatively large number of nodes.
However, it is possible for these
procedures to harvest only a few nodes.
If relatively few nodes are pathologically
examined, review the operative report to
confirm whether the procedure was
limited to a SLNBx only
Generally, SLNBx followed by ALND
will yield a minimum of 7-9 nodes.
However, it is possible for these
procedures to harvest fewer (or
more) nodes
If relatively few nodes are
pathologically examined, review the
operative report to confirm whether
the procedure was limited to a SLNBx
only, or whether a SLNBx plus an
ALND was performed

200
Scope of the Regional Lymph Node Surgery 2012 continued
9
Unknown or not
applicable
The status of regional lymph node evaluation should be known for surgically
treated cases (i.e., cases coded 19-90 in the data item Surgical Procedure of
Primary Site (NAACCR Item #1290). Review surgically treated cases coded 9 in
Scope of Regional Lymph Node Surgery (NAACCR Item #1292) to confirm the code.
Examples
Code
Reason
0
No effort was made to locate sentinel lymph nodes, and no nodes were found in pathologic analysis.
2
(C50.1-Breast) There was an attempt at sentinel lymph node dissection, but no lymph nodes were
found in the pathologic specimen.
1
(C14.0-Pharynx) Aspiration of regional lymph node to confirm histology of widely metastatic disease.
2
(C44.5-Skin of Back) Patient has melanoma of the back. A sentinel lymph node dissection was done
with the removal of one lymph node. This node was negative for disease.
3
(C61.9-Prostate) Bilateral pelvic lymph node dissection for prostate cancer.
6
(C50.3-Breast) Sentinel lymph node biopsy (SLNBx) of right axilla, followed by right axillary lymph node
dissection (ALND) during the same surgical event.
7
(C50.4-Breast) Sentinel lymph node biopsy (SLNBx) of left axilla, followed in a second procedure 5 days
later by a left axillary lymph node dissection (ALND).
9
(C34.9-Lung) Patient was admitted for radiation therapy following surgery for lung cancer. There is no
documentation on the extent of the lymph node surgery in patient record.
201
Surgical Procedure Other Site
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: RX_SUMM_SURG_OTH_REGDIS
NAACCR Item #: 1294
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 5, 9
Description:
Records the surgical removal of distant lymph nodes or other tissue(s)/organ(s)
beyond the primary site.
Registry Coding Instructions:
Assign the highest numbered code that describes the surgical resection of distant
lymph
node(s) and/or regional/distant tissue or organs.
Incidental removal of tissue or organs is not recorded as a Surgical
Procedure/Other Site
(NAACCR Item #1294).
Code 1 if any surgery is performed to treat tumors of unknown or ill-defined
primary sites
(C76.0-C76.8, C80.9) or for hematopoietic, reticuloendothelial,
immunoproliferative, or
myeloproliferative disease (C42.0, C42.1, C42.3,
C42.4 or any site with hematopoietic
histologies).
If the procedure coded in this item was provided to prolong a patient’s life by
controlling
symptoms, to alleviate pain, or to make the patient more
comfortable, then also record this
surgery in the item Palliative Care
(NAACCR Item #3270).
Analytic Note: None.

202
Surgical Procedure Other Site continued
Code
Definition
Description
0 None
No surgical procedure of non-primary site was
performed
1
Non-primary surgical procedure
performed
Non-primary surgical resection to other site(s),
unknown if whether the site(s) is regional or distant
2
Non-primary surgical procedure to
other regional sites
Resection of regional site
3
Non-primary surgical procedure to
distant lymph node(s)
Resection of distant lymph node(s)
4
Non-primary surgical procedure to
distant site
Resection of distant site
5
Combination of codes
Any combination of surgical procedures 2, 3, or 4
9 Unknown
It is unknown whether any surgical procedure of a
non-primary site was performed

203
Surgical Inpatient Stay, Days from Surgery
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: SURG_DISCHARGE_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Most Definitive Surgical Resection of the
Primary Site (NAACCR Item #3170) and the Date of Surgical Discharge (NAACCR Item
#3180).
Registry Coding Instructions: Not applicable
Analytic Note: None.
Code
Definition
0000 - 9999
Number of elapsed days
blank
No first course surgery, surgery unknown, elapsed days cannot be
computed, or not available for these diagnosis years

204
Readmission to the Same Hospital within 30 Days of Surgical Discharge
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: READM_HOSP_30_DAYS
NAACCR Item #: 3190
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3, 9
Description: Records a readmission to the same hospital, for the same illness, within 30 days of
discharge following hospitalization for surgical resection of the primary site.
Registry Coding Instructions:
Consult patient record or information from the billing department to determine if a
readmission to the same hospital occurred within 30 days of the date recorded in the
item Date of Surgical Discharge (NAACCR Item #3180). Only record a readmission related
to the treatment of this cancer. Review the treatment plan to determine whether the
readmission was planned.
If there was an unplanned admission following surgical discharge, check for an ICD-9-CM
"E" code and record it, space allowing, as an additional ICD-9-CM Comorbidities and
Complications item (NAACCR #3110, 3120, 3130, 3140, 3150, 3160, 3161, 3162, 3163,
3164).
Analytic Note: None.
Code
Definition
0
No surgical procedure of the primary site was performed, or the patient was not readmitted to the
same hospital within 30 days of discharge
1
A patient was surgically treated and was readmitted to the same hospital within 30 days of being
discharged. This readmission was unplanned
2
A patient was surgically treated and was then readmitted to the same hospital within 30 days of
being discharged. This readmission was planned (chemotherapy port insertion, revision of
colostomy, etc.)
3
A patient was surgically treated and, within 30 days of being discharged, the patient had both a
planned and an unplanned readmission to the same hospital
9
It is unknown whether surgery of the primary site was recommended or performed. It is unknown
whether the patient was readmitted to the same hospital within 30 days of discharge
205
Reason for No Surgery of Primary Site
Data Dictionary Category: Treatment: Surgery
PUF Data Item Name: REASON_FOR_NO_SURGERY
NAACCR Item #: 1340
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 2, 5 - 9
Description:
Records the reason that no surgery was performed on the primary site.
Registry Coding Instructions:
If Surgical Procedure of Primary Site (NAACCR Item #1290) is coded 00, then record the
reason based on documentation in the patient record.
Code 1 if the treatment plan offered multiple options and the patient selected
treatment that did not include surgery of the primary site, or if the option of "no
treatment" was accepted by the patient.
Code 1 if Surgical Procedure of Primary Site (NAACCR Item #1290) is coded 98.
Code 7 if the patient refused recommended surgical treatment, made a blanket refusal
of all recommended treatment, or refused all treatment before any was recommended.
Cases coded 8 should be followed and updated to a more definitive code as appropriate.
Code 9 if the treatment plan offered multiple choices, but it is unknown which
treatment, if any was provided.
Analytic Note: None.

206
Reason For No Surgery of Primary Site continued
Code
Definition
0
Surgery of the primary site was performed
1
Surgery of the primary site was not performed because it was not part of the
planned first course treatment
2
Surgery of the primary site was not recommended/performed because it was
contraindicated due to patient risk factors (comorbid conditions, advanced age,
progression of tumor prior to planned surgery, etc.)
5
Surgery of the primary site was not performed because the patient died prior to
planned or recommended surgery
6
Surgery of the primary site was not performed; it was recommended by the
patient’s physician, but was not performed as part of the first course of therapy.
No reason was noted in patient record
7
Surgery of the primary site was not performed; it was recommended by the
patient’s physician, but this treatment was refused by the patient, the patient’s
family member, or the patient’s guardian. The refusal was noted in patient record
8
Surgery of the primary site was recommended, but it is unknown if it was
performed. Further follow up is recommended
9
It is unknown whether surgery of the primary site was recommended or
performed
207
Treatment: Radiation

208
Radiation, Days from Dx
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: DX_RAD_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date Radiation Started (NAACCR Item #1210).
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Radiation therapy not administered, radiation therapy unknown, or
cannot compute days elapsed due to missing or incomplete dates

209
Location of Radiation Therapy
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: RAD_LOCATION_OF_RX
NAACCR Item #: 1550
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 4, 8, 9
Description: Identifies the location where radiation therapy was administered during the first course
of treatment, as "at the reporting facility" or "elsewhere".
Registry Coding Instructions:
If the radiation treatment was provided to prolong a patient’s life by controlling
symptoms, to alleviate pain, or to make the patient more comfortable, then also record
the radiation administered in the items Palliative Care (NAACCR Item #3270) and/or
Palliative Care at this Facility (NAACCR Item #3280), as appropriate.
Analytic Note: None.
Code
Definition
Description
0
No radiation treatment
No radiation therapy was administered to the patient
1
All radiation treatment at this
facility
All radiation therapy was administered at the
reporting facility
2
Regional treatment at this
facility, boost elsewhere
Regional treatment was administered at the
reporting facility; a boost dose was administered
elsewhere
3
Boost radiation at this facility,
regional elsewhere
Regional treatment was administered elsewhere; a
boost dose was administered at the reporting facility
4
All radiation treatment
elsewhere
All radiation therapy was administered elsewhere
8 Other
Radiation therapy was administered, but the pattern
does not fit the above categories
9 Unknown
Radiation therapy was administered, but the
location of the treatment facility is unknown or not
stated in patient record; it is unknown whether
radiation therapy was administered
210
Phase I Radiation Primary Treatment Volume
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_RT_VOLUME
NAACCR Item #: 1504
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 07, 09 - 14, 20 - 26, 29 - 32, 39 - 42, 50 - 58, 60 - 68, 70 - 73, 80 - 86, 88, 90 - 95,
97 - 99
Description:
This is a new item in 2018. It was required in 2018 and optional in 2017. This item, in
conjunction with Phase I Radiation to Draining Lymph Nodes (NAACCR Item #1505)
replaces Radiation Treatment Volume (NAACCR Item #1540) and includes converted
historical values.
Identifies the primary treatment volume or primary anatomic target treated during the
first phase of radiation therapy during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018.
Rationale
Radiation treatment is commonly delivered in one or more phases. Typically, in each
phase, the primary tumor or tumor bed is treated. This data item should be used to
indicate the primary target volume, which might include the primary tumor or tumor
bed. If the primary tumor was not targeted, record the other regional or distant site that
was targeted. Draining lymph nodes may also be concurrently targeted during the first
phase. These will be identified in a separate data item Phase I Radiation to Draining
Lymph Nodes [1505]. This data item provides information describing the anatomical
structure targeted by radiation therapy during the first phase of radiation treatment and
can be used to determine whether the site of the primary disease was treated with
radiation or if other regional or distant sites were targeted. This information is useful in
evaluating the patterns of care within a facility and on a regional or national basis. The
breakdown and reorganization of the sites will allow for concise reporting.
Registry Coding Instructions
• Radiation treatment volume will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the exact treatment
volume may require assistance from the radiation oncologist for consistent coding.
211
Phase I Radiation Primary Treatment Volume continued
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
• If one or more discrete volumes are treated and one of those includes the primary
site, record the treatment to the primary site in this data item.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system, and it should be coded as a new phase
of radiation therapy. O Note: “on-line adaptive therapy” refers to treatments where
radiation treatment plans are adapted or updated while a patient is on the treatment
table. When treatment plans are adapted, the shape of the target volume may change
from day to day, but for registry purposes, the volume that is being targeted won’t
change. An adapted plan should not be coded as though a new phase of treatment has
been initiated unless, as above, the radiation oncologist documents it as a new phase in
the radiation treatment summary.
• Phase I of radiation treatment also commonly includes draining lymph node regions
that are associated with the primary tumor or tumor bed. The draining lymph nodes are
recorded in the Phase I Radiation to Draining Lymph Nodes [1505]. Use codes 01 to 09
only when the lymph nodes are the primary target.
Note: When the primary volume is lymph nodes, draining lymph nodes are not targeted.
Record code 88 in the Phase I Radiation to Draining Lymph Nodes [1505].
• This data item, in conjunction with Phase I Radiation to Draining Lymph Nodes [1505],
replaces the Radiation Treatment Volume [1540] and includes converted historical
values. Conversion took place upon upgrade to NAACCR v18-compliant software; as of
2018 this data item is required for all cases regardless of diagnosis year.
See STORE Manual 2018 for more information at
https://www.facs.org/-/media/files/quality-
programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None

212
Phase I Radiation Primary Treatment Volume continued
Code
Definition
Description
00
No radiation
treatment
Radiation therapy not administered
01
Neck lymph node
regions
The primary treatment is directed at lymph node regions of the neck.
Examples include treatment of lymphoma or lymph node recurrence (in the
absence of primary site failure) following definitive surgery of the primary
tumor. If radiation to the neck lymph nodes includes the supraclavicular region
use code 03
02
Thoracic lymph
node regions
Radiation therapy is directed to some combination of hilar, mediastinal, and
supraclavical lymph nodes without concurrent treatment of a visceral organ
site. Examples include mantle or mini-mantle for lymphomas, and treatment
of lymphatic recurrence after complete surgical excision of a thoracic primary.
Note that the supraclavical region may be part of a head and neck lymph node
region. Use code 03 for treatments directed at neck nodes and supraclavicular
lymph nodes with a head and neck primary. Use code 04 if supraclavicular
lymph nodes are part of breast treatment
03
Neck and thoracic
lymph node regions
Treatment is delivered to lymph nodes in the neck and thoracic region without
concurrent treatment of a primary visceral tumor. This code might apply to
some mantle or mini-mantle fields used in lymphoma treatments or some
treatments for lymphatic recurrences following definitive treatment for tumors
of the head and neck thoracic regions
04
Breast/Chest wall
lymph node regions
Radiation is directed primarily to some combination of axillary, supraclavicular,
and/or internal mammary lymph node sites WITHOUT concurrent treatment of
the breast or chest wall. If the breast AND lymph nodes are being treated, then
code the Primary Treatment Volume to Breast (codes 40 or 41) and
Breast/chest wall lymph nodes (code 04) in Radiation to Draining Lymph Nodes
05
Abdominal lymph
nodes
Treatment is directed to some combination of the lymph nodes of the
abdomen, including retro-crural, peri-gastric, peri-hepatic, portocaval and
para-aortic nodes. Possible situations might include seminoma, lymphoma or
lymph node recurrence following surgical resection of the prostate, bladder or
uterus

213
Phase I Radiation Primary Treatment Volume continued
06 Pelvic lymph nodes
Treatment is directed to some combination of the lymph nodes of the pelvis,
including the common, internal and external iliac, obturator, inguinal and peri-
rectal lymph nodes. This might be done for lymphoma or lymph node
recurrence following definitive surgery for a pelvic organ
07
Abdominal and
pelvic lymph nodes
Treatment is directed to a combination of lymph nodes in both the abdomen
and pelvis. This code includes extended fields (“hockey stick”, “dog-leg”,
“inverted Y”, etc.) utilized to treat seminomas and lymphomas or recurrence of
a solid tumor
09
Lymph node region
NOS
This category should be used to code treatments directed at lymph node
regions that are not adequately described by codes 01-07
10
Eye/orbit/optic
nerve
Treatment is directed at all or a portion of the eye, orbit and/or optic nerve
11 Pituitary Treatment is directed at the pituitary gland
12
Brain
Treatment is directed at all the brain and its meninges (“Whole brain”)
13 Brain (limited)
Treatment is directed at one or more sub-sites of the brain but not the whole
brain. Chart may describe “SRS”, “Stereotactic Radiosurgery”, “Gamma Knife®”
14 Spinal cord Treatment is directed at all or a portion of the spinal cord or its meninges
20 Nasopharynx Treatment is directed at all or a portion of the nasopharynx
21 Oral cavity
Treatment is directed at all or a portion of the oral cavity, including the lips,
gingiva, alveolus, buccal mucosa, retromolar trigone, hard palate, floor of
mouth and oral tongue
22 Oropharynx
Treatment is directed at all or a portion of the oropharynx, including the soft
palate, tonsils, base of tongue and pharyngeal wall
23
Larynx (glottis) or
hypopharynx
Treatment is directed at all or a portion of the larynx and/or hypopharynx
24 Sinuses/Nasal tract
Treatment is directed at all or a portion of the sinuses and nasal tract, including
the frontal, ethmoid, sphenoid and maxillary sinuses
25
Parotid or other
salivary glands
Treatment is directed at the parotid or other salivary glands, including the
submandibular, sublingual and minor salivary glands
26 Thyroid
Treatment is directed at all or a portion of the thyroid. Code this volume when
the thyroid is treated with I-131 radioisotope

214
Phase I Radiation Primary Treatment Volume continued
29
Head and neck
(NOS)
The treatment volume is directed at a primary tumor of the head and neck, but
the primary sub-site is not a head and neck organ identified by codes 20-26 or
it is an “unknown primary”
30 Lung or bronchus Treatment is directed at all or a portion of the lung or bronchus
31 Mesothelium
Treatment is directed to all or a portion of the mesothelium. This code should
be used for mesothelioma primaries, even if a portion of the lung is included in
the radiation field
32 Thymus Treatment is directed to all or a portion of the thymus
39 Chest/lung (NOS)
The treatment is directed at a primary tumor of the chest, but the primary sub-
site is unknown or not identified in codes 30-32. For example, this code should
be used for sarcomas arising from the mediastinum
40 Breast (whole)
Treatment is directed at all the intact breast. Intact breast includes breast
tissue that either was not surgically treated or received a lumpectomy or
partial mastectomy
41 Breast (partial)
Treatment is directed at a portion of the intact breast but not the whole
breast. The chart may have terms such as “Mammosite”, “interstitial (seed)
implant)”, or “(accelerated) partial breast irradiation”. Consider the possibility
of partial breast irradiation when “IMRT” is documented in the record
42 Chest wall Treatment encompasses the chest wall (following mastectomy)
50 Esophagus
Treatment is directed at all or a portion of the esophagus. Include tumors of
the gastro-esophageal junction
51 Stomach Treatment is directed at all or a portion of the stomach
52 Small bowel Treatment is directed at all or a portion of the small bowel
53 Colon Treatment is directed at all or a portion of the colon
54
Rectum
Treatment is directed at all or a portion of the rectum
55
Anus
Treatment is directed at all or a portion of the anus
56
Liver
Treatment is directed at all or a portion of the liver
57
Biliary tree or
gallbladder
Treatment is directed at all or a portion of the biliary tree or gallbladder

215
Phase I Radiation Primary Treatment Volume continued
58
Pancreas or
hepatopancreatic
ampulla
Treatment is directed at all or a portion of the pancreas or the
hepatopancreatic ampulla. Hepatopancreatic ampulla tumors are sometimes
referred to as periampullary tumors
59 Abdomen (NOS)
The treatment volume is directed at a primary tumor of the abdomen, but the
primary sub-site is not an abdominal organ defined by codes 50-58 or it is
considered to be an "unknown primary". For example, this code should be
used for sarcomas arising from the abdominal retroperitoneum.
60 Bladder (whole) Treatment is directed at all the bladder
61 Bladder (partial) Treatment is directed at a portion of the bladder but not the whole bladder
62
Kidney
Treatment is directed at all or a portion of the kidney
63 Ureter Treatment is directed at all or a portion of the ureter
64 Prostate (whole)
Treatment is directed at all the prostate and/or seminal vesicles. Use this code
even if seminal vesicles are not explicitly targeted
65 Prostate (partial) Treatment is directed at a portion of the prostate but not the whole prostate
66
Urethra
Treatment is directed at all or a portion of the urethra
67 Penis
Treatment is directed at all or a portion of the penis. Treatments of urethral
primaries should be coded as ‘urethra’ (code 66)
68 Testicle or scrotum Treatment is directed at all or a portion of the testicle and/or scrotum
70
Ovaries or fallopian
tubes
Treatment is directed at all or a portion of the ovaries or fallopian tubes
71 Uterus or cervix Treatment is directed at all or a portion of the uterus, endometrium or cervix
72 Vagina
Treatment is directed at all or a portion of the vagina. Treatments of urethral
primaries should be coded as ‘urethra’ (code 66)
73 Vulva
Treatment is directed at all or a portion of the vulva. Treatments of urethral
primaries should be coded as ‘urethra’ (code 66)
80 Skull
Treatment is directed at all or a portion of the bones of the skull. Any brain
irradiation is a secondary consequence
81
Spine/vertebral
bodies
Treatment is directed at all or a portion of the bones of the spine/vertebral
bodies, including the sacrum. Spinal cord malignancies should be coded using
‘spinal cord’ (code 14)

216
Phase I Radiation Primary Treatment Volume continued
82 Shoulder
Treatment is directed to all or a portion of the proximal humerus, scapula,
clavicle, or other components of the shoulder complex
83
Ribs
Treatment is directed at all or a portion of one or more ribs
84 Hip Treatment is directed at all or a portion of the proximal femur or acetabulum
85 Pelvic bones
Treatment is directed at all or a portion of the bones of the pelvis other than
the hip or sacrum
86
Pelvis (NOS, non-
visceral)
The treatment volume is directed at a primary tumor of the pelvis, but the
primary sub-site is not a pelvic organ or is not known or indicated. For
example, this code should be used for sarcomas arising from the pelvis
88
Extremity bone,
NOS
Treatment is directed at all or a portion of the bones of the arms or legs. This
excludes the proximal femur (Hip, code 84). This excludes the proximal
humerus (Shoulder, code 82)
90 Skin
Treatment is directed at all or a portion of the skin. The primary malignancy
originates in the skin and the skin is the primary target. So-called skin
metastases are usually subcutaneous and should be coded as a soft tissue site
91 Soft Tissue
This category should be used to code primary or metastatic soft tissue
malignancies not fitting other categories
92 Hemibody
A single treatment volume encompassing either all structures above the
diaphragm, or all structures below the diaphragm. This is almost always
administered for palliation of widespread bone metastasis in patients with
prostate or breast cancer
93 Whole body Treatment is directed to the entire body included in a single treatment
94
Mantle, mini-
mantle (obsolete
after 2017)
For conversion of historic data only
95
Lower extended
field (obsolete after
2017)
For conversion of historic data only
97
Invalid historical
FORDS value
Conversion to new STORE data item could not take place due to an invalid
FORDS Volume code

217
Phase I Radiation Primary Treatment Volume continued
98 Other
Radiation therapy administered; treatment volume other than those previously
categorized by codes 01-93
99 Unknown
This category should be used to code treatments for which there is no
information available about the treatment volume, or it is unknown if radiation
treatment was administered
218
Phase I Radiation to Draining Lymph Nodes
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_RT_TO_LN
NAACCR Item #: 1505
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 – 08, 88, 99
Description:
This is a new item in 2018. It was required in 2018, and optional in 2017. This data item,
in conjunction with Phase I Radiation Primary Treatment Volume [1504], replaces the
Radiation Treatment Volume [1540] and includes converted historical values.
Identifies the draining lymph nodes treated (if any) during the first phase of radiation
therapy delivered to the patient during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018.
Rationale
The first phase of radiation treatment commonly targets both the primary tumor (or
tumor bed) and draining lymph nodes as a secondary site. This data item should be used
to indicate the draining regional lymph nodes, if any, that were irradiated during the
first phase of radiation to the primary site.
Registry Coding Instructions
• Radiation treatment to draining lymph nodes will typically be found in the radiation
oncologist’s summary letter for the first course of treatment. Determination of the exact
draining lymph nodes may require assistance from the radiation oncologist for
consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
• Phase I of radiation treatment includes primary tumor or tumor bed in addition to the
draining lymph node regions that are associated with the primary tumor or tumor bed.
The primary tumor or tumor bed is recorded in the Phase I Radiation Primary Treatment
Volume [1504]. Note: When the Primary Treatment Volume is lymph nodes, draining
lymph nodes are not targeted. Record code 88 in this data item.

219
Phase I Radiation to Draining Lymph Nodes continued
• This data item, in conjunction with Phase I Radiation Primary Treatment Volume
[1504], replaces the Radiation Treatment Volume [1540] and includes converted
historical values. Conversion took place upon upgrade to NAACCR v18-compliant
software; as of 2018 this data item is required for all cases regardless of diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None
Code
Definition
00
No radiation to draining lymph nodes.
01
Neck lymph node regions
02
Thoracic lymph node regions
03
Neck and thoracic lymph node regions
04
Breast/ Chest wall lymph node regions
05
Abdominal lymph nodes
06
Pelvic lymph nodes
07
Abdominal and pelvic lymph nodes
08
Lymph node region, NOS
88
Not applicable; Radiation primary treatment is lymph nodes
99
Unknown if any radiation treatment to draining lymph
nodes; Unknown if radiation treatment administered
220
Phase I Radiation Treatment Modality
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_RT_MODALITY
NAACCR Item #: 1506
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 16, 99
Description:
This is a new data item, introduced in 2018. It was required in 2018, and optional in
2017. This data item, in conjunction with Phase I Radiation External Beam Planning
Technique [1502], replaces the Rad--Regional RX Modality [1570] and includes
converted historical values.
Identifies the radiation modality administered during the first phase of radiation
treatment delivered during the first course of treatment. This data item is required for
CoC-accredited facilities as of 01/01/2018.
Rationale
Radiation modality reflects whether a treatment was external beam, brachytherapy, a
radioisotope as well as their major subtypes, or a combination of modalities. This data
item should be used to indicate the radiation modality administered during the first
phase of radiation. Historically, the previously-named Regional Treatment Modality
[1570] utilized codes that were not mutually exclusive. Rather, it included codes
describing a mix of modalities, treatment planning techniques, and delivery techniques
that are commonly utilized by radiation oncologists. However, every phase of radiation
treatment will include a specified modality, planning technique, and delivery technique.
The goal of the 2018 implementation of separate phase-specific data items for the
recording of radiation modality and external beam radiation treatment planning
techniques is to clarify this information and implement mutually exclusive categories. A
separate data item for delivery technique has not been implemented because this
information is not consistently reported in end of treatment summaries.
Registry Coding Instructions
• Radiation treatment modality will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Segregation of treatment components
into Phases and determination of the respective treatment modality may require
assistance from the radiation oncologist to ensure consistent coding.
221
Phase I Radiation Treatment Modality continued
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (I.e. dose given during a session), modality or treatment
technique. Any one of these changes will mean that a new radiation plan will be
generated in the treatment planning system, and it should be coded as a new phase of
radiation therapy.
• For purposes of this data item, photons, x-rays and gamma-rays are equivalent.
• Use code 13 - Radioisotopes, NOS for radioembolization procedures, e.g. intravascular
Yttrium-90.
• This data item intentionally does not include reference to various MV energies
because this is not a clinically important aspect of technique. A change in MV energy
(e.g., 6MV to 12MV) is not clinically relevant and does not represent a change in
treatment technique. It is rare for change in MV energy to occur during any phase of
radiation therapy.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system and should be coded as a new phase of
radiation therapy.
• If this data item is coded to any of the External beam codes (01-06), the planning
technique must be recorded in the data item Phase I External Beam Radiation Planning
Technique [1502].
Note: Do not confuse a radioiodine scan with treatment. Only treatment is recorded in
this item.
• This data item, in conjunction with Phase I Radiation External Beam Planning
Technique [1502], replaces the Rad--Regional RX Modality [1570] and includes
converted historical values. Conversion took place upon upgrade to NAACCR v18-
compliant software; as of 2018 this data item is required for all cases regardless of
diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

222
Phase I Radiation Treatment Modality continued
Code
Definition
00
No radiation treatment
01
External beam, NOS
02
External beam, photons
03
External beam, protons
04
External beam, electrons
05
External beam, neutrons
06
External beam, carbon ions
07
Brachytherapy, NOS
08
Brachytherapy, intracavitary, LDR
09
Brachytherapy, intracavitary, HDR
10
Brachytherapy, interstitial, LDR
11
Brachytherapy, interstitial, HDR
12
Brachytherapy, electronic
13
Radioisotopes, NOS
14
Radioisotopes, Radium-223
15
Radioisotopes, Strontium-89
16
Radioisotopes, Strontium-90
98
Radiation Rx administered, Rx modality
unknown
99
Radiation treatment modality unknown;
Unknown if radiation treatment
administered
223
Phase I External Beam Radiation Planning Technique
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_BEAM_TECH
NAACCR Item #: 1502
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 10, 88, 98, 99
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This data
item, in conjunction with Phase I Radiation Treatment Modality [1506], replaces the
Rad-- Regional RX Modality [1570] and includes converted historical values.
Identifies the external beam radiation planning technique used to administer the first
phase of radiation treatment during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018.
Rationale
External beam radiation is the most commonly-used radiation modality in North
America. In this data item we specified the planning technique for external beam
treatment. Identifying the radiation technique is of interest for patterns of care and
comparative effectiveness studies. Historically, the previously-named Regional
Treatment Modality [1570] utilized codes that were not mutually exclusive. Rather, it
included codes describing a mix of modalities, treatment planning techniques, and
delivery techniques that are commonly utilized by radiation oncologists. However, every
phase of radiation treatment will include a specified modality, planning technique, and
delivery technique. The goal of the 2018 implementation of separate phase-specific data
items for the recording of Phase I Radiation Treatment Modality [1506] and Phase I
External Beam Radiation Planning Technique [1502] is to clarify this information and
implement mutually exclusive categories. Note that Planning Technique details are not
being captured for non-External Beam modalities. A separate data item for delivery
technique has not been implemented because this information is not consistently
reported in end treatment summaries.
Registry Coding Instructions
• Radiation external beam treatment planning technique will typically be found in the
radiation oncologist’s summary letter for the first course of treatment. Determination of
the external beam planning technique may require assistance from the radiation
oncologist to ensure consistent coding.
224
Phase I External Beam Radiation Planning Technique continued
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase III,
etc. accordingly.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment technique.
Any one of these changes will generally mean that a new radiation plan will be generated
in the treatment planning system and should be coded as a new phase of radiation
therapy.
• Note: “on-line adaptive therapy” refers to treatments where radiation treatment plans are
adapted or updated while a patient is on the treatment table. When treatment plans are
adapted, the shape of the target volume may change from day to day but, for registry
purposes, the volume that is being targeted won’t change. An adapted plan should not be
coded as though a new phase of treatment has been initiated unless, as above, the
radiation oncologist documents it as a new phase in the radiation treatment summary.
Two new technique codes have been added to capture when online adaptive therapy is
occurring: CT guided and MR guided adaptive therapy.
• Code 05 for Intensity Modulated Therapy (IMT) or Intensity Modulated Radiation Therapy
(IMRT)
• Code 04 for Conformal or 3-D Conformal Therapy whenever either is explicitly mentioned.
• When code 98 is recorded, document the planning technique in the appropriate text data
item.
• This data item, in conjunction with Phase I Radiation Treatment Modality [1506], replaces
the Rad-- Regional RX Modality [1570] and includes converted historical values. Conversion
took place upon upgrade to NAACCR v18-compliant software; as of 2018 this data item is
required for all cases regardless of diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
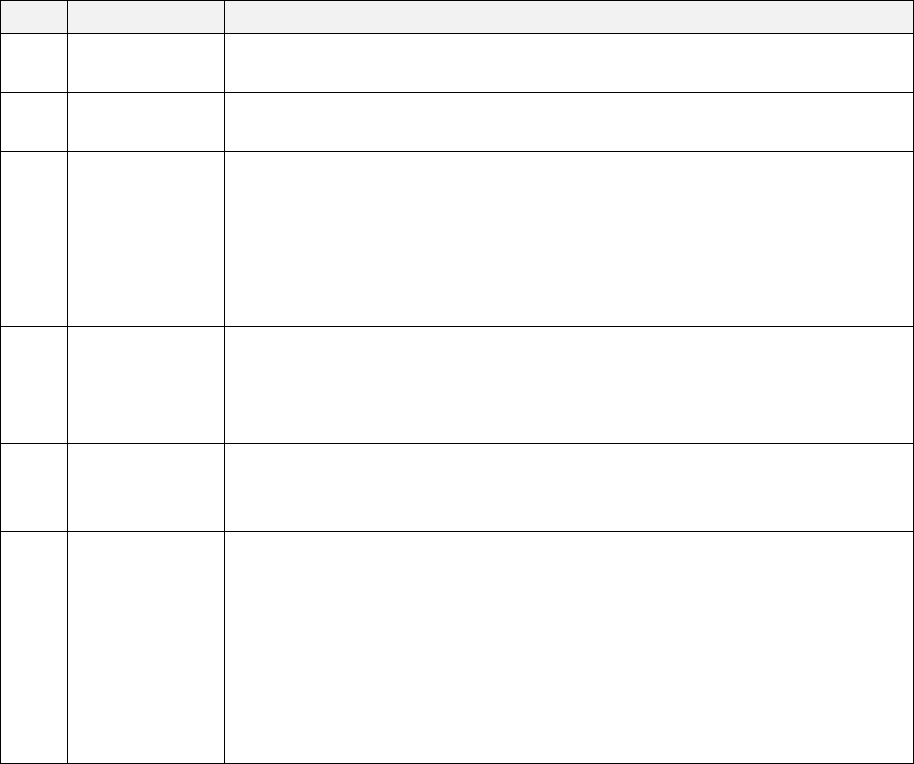
225
Phase I External Beam Radiation Planning Technique continued
Code
Definition
Description
00
No radiation
treatment
Radiation therapy was not administered to the patient
01
External beam,
NOS
The treatment is known to be by external beam, but there is insufficient
information to determine the specific planning technique
02
Low energy x-
ray/photon
therapy
External beam therapy administered using equipment with a maximum
energy of less than one (1) million volts (MV). Energies are typically
expressed in units of kilovolts (kV). These types of treatments are
sometimes referred to as electronic brachytherapy or orthovoltage or
superficial therapy. Clinical notes may refer to the brand names of low
energy x-ray delivery devices, e.g. Axxent®, INTRABEAM®, or Esteya®
03 2-D therapy
An external beam planning technique using 2-D imaging, such as plain film
x-rays or fluoroscopic images, to define the location and size of the
treatment beams. Should be clearly described as 2-
D therapy. This planning
modality is typically used only for palliative treatments
04
Conformal or 3-
D conformal
therapy
An external beam planning technique using multiple, fixed beams shaped
to conform to a defined target volume. Should be clearly described as
conformal or 3-D therapy in patient record
05
Intensity
modulated
therapy
An external beam planning technique where the shape or energy of beams
is optimized using software algorithms. Any external beam modality can be
modulated but these generally refer to photon or proton beams. Intensity
modulated therapy can be described as intensity modulated radiation
therapy (IMRT), intensity modulated xray or proton therapy (IMXT/IMPT),
volumetric arc therapy (VMAT) and other ways. If a treatment is described
as IMRT with online reoptimization/re-planning, then it should be
categorized as online reoptimization or re-planning

226
Phase I External Beam Radiation Planning Technique continued
06
Stereotactic
radiotherapy or
radiosurgery,
NOS
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques, but the treatment is not described as Cyberknife® or Gamma
Knife®. These approaches are sometimes described as SBRT (stereotactic
body radiation), SABR (stereotactic ablative radiation), SRS (stereotactic
radiosurgery), or SRT (stereotactic radiotherapy). If the treatment is
described as robotic radiotherapy (e.g. Cyberknife®) or Gamma Knife®, use
stereotactic radiotherapy subcodes below. If a treatment is described as
stereotactic radiotherapy or radiosurgery with online re-optimization/re-
planning, then it should be categorized as online re-optimization or re-
planning
07
Sterotactic
radiotherapy or
radiosurgery,
robotic
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques which is specifically described as robotic (e.g. Cyberknife®)
08
Stereotactic
radiotherapy or
radiosurgery,
Gamma Knife®
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques which uses a Cobalt-60 gamma ray source and is specifically
described as Gamma Knife®. This is most commonly used for treatments in
the brain
09
CT-guided
online adaptive
therapy
An external beam technique in which the treatment plan is adapted over
the course of radiation to reflect changes in the patient’s tumor or normal
anatomy radiation using a CT scan obtained at the treatment machine
(online). These approaches are sometimes described as CT-guided online
re-optimization or online re-planning. If a treatment technique is described
as both CT-guided online adaptive therapy as well as another external
beam technique (IMRT, SBRT, etc.), then it should be categorized as CT-
guided online adaptive therapy. If a treatment is described as “adaptive”
but does not include the descriptor “online”, this code should not be used
10
MR-guided
online adaptive
therapy
An external beam technique in which the treatment plan is adapted over
the course of radiation to reflect changes in the patient’s tumor or normal
anatomy radiation using an MRI scan obtained at the treatment machine
(online). These approaches are sometimes described as MR-guided online
re-optimization or online re-planning. If a treatment technique is described
as both MR-guided online adaptive therapy as well as another external
beam technique (IMRT, SBRT, etc.), then it should be categorized as MR-
guided online adaptive therapy. If a treatment is described as “adaptive”
but does not include the descriptor “online”, this code should not be used

227
Phase I External Beam Radiation Planning Technique continued
88
Not applicable
Treatment not by external beam
98 Other, NOS
Other radiation, NOS; Radiation therapy administered, but the treatment
modality is not specified or known
99
Unknown
It is unknown whether radiation therapy was administered
228
Phase I Dose per Fraction
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_DOSE_FRACT
NAACCR Item #: 1501
Diagnosis Years Available: 2004 +
Length: 5
Allowable Values: 00000 - 99999
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This data
item replaces the Rad--Regional Dose: cGy [1510] and includes mapped historical values.
Records the dose per fraction (treatment session) delivered to the patient in the first
phase of radiation during the first course of treatment. The unit of measure is centi-Gray
(cGy). This data item is required for CoC-accredited facilities as of 01/01/2018.
Rationale
Radiation therapy is delivered in one or more phases with identified dose per fraction.
It is necessary to capture information describing the dose per fraction to evaluate
patterns of radiation oncology care. Outcomes are strongly related to the dose
delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording
doses at the axis point where applicable (opposed fields, four field box, wedged pair,
and so on). For maximum consistency in this data item, the ICRP recommendations
should be followed whenever possible. Where there is no clear axis point, record the
total dose as indicated in the summary chart.
• Radiation treatment Phase I dose will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the Phase I dose of
radiation therapy may require assistance from the radiation oncologist for consistent
coding.
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
• Record the actual dose delivered (NOT the initially prescribed dose) as documented in
the treatment summary.

229
Phase I Dose per Fraction continued
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt
Gray Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase I Total Dose multiply
cGe by 100).
• Note that dose is still occasionally specified in “rads”. One rad is equivalent to one
centi-Gray (cGy).
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• Code 99998 when radioisotopes were administered to the patient (codes 13-16 for
Phase I Treatment Modality [1506]).
• This data item replaces the Rad--Regional Dose: cGy [1510] and includes mapped
historical values. 1-1 mapping took place upon upgrade to NAACCR v18-compliant
software; as of 2018 this data is required for all cases regardless of diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
00000
No radiation treatment
00001-99997
Record the actual Phase I dose delivered in cGy
99998
Not applicable, radioisotopes administered to the patient
99999
Regional radiation therapy was administered but dose is unknown;
Unknown whether radiation therapy was administered

230
Phase I Dose per Fraction continued
Examples
Code
Reason
00200
A patient with Stage III prostate carcinoma received pelvic irradiation to 5,000 cGy over 25
fractions followed by a Phase II (boost) prostate irradiation to 7,000 cGy. Record the Phase I
dose per fraction as 00200 (5000/25).
00150
A patient with a left supraclavicular metastasis from a gastric carcinoma received 6,000 cGy
to the left supraclavicular region over 40 fractions. The dose is calculated at the prescribed
depth of 3cm. A secondary calculation shows a Dmax dose of 6,450 cGy. Record the Phase I
dose per fraction as 00150 (6000/40).
00220
A patient with a Stage II breast carcinoma is treated with the breast intact. Tangent fields are
utilized to bring the dose of the breast to 5,500 cGy over 25 fractions. Phase II (boost) in the
primary tumor bed delivered to a small volume in the breast. Record phase I dose per
fraction as 00220 (5500/25).
231
Phase I Number of Fractions
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_NUM_FRACT
NAACCR Item #: 1503
Diagnosis Years Available: 2004 +
Length: 3
Allowable Values: 000 - 999
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. It replaces Number of
Treatments to this Volume (NAACCR Item #1520) and includes mapped historical values.
Records the total number of fractions (treatment sessions) delivered to the patient in the first
phase of radiation during the first course of treatment. This data item is required for CoC-
accredited facilities as of 01/01/2018.
Rationale
Radiation therapy is delivered in one or more phases with each phase spread out over a number
of fractions (treatment sessions). It is necessary to capture information describing the number
of fraction(s) to evaluate patterns of radiation oncology care.
Registry Coding instructions
• The number of fractions or treatments will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the exact number of
treatments or fractions delivered to the patient may require assistance from the radiation
oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase may
be referred to as a boost or cone down, and would be recorded as Phase II, Phase III, etc.
accordingly.
• Although a fraction or treatment session may include several treatment portals delivered
within a relatively confined period of time-usually a few minutes-it is still considered one
session.
• Count each separate administration of brachytherapy or implants as a single fraction or
treatment.
• Record the actual number of fractions delivered (NOT initially prescribed), as documented in
the treatment summary.

232
Phase I Number of Fractions continued
• There may be times when the first course of treatment information is incomplete. Therefore,
it is important to continue follow-up efforts to be certain the complete treatment information is
collected.
• This data item replaces the Rad--No of Treatment Vol [1520] and includes mapped values for
historical cases. 1-1 mapping took place upon upgrade to NAACCR v18-compliant software; as of
2018 this item was required regardless of the diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-/media/files/quality-
programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000
No radiation treatment
001-998
Number of fractions administered to the patient during the first phase of radiation
therapy
999
Phase I Radiation therapy was administered, but the number of fractions is unknown;
It is unknown whether radiation therapy was administered
Examples
Code
Reason
025
A patient with breast carcinoma had treatment sessions in which treatment was delivered to
the chest wall and encompassing the ipsilateral supraclavicular region for a total of three
fraction portals. Twenty-five treatment sessions were given. Record 25 fractions as 025.
025
A patient with Stage IIIB bronchogenic carcinoma received 25 treatments to the left hilum and
mediastinum, given in 25 daily fractions over five weeks.
050
A patient with advanced head and neck cancer was treated using “hyperfractionation.” Three
fields were delivered in each session; two sessions were given each day, six hours apart, with
each session delivering a total dose of 150 cGy. Treatment was given for a total of 25 days.
Record 50 fractions as 050.
010
The patient was given Mammosite® brachytherapy, repeated in 10 separate sessions. Record
10 fractions as 010.
001
Prostate cancer patient treated with a single administration of seeds. Record 1 fraction as 001.
233
Phase I Total Dose
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_I_TOTAL_DOSE
NAACCR Item #: 1507
Diagnosis Years Available: 2004 +
Length: 6
Allowable Values: 000000 - 999999
Description:
This data item is an all new data item in 2018 includes mapped values for historical cases. It was
optional for 2017 and required for 2018.
Identifies the total radiation dose delivered to the patient in the first phase of radiation
treatment during the first course of treatment. The unit of measure is centi-Gray (cGy). This data
item is required for CoC accredited facilities for cases diagnosed as of 01/01/2018.
Rationale
To evaluate the patterns of radiation care, it is necessary to capture information describing the
prescribed dose of Phase I radiation to the patient during the first course of treatment.
Outcomes are strongly related to the total dose delivered.
Registry Coding instructions
• The International Council for Radiation Protection (ICRP) recommends recording doses at the
axis point where applicable (opposed fields, four field box, wedged pair, and so on). For
maximum consistency in this data item, the ICRP recommendations should be followed
whenever possible. Where there is no clear axis point, record the total dose as indicated in the
summary chart. Determining the exact dose may require assistance from the radiation
oncologist for consistent coding.
• Phase I radiation treatment dose will typically be found in the radiation oncologist’s summary
letter for the first course of treatment. Determination of the Phase I dose of radiation therapy
may require assistance from the radiation oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase may
be referred to as a boost or cone down, and would be recorded as Phase II, Phase III, etc.
accordingly.
• Record the actual total dose delivered (NOT initially prescribed), as documented in the
treatment summary. The value recorded for this data item should NOT be auto-calculated
within the registry abstraction software.

234
Phase I Total Dose continued
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt Gray
Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase I Total Dose, you would need to
multiply cGe by 100).
• Note that dose is still occasionally specified in “rads”. One rad is equivalent to one centi-Gray
(cGy).
• Code 000000, radiation therapy not administered.
• Code 999998 when radioisotopes are administered to the patient (codes 13-16 recorded in the
Phase I Treatment Modality [1506]).
• There may be times when the first course of treatment information is incomplete. Therefore,
it is important to continue follow-up efforts to be certain the complete treatment information is
collected.
• This data item is an all new data item in 2018 includes mapped values for historical cases.
Mapping took place upon upgrade to NAACCR v18-compliant software; as of 2018 this data item
is required for all cases regardless of diagnosis year.
See STORE Manual 2018 for more information at https://www.facs.org/-/media/files/quality-
programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000000
No radiation treatment
000001-999997
Record the actual dose delivered in cGy
999998
Not applicable, radioisotopes administered to the patient
999999
Radiation therapy was administered, but the total dose is
unknown;
it is unknown whether radiation therapy was administered

235
Phase I Total Dose continued
Examples
Code
Reason
005000
A patient with Stage III prostate carcinoma received pelvic irradiation of 5,000 cGy during
Phase I Radiation Treatment. Record the Phase I Total Dose of 5,000 cGy as 005000.
006000
A patient with a left supraclavicular metastasis from a gastric carcinoma received 6,000 cGy
to the left supraclavicular region. Record the Phase I Total Dose of 6,000 cGy as 006000.
005500
A patient with a Stage II breast carcinoma is treated with the breast intact. Tangent fields
are utilized to bring the dose of the breast to 5,500 cGy. The supraclavicular (draining)
lymph nodes are treated 4,500 cGy, calculated to a depth of 3 cm, and Phase II radiation
treatment in the primary tumor bed is delivered to a small volume in the breast. Record the
Phase I Total Dose of 5,500cGy as 005500. Ignore the fact that a sub-region (supraclavicular
nodes) received a lower dose than the breast in Phase I. Planned or otherwise, dose
variations in the target volume may vary up to about 10%.
236
Phase II Radiation Primary Treatment Volume
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_RT_VOLUME
NAACCR Item #: 1514
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 07, 09 - 14, 20 - 26, 29 - 32, 39 - 42, 50 - 58, 60 - 68, 70 - 73, 80 - 86, 88, 90 - 95,
97 - 99, blank
Description:
This is a new item in 2018. It was required in 2018 and optional in 2017. This data item may
include converted historical values. It was converted from Radiation Treatment Volume
(NAACCR Item #1540) when Boost Treatment Modality (NAACCR Item #3200) was administered.
Identifies the primary treatment volume or primary anatomic target treated during the second
phase of radiation therapy during the first course of treatment. This data item is required for
CoC-accredited facilities as of 01/01/2018.
Rationale
Radiation treatment is commonly delivered in one or more phases. Typically, in each phase, the
primary tumor or tumor bed is treated. This data item should be used to indicate the primary
target volume, which might include the primary tumor or tumor bed. If the primary tumor was
not targeted, record the other regional or distant site that was targeted. Draining lymph nodes
may also be targeted during the second phase. These will be identified in a separate data item
Phase II Radiation to Draining Lymph Nodes [1515]. This data item provides information
describing the anatomical structure targeted by radiation therapy during the second phase of
radiation treatment and can be used to determine whether the site of the primary disease was
treated with radiation or if other regional or distant sites were targeted. This information is
useful in evaluating the patterns of care within a facility and on a regional or national basis. The
breakdown and reorganization of the sites will allow for concise reporting.
Registry Coding Instructions
• Radiation treatment volume will typically be found in the radiation oncologist’s summary
letter for the first course of treatment. Determination of the exact treatment volume may
require assistance from the radiation oncologist for consistent coding.
• The first phase of radiation treatment may be commonly referred to as an initial plan and a
subsequent phase may be referred to as a boost or cone down, and would be recorded in this
field with subsequent phases recorded as Phase II, Phase III, etc. accordingly.
237
Phase II Radiation Primary Treatment Volume continued
• If one or more discrete volumes are treated and one of those includes the primary site, record
the Phase II treatment to the primary site in this data item.
• A new phase begins when there is a clinically meaningful change in target volume, treatment
fraction size (i.e., dose given during a session), modality or treatment technique. Any one of
these changes will generally mean that a new radiation plan will be generated in the treatment
planning system, and it should be coded as a new phase of radiation therapy.
Note: “on-line adaptive therapy” refers to treatments where radiation treatment plans are
adapted or updated while a patient is on the treatment table. When treatment plans are
adapted, the shape of the target volume may change from day to day, but for registry purposes,
the volume that is being targeted won’t change. An adapted plan should not be coded as though
a new phase of treatment has been initiated unless, as above, the radiation oncologist
documents it as a new phase in the radiation treatment summary.
• Phase II of radiation treatment also commonly includes draining lymph node regions that are
associated with the primary tumor or tumor bed. The draining lymph nodes are recorded in the
Phase II Radiation to Draining Lymph Nodes [1515].
Note: When the primary volume is lymph nodes draining lymph nodes are not targeted. Record
code 88 in the Phase II Radiation to Draining Lymph Nodes [1515]
• This data item may include converted historical values. It was converted from Radiation
Treatment Volume [1540] when Rad--Boost RX Modality [3200] was administered. Conversion
took place upon upgrade to NAACCR v18-compliant software; as of 2018 this data item is
required for all cases regardless of diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered
See STORE Manual 2018 for more information at https://www.facs.org/-/media/files/quality-
programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
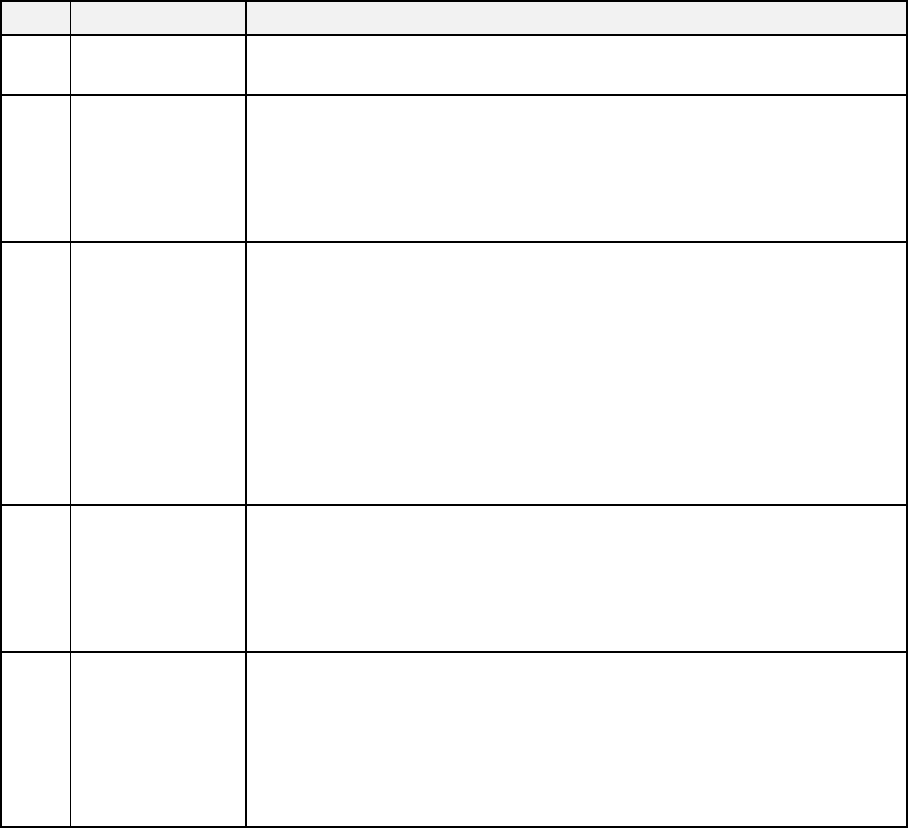
238
Phase II Radiation Primary Treatment Volume continued
Code
Definition
Description
00,
blank
No radiation
treatment
Radiation therapy not administered
01
Neck lymph node
regions
The primary treatment is directed at lymph node regions of the neck.
Examples include treatment of lymphoma or lymph node recurrence (in
the absence of primary site failure) following definitive surgery of the
primary tumor. If radiation to the neck lymph nodes includes the
supraclavicular region use code 03
02
Thoracic lymph
node regions
Radiation therapy is directed to some combination of hilar, mediastinal,
and supraclavical lymph nodes without concurrent treatment of a
visceral organ site. Examples include mantle or mini-mantle for
lymphomas, and treatment of lymphatic recurrence after complete
surgical excision of a thoracic primary. Note that the supraclavical
region may be part of a head and neck lymph node region. Use code 03
for treatments directed at neck nodes and supraclavicular lymph nodes
with a head and neck primary. Use code 04 if supraclavicular lymph
nodes are part of breast treatment
03
Neck and thoracic
lymph node
regions
Treatment is delivered to lymph nodes in the neck and thoracic region
without concurrent treatment of a primary visceral tumor. This code
might apply to some mantle or mini-mantle fields used in lymphoma
treatments or some treatments for lymphatic recurrences following
definitive treatment for tumors of the head and neck thoracic regions
04
Breast/Chest wall
lymph node
regions
Radiation is directed primarily to some combination of axillary,
supraclavicular, and/or internal mammary lymph node sites WITHOUT
concurrent treatment of the breast or chest wall. If the breast AND
lymph nodes are being treated, then code the Primary Treatment
Volume to Breast (codes 40 or 41) and Breast/chest wall lymph nodes
(code 04) in Radiation to Draining Lymph Nodes

239
Phase II Radiation Primary Treatment Volume continued
05
Abdominal lymph
nodes
Treatment is directed to some combination of the lymph nodes of the
abdomen, including retro-crural, peri-gastric, peri-hepatic, portocaval
and para-aortic nodes. Possible situations might include seminoma,
lymphoma or lymph node recurrence following surgical resection of the
prostate, bladder or uterus
06
Pelvic lymph
nodes
Treatment is directed to some combination of the lymph nodes of the
pelvis, including the common, internal and external iliac, obturator,
inguinal and peri-rectal lymph nodes. This might be done for lymphoma
or lymph node recurrence following definitive surgery for a pelvic organ
07
Abdominal and
pelvic lymph
nodes
Treatment is directed to a combination of lymph nodes in both the
abdomen and pelvis. This code includes extended fields ("hockey stick",
"dog-leg", "inverted Y", etc.) utilized to treat seminomas and
lymphomas or recurrence of a solid tumor
09
Lymph node
region NOS
This category should be used to code treatments directed at lymph
node regions that are not adequately described by codes 01-07
10
Eye/orbit/optic
nerve
Treatment is directed at all or a portion of the eye, orbit and/or optic
nerve
11
Pituitary
Treatment is directed at the pituitary gland.
12
Brain
Treatment is directed at all the brain and its meninges ("Whole brain")
13 Brain (limited)
Treatment is directed at one or more sub-sites of the brain but not the
whole brain. Chart may describe "SRS", "Stereotactic Radiosurgery",
"Gamma Knife®"
14 Spinal cord
Treatment is directed at all or a portion of the spinal cord or its
meninges
20
Nasopharynx
Treatment is directed at all or a portion of the nasopharynx
21 Oral cavity
Treatment is directed at all or a portion of the oral cavity, including the
lips, gingiva, alveolus, buccal mucosa, retromolar trigone, hard palate,
floor of mouth and oral tongue
22 Oropharynx
Treatment is directed at all or a portion of the oropharynx, including the
soft palate, tonsils, base of tongue and pharyngeal wall

240
Phase II Radiation Primary Treatment Volume continued
23
Larynx (glottis) or
hypopharynx
Treatment is directed at all or a portion of the larynx and/or
hypopharynx
24
Sinuses/Nasal
tract
Treatment is directed at all or a portion of the sinuses and nasal tract,
including the frontal, ethmoid, sphenoid and maxillary sinuses
25
Parotid or other
salivary glands
Treatment is directed at the parotid or other salivary glands, including
the submandibular, sublingual and minor salivary glands
26 Thyroid
Treatment is directed at all or a portion of the thyroid. Code this volume
when the thyroid is treated with I-131 radioisotope
29
Head and neck
(NOS)
The treatment volume is directed at a primary tumor of the head and
neck, but the primary sub-site is not a head and neck organ identified
by codes 20-26 or it is an "unknown primary"
30
Lung or bronchus
Treatment is directed at all or a portion of the lung or bronchus
31 Mesothelium
Treatment is directed to all or a portion of the mesothelium. This code
should be used for mesothelioma primaries, even if a portion of the
lung is included in the radiation field
32
Thymus
Treatment is directed to all or a portion of the thymus
39 Chest/lung (NOS)
The treatment is directed at a primary tumor of the chest, but the
primary sub-site is unknown or not identified in codes 30-32. For
example, this code should be used for sarcomas arising from the
mediastinum
40 Breast (whole)
Treatment is directed at all the intact breast. Intact breast includes
breast tissue that either was not surgically treated or received a
lumpectomy or partial mastectomy
41 Breast (partial)
Treatment is directed at a portion of the intact breast but not the whole
breast. The chart may have terms such as "Mammosite", "interstitial
(seed) implant)", or "(accelerated) partial breast irradiation". Consider
the possibility of partial breast irradiation when "IMRT" is documented
in the record
42
Chest wall
Treatment encompasses the chest wall (following mastectomy)
50 Esophagus
Treatment is directed at all or a portion of the esophagus. Include
tumors of the gastro-esophageal junction

241
Phase II Radiation Primary Treatment Volume continued
51
Stomach
Treatment is directed at all or a portion of the stomach
52
Small bowel
Treatment is directed at all or a portion of the small bowel
53
Colon
Treatment is directed at all or a portion of the colon
54
Rectum
Treatment is directed at all or a portion of the rectum
55
Anus
Treatment is directed at all or a portion of the anus.
56
Liver
Treatment is directed at all or a portion of the liver
57
Biliary tree or
gallbladder
Treatment is directed at all or a portion of the biliary tree or gallbladder
58
Pancreas or
hepatopancreatic
ampulla
Treatment is directed at all or a portion of the pancreas or the
hepatopancreatic ampulla. Hepatopancreatic ampulla tumors are
sometimes referred to as periampullary tumors
59 Abdomen (NOS)
The treatment volume is directed at a primary tumor of the abdomen,
but the primary sub-site is not an abdominal organ defined by codes 50-
58 or it is considered to be an "unknown primary". For example, this
code should be used for sarcomas arising from the abdominal
retroperitoneum.
60
Bladder (whole)
Treatment is directed at all the bladder
61 Bladder (partial)
Treatment is directed at a portion of the bladder but not the whole
bladder
62
Kidney
Treatment is directed at all or a portion of the kidney
63
Ureter
Treatment is directed at all or a portion of the ureter
64 Prostate (whole)
Treatment is directed at all the prostate and/or seminal vesicles. Use
this code even if seminal vesicles are not explicitly targeted
65 Prostate (partial)
Treatment is directed at a portion of the prostate but not the whole
prostate
66
Urethra
Treatment is directed at all or a portion of the urethra
67 Penis
Treatment is directed at all or a portion of the penis. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)

242
Phase II Radiation Primary Treatment Volume continued
68
Testicle or
scrotum
Treatment is directed at all or a portion of the testicle and/or scrotum
70
Ovaries or
fallopian tubes
Treatment is directed at all or a portion of the ovaries or fallopian tubes
71 Uterus or cervix
Treatment is directed at all or a portion of the uterus, endometrium or
cervix
72 Vagina
Treatment is directed at all or a portion of the vagina. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)
73 Vulva
Treatment is directed at all or a portion of the vulva. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)
80 Skull
Treatment is directed at all or a portion of the bones of the skull. Any
brain irradiation is a secondary consequence
81
Spine/vertebral
bodies
Treatment is directed at all or a portion of the bones of the
spine/vertebral bodies, including the sacrum. Spinal cord malignancies
should be coded using ‘spinal cord’ (code 14)
82 Shoulder
Treatment is directed to all or a portion of the proximal humerus,
scapula, clavicle, or other components of the shoulder complex
83
Ribs
Treatment is directed at all or a portion of one or more ribs
84 Hip
Treatment is directed at all or a portion of the proximal femur or
acetabulum
85 Pelvic bones
Treatment is directed at all or a portion of the bones of the pelvis other
than the hip or sacrum
86
Pelvis (NOS, non-
visceral)
The treatment volume is directed at a primary tumor of the pelvis, but
the primary sub-site is not a pelvic organ or is not known or indicated.
For example, this code should be used for sarcomas arising from the
pelvis
88
Extremity bone,
NOS
Treatment is directed at all or a portion of the bones of the arms or
legs. This excludes the proximal femur (Hip, code 84). This excludes the
proximal humerus (Shoulder, code 82)
90 Skin
Treatment is directed at all or a portion of the skin. The primary
malignancy originates in the skin and the skin is the primary target. So-
called skin metastases are usually subcutaneous and should be coded as
a soft tissue site

243
Phase II Radiation Primary Treatment Volume continued
91 Soft Tissue
This category should be used to code primary or metastatic soft tissue
malignancies not fitting other categories
92 Hemibody
A single treatment volume encompassing either all structures above the
diaphragm, or all structures below the diaphragm. This is almost always
administered for palliation of widespread bone metastasis in patients
with prostate or breast cancer
93
Whole body
Treatment is directed to the entire body included in a single treatment
94
Mantle, mini-
mantle (obsolete
after 2017)
For conversion of historic data only
95
Lower extended
field (obsolete
after 2017)
For conversion of historic data only.
97
Invalid historical
FORDS
value
Conversion to new STORE data item could not take place due to an
invalid
FORDS
Volume code
98 Other
Radiation therapy administered; treatment volume other than those
previously categorized by codes 01-93
99 Unknown
This category should be used to code treatments for which there is no
information available about the treatment volume, or it is unknown if
radiation treatment was administered
244
Phase II Radiation to Draining Lymph Nodes
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_RT_TO_LN
NAACCR Item #: 1515
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 08, 88, 99, blank
Description:
This is a new item in 2018. It was required in 2018, and optional in 2017. This item may
include historical converted historical values. For conversion of historical values this
data item includes a mapped value of 99 when Boost Treatment Modality (NAACCR Item
#3200) was administered. Blanks allowed if no Phase II radiation administered.
Identifies the draining lymph nodes treated (if any) during the second phase of radiation
therapy delivered to the patient during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018.
Rationale
The second phase of radiation treatment commonly targets both the primary tumor (or
tumor bed) and draining lymph nodes as a secondary site. This data item should be used
to indicate the draining regional lymph nodes, if any, that were irradiated during the
second phase of radiation to the primary site.
Registry Coding Instructions
• Radiation treatment to draining lymph nodes will typically be found in the radiation
oncologist’s summary letter for the first course of treatment. Determination of the exact
draining lymph nodes may require assistance from the radiation oncologist for
consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent
phase be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.
• The second phase of radiation treatment includes primary tumor or tumor bed in
addition to the draining lymph node regions that are associated with the primary tumor
or tumor bed. The primary tumor or tumor bed is recorded in the Phase II Radiation
Primary Treatment Volume [1514]. Note: When the Phase II Primary Treatment

245
Phase II Radiation to Draining Lymph Nodes continued
Volume is lymph nodes, draining lymph nodes are not targeted. Record code 88 in this
data item.
• This data item may include converted historical values. For conversion of historical
values, this data item includes a mapped value of 99 when Rad--Boost RX Modality
[3200] was administered. Conversion took place upon upgrade to NAACCR v18-
compliant software; as of 2018 this data item is required for all cases regardless of
diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None
Code
Definition
00, blank
No radiation to draining lymph nodes.
01
Neck lymph node regions
02
Thoracic lymph node regions
03
Neck and thoracic lymph node regions
04
Breast/ Chest wall lymph node regions
05
Abdominal lymph nodes
06
Pelvic lymph nodes
07
Abdominal and pelvic lymph nodes
08
Lymph node region, NOS
88
Not applicable; Radiation primary treatment is lymph nodes
99
Unknown if any radiation treatment to draining lymph nodes
246
Phase II Radiation Treatment Modality
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_RT_MODALITY
NAACCR Item #: 1516
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 16, 99, blank
Description:
This is a new data item, introduced in 2018. It was required in 2018, and optional in
2017. This data item, in conjunction with Phase II Radiation External Beam Planning
Technique (NAACCR Item # 1512), replaces the Boost Treatment Modality (NAACCR Item
#3200) and may include converted historical values.
Description
Identifies the radiation modality administered during the second phase of radiation
treatment delivered during the first course of treatment. This data item is required for
CoC-accredited facilities as of 01/01/2018.
Rationale
Radiation modality reflects whether a treatment was external beam, brachytherapy, a
radioisotope as well as their major subtypes, or a combination of modalities. This data
item should be used to indicate the radiation modality administered during the second
phase of radiation. Historically, the previously-named Radiation Treatment Modality
[1570] utilized codes that were not mutually exclusive. Rather, it included codes
describing a mix of modalities, treatment planning techniques, and delivery techniques
that are commonly utilized by radiation oncologists. However, every phase of radiation
treatment will include a specified modality, planning technique, and delivery technique.
The goal of the 2018 implementation of separate phase-specific data items for the
recording of radiation modality and external beam radiation treatment planning
techniques is to clarify this information and implement mutually exclusive categories. A
separate data item for delivery technique has not been implemented because this
information is not consistently reported in end of treatment summaries.
Registry Coding Instructions
• Radiation treatment modality will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Segregation of treatment components
into Phases and determination of the respective treatment modality may require
assistance from the radiation oncologist to ensure consistent coding.
247
Phase II Radiation Treatment Modality continued
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (I.e. dose given during a session), modality or treatment
technique. Any one of these changes will mean that a new radiation plan will be
generated in the treatment planning system, and it should be coded as a new phase of
radiation therapy.
• For purposes of this data item, photons, x-rays and gamma-rays are equivalent.
• Use code 13 - Radioisotopes, NOS for radioembolization procedures, e.g. intravascular
Yttrium-90.
• This data item intentionally does not include reference to various MV energies
because this is not a clinically important aspect of technique. A change in MV energy
(e.g., 6MV to 12MV) is not clinically relevant and does not represent a change in
treatment technique. It is rare for change in MV energy to occur during any phase of
radiation therapy.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system and should be coded as a new phase of
radiation therapy.
• If this data item is coded to any of the External beam codes (01-06), the planning
technique must be recorded in the data item Phase II External Beam Radiation Planning
Technique [1512]
• If this data item is coded to any of the Brachytherapy or Radioisotopes codes (07-16)
the code of 88 must be recorded in the data item Phase II External Beam Radiation
Planning Technique [1512].
Note: Do not confuse a radioiodine scan with treatment. Only treatment is recorded in
this item.
• This data item, in conjunction with Phase II Radiation External Beam Planning
Technique [1512], replaces the Rad--Boost RX Modality [3200] and may include
converted historical values. Conversion took place upon upgrade to NAACCR v18-
compliant software; as of 2018 this data item is required for all cases regardless of
diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered

248
Phase II Radiation Treatment Modality continued
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
00, blank
No radiation treatment
01
External beam, NOS
02
External beam, photons
03
External beam, protons
04
External beam, electrons
05
External beam, neutrons
06
External beam, carbon ions
07
Brachytherapy, NOS
08
Brachytherapy, intracavitary, LDR
09
Brachytherapy, intracavitary, HDR
10
Brachytherapy, interstitial, LDR
11
Brachytherapy, interstitial, HDR
12
Brachytherapy, electronic
13
Radioisotopes, NOS
14
Radioisotopes, Radium-223
15
Radioisotopes, Strontium-89
16
Radioisotopes, Strontium-90
98
Radiation Rx administered, Rx modality
unknown
99
Radiation treatment modality unknown;
Unknown if radiation treatment
administered
249
Phase II External Beam Radiation Planning Technique
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_BEAM_TECH
NAACCR Item #: 1512
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 10, 88, 98, 99, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This item, in
conjunction with Phase II Radiation Treatment Modality (NAACCR Item #1516), replaces
the Boost Treatment Modality (NAACCR Item #3200) and may include converted
historical values.
Identifies the external beam radiation planning technique used to administer the second
phase of radiation treatment during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018.
Rationale
External beam radiation is the most commonly-used radiation modality in North
America. In this data item we specified the planning technique for external beam
treatment. Identifying the radiation technique is of interest for patterns of care and
comparative effectiveness studies. Historically, the previously-named Regional
Treatment Modality [3200] utilized codes that were not mutually exclusive. Rather, it
included codes describing a mix of modalities, treatment planning techniques, and
delivery techniques that are commonly utilized by radiation oncologists. However, every
phase of radiation treatment will include a specified modality, planning technique, and
delivery technique. The goal of the 2018 implementation of separate phase-specific data
items for the recording of Phase II Radiation Treatment Modality [1516] and Phase II
External Beam Radiation Planning Technique [1512] is to clarify this information and
implement mutually exclusive categories. Note that Planning Technique details are not
being captured for non-External Beam modalities. A separate data item for delivery
technique has not been implemented because this information is not consistently
reported in end treatment summaries.
Registry Coding Instructions
• Radiation external beam treatment planning technique will typically be found in the
radiation oncologist’s summary letter for the first course of treatment.
250
Phase II External Beam Radiation Planning Technique
• Determination of the external beam planning technique may require assistance
from the radiation oncologist to ensure consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase
II, Phase III, etc. accordingly.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment technique.
Any one of these changes will generally mean that a new radiation plan will be generated in
the treatment planning system and should be coded as a new phase of radiation therapy.
• Note: “on-line adaptive therapy” refers to treatments where radiation treatment
plans are adapted or updated while a patient is on the treatment table. When
treatment plans are adapted, the shape of the target volume may change from day
to day but, for registry purposes, the volume that is being targeted won’t change.
An adapted plan should not be coded as though a new phase of treatment has been
initiated unless, as above, the radiation oncologist documents it as a new phase in
the radiation treatment summary. Two new technique codes have been added to
capture when online adaptive therapy is occurring: CT guided and MR guided
adaptive therapy.
Code 05 for Intensity Modulated Therapy (IMT) or Intensity Modulated Radiation
Therapy (IMRT).
• Code 04 for Conformal or 3-D Conformal Therapy whenever either is explicitly
mentioned.
• When code 98 is recorded, document the planning technique in the appropriate text
data item.
• This data item, in conjunction with Phase II Radiation Treatment Modality [1516],
replaces the Rad-- Boost RX Modality [3200] and may include converted historical
values. Conversion took place upon upgrade to NAACCR v18-compliant software; as of
2018 this data item is required for all cases regardless of diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

251
Phase II External Beam Radiation Planning Technique
Code
Definition
Description
00,
blank
No radiation
treatment
Radiation therapy was not administered to the patient
01
External beam,
NOS
The treatment is known to be by external beam, but there is insufficient
information to determine the specific planning technique
02
Low energy x-
ray/photon
therapy
External beam therapy administered using equipment with a maximum
energy of less than one (1) million volts (MV). Energies are typically
expressed in units of kilovolts (kV). These types of treatments are
sometimes referred to as electronic brachytherapy or orthovoltage or
superficial therapy. Clinical notes may refer to the brand names of low
energy x-ray delivery devices, e.g. Axxent®, INTRABEAM®, or Esteya®
03 2-D therapy
An external beam planning technique using 2-D imaging, such as plain film
x-rays or fluoroscopic images, to define the location and size of the
treatment beams. Should be clearly described as 2-
D therapy. This planning
modality is typically used only for palliative treatments
04
Conformal or 3-
D conformal
therapy
An external beam planning technique using multiple, fixed beams shaped
to conform to a defined target volume. Should be clearly described as
conformal or 3-D therapy in patient record
05
Intensity
modulated
therapy
An external beam planning technique where the shape or energy of beams
is optimized using software algorithms. Any external beam modality can be
modulated but these generally refer to photon or proton beams. Intensity
modulated therapy can be described as intensity modulated radiation
therapy (IMRT), intensity modulated xray or proton therapy (IMXT/IMPT),
volumetric arc therapy (VMAT) and other ways. If a treatment is described
as IMRT with online reoptimization/re-planning, then it should be
categorized as online reoptimization or re-planning

252
Phase II External Beam Radiation Planning Technique
06
Stereotactic
radiotherapy or
radiosurgery,
NOS
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques, but the treatment is not described as Cyberknife® or Gamma
Knife®. These approaches are sometimes described as SBRT (stereotactic
body radiation), SABR (stereotactic ablative radiation), SRS (stereotactic
radiosurgery), or SRT (stereotactic radiotherapy). If the treatment is
described as robotic radiotherapy (e.g. Cyberknife®) or Gamma Knife®, use
stereotactic radiotherapy subcodes below. If a treatment is described as
stereotactic radiotherapy or radiosurgery with online re-optimization/re-
planning, then it should be categorized as online re-optimization or re-
planning
07
Stereotactic
radiotherapy or
radiosurgery,
robotic
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques which is specifically described as robotic (e.g. Cyberknife®)
08
Stereotactic
radiotherapy or
radiosurgery,
Gamma Knife®
Treatment planning using stereotactic radiotherapy/radiosurgery
techniques which uses a Cobalt-60 gamma ray source and is specifically
described as Gamma Knife®. This is most commonly used for treatments in
the brain
09
CT-guided
online adaptive
therapy
An external beam technique in which the treatment plan is adapted over
the course of radiation to reflect changes in the patient’s tumor or normal
anatomy radiation using a CT scan obtained at the treatment machine
(online). These approaches are sometimes described as CT-guided online
re-optimization or online re-planning. If a treatment technique is described
as both CT-guided online adaptive therapy as well as another external
beam technique (IMRT, SBRT, etc.), then it should be categorized as CT-
guided online adaptive therapy. If a treatment is described as “adaptive”
but does not include the descriptor “online”, this code should not be used
10
MR-guided
online adaptive
therapy
An external beam technique in which the treatment plan is adapted over
the course of radiation to reflect changes in the patient’s tumor or normal
anatomy radiation using an MRI scan obtained at the treatment machine
(online). These approaches are sometimes described as MR-guided online
re-optimization or online re-planning. If a treatment technique is described
as both MR-guided online adaptive therapy as well as another external
beam technique (IMRT, SBRT, etc.), then it should be categorized as MR-
guided online adaptive therapy. If a treatment is described as “adaptive”
but does not include the descriptor “online”, this code should not be used
253
Phase II External Beam Radiation Planning Technique
88
Not applicable
Treatment not by external beam
98 Other, NOS
Other radiation, NOS; Radiation therapy administered, but the treatment
modality is not specified or known
99
Unknown
It is unknown whether radiation therapy was administered
254
Phase II Dose per Fraction
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_DOSE_FRACT
NAACCR Item #: 1511
Diagnosis Years Available: 2004 +
Length: 5
Allowable Values: 00000 - 99999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This data
item replaces the Rad--Boost Dose cGy [3210] and may include mapped values for
historical cases.
Records the dose per fraction (treatment session) delivered to the patient in the second
phase of radiation during the first course of treatment. The unit of measure is centi-Gray
(cGy). This data item is required for CoC-accredited facilities as of 01/01/2018. Rationale
Radiation therapy is delivered in one or more phases with identified dose per fraction. It
is necessary to capture information describing the dose per fraction to evaluate patterns
of radiation oncology care. Outcomes are strongly related to the dose delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording
doses at the axis point where applicable (opposed fields, four field box, wedged pair,
and so on). For maximum consistency in this data item, the ICRP recommendations
should be followed whenever possible. Where there is no clear axis point, record the
total dose as indicated in the summary chart. Determining the exact dose may require
assistance from the radiation oncologist for consistent coding.
• Radiation treatment Phase II dose will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the Phase II dose of
radiation therapy may require assistance from the radiation oncologist for consistent
coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred as a boost or cone down, and would be recorded as Phase II, Phase III,
etc. accordingly.
• Record the actual dose delivered (NOT the initially prescribed dose) as documented in
the treatment summary.

255
Phase II Dose per Fraction continued
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt
Gray Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase I Total Dose, you would
need to multiply cGe by 100). o Note that dose is still occasionally specified in “rads”.
One rad is equivalent to one centiGray (cGy).
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• Code 99998 when radioisotopes were administered to the patient (codes 13-16 for
Phase II Radiation Treatment Modality [1516]).
• This data item replaces the Rad--Boost Dose cGy [3210] and may include mapped
values for historical cases. 1-1 mapping took place upon upgrade to NAACCR v18-
compliant software; as of 2018 this data item is required for all cases regardless of
diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
00000, blank
No radiation treatment
00001-99997
Record the actual Phase II dose delivered in cGy
99998
Not applicable, radioisotopes administered to the patient
99999
Phase II (Boost) radiation therapy was administered but dose is
unknown; it is unknown whether Phase II radiation therapy was
administered

256
Phase II Dose Per Fraction continued
Examples
Code
Reason
00200
A patient with Stage III prostate carcinoma
receives pelvic irradiation to 5,000 cGy in 25
fractions followed by a conformal prostate boost
to 7,000 cGy in 10 additional fractions. Record
the prescribed (and delivered) Phase II dose per
fractions as 00200 (2000/10)
Blank
A patient with a left supraclavicular metastasis
from a gastric carcinoma receives 6,000 cGy to
the left supraclavicular region. The dose is
calculated at a prescribed depth of 3 cm. A
secondary calculation shows a D max dose (dose
at depth of maximum dose) of 6,450 cGy. Do not
confuse D max doses with Phase II doses. In this
case, there is no planned Phase II dose. Leave
Phase II Dose per Fraction blank.
99999
A patient with a Stage II breast carcinoma is
treated with the breast intact. Tangent fields are
utilized to bring the central axis dose in the breast
to 5,040 cGy encompassing the supraclavicular
nodes, and an intracavitary boost in the primary
tumor bed is delivered to a small volume in the
breast in a single session. Record the Phase II
dose per fraction as 99999. Dosage
(brachytherapy) unknown.
257
Phase II Number of Fractions
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_NUM_FRACT
NAACCR Item #: 1513
Diagnosis Years Available: 2004 +
Length: 3
Allowable Values: 000 - 999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This data item
may include mapped values for historical cases. This data item includes a mapped value
of 999 when Boost Treatment Modality (NAACCR Item #3200) was administered.
Description
Records the total number of fractions (treatment sessions) administered to the patient
in the second phase of radiation during the first course of treatment. This data item is
required for CoC-accredited facilities as of 01/01/2018. Rationale Radiation therapy is
delivered in one or more phases with each phase spread out over a number of fractions
(treatment sessions). It is necessary to capture information describing the number of
fraction(s) to evaluate patterns of radiation oncology care.
Registry Coding Instructions
• The number of fractions or treatments will typically be found in the radiation
oncologist’s summary letter for the first course of treatment. Determination of the exact
number of treatments or fractions delivered to the patient may require assistance from
the radiation oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.
• Although a fraction or treatment session may include several treatment portals
delivered within a relatively confined period of time-usually a few minutes-it is still
considered one session.
• Count each separate administration of brachytherapy or implants as a single fraction
or treatment.
• Record the actual number of fractions delivered (NOT initially prescribed), as
documented in the treatment summary.

258
Phase II Number of Fractions continued
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• This data item may include mapped values for historical cases. This data item includes
a mapped value of 999 when Rad--Boost RX Modality [3200] was administered. Mapping
took place upon upgrade to NAACCR v18-compliant software; as of 2018 this data item
is required for all cases regardless of diagnosis year.
• Blanks allowed if no Phase II radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000, blank
No radiation treatment
001-998
Number of fractions administered to the patient during the second phase of radiation
therapy
999
Phase II Radiation therapy was administered, but the number of fractions is
unknown; It is unknown whether radiation therapy was administered

259
Phase II Number of Fractions continued
Examples
Code
Reason
005
A patient with breast carcinoma had treatment sessions in which treatment was delivered to
the chest wall encompassing the ipsilateral supraclavicular region for a total of three fraction
portals. Twenty-five treatment sessions were given. Additional 1000 cGy external beam boost
to the tumor bed given in 5 fractions. Code 005 for 5 fractions for phase II.
Blank
A patient with Stage IIIB bronchogenic carcinoma received 25 treatments to the left hilum and
mediastinum, given in 25 daily fractions over five weeks. No Phase II treatment, leave blank.
010
A patient with advanced head and neck cancer was treated with 6000 cGy in 25 fractions
encompassing the primary site and draining nodes with a boost of 1200 cGy in 10 fractions to
the tumor bed. Record 010 for 10 fractions for phase II.
005
The patient was given a course of external beam to the prostate followed by 5 HDR
brachytherapy treatments. Record 005 for 5 fractions for phase II.
030
Prostate cancer patient treated with a single administration of seeds followed by 4500 cGy
IMRT in 30 fractions. Code 030 for 30 fractions for phase II.
260
Phase II Total Dose
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_II_TOTAL_DOSE
NAACCR Item #: 1517
Diagnosis Years Available: 2004 +
Length: 6
Allowable Values: 000000 - 999999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017. This data
item may include mapped values for historical cases. This data item includes a mapped
value of 999999 when Boost Treatment Modality (NAACCR Item #3200) was
administered.
Description
Identifies the total radiation dose administered in the second phase of radiation
treatment delivered to the patient during the first course of treatment. The unit of
measure is centi-Gray (cGy). This data item is required for CoC-accredited facilities as of
01/01/2018.
Rationale
To evaluate the patterns of radiation care, it is necessary to capture information
describing the prescribed dose of Phase II radiation to the patient during the first course
of treatment. Outcomes are strongly related to the total dose delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording
doses at the axis point where applicable (opposed fields, four field box, wedged pair,
and so on). For maximum consistency in this data item, the ICRP recommendations
should be followed whenever possible. Where there is no clear axis point, record the
total dose as indicated in the summary chart. Determining the exact dose may be highly
subjective and require assistance from the radiation oncologist for consistent coding.
• Phase II radiation treatment dose will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the Phase II dose of
radiation therapy may require assistance from the radiation oncologist for consistent
coding.

261
Phase II Total Dose continued
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.
• Record the actual total dose delivered (NOT initially prescribed), as documented in the
treatment summary. The value recorded for this data item should NOT be auto-
calculated within the registry abstraction software.
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt
Gray Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase II Total Dose, you
would need to multiply cGe by 100).
• Note that dose is still occasionally specified in “rads”. One rad is equivalent to one
centi-Gray (cGy).
• Code 999998 when radioisotopes are administered to the patient (codes 13-16
recorded in the Phase II Treatment Modality [1516]).
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• This data item may include mapped values for historical cases. This data item includes
a mapped value of 999999 when Rad--Boost RX Modality [3200] was administered.
Mapping took place upon STORE 2018 Phase II Total Dose
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000000, blank
No radiation treatment
000001-999997
Record the actual dose delivered in cGy
999998
Not applicable, radioisotopes administered to the patient
999999
Radiation therapy was administered, but the total dose is unknown;
it is unknown whether radiation therapy was administered

262
Phase II Total Dose continued
Examples
Code
Reasons
005000
A patient with Stage III prostate carcinoma received pelvic irradiation of 5,000 cGy during
Phase II Radiation Treatment. Record the Phase II Total Dose of 5,000 cGy as 005000.
006000
A patient with a left supraclavicular metastasis from a gastric carcinoma received 6,000 cGy
to the left supraclavicular region during Phase II Radiation Treatment. Record the Phase II
Total Dose of 6,000 cGy as 006000.
005500
A patient with a Stage II breast carcinoma is treated with the breast intact. During Phase II
treatment tangent fields are utilized to bring the dose of the breast to 5,500 cGy. The
supraclavicular (draining) lymph nodes are treated 4,500 cGy, calculated to a depth of 3 cm.
Record the Phase II Total Dose of 5,500cGy as 005500.
263
Phase III Radiation Primary Treatment Volume
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_RT_VOLUME
NAACCR Item #: 1524
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 07, 09 - 14, 20 - 26, 29 - 32, 39 - 42, 50 - 58, 60 - 68, 70 - 73, 80 - 86, 88, 90 - 95,
96 - 99, blank
Description:
This is a new item in 2018. It was required in 2018 and optional in 2018.
Description
Identifies the primary treatment volume or primary anatomic target treated during the
third phase of radiation therapy during the first course of treatment. This data item is
required for CoC-accredited facilities for cases diagnosed 01/01/2018 and later.
Rationale
Radiation treatment is commonly delivered in one or more phases. Typically, in each
phase, the primary tumor or tumor bed is treated. This data item should be used to
indicate the primary target volume, which might include the primary tumor or tumor
bed. If the primary tumor was not targeted, record the other regional or distant site that
was targeted. Draining lymph nodes may also be targeted during the first phase. These
will be identified in a separate data item Phase III Radiation to Draining Lymph Nodes
[1525]. This data item provides information describing the anatomical structure
targeted by radiation therapy during the third phase of radiation treatment and can be
used to determine whether the site of the primary disease was treated with radiation or
if other regional or distant sites were targeted. This information is useful in evaluating
the patterns of care within a facility and on a regional or national basis. The breakdown
and reorganization of the sites will allow for concise reporting.
Registry Coding Instructions
• Radiation treatment volume will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the exact treatment
volume may require assistance from the radiation oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent
phase may be referred to as a boost or cone down, and would be recorded as Phase II,
Phase III, etc. accordingly.
264
Phase III Radiation Primary Treatment Volume continued
• If one or more discrete volumes are treated and one of those includes the primary
site, record the treatment to the primary site in this data item.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system, and it should be coded as a new phase
of radiation therapy.
Note: “on-line adaptive therapy” refers to treatments where radiation treatment plans
are adapted or updated while a patient is on the treatment table. When treatment plans
are adapted, the shape of the target volume may change from day to day, but for
registry purposes, the volume that is being targeted won’t change. An adapted plan
should not be coded as though a new phase of treatment has been initiated unless, as
above, the radiation oncologist documents it as a new phase in the radiation treatment
summary.
• Phase III of radiation treatment also commonly includes draining lymph node regions
that are associated with the primary tumor or tumor bed. The draining lymph nodes are
recorded in the Phase III Radiation to Draining Lymph Nodes [1525].
Note: When the Primary Treatment Volume is lymph nodes draining lymph nodes are
not targeted. Record code 88 in the Phase III Radiation to Draining Lymph Nodes [1525].
• Blanks allowed if no Phase II radiation treatment administered
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

265
Phase III Radiation Primary Treatment Volume continued
Code
Definition
Description
00,
blank
No radiation
treatment
Radiation therapy not administered
01
Neck lymph node
regions
The primary treatment is directed at lymph node regions of the neck.
Examples include treatment of lymphoma or lymph node recurrence (in
the absence of primary site failure) following definitive surgery of the
primary tumor. If radiation to the neck lymph nodes includes the
supraclavicular region use code 03
02
Thoracic lymph
node regions
Radiation therapy is directed to some combination of hilar, mediastinal,
and supraclavical lymph nodes without concurrent treatment of a
visceral organ site. Examples include mantle or mini-mantle for
lymphomas, and treatment of lymphatic recurrence after complete
surgical excision of a thoracic primary. Note that the supraclavical
region may be part of a head and neck lymph node region. Use code 03
for treatments directed at neck nodes and supraclavicular lymph nodes
with a head and neck primary. Use code 04 if supraclavicular lymph
nodes are part of breast treatment
03
Neck and thoracic
lymph node
regions
Treatment is delivered to lymph nodes in the neck and thoracic region
without concurrent treatment of a primary visceral tumor. This code
might apply to some mantle or mini-mantle fields used in lymphoma
treatments or some treatments for lymphatic recurrences following
definitive treatment for tumors of the head and neck thoracic regions
04
Breast/Chest wall
lymph node
regions
Radiation is directed primarily to some combination of axillary,
supraclavicular, and/or internal mammary lymph node sites WITHOUT
concurrent treatment of the breast or chest wall. If the breast AND
lymph nodes are being treated, then code the Primary Treatment
Volume to Breast (codes 40 or 41) and Breast/chest wall lymph nodes
(code 04) in Radiation to Draining Lymph Nodes
05
Abdominal lymph
nodes
Treatment is directed to some combination of the lymph nodes of the
abdomen, including retro-crural, peri-gastric, peri-hepatic, portocaval
and para-aortic nodes. Possible situations might include seminoma,
lymphoma or lymph node recurrence following surgical resection of the
prostate, bladder or uterus

266
Phase III Radiation Primary Treatment Volume continued
06
Pelvic lymph
nodes
Treatment is directed to some combination of the lymph nodes of the
pelvis, including the common, internal and external iliac, obturator,
inguinal and peri-rectal lymph nodes. This might be done for lymphoma
or lymph node recurrence following definitive surgery for a pelvic organ
07
Abdominal and
pelvic lymph
nodes
Treatment is directed to a combination of lymph nodes in both the
abdomen and pelvis. This code includes extended fields ("hockey stick",
"dog-leg", "inverted Y", etc.) utilized to treat seminomas and
lymphomas or recurrence of a solid tumor
09
Lymph node
region NOS
This category should be used to code treatments directed at lymph
node regions that are not adequately described by codes 01-07
10
Eye/orbit/optic
nerve
Treatment is directed at all or a portion of the eye, orbit and/or optic
nerve
11
Pituitary
Treatment is directed at the pituitary gland
12
Brain
Treatment is directed at all the brain and its meninges ("Whole brain")
13 Brain (limited)
Treatment is directed at one or more sub-sites of the brain but not the
whole brain. Chart may describe "SRS", "Stereotactic Radiosurgery",
"Gamma Knife®"
14 Spinal cord
Treatment is directed at all or a portion of the spinal cord or its
meninges
20
Nasopharynx
Treatment is directed at all or a portion of the nasopharynx
21 Oral cavity
Treatment is directed at all or a portion of the oral cavity, including the
lips, gingiva, alveolus, buccal mucosa, retromolar trigone, hard palate,
floor of mouth and oral tongue
22 Oropharynx
Treatment is directed at all or a portion of the oropharynx, including the
soft palate, tonsils, base of tongue and pharyngeal wall
23
Larynx (glottis) or
hypopharynx
Treatment is directed at all or a portion of the larynx and/or
hypopharynx
24
Sinuses/Nasal
tract
Treatment is directed at all or a portion of the sinuses and nasal tract,
including the frontal, ethmoid, sphenoid and maxillary sinuses
25
Parotid or other
salivary glands
Treatment is directed at the parotid or other salivary glands, including
the submandibular, sublingual and minor salivary glands

267
Phase III Radiation Primary Treatment Volume continued
26 Thyroid
Treatment is directed at all or a portion of the thyroid. Code this volume
when the thyroid is treated with I-131 radioisotope
29
Head and neck
(NOS)
The treatment volume is directed at a primary tumor of the head and
neck, but the primary sub-site is not a head and neck organ identified
by codes 20-26 or it is an "unknown primary"
30
Lung or bronchus
Treatment is directed at all or a portion of the lung or bronchus
31 Mesothelium
Treatment is directed to all or a portion of the mesothelium. This code
should be used for mesothelioma primaries, even if a portion of the
lung is included in the radiation field
32
Thymus
Treatment is directed to all or a portion of the thymus
39 Chest/lung (NOS)
The treatment is directed at a primary tumor of the chest, but the
primary sub-site is unknown or not identified in codes 30-32. For
example, this code should be used for sarcomas arising from the
mediastinum
40 Breast (whole)
Treatment is directed at all the intact breast. Intact breast includes
breast tissue that either was not surgically treated or received a
lumpectomy or partial mastectomy
41 Breast (partial)
Treatment is directed at a portion of the intact breast but not the whole
breast. The chart may have terms such as "Mammosite", "interstitial
(seed) implant)", or "(accelerated) partial breast irradiation". Consider
the possibility of partial breast irradiation when "IMRT" is documented
in the record
42
Chest wall
Treatment encompasses the chest wall (following mastectomy)
50 Esophagus
Treatment is directed at all or a portion of the esophagus. Include
tumors of the gastro-esophageal junction
51
Stomach
Treatment is directed at all or a portion of the stomach
52
Small bowel
Treatment is directed at all or a portion of the small bowel
53
Colon
Treatment is directed at all or a portion of the colon.
54
Rectum
Treatment is directed at all or a portion of the rectum
55
Anus
Treatment is directed at all or a portion of the anus

268
Phase III Radiation Primary Treatment Volume continued
56
Liver
Treatment is directed at all or a portion of the liver
57
Biliary tree or
gallbladder
Treatment is directed at all or a portion of the biliary tree or gallbladder
58
Pancreas or
hepatopancreatic
ampulla
Treatment is directed at all or a portion of the pancreas or the
hepatopancreatic ampulla. Hepatopancreatic ampulla tumors are
sometimes referred to as periampullary tumors
59 Abdomen (NOS)
The treatment volume is directed at a primary tumor of the abdomen,
but the primary sub-site is not an abdominal organ defined by codes 50-
58 or it is considered to be an "unknown primary". For example, this
code should be used for sarcomas arising from the abdominal
retroperitoneum.
60
Bladder (whole)
Treatment is directed at all the bladder
61 Bladder (partial)
Treatment is directed at a portion of the bladder but not the whole
bladder
62
Kidney
Treatment is directed at all or a portion of the kidney
63
Ureter
Treatment is directed at all or a portion of the ureter
64 Prostate (whole)
Treatment is directed at all the prostate and/or seminal vesicles. Use
this code even if seminal vesicles are not explicitly targeted
65 Prostate (partial)
Treatment is directed at a portion of the prostate but not the whole
prostate
66
Urethra
Treatment is directed at all or a portion of the urethra
67 Penis
Treatment is directed at all or a portion of the penis. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)
68
Testicle or
scrotum
Treatment is directed at all or a portion of the testicle and/or scrotum
70
Ovaries or
fallopian tubes
Treatment is directed at all or a portion of the ovaries or fallopian tubes
71 Uterus or cervix
Treatment is directed at all or a portion of the uterus, endometrium or
cervix

269
Phase III Radiation Primary Treatment Volume continued
72 Vagina
Treatment is directed at all or a portion of the vagina. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)
73 Vulva
Treatment is directed at all or a portion of the vulva. Treatments of
urethral primaries should be coded as ‘urethra’ (code 66)
80 Skull
Treatment is directed at all or a portion of the bones of the skull. Any
brain irradiation is a secondary consequence
81
Spine/vertebral
bodies
Treatment is directed at all or a portion of the bones of the
spine/vertebral bodies, including the sacrum. Spinal cord malignancies
should be coded using ‘spinal cord’ (code 14)
82 Shoulder
Treatment is directed to all or a portion of the proximal humerus,
scapula, clavicle, or other components of the shoulder complex
83
Ribs
Treatment is directed at all or a portion of one or more ribs
84 Hip
Treatment is directed at all or a portion of the proximal femur or
acetabulum
85 Pelvic bones
Treatment is directed at all or a portion of the bones of the pelvis other
than the hip or sacrum
86
Pelvis (NOS, non-
visceral)
The treatment volume is directed at a primary tumor of the pelvis, but
the primary sub-site is not a pelvic organ or is not known or indicated.
For example, this code should be used for sarcomas arising from the
pelvis
88
Extremity bone,
NOS
Treatment is directed at all or a portion of the bones of the arms or
legs. This excludes the proximal femur (Hip, code 84). This excludes the
proximal humerus (Shoulder, code 82)
90 Skin
Treatment is directed at all or a portion of the skin. The primary
malignancy originates in the skin and the skin is the primary target. So-
called skin metastases are usually subcutaneous and should be coded as
a soft tissue site
91 Soft Tissue
This category should be used to code primary or metastatic soft tissue
malignancies not fitting other categories

270
Phase III Radiation Primary Treatment Volume continued
92 Hemibody
A single treatment volume encompassing either all structures above the
diaphragm, or all structures below the diaphragm. This is almost always
administered for palliation of widespread bone metastasis in patients
with prostate or breast cancer
93
Whole body
Treatment is directed to the entire body included in a single treatment
94
Mantle, mini-
mantle (obsolete
after 2017)
For conversion of historic data only
95
Lower extended
field (obsolete
after 2017)
For conversion of historic data only.
97
Invalid historical
FORDS
value
Conversion to new STORE data item could not take place due to an
invalid
FORDS
Volume code
98 Other
Radiation therapy administered; treatment volume other than those
previously categorized by codes 01-93
99 Unknown
This category should be used to code treatments for which there is no
information available about the treatment volume, or it is unknown if
radiation treatment was administered
271
Phase III Radiation to Draining Lymph Nodes
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_RT_TO_LN
NAACCR Item #: 1525
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 08, 88, 99, blank
Description: This is a new item in 2018. It was required in 2018, and optional in 2017.
Description
Identifies the draining lymph nodes treated (if any) during the third phase of radiation therapy
delivered to the patient during the first course of treatment. This data item is required for CoC-
accredited facilities for cases diagnosed 01/01/2018 and later.
Rationale
The third phase of radiation treatment commonly targets both the primary tumor (or tumor bed) and
draining lymph nodes as a secondary site. This data item should be used to indicate the draining regional
lymph nodes, if any, that were irradiated during the third phase of radiation to the primary site.
Registry Coding Instructions:
• Radiation treatment to draining lymph nodes will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the exact draining lymph nodes may
require assistance from the radiation oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase may be
referred to as a boost or cone down, and would be recorded as Phase II, Phase III, etc. accordingly.
• Phase III of radiation treatment includes primary tumor or tumor bed in addition to the draining lymph
node regions that are associated with the primary tumor or tumor bed. The primary tumor or tumor bed
is recorded in the Phase III Radiation Primary Treatment Volume [1524].
Note: When the Primary Treatment Volume is lymph nodes, draining lymph nodes are not targeted.
Record code 88 in this data item.
• Blanks allowed if no Phase III radiation treatment administered
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

272
Phase III Radiation to Draining Lymph Nodes continued
Code
Definition
00, blank
No radiation to draining lymph nodes.
01
Neck lymph node regions
02
Thoracic lymph node regions
03
Neck and thoracic lymph node regions
04
Breast/ Chest wall lymph node regions
05
Abdominal lymph nodes
06
Pelvic lymph nodes
07
Abdominal and pelvic lymph nodes
08
Lymph node region, NOS
88
Not applicable; Radiation primary treatment is lymph nodes
99
Unknown if any radiation treatment to draining lymph
nodes; Unknown if radiation treatment administered
273
Phase III Radiation Treatment Modality
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_RT_MODALITY
NAACCR Item #: 1526
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 16, 99, blank
Description:
This is a new data item, introduced in 2018. It was required in 2018, and optional in
2017.
Identifies the radiation modality administered during the third phase of radiation
treatment delivered during the first course of treatment. This data item is required for
CoC-accredited facilities for cases diagnosed 01/01/2018 and later.
Rationale
Radiation modality reflects whether a treatment was external beam, brachytherapy, a
radioisotope as well as their major subtypes, or a combination of modalities. This data
item should be used to indicate the radiation modality administered during the third
phase of radiation. Historically, the previously-named Radiation Treatment Modality
[1570] utilized codes that were not mutually exclusive. Rather, it included codes
describing a mix of modalities, treatment planning techniques, and delivery techniques
that are commonly utilized by radiation oncologists. However, every phase of radiation
treatment will include a specified modality, planning technique, and delivery technique.
The goal of the 2018 implementation of separate phase-specific data items for the
recording of radiation modality and external beam radiation treatment planning
techniques is to clarify this information and implement mutually exclusive categories. A
separate data item for delivery technique has not been implemented because this
information is not consistently reported in end of treatment summaries.
Registry Coding Instructions
• Radiation treatment modality will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Segregation of treatment components
into Phases and determination of the respective treatment modality may require
assistance from the radiation oncologist to ensure consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.
274
Phase III Radiation Treatment Modality continued
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (I.e. dose given during a session), modality or treatment
technique. Any one of these changes will mean that a new radiation plan will be
generated in the treatment planning system, and it should be coded as a new phase of
radiation therapy.
• For purposes of this data item, photons, x-rays and gamma-rays are equivalent.
• Use code 13 - Radioisotopes, NOS for radioembolization procedures, e.g. intravascular
Yttrium-90.
• This data item intentionally does not include reference to various MV energies
because this is not a clinically important aspect of technique. A change in MV energy
(e.g., 6MV to 12MV) is not clinically relevant and does not represent a change in
treatment technique. It is rare for change in MV energy to occur during any phase of
radiation therapy.
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system and should be coded as a new phase of
radiation therapy.
If this data item is coded to any of the External beam codes (01-06), the planning
technique must be recorded in the data item Phase III External Beam Radiation Planning
Technique [1522].
• If this data item is coded to any of the radioisotopes codes (13-16) the code of 88 must
be recorded in the data item Phase III External Beam Radiation Planning Technique
[1522]. o Note: Do not confuse a radioiodine scan with treatment. Only treatment is
recorded in this item.
• Blanks allowed if no Phase III radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx..
Analytic Note: None.

275
Phase III Radiation Primary Treatment Volume continued
Code
Definition
00, blank
No radiation treatment
01
External beam, NOS
02
External beam, photons
03
External beam, protons
04
External beam, electrons
05
External beam, neutrons
06
External beam, carbon ions
07
Brachytherapy, NOS
08
Brachytherapy, intracavitary, LDR
09
Brachytherapy, intracavitary, HDR
10
Brachytherapy, interstitial, LDR
11
Brachytherapy, interstitial, HDR
12
Brachytherapy, electronic
13
Radioisotopes, NOS
14
Radioisotopes, Radium-223
15
Radioisotopes, Strontium-89
16
Radioisotopes, Strontium-90
98
Radiation Rx administered, Rx modality
unknown
99
Radiation treatment modality unknown;
Unknown if radiation treatment
administered
276
Phase III External Beam Radiation Planning Technique
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_BEAM_TECH
NAACCR Item #: 1522
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 10, 88, 98, 99, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017.
Identifies the external beam radiation planning technique used to administer the third
phase of radiation treatment during the first course of treatment. This data item is
required for CoC-accredited facilities for cases diagnosed 01/01/2018 and later.
Rationale External beam radiation is the most commonly-used radiation modality in
North America. In this data item we specified the planning technique for external beam
treatment. Identifying the radiation technique is of interest for patterns of care and
comparative effectiveness studies. Historically, the previously-named Regional
Treatment Modality [1570] utilized codes that were not mutually exclusive. Rather, it
included codes describing a mix of modalities, treatment planning techniques, and
delivery techniques that are commonly utilized by radiation oncologists. However, every
phase of radiation treatment will include a specified modality, planning technique, and
delivery technique. The goal of the 2018 implementation of separate phase-specific data
items for the recording of Phase III Radiation Treatment Modality [1526] and Phase III
External Beam Radiation Planning Technique [1522] is to clarify this information and
implement mutually exclusive categories. Note that Planning Technique details are not
being captured for non-External Beam modalities. A separate data item for delivery
technique has not been implemented because this information is not consistently
reported in end treatment summaries.
Registry Coding instructions
• Radiation external beam treatment planning technique will typically be found in the
radiation oncologist’s summary letter for the first course of treatment. Determination of
the external beam planning technique may require assistance from the radiation
oncologist to ensure consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.
277
Phase III External Beam Radiation Planning Technique continued
• A new phase begins when there is a clinically meaningful change in target volume,
treatment fraction size (i.e., dose given during a session), modality or treatment
technique. Any one of these changes will generally mean that a new radiation plan will
be generated in the treatment planning system and should be coded as a new phase of
radiation therapy.
• Note: “on-line adaptive therapy” refers to treatments where radiation treatment plans
are adapted or updated while a patient is on the treatment table. When treatment plans
are adapted, the shape of the target volume may change from day to day but, for
registry purposes, the volume that is being targeted won’t change. An adapted plan
should not be coded as though a new phase of treatment has been initiated unless, as
above, the radiation oncologist documents it as a new phase in the radiation treatment
summary. Two new technique codes have been added to capture when online adaptive
therapy is occurring: CT guided and MR guided adaptive therapy.
• Code 05 for Intensity Modulated Therapy (IMT) or Intensity Modulated Radiation
Therapy (IMRT).
• Code 04 for Conformal or 3-D Conformal Therapy whenever either is explicitly
mentioned.
• When code 98 is recorded, document the planning technique in the appropriate text
data item.
• Blanks allowed if no Phase III radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

278
Phase III External Beam Radiation Planning Technique continued
Code
Definition
Description
00,
blank
No radiation
treatment
Radiation therapy was not administered to the patient
01
External beam,
NOS
The treatment is known to be by external beam, but there is insufficient
information to determine the specific planning technique
02
Low energy x-
ray/photon
therapy
External beam therapy administered using equipment with a maximum
energy of less than one (1) million volts (MV). Energies are typically
expressed in units of kilovolts (kV). These types of treatments are
sometimes referred to as electronic brachytherapy or orthovoltage or
superficial therapy. Clinical notes may refer to the brand names of low
energy x-ray delivery devices, e.g. Axxent®, INTRABEAM®, or Esteya®
03 2-D therapy
An external beam planning technique using 2-D imaging, such as plain film
x-rays or fluoroscopic images, to define the location and size of the
treatment beams. Should be clearly described as 2-
D therapy. This planning
modality is typically used only for palliative treatments
04
Conformal or 3-
D conformal
therapy
An external beam planning technique using multiple, fixed beams shaped
to conform to a defined target volume. Should be clearly described as
conformal or 3-D therapy in patient record
05
Intensity
modulated
therapy
An external beam planning technique where the shape or energy of beams
is optimized using software algorithms. Any external beam modality can be
modulated but these generally refer to photon or proton beams. Intensity
modulated therapy can be described as intensity modulated radiation
therapy (IMRT), intensity modulated xray or proton therapy (IMXT/IMPT),
volumetric arc therapy (VMAT) and other ways. If a treatment is described
as IMRT with online reoptimization/re-planning, then it should be
categorized as online reoptimization or re-planning
279
Phase III External Beam Radiation Planning Technique continued
06
Stereotactic
radiotherapy or
radiosurgery,
NOS
Treatment planning using stereotactic radiotherapy/radiosurgery techniques, but
the treatment is not described as Cyberknife® or Gamma Knife®. These
approaches are sometimes described as SBRT (stereotactic body radiation), SABR
(stereotactic ablative radiation), SRS (stereotactic radiosurgery), or SRT
(stereotactic radiotherapy). If the treatment is described as robotic radiotherapy
(e.g. Cyberknife®) or Gamma Knife®, use stereotactic radiotherapy subcodes
below. If a treatment is described as stereotactic radiotherapy or radiosurgery
with online re-optimization/re-planning, then it should be categorized as online re-
optimization or re-planning
07
Stereotactic
radiotherapy or
radiosurgery,
robotic
Treatment planning using stereotactic radiotherapy/radiosurgery techniques
which is specifically described as robotic (e.g. Cyberknife®)
08
Stereotactic
radiotherapy or
radiosurgery,
Gamma Knife®
Treatment planning using stereotactic radiotherapy/radiosurgery techniques
which uses a Cobalt-60 gamma ray source and is specifically described as Gamma
Knife®. This is most commonly used for treatments in the brain
09
CT-guided online
adaptive therapy
An external beam technique in which the treatment plan is adapted over the
course of radiation to reflect changes in the patient’s tumor or normal anatomy
radiation using a CT scan obtained at the treatment machine (online). These
approaches are sometimes described as CT-guided online re-
optimization or online
re-planning. If a treatment technique is described as both CT-guided online
adaptive therapy as well as another external beam technique (IMRT, SBRT, etc.),
then it should be categorized as CT-guided online adaptive therapy. If a treatment
is described as “adaptive” but does not include the descriptor “online”, this code
should not be used
10
MR-guided
online adaptive
therapy
An external beam technique in which the treatment plan is adapted over the
course of radiation to reflect changes in the patient’s tumor or normal anatomy
radiation using an MRI scan obtained at the treatment machine (online). These
approaches are sometimes described as MR-guided online re-optimization or
online re-planning. If a treatment technique is described as both MR-guided online
adaptive therapy as well as another external beam technique (IMRT, SBRT, etc.),
then it should be categorized as MR-guided online adaptive therapy. If a treatment
is described as “adaptive” but does not include the descriptor “online”, this code
should not be used
88
Not applicable
Treatment not by external beam
98 Other, NOS
Other radiation, NOS; Radiation therapy administered, but the treatment modality
is not specified or known
99
Unknown
It is unknown whether radiation therapy was administered
280
Phase III Dose per Fraction
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_DOSE_FRACT
NAACCR Item #: 1521
Diagnosis Years Available: 2018 +
Length: 5
Allowable Values: 00000 - 99999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017.
Records the dose per fraction (treatment session) delivered to the patient in the third
phase of radiation during the first course of treatment. The unit of measure is centi-Gray
(cGy). This data item is required for CoC-accredited facilities for cases diagnosed as of
01/01/2018 and later.
Rationale
Radiation therapy is delivered in one or more phases with identified dose per fraction.
It is necessary to capture information describing the dose per fraction to evaluate
patterns of radiation oncology care. Outcomes are strongly related to the dose
delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording
doses at the axis point where applicable (opposed fields, four field box, wedged pair,
and so on). For maximum consistency in this data item, the ICRP recommendations
should be followed whenever possible. Where there is no clear axis point, record the
total dose as indicated in the summary chart. Determining the exact dose may require
assistance from the radiation oncologist for consistent coding.
• Radiation treatment Phase III dose will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the Phase III dose of
radiation therapy may require assistance from the radiation oncologist for consistent
coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase
may be referred to as a boost or cone down, and would be recorded as Phase II, Phase
III, etc. accordingly.

281
Phase III Dose Per Fraction continued
• Record the actual dose delivered (NOT the initially prescribed dose) as documented in
the treatment summary.
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt
Gray Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase I Total Dose, you would
need to multiply cGe by 100).
o Note that dose is still occasionally specified in “rads”. One rad is equivalent to one
centiGray (cGy).
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• Code 99998 when radioisotopes were administered to the patient (codes 13-16 for
Phase III Treatment Modality [1526]).
• Blanks allowed if no Phase III radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
00000, blank
No radiation treatment
00001-99997 Record the actual Phase III dose delivered in cGy
99998
Not applicable, radioisotopes administered to the patient
99999
Phase III radiation therapy was administered but dose is unknown;
Unknown whether Phase III radiation therapy was administered

282
Phase III Dose Per Fraction continued
Examples
Code
Reason
00200
A patient with a metastatic left supraclavicular node and an isolated liver metastasis from a
gastric carcinoma received 6,000 cGy to the stomach. 2000 cGy external beam administered
to the supraclavicular node in 10 fractions followed by 2000 cGy administered to the liver
metastasis in ten fractions. Record 00200 for phase III dose per fraction.
00200
A patient with a Stage II breast carcinoma is treated with the breast intact. Tangent fields are
utilized to bring the dose of the breast to 5,500 cGy in 25 fractions. The axillary lymph nodes
were then treated with an additional 1000 cGy in 10 fractions. Phase III in the primary tumor
bed delivered to a small volume in the breast of 1000 cGy in 5 fractions. Record 00200 for
phase III dose per fraction.
283
Phase III Number of Fractions
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_NUM_FRACT
NAACCR Item #: 1523
Diagnosis Years Available: 2018 +
Length: 3
Allowable Values: 000 - 999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017.
Records the total number of fractions (treatment sessions) delivered to the patient in the third
phase of radiation during the first course of treatment. This data item is required for CoC-
accredited facilities for cases diagnosed as of 01/01/2018 and later.
Rationale
Radiation therapy is delivered in one or more phases with each phase spread out over a number
of fractions (treatment sessions). It is necessary to capture information describing the number
of fraction(s) to evaluate patterns of radiation oncology care.
Registry Coding Instructions
• The number of fractions or treatments will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. Determination of the exact number of
treatments or fractions delivered to the patient may require assistance from the radiation
oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase may be
referred to as a boost or cone down, and would be recorded as Phase II, Phase III, etc.
accordingly.
• Although a fraction or treatment session may include several treatment portals delivered
within a relatively confined period of time-usually a few minutes-it is still considered one
session.
• Count each separate administration of brachytherapy or implants as a single fraction or
treatment.
• Record the actual number of fractions delivered (NOT initially prescribed), as documented in
the treatment summary.

284
Phase III Number of Fractions continued
• There may be times when the first course of treatment information is incomplete. Therefore,
it is important to continue follow-up efforts to be certain the complete treatment information is
collected.
• Blanks allowed if no Phase III radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000, blank
No radiation treatment
001-998
Number of fractions administered to the patient during the third phase of radiation
therapy
999
Phase III Radiation therapy was administered, but the number of fractions is unknown;
It is unknown whether radiation therapy was administered

285
Phase III Number of Fractions continued
Examples
Code
Reason
005
A patient with breast carcinoma had treatment sessions in which treatment was delivered to
the chest wall and separately to the ipsilateral supraclavicular region for a total of three
fraction portals. Phase III was an additional 1000 cGy to axillary nodes for 5 fractions. Record
005 for Phase III Number of Fractions.
Blank
A patient with Stage IIIB bronchogenic carcinoma received 25 treatments to the left hilum and
mediastinum, given in 25 daily fractions over five weeks. Leave Phase III Number of Fractions
blank. Only one phase of radiation therapy administered.
010
A patient with metastatic head and neck cancer was treated using “hyperfractionation.” Three
fields were delivered in each session; two sessions were given each day, six hours apart, with
each session delivering a total dose of 150 cGy. Treatment was given for a total of 25 days.
Additional 1000 cGy in 10 fractions given to thoracic spine followed by 1000 cGy in 10
fractions to liver. Record 010 for Phase III Number of Fractions.
286
Phase III Total Dose
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: PHASE_III_TOTAL_DOSE
NAACCR Item #: 1527
Diagnosis Years Available: 2018 +
Length: 6
Allowable Values: 000000 - 999999, blank
Description:
This is a new item for 2018. It was required in 2018 and optional in 2017.
Identifies the total radiation dose administered during the third phase of radiation treatment delivered
to the patient during the first course of treatment. The unit of measure is centi-Gray (cGy). This data
item is required for CoC-accredited facilities for cases diagnosed as of 01/01/2018 and later.
Rationale
To evaluate the patterns of radiation care, it is necessary to capture information describing the
prescribed dose of Phase III radiation to the patient during the first course of treatment. Outcomes are
strongly related to the total dose delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording doses at the axis
point where applicable (opposed fields, four field box, wedged pair, and so on). For maximum
consistency in this data item, the ICRP recommendations should be followed whenever possible. Where
there is no clear axis point, record the total dose as indicated in the summary chart. Determining the
exact dose may be highly subjective and require assistance from the radiation oncologist for consistent
coding.
• Phase III radiation treatment dose will typically be found in the radiation oncologist’s summary letter
for the first course of treatment. Determination of the Phase III dose of radiation therapy may require
assistance from the radiation oncologist for consistent coding.
• The first phase may be commonly referred to as an initial plan and a subsequent phase may be
referred to as a boost or cone down, and would be recorded as Phase II, Phase III, etc. accordingly.
• Record the actual total dose delivered (NOT initially prescribed), as documented in the treatment
summary. The value recorded for this data item should NOT be auto-calculated within the registry
abstraction software.
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt Gray Equivalent)
rather than cGy. 1 cGe = 100 cGy (for the Phase III Total Dose, you would need to multiply cGe by 100).

287
Phase III Total Dose continued
Note that dose is still occasionally specified in “rads”. One rad is equivalent to one centiGray (cGy).
• Code 999998 when radioisotopes are administered to the patient (codes 13-16 recorded in the Phase
III Treatment Modality [1526]).
• There may be times when the first course of treatment information is incomplete. Therefore, it is
important to continue follow-up efforts to be certain the complete treatment information is collected.
• Blanks allowed if no Phase III radiation treatment administered.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000000, blank
No radiation treatment
000001-999997
Record the actual dose delivered in cGy
999998
Not applicable, radioisotopes administered to the patient
999999
Radiation therapy was administered, but the total dose is
unknown; it is unknown whether radiation therapy was
administered

288
Phase III Total Dose continued
Examples
Code
Reason
005000
A patient with Stage III prostate carcinoma received pelvic irradiation of 5,000 cGy during
Phase III Radiation Treatment. Record the Phase III Total Dose of 5,000 cGy as 005000
006000
A patient with a left supraclavicular metastasis from a gastric carcinoma received 6,000 cGy
to the left supraclavicular region during Phase III Radiation Treatment. Record the Phase III
Total Dose of 6,000 cGy as 006000.
005500
A patient with a Stage II breast carcinoma is treated with the breast intact. During Phase III
treatment tangent fields are utilized to bring the dose of the breast to 5,500 cGy. The
supraclavicular (draining) lymph nodes are treated 4,500 cGy, calculated to a depth of 3 cm.
Record the Phase III Total Dose of 5,500cGy as 005500
289
Number of Phases of Radiation Treatment to this Volume
Data Dictionary Category: Radiation
PUF Data Item Name: NUMBER_PHASES_RAD_RX
NAACCR Item #: 1532
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 04, 99
Description:
This is a new item in 2018. It was optional in 2017.
Identifies the total number of phases administered to the patient during the first course
of treatment. A “phase” consists of one or more consecutive treatments delivered to
the same anatomic volume with no clinically meaningful change in fraction size,
modality or treatment technique. Although the majority of courses of radiation therapy
are completed in one or two phases (historically, the “regional” and “boost” treatments)
there are occasions in which three or more phases are used, most typically with head
and neck malignancies. This data item is required for CoC-accredited facilities for cases
diagnosed as of 01/01/2018 and later.
Rationale
The number of phases of radiation treatment is used to evaluate patterns of radiation
therapy and the treatment schedule.
Registry Coding Instructions
• The number of phases of radiation treatment will typically be found in the radiation
oncologist’s summary letter for the first course of treatment. Determination of the exact
number of phases delivered to the patient may require assistance from the radiation
oncologist for consistent coding
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.

290
Number of Phases of Radiation Treatment to this Volume continued
Code
Definition
00
No radiation treatment
01
1 phase
02
2 phases
03
3 phases
04
4 or more phases
99
Unknown number of phases; Unknown if
radiation therapy administered
Examples
Code
Reason
00
Radiation therapy was not administered.
02
Patient with breast carcinoma treated in two phases, the whole breast with opposed x-ray
fields (Phase I) followed by an electron beam boost to the surgical bed (Phase II).
291
Radiation Treatment Discontinued Early
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: RAD_RX_DISC_EARLY
NAACCR Item #: 1531
Diagnosis Years Available: 2018 +
Length: 2
Allowable Values: 00 - 07, 99
Description:
This is a new item in 2018. It was optional in 2017.
This field is used to identify patients/tumors whose radiation treatment course was
discontinued earlier than initially planned. That is, the patients/tumors received fewer
treatment fractions (sessions) than originally intended by the treating physician. This
data item is required for CoC-accredited facilities for cases diagnosed 01/01/2018 and
later.
Rationale
Currently, the total dose of radiation reflects what was actually delivered rather than
what was intended. When a patient doesn’t complete a radiation course as initially
intended this is typically commented on within the radiation end of treatment summary.
By flagging these patients within the cancer registry database, these patients can be
excluded from analyses attempting to describe adherence to radiation treatment
guidelines or patterns of care analyses.
Registry Coding Instructions
• Radiation treatment recorded as discontinued early will typically be found in the
radiation oncologist’s summary letter for the first course of treatment.
• Use code 01 when there is no indication in the record that radiation therapy was
discontinued or completed early.
• Use code 02-07 when there is an indication in the record that the radiation therapy
discontinued or was completed early.
• Use code 99 when radiation therapy was administered, but it is not clear if the
treatment course was discontinued early, or if it is unknown whether radiation therapy
was administered
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.

292
Radiation Treatment Discontinued Early continued
Analytic Note: None.
Code
Definition
00
No radiation treatment
01
Radiation treatment completed as prescribed
02
Radiation treatment discontinued early; toxicity
03
Radiation treatment discontinued early; contraindicated to other patient
risk factors (comorbid conditions, advanced age, progression of tumor
prior to planned radiation, etc.
04
Radiation treatment discontinued early; patient decision
05
Radiation treatment discontinued early; family decision
06
Radiation treatment discontinued early; patient expired
07
Radiation treatment discontinued early; reason not documented
99
Unknown if radiation treatment discontinued; Unknown whether
radiation therapy administered
293
Total Dose
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: TOTAL_DOSE
NAACCR Item #: 1533
Diagnosis Years Available: 2018 +
Length: 6
Allowable Values: 000000 - 999999
Description:
This is a new item in 2018. It was optional in 2017.
Identifies the total cumulative radiation dose administered to the patient across all
phases during the first course of treatment. The unit of measure is centi-Gray (cGy).
This data item is required for CoC-accredited facilities for cases diagnosed 01/01/2018
and later.
Rationale
To evaluate the patterns of radiation care, it is necessary to capture information
describing the prescribed total dose of radiation during the first course of treatment.
Outcomes are strongly related to the dose delivered.
Registry Coding Instructions
• The International Council for Radiation Protection (ICRP) recommends recording
doses at the axis point where applicable (opposed fields, four field box, wedged pair,
and so on). For maximum consistency in this data item, the ICRP recommendations
should be followed whenever possible. Where there is no clear axis point, record the
total dose as indicated in the summary chart. Determining the exact dose may require
assistance from the radiation oncologist for consistent coding.
• Total radiation treatment dose will typically be found in the radiation oncologist’s
summary letter for the first course of treatment. If the total is not documented, then
add the dose from each phase (I, II, III, or IV or more) and document the total
cumulative dose. However, do not sum doses across phases if the phases use different
treatment fraction sizes or modalities (i.e. external beam in Phase I and brachytherapy
in Phase II). Determination of the total dose of radiation therapy may require
assistance from the radiation oncologist for consistent coding.
• For proton treatment, dosage may occasionally be specified as in cGe units (Cobalt
Gray Equivalent) rather than cGy. 1 cGe = 100 cGy (for the Phase I Total Dose, you

294
Total Dose continued
would need to multiply cGe by 100). o Note that dose is still occasionally specified in
“rads”. One rad is equivalent to one centiGray (cGy).
• There may be times when the first course of treatment information is incomplete.
Therefore, it is important to continue follow-up efforts to be certain the complete
treatment information is collected.
• Code 999998 when radioisotopes are administered to the patient (codes 13-16
recorded in the Phase I, Phase II, or Phase III Treatment Modality [1506, 1516, 1526]
data items).
• Doses should ONLY be summed across phases to create a Total Dose when all of the
phases were delivered sequentially to the same body site using the same modality and
dose-fractionation. If phases were delivered simultaneously (multiple body sites
[volumes], e.g. simultaneous treatment to multiple metastatic sites, or dose-painting),
with brachytherapy and any other different modality (e.g. external beam with a
brachytherapy boost), or using different fractionation schemes, then code 999998, Not
applicable.
See STORE Manual 2018 for more information at https://www.facs.org/-
/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx.
Analytic Note: None.
Code
Definition
000000
No radiation treatment
000001-999997
Record the actual total delivered in Gy
999998
Not applicable, radioisotopes administered to the patient
999999
Radiation therapy administered but the total dose is
unknown; it is unknown whether radiation therapy was
administered
295
Radiation/Surgery Sequence
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: RX_SUMM_SURGRAD_SEQ
NAACCR Item #: 1380
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0, 2 - 7, 9
Description:
Records the sequencing of radiation and surgical procedures given as part of the first
course of treatment.
Rationale:
The sequence of radiation and surgical procedures given as part of the first course of
treatment cannot always be determined using the date on which each modality was
started or performed. This data item can be used to more precisely evaluate the timing
of delivery of treatment to the patient.
Registry Coding Instructions:
• Surgical procedures include Surgical Procedure of Primary Site [1290]; Scope of
Regional Lymph Node Surgery [1292]; Surgical Procedure/Other Site [1294]. If all these
procedures are coded 0, or it is not known whether the patient received both surgery
and radiation, then this item should be coded 0.
• If the patient received both radiation therapy and any one or a combination of the
following surgical procedures: Surgical Procedure of Primary Site, Regional Lymph Node
Surgery, or Surgical Procedure/Other Site, then code this item 2–9, as appropriate.
• If multiple first course treatment episodes were given such that both codes 4 and 7
seem to apply, use the code that defines the first sequence that applies.
Analytic Note:
Beginning with 2010 diagnoses, when it is unknown whether radiation and/or surgery
were performed, the code assigned changed from 9 to 0. It is likely a shift in
distribution of these two codes may be noticeable around that time.

296
Radiation/Surgery Sequence continued
Code
Definition
Description
0
No radiation
therapy and/or
surgical procedures
No radiation therapy given or unknown if radiation therapy given; and/or no
surgery of the primary site; no scope of regional lymph node surgery; no
surgery to other regional site(s), distant site(s), or distant lymph node(s) or
it is unknown whether any surgery given.
2
Radiation therapy
before surgery
Radiation therapy given before surgery to primary site; scope of regional
lymph node surgery, surgery to other regional site(s), distant site(s), or
distant lymph node(s)
3
Radiation therapy
after surgery
Radiation therapy given after surgery to primary site; scope of regional
lymph node surgery, surgery to other regional site(s), distant site(s), or
distant lymph node(s)
4
Radiation therapy
both before and
after surgery
At least two courses of radiation therapy are given before and at least two
more after surgery to the primary site; scope of regional lymph node
surgery, surgery to other regional site(s), distant site(s), or distant lymph
node(s)
5
Intraoperative
radiation therapy
Intraoperative therapy given during surgery to primary site; scope of regional
lymph node surgery, surgery to other regional site(s), distant site(s), or
distant lymph node(s)
6
Intraoperative
radiation therapy
with other therapy
administered
before or after
surgery
Intraoperative radiation therapy given during surgery to primary site; scope
of regional lymph node surgery, surgery to other regional site(s), distant
site(s), or distant lymph node(s) with other radiation therapy administered
before or after surgery to primary site; scope of regional lymph node
surgery, surgery to other regional site(s), distant site(s), or distant lymph
node(s)
7
Surgery both before
and after radiation
Radiation was administered between two separate surgical procedures to
the primary site; regional lymph nodes; surgery to other regional site(s);
distant site(s); or distant lymph node(s)
9 Sequence unknown
Administration of radiation therapy and surgery to primary site, scope of
regional lymph node surgery, surgery to other regional site(s), distant site(s),
or distant lymph node(s) were performed and the sequence of the treatment
is not stated in the patient record.

297
Radiation/Surgery Sequence continued
Examples
Code
Reason
0
Due to other medical conditions surgery was not performed. The patient received palliative
radiation therapy to alleviate pain.
2
A large lung lesion received radiation therapy prior to resection.
3
A patient received a wedge resection of a right breast mass with axillary lymph node
dissection followed by radiation to right breast.
4
Preoperative radiation therapy was given to a large, bulky vulvar lesion and was followed by a
lymph node dissection. This was then followed by radiation therapy to treat positive lymph
nodes
5
A cone biopsy of the cervix was followed by intracavitary implant for IIIB cervical carcinoma
6
Stage IV vaginal carcinoma was treated with 5,000 cGy to the pelvis followed by a lymph node
dissection and 2,500 cGy of intracavitary brachytherapy.
9
An unknown primary of the head and neck was treated with surgery and radiation prior to
admission, but the sequence is unknown. The patient enters for chemotherapy.

298
Radiation Ended, Days from Start of Radiation
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: RAD_ELAPSED_RX_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 3
Allowable Values: 0 - 999
Description:
This item is calculated as the number of days between the Date Radiation Started
(NAACCR Item #1210) and the Date Radiation Ended (NAACCR Item #3220). One is
added to the number of days elapsed. This means that if radiation starts and ends on
the same date, then 1 day has elapsed, if radiation ends the day after it is started, then
2 days have elapsed, and so on.
Registry Coding Instructions: Not applicable.
Analytic Note: Not applicable.
Code
Definition
0
None, radiation not administered
1-998
Number of elapsed days
999
Missing or incomplete dates for radiation start and end,
days elapsed missing, or unknown if had radiation
299
Reason for No Radiation
Data Dictionary Category: Treatment: Radiation
PUF Data Item Name: REASON_FOR_NO_RADIATION
NAACCR Item #: 1430
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 2, 5 - 9
Description:
Records the reason that no regional radiation therapy was administered to the patient.
Rationale
When evaluating the quality of care, it is useful to know the reason that various
methods of therapy were not used, and whether the failure to provide a given type of
therapy was due to the physician’s failure to recommend that treatment, or due to the
refusal of the patient, a family member, or the patient’s guardian.
Registry Coding Instructions
• If Number of Phases of Radiation Treatment to this Volume [1532] is coded 00, Phase
I Radiation Primary Treatment Volume [1504] is coded 00, Radiation Treatment
Discontinued Early [1531] is coded 00, and Total Dose [1533] is coded 000000, then
record the reason based on documentation in patient record.
• Code 1 if the treatment plan offered multiple alternative treatment options and the
patient selected treatment that did not include radiation therapy.
• Code 7 if the patient refused recommended radiation therapy, made a blanket
refusal of all recommended treatment, or refused all treatment before any was
recommended.
• Code 8 if it is known that a physician recommended radiation treatment, but no
further documentation is available yet to confirm its administration.
• Code 8 to indicate referral to a radiation oncologist was made and the registry should
follow to determine whether radiation was administered. If follow-up to the specialist
or facility determines the patient was never there and no other documentation can be
found, code 1.
• Cases coded 8 should be followed and updated to a more definitive code as
appropriate.

300
Reason for No Radiation continued
• Code 9 if the treatment plan offered multiple alternative treatment options, but it is
unknown which treatment, if any, was provided.
Analytic Note: None.
Code
Definition
0
Radiation therapy was administered
1
Radiation therapy was not administered because it was not part of the planned first
course treatment
2
Radiation therapy was not recommended/administered because it was
contraindicated due to other patient risk factors (comorbid conditions, advanced age,
etc.)
5
Radiation therapy was not administered because the patient died prior to planned or
recommended therapy
6
Radiation therapy was not administered; it was recommended by the patient’s
physician, but was not administered as part of first course treatment. No reason was
noted in patient record
7
Radiation therapy was not administered; it was recommended by the patient’s
physician, but this treatment was refused by the patient, the patient’s family
member, or the patient’s guardian. The refusal was noted in patient record
8
Radiation therapy was recommended, but it is unknown whether it was
administered
9
It is unknown if radiation therapy was recommended or administered
Examples
Code
Reason
1
A patient with Stage I prostate cancer is offered either surgery or brachytherapy to treat his
disease. The patient elects to be surgically treated.
301
Treatment: Systemic

302
Systemic, Days from Dx
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: DX_SYSTEMIC_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and
the Date Systemic Therapy Started [chemotherapy, hormone therapy,
immunotherapy, or hematologic transplant and endocrine procedures] (NAACCR Item
#3230).
Registry Coding Instructions: Not applicable
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all
sources. Systemic treatment may have occurred at any facility, or at multiple facilities,
not limited to the one whose report is included in this file. This refers to the first
administration of systemic treatment for the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Systemic therapy not administered, therapy unknown, cannot
compute days elapsed, or not available for these diagnosis
years

303
Chemotherapy
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_SUMM_CHEMO
NAACCR Item #: 1390
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 03, 82, 85 - 88, 99
Description:
Records the type of chemotherapy administered as first course treatment at any facility.
If chemotherapy was not administered, then this item records the reason it was not
administered to the patient. Chemotherapy consists of a group of anticancer drugs
that inhibit the reproduction of cancer cells by interfering with DNA synthesis and
mitosis.
Registry Coding Instructions:
Code 00 if chemotherapy was not administered to the patient, and it is known that it
is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include chemotherapy.
If it is known that chemotherapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.
Code 87 if the patient refused recommended chemotherapy, made a blanket refusal of
all recommended treatment, or refused all treatment before any was recommended.
Code 99
if it is not known whether chemotherapy is usually administered for this type
and stage of cancer and there is no mention in the patient record whether it was
recommended or administered.
If the managing physician changes one of the agents in a combination regimen, and the
replacement agent belongs to a different group (chemotherapeutic agents are grouped
as alkylating agents, antimetabolites, natural products, or other miscellaneous) than
the original agent, the new regimen represents the start of subsequent therapy, and
only the original agent or regimen is recorded as first course therapy.
Refer to SEER*Rx (https://seer.cancer.gov/tools/seerrx/
for coding of
chemotherapeutic, hormonal and immunotherapies.
304
Chemotherapy continued
If chemotherapy was provided to prolong a patient’s life by controlling symptoms, to
alleviate pain, or to make the patient more comfortable, then also record the
chemotherapy administered in the item Palliative Care (NAACCR Item #3270).
Update as of 2013 PUF: Six drugs previously classified as Chemotherapy were
reclassified as BRM/Immunotherapy. This change in classification is effective only for
cases diagnosed in January 1st, 2013 and forward. While the NCDB does not provide
drug-specific data, changes in case counts may be observed for the Chemotherapy
(NAACCR Item #1390) and Immunotherapy (NAACCR Item #1410) variables for cases
diagnosed in 2013 due to the change in classification. The drugs are:
Alemtuzumab/Campath, Bvacizumab/Avastin, Rituximab, Trastuzumab/Herceptin,
Pertuzumab/Perjeta, and Cetuxumab/Erbitux.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all sources. This
item identifies chemotherapy given at the reporting facility. The item Chemotherapy (NAACCR Item
#1390) identifies chemotherapy given by any facility.

305
Chemotherapy continued
Code
Definition
00
None, chemotherapy was not part of the planned first course
of therapy
01
Chemotherapy administered as first course therapy, but the
type and number of agents is not documented in patient record
02
Single-agent chemotherapy administered as first course therapy
03
Multiagent chemotherapy administered as first course therapy
82
Chemotherapy was not recommended/administered because it
was contraindicated due to patient risk factors (ie, comorbid
conditions, advanced age, progression of tumor prior to
administration, etc.)
85
Chemotherapy was not administered because the patient died
prior to planned or recommended therapy
86
Chemotherapy was not administered. It was recommended by
the patient's physician, but was not administered as part of the
first course of therapy. No reason was stated in patient record
87
Chemotherapy was not administered. It was recommended by
the patient's physician, but this treatment was refused by the
patient, a patient's family member, or the patient's guardian.
The refusal was noted in patient record
88
Chemotherapy was recommended, but it is unknown if it was
administered
99
It is unknown whether a chemotherapeutic agent(s) was
recommended or administered because it is not stated in
patient record.

306
Chemotherapy at this Facility
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_HOSP_CHEMO
NAACCR Item #: 700
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00 - 03, 99
Description:
Records the type of chemotherapy administered as first course treatment by the facility
that submitted this record. If chemotherapy was not administered, then this item
records the reason it was not administered to the patient.
Registry Coding Instructions:
Code 00 if chemotherapy was not administered to the patient, and it is known that it
is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include chemotherapy.
Codes 82-88 are only included in the Chemotherapy (NAACCR Item #1390) variable.
If it is known that chemotherapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.
Code 87 if the patient refused recommended chemotherapy, made a blanket refusal of
all recommended treatment, or refused all treatment before any was recommended.
Code 99
if it is not known whether chemotherapy is usually administered for this type
and stage of cancer and there is no mention in the patient record whether it was
recommended or administered.
If the managing physician changes one of the agents in a combination regimen, and
the replacement agent belongs to a different group (chemotherapeutic agents are
grouped as alkylating agents, antimetabolites, natural products, or other miscellaneous)
than the original agent, the new regimen represents the start of subsequent therapy,
and only the original agent or regimen is recorded as first course therapy. Refer to
SEER*Rx https://seer.cancer.gov/tools/seerrx/
for coding of chemotherapeutic,
hormonal and immunotherapies.

307
Chemotherapy at this Facility continued
Update: As of the 2013 PUF, six drugs previously classified as Chemotherapy were
reclassified as BRM/Immunotherapy. This change in classification is effective only for
cases diagnosed in January 1st, 2013 and forward. While the NCDB does not provide
drug-specific data, changes in case counts may be observed for the Chemotherapy
(NAACCR Item #1390) and Immunotherapy (NAACCR Item #1410) variables for cases
diagnosed in 2013 due to the change in classification. The drugs are:
Alemtuzumab/Campath, Bvacizumab/Avastin, Rituximab, Trastuzumab/Herceptin,
Pertuzumab/Perjeta, and Cetuxumab/Erbitux.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. This item identifies chemotherapy given at the reporting facility. The item
Chemotherapy identifies chemotherapy given by any facility.
Code
Definition
00
None, chemotherapy was not part of the planned first course of
therapy
01
Chemotherapy administered as first course therapy, but the type and
number of agents is not documented in patient record
02
Single-agent chemotherapy administered as first course therapy
03
Multiagent chemotherapy administered as first course therapy
99
It is unknown whether a chemotherapeutic agent(s) was
recommended or administered because it is not stated in patient
record

308
Chemotherapy, Days from Dx
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: DX_CHEMO_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date Chemotherapy Started (NAACCR Item #1220).
Registry Coding Instructions: Not applicable
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all
sources. Chemotherapy treatment may have occurred at any facility, or at multiple
facilities, not limited to the one whose report is included in this file. This refers to the
first administration of chemotherapy for the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Chemotherapy not administered, chemotherapy unknown, or days
elapsed cannot be computed due to missing or incomplete dates
309
Hormone Therapy
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_SUMM_HORMONE
NAACCR Item #: 1400
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 01, 82, 85 - 88, 99
Description:
Records the type of hormone therapy administered as first course treatment at any
facility. If hormone therapy was not administered, then this item records the reason it
was not administered to the patient. Hormone therapy consists of a group of drugs
that may affect the long-term control of a cancer's growth.
Registry Coding Instructions:
Record prednisone as hormonal therapy when administered in combination with
chemotherapy, such as MOPP (mechlorethamine, vincristine, procarbazine,
prednisone) or COPP (cyclophosphamide, vincristine, procarbazine, prednisone).
Do not code prednisone as hormone therapy when it is administered for reasons other
than chemotherapeutic treatment.
Tumor involvement or treatment may destroy hormone-producing tissue. Hormone
replacement therapy will be given if the hormone is necessary to maintain normal
metabolism and body function. Do not code hormone replacement therapy as part of
first course therapy.
Code 00 if hormone therapy was not administered to the patient, and it is known that
it is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include hormone therapy.
Code 01 for thyroid replacement therapy which inhibits TSH (thyroid- stimulating
hormone). TSH is a product of the pituitary gland that can stimulate tumor growth.
If it is known that hormone therapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.

310
Hormone Therapy continued
Code 87 if the patient refused recommended hormone therapy, made a blanket
refusal of all recommended treatment, or refused all treatment before any was
recommended.
Code 99 if it is not known whether hormone therapy is usually administered for this
type and stage of cancer, and there is no mention in the patient record whether it was
recommended or administered.
Refer to SEER*Rx https://seer.cancer.gov/tools/seerrx/
for instructions for coding
hormonal, chemotherapeutic and immunotherapy agents.
If hormone therapy was provided to prolong a patient’s life by controlling symptoms,
to alleviate pain, or to make the patient more comfortable, then also record the
hormone therapy administered in the item Palliative Care (NAACCR Item #3270).
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Hormone treatment may have been given by any facility, or at multiple
facilities, not limited to the one whose report is included in this file.
Code
Definition
00
None, hormone therapy was not part of the planned first course of therapy
01
Hormone therapy administered as first course therapy
82
Hormone therapy was not recommended/administered because it was
contraindicated due to patient risk factors (ie, comorbid conditions, advanced age,
progression of tumor prior to administration)
85
Hormone therapy was not administered because the patient died prior to planned
or recommended therapy
86
Hormone therapy was not administered. It was recommended by the patient's
physician, but was not administered as part of the first course of therapy. No
reason was stated in patient record
87
Hormone therapy was not administered. It was recommended by the patient's
physician, but this treatment was refused by the patient, a patient's family
member, or the patient's guardian. The refusal was noted in patient record
88
Hormone therapy was recommended, but it is unknown if it was administered
99
It is unknown whether a hormonal agent(s) was recommended or administered
because it is not stated in patient record.
311
Hormone Therapy at This Facility
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_HOSP_HORMONE
NAACCR Item #: 710
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 01, 99
Description:
This item records the type of hormone therapy administered as first course treatment
by the facility that submitted this record. If hormone therapy was not administered,
then this item records the reason it was not administered to the patient. Hormone
therapy consists of a group of drugs that may affect the long- term control of a cancer's
growth.
Registry Coding Instructions:
Record prednisone as hormonal therapy when administered in combination with
chemotherapy, such as MOPP (mechlorethamine, vincristine, procarbazine,
prednisone) or COPP (cyclophosphamide, vincristine, procarbazine, prednisone).
Do not code prednisone as hormone therapy when it is administered for reasons other
than chemotherapeutic treatment.
Tumor involvement or treatment may destroy hormone-producing tissue. Hormone
replacement therapy will be given if the hormone is necessary to maintain normal
metabolism and body function. Do not code hormone replacement therapy as part of
first course therapy.
Code 00 if hormone therapy was not administered to the patient, and it is known that
it is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include hormone therapy.
Code 01 for thyroid replacement therapy which inhibits TSH (thyroid- stimulating
hormone). TSH is a product of the pituitary gland that can stimulate tumor growth.
Codes 82-88 are only coded in the Hormone Therapy (NAACCR Item #1400) variable.

312
Hormone Therapy at this Facility continued
If it is known that hormone therapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.
Code 87 if the patient refused recommended hormone therapy, made a blanket refusal
of all recommended treatment, or refused all treatment before any was
recommended.
Code 99 if it is not known whether hormone therapy is usually administered for this
type and stage of cancer, and there is no mention in the patient record whether it was
recommended or administered.
Refer to SEER*Rx (https://seer.cancer.gov/tools/seerrx/
) for instructions for coding
hormonal, chemotherapeutic and immunotherapy agents.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all
sources. This item identifies hormone therapy given at this facility. The item Hormone
Therapy records first course hormone therapy from any facility.
Code
Definition
00
None, hormone therapy was not part of the planned first course of
therapy
01
Hormone therapy administered as first course therapy
99
It is unknown whether a hormonal agent(s) was recommended or
administered because it is not stated in patient record.

313
Hormone Therapy, Days from Dx
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: DX_HORMONE_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date Hormone Therapy Started (NAACCR Item #1230).
Registry Coding Instructions: Not applicable
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Hormone treatment may have been provided by any facility, or multiple
facilities, not limited to the one whose report is included in this file. This refers to the
first administration of hormone treatment for the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Hormone therapy not administered, hormone therapy unknown, or
cannot compute elapsed days due to missing or incomplete dates

314
Immunotherapy
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_SUMM_IMMUNOTHERAPY
NAACCR Item #: 1410
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 01, 82, 85 - 88, 99
Description:
Records the type of immunotherapy administered as first course treatment at this and
all other facilities. If immunotherapy was not administered, then this item records the
reason it was not administered to the patient. Immunotherapy consists of biological or
chemical agents that alter the immune system or change the host's response to tumor
cells.
Registry Coding Instructions:
Code 00 if immunotherapy was not administered to the patient, and it is known that it
is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include immunotherapy.
If it is known that immunotherapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.
Code 87 if the patient refused recommended immunotherapy, made a blanket refusal
of all recommended treatment, or refused all treatment before any was
recommended.
Code 99
if it is not known whether immunotherapy is usually administered for this type
and stage of cancer, and there is no mention in the patient record whether it was
recommended or administered.
Refer to SEER*Rx https://seer.cancer.gov/tools/seerrx/
instructions for coding
immunotherapy, chemotherapeutic and hormonal agents.
If immunotherapy was provided to prolong a patient’s life by controlling symptoms, to
alleviate pain, or to make the patient more comfortable, then also record the
immunotherapy administered in the item Palliative Care (NAACCR Item #3270).

315
Immunotherapy continued
Update for 2013 PUF: Six drugs previously classified as Chemotherapy were reclassified
as BRM/Immunotherapy. This change in classification is effective only for cases
diagnosed in January 1st, 2013 and forward. While the NCDB does not provide drug
specific data, changes in case counts may be observed for the Chemotherapy (NAACCR
Item #1390) and Immunotherapy (NAACCR Item #1410) variables for cases diagnosed in
2013 due to the change in classification. The drugs are: Alemtuzumab/Campath,
Bvacizumab/Avastin, Rituximab, Trastuzumab/Herceptin, Pertuzumab/Perjeta, and
Cetuxumab/Erbitux.
Analytic Note:
Immunotherapy is sometimes called biologic response modifier (BRM). CoC cancer
programs are required to identify treatment their patients received from all sources.
Immunotherapy may have occurred at any facility, or at multiple facilities, not limited
to the one whose report is included in this file.
Code
Definition
00
None, immunotherapy was not part of the planned first course of therapy
01
Immunotherapy administered as first course therapy
82
Immunotherapy was not recommended/administered because it was
contraindicated due to patient risk factors (i.e, comorbid conditions, advanced
age, progression of tumor prior to administration)
85
Immunotherapy was not administered because the patient died prior to planned
or recommended therapy
86
Immunotherapy was not administered. It was recommended by the patient's
physician, but was not administered as part of the first course of therapy. No
reason was stated in patient record
87
Immunotherapy was not administered. It was recommended by the patient's
physician, but this treatment was refused by the patient, a patient's family
member, or the patient's guardian. The refusal was noted in patient record
88
Immunotherapy was recommended, but it is unknown if it was administered
99
It is unknown whether an immunotherapeutic agent(s) was recommended or
administered because it is not stated in patient record.

316
Immunotherapy at this Facility
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_HOSP_IMMUNOTHERAPY
NAACCR Item #: 720
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 01, 99
Description:
Records the type of immunotherapy administered as first course treatment at the
facility that submitted the record. If immunotherapy was not administered, then this
item records the reason it was not administered to the patient.
Registry Coding Instructions:
Code 00 if immunotherapy was not administered to the patient, and it is known that it
is not usually administered for this type and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include immunotherapy.
Codes 82-88 are included in the Immunotherapy (NAACCR Item #1410) variable.
If it is known that immunotherapy is usually administered for this type and stage of
cancer, but was not administered to the patient, use code 82, 85, 86, or 87 to record
the reason why it was not administered.
Code 87 if the patient refused recommended immunotherapy, made a blanket refusal
of all recommended treatment, or refused all treatment before any was
recommended.
Code 99
if it is not known whether immunotherapy is usually administered for this
type and stage of cancer, and there is no mention in the patient record whether it was
recommended or administered.
Refer to SEER*Rx https://seer.cancer.gov/tools/seerrx/
for instructions for coding
immunotherapy, chemotherapeutic and hormonal agents.

317
Immunotherapy at this Facility continued
Update for 2013 PUF: Six drugs previously classified as Chemotherapy were reclassified
as BRM/Immunotherapy. This change in classification is effective only for cases
diagnosed in January 1st, 2013 and forward. While the NCDB does not provide drug
specific data, changes in case counts may be observed for the Chemotherapy (NAACCR
Item #1390) and Immunotherapy (NAACCR Item #1410) variables for cases diagnosed in
2013 due to the change in classification. The drugs are: Alemtuzumab/Campath,
Bvacizumab/Avastin, Rituximab, Trastuzumab/Herceptin, Pertuzumab/Perjeta, and
Cetuxumab/Erbitux.
Analytic Note:
Immunotherapy is sometimes called biologic response modifier (BRM). CoC cancer
programs are required to identify treatment their patients received from all sources.
Immunotherapy may have occurred at any facility, or at multiple facilities, not limited
to the one whose report is included in this file.
Code
Definition
00
None, immunotherapy was not part of the planned first course of
therapy
01
Immunotherapy administered as first course therapy
99
It is unknown whether an immunotherapeutic agent was
recommended or administered because it is not stated in the patient
record

318
Immunotherapy, Days from Dx
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: DX_IMMUNO_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date Immunotherapy Started (NAACCR Item #1240).
Registry Coding Instructions: Not applicable.
Analytic Note:
Agents included for immunotherapy are also known as biologic response modifiers.
CoC cancer programs are required to identify treatment their patients received from all
sources. Immunotherapy may have occurred at any facility, or at multiple facilities, not
limited to the one whose report is included in this file. This refers to the first
administration of immunotherapy for the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Immunotherapy not administered, immunotherapy unknown, or
cannot compute days elapsed due to missing or incomplete dates
319
Hematologic Transplant and Endocrine Procedures
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_SUMM_TRNSPLNT_ENDO
NAACCR Item #: 3250
Diagnosis Years Available: 2004 +
Length: 2
Allowable Values: 00, 10 - 12, 20, 30, 40, 82, 85 - 88, 99
Description:
Identifies systemic therapeutic procedures performed as part of the first course of
treatment at this and all other facilities. If none of these procedures was performed,
then this item records the reason why not. These procedures include bone marrow
transplants, stem cell harvests, and surgical and/or radiation endocrine therapy.
Registry Coding Instructions:
Bone marrow transplants should be coded as either autologous (bone marrow
originally taken from the patient) or allogeneic (bone marrow donated by a person
other than the patient). For cases in which the bone marrow transplant was syngeneic
(transplanted marrow from an identical twin), the item is coded as allogeneic.
Stem cell harvests involve the collection of immature blood cells from the patient and
the reintroduction by transfusion of the harvested cells following chemotherapy or
radiation therapy.
Endocrine irradiation and/or endocrine surgery are procedures which suppress the
naturally occurring hormonal activity of the patient and thus alter or effect the long-
term control of the cancer's growth. These procedures must be bilateral to qualify as
endocrine surgery or endocrine radiation. If only one gland is intact at the start of
treatment, surgery and/or radiation to that remaining gland is coded as endocrine
surgery or endocrine radiation.
Code 00 if a transplant or endocrine procedure was not administered to the patient,
and it is known that these procedures are not usually administered for this type
and stage of cancer.
Code 00 if the treatment plan offered multiple options, and the patient selected
treatment that did not include a transplant or endocrine procedure.
If it is known that a transplant or endocrine procedure is usually administered for this
type and stage of cancer, but was not administered to the patient, use code 82, 85,
86, or 87 to record the reason why it was not administered.

320
Hematologic Transplant and Endocrine Procedures continued
Code 87 if the patient refused a recommended transplant or endocrine procedure,
made a blanket refusal of all recommended treatment, or refused all treatment before
any was recommended.
Code 99 if it is not known whether a transplant or endocrine procedure is usually
administered for this type and stage of cancer, and there is no mention in the patient
record whether it was recommended or administered.
If hematologic transplant or endocrine procedure coded in this item was provided to
prolong a patient’s life by controlling symptoms, to alleviate pain, or to make the
patient more comfortable, then also record the hematologic transplant or endocrine
procedure provided in the item Palliative Care (NAACCR Item #3270) and/or Palliative
Care at this Facility (NAACCR Item #3280), as appropriate.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Procedures may have occurred at any facility, not limited to the one whose
report is included in this file.
Code
Definition
00
No transplant procedure or endocrine therapy was administered as part of first
course therapy
10
A bone marrow transplant procedure was administered, but the type was not
specified
11
Bone marrow transplant - autologous
12
Bone marrow transplant - allogeneic
20
Stem cell harvest and infusion. Umbilical cord stem cell transplant, with blood
from one or multiple umbilical cords.
30
Endocrine surgery and/or endocrine radiation therapy
40
Combination of endocrine surgery and/or radiation with a transplant procedure.
(Combination of codes 30 and 10, 11, 12, or 20)
82
Hematologic transplant and/or endocrine surgery/radiation was not
recommended/administered because it was contraindicated due to patient risk
factors (i.e, comorbid conditions, advanced age, progression of disease prior to
administration, etc.)

321
Hematologic Transplant and Endocrine Procedures continued
85
Hematologic transplant and/or endocrine surgery/radiation was not
administered because the patient died prior to planned or recommended
therapy
86
Hematologic transplant and/or endocrine surgery/radiation was not
administered. It was recommended by the patient's physician, but was not
administered as part of the first course of therapy. No reason was stated in
patient record
87
Hematologic transplant and/or endocrine surgery/radiation was not
administered. It was recommended by the patient's physician, but this
treatment was refused by the patient, a patient's family member, or the
patient's guardian. The refusal was noted in patient record
88
Hematologic transplant and/or endocrine surgery/radiation was recommended,
but it is unknown if it was administered
99
It is unknown whether hematologic transplant and/or endocrine
surgery/radiation was recommended or administered because it is not stated in
patient record.
322
Systemic/Surgery Sequence
Data Dictionary Category: Treatment: Systemic
PUF Data Item Name: RX_SUMM_SYSTEMIC_SUR_SEQ
NAACCR Item #: 1639
Diagnosis Years Available: 2006 +
Length: 1
Allowable Values: 0, 2 - 7, 9, blank
Description:
Records the sequencing of systemic treatment and surgical procedures given as part of
the first course of treatment.
Registry Coding Instructions:
Surgical procedures include Surgical Procedures of Primary Site (NAACCR Item #1290),
Scope of Regional Lymph Node Surgery (NAACCR Item #1292), and Surgical
Procedure/Other Site (NAACCR Item #1294). Systemic therapy includes Chemotherapy
(NAACCR Item #1390), Hormone Therapy (NAACCR Item #1400), Immunotherapy
(NAACCR Item #1410) and Hematologic Transplant and Endocrine Procedures (NAACCR
Item #3250). If no surgical procedure was performed, or no systemic treatment was
given, this item is coded 0.
If both surgery and systemic treatment were provided for this cancer, then code 2- 9, as
appropriate.
Analytic Note:
This item was added to FORDS for use with cases diagnosed in 2006 or later.
CoC cancer programs are required to identify treatment their patients received from all
sources. Treatment may have occurred at any facility, or at multiple facilities, not
limited to the one whose report is included in this file.

323
Systemic/Surgery Sequence continued
Code
Label
Definition
0
No systemic therapy and/or
surgical procedures
No systemic therapy was given; and/or no surgical procedure of
primary site; no scope of regional lymph node surgery; no surgery to
other regional site(s), distant site(s), or distant lymph node(s); or no
reconstructive surgery was performed. Or: It is unknown whether
both surgery and systemic treatment were provided
2
Systemic therapy before
surgery
Systemic therapy was given before surgical procedure of primary
site; scope of regional lymph node surgery; surgery to other
regional site(s), distant site(s), or distant lymph node(s) was
performed
3
Systemic therapy after
surgery
Systemic therapy was given after surgical procedure of primary
site; scope of regional lymph node surgery; surgery to other
regional site(s), distant site(s), or distant lymph node(s) was
performed
4
Systemic therapy both
before and after surgery
At least two courses of systemic therapy were given before and at
least two more after a surgical procedure of primary site; scope of
regional lymph node surgery; surgery to other regional site(s), or
distant site(s), or lymph node(s) was performed
5
Intraoperative systemic
therapy
Intraoperative systemic therapy was given during surgical
procedure of primary site; scope of regional lymph node surgery;
surgery to other regional site(s), distant site(s), or distant lymph
node(s)
6
Intraoperative systemic
therapy with other
systemic therapy
administered before or
after surgery
Intraoperative systemic therapy was given during surgical
procedure of primary site; scope of regional lymph node surgery;
surgery to other regional site(s), distant site(s), or distant lymph
node(s) with other systemic therapy administered before or after
surgical procedure of primary site; scope of regional lymph node
surgery; surgery to other regional site(s), distant site(s), or distant
lymph node(s) was performed
7
Surgery both before and
after systemic therapy
Systemic therapy was administered between two separate surgical
procedures to the primary site; regional lymph nodes; surgery to
other regional site(s), distant site(s), or distant lymph node(s).
9 Sequence unknown
Both surgery and systemic therapy were provided, but the
sequence is unknown
blank
Not available
324
Treatment: Other Treatment

325
Other Treatment
Data Dictionary Category: Treatment: Other Treatment
PUF Data Item Name: RX_SUMM_OTHER
NAACCR Item #: 1420
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3, 6 - 9
Description:
Identifies other treatment that cannot be defined as surgery, radiation, or systemic
therapy according to the defined data items in this manual.
Registry Coding Instructions:
In order to report the hematopoietic cases in which the patient received supportive
care, SEER and the Commission on Cancer have agreed to record treatments such as
phlebotomy, transfusion, or aspirin as Other Treatment (NAACCR Item #1420) Code 1
for certain hematopoietic diseases ONLY. Consult https://seer.cancer.gov/tools/seerrx/
for instructions for coding care of specific hematopoietic neoplasms in this item.
Code 1 for embolization using alcohol as an embolizing agent.
Code 1 for embolization to a site other than the liver where the embolizing agent is
unknown.
Code 1 for PUFA (psoralen and long-wave ultraviolet radiation). Do not code pre-
surgical embolization given to shrink the tumor.
Code 8 if it is known that a physician recommended treatment coded as Other
Treatment, and no further documentation is available yet to confirm its
administration.
Code 8 to indicate referral to a specialist for Other Treatment; the registry should
follow. If follow-up with the specialist or facility determines the patient was never
there, code 0.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Other treatment may have been given by any facility, or multiple facilities,
not limited to the one whose report is included in this file. This refers to the first use of
other treatment for the cancer by any facility.

326
Other Treatment continued
Code
Definition
Description
0 None
All cancer treatment was coded in other treatment fields
(surgery, radiation, systemic therapy). Patient received no
cancer treatment
1 Other
Cancer treatment that cannot be appropriately assigned to
specified treatment data items (surgery, radiation, systemic).
Use this code for treatment unique to hematopoietic diseases
2
Other-
Experimental
This code is not defined. It may be used to record
participation in institution-based clinical trials
3
Other-Double
Blind
A patient is involved in a double-blind clinical trial. Code the
treatment actually administered when the double-blind trial
code is broken
6
Other-Unproven
Cancer treatments administered by nonmedical personnel
7 Refusal
Other treatment was not administered. It was recommended
by the patient's physician, but this treatment (which would
have been coded 1, 2, or 3) was refused by the patient, a
patient's family member, or the patient's guardian. The refusal
was noted in the patient record
8
Recommended;
unknown if
administered
Other treatment was recommended, but it is unknown
whether it was administered
9 Unknown
It is unknown whether other treatment was recommended or
administered, and there is no information in the medical
record to confirm the recommendation or administration of
other treatment.

327
Other Treatment at this Facility
Data Dictionary Category: Treatment: Other Treatment
PUF Data Item Name: RX_HOSP_OTHER
NAACCR Item #: 730
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 3, 6 - 9
Description:
Identifies other treatment given at the reporting facility that cannot be defined as
surgery, radiation, or systemic therapy.
Registry Coding Instructions:
In order to report the hematopoietic cases in which the patient received supportive
care, SSER and the Commission on Cancer have agreed to record treatments such as
phlebotomy, transfusion, or aspirin as Other Treatment (NAACCR Item #1420) Code 1
for certain hematopoietic diseases ONLY. Consult https://seer.cancer.gov/tools/seerrx/
for instructions for coding care of specific hematopoietic neoplasms in this item.
Code 1 for embolization using alcohol as an embolizing agent.
Code 1 for embolization to a site other than the liver where the embolizing agent is
unknown.
Code 1 for PUFA (psoralen and long-wave ultraviolet radiation). Do not code pre-
surgical embolization given to shrink the tumor.
Code 8 if it is known that a physician recommended treatment coded as Other
Treatment, and no further documentation is available yet to confirm its
administration.
Code 8 to indicate referral to a specialist for Other Treatment; the registry should
follow. If follow-up with the specialist or facility determines the patient was never
there, code 0.
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from
all sources. Other treatment may have been given by any facility, or multiple facilities,
not limited to the one whose report is included in this file. This refers to the first use of
other treatment for the cancer by the reporting facility.

328
Other Treatment at this Facility continued
Code
Definition
Description
0 None
All cancer treatment was coded in other treatment fields
(surgery, radiation, systemic therapy). Patient received no
cancer treatment
1 Other
Cancer treatment that cannot be appropriately assigned to
specified treatment data items (surgery, radiation, systemic).
Use this code for treatment unique to hematopoietic diseases
2
Other-
Experimental
This code is not defined. It may be used to record
participation in institution-based clinical trials
3
Other-Double
Blind
A patient is involved in a double-blind clinical trial. Code the
treatment actually administered when the double-blind trial
code is broken
6
Other-Unproven
Cancer treatments administered by nonmedical personnel
7 Refusal
Other treatment was not administered. It was recommended
by the patient's physician, but this treatment (which would
have been coded 1, 2, or 3) was refused by the patient, a
patient's family member, or the patient's guardian. The refusal
was noted in the patient record
8
Recommended;
unknown if
administered
Other treatment was recommended, but it is unknown
whether it was administered
9 Unknown
It is unknown whether other treatment was recommended or
administered, and there is no information in the medical
record to confirm the recommendation or administration of
other treatment.

329
Other Treatment, Days from Dx
Data Dictionary Category: Treatment: Other Treatment
PUF Data Item Name: DX_OTHER_STARTED_DAYS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 +
Length: 8
Allowable Values: -9999999 – 99999999 (negative and positive), blank
Description:
The number of days between the Date of Initial Diagnosis (NAACCR Item #390) and the
Date Other Treatment Started (NAACCR Item #1250).
Registry Coding Instructions: Not applicable
Analytic Note:
CoC cancer programs are required to identify treatment their patients received from all
sources. This treatment may have been given by any facility, or multiple facilities, not
limited to the one whose report is included in this file. This refers to the first given for
the cancer by any facility.
Code
Definition
0000 - 9999
Number of elapsed days
blank
Other therapy not administered, other therapy unknown, or
cannot compute elapsed days due to missing or incomplete dates
330
Palliative Care
Data Dictionary Category: Treatment: Other Treatment
PUF Data Item Name: PALLIATIVE_CARE
NAACCR Item #: 3270
Diagnosis Years Available: 2004 +
Length: 1
Allowable Values: 0 - 7, 9
Description:
Identifies any care provided in an effort to palliate or alleviate symptoms. Palliative care
is performed to relieve symptoms and may include surgery, radiation therapy, systemic
therapy (chemotherapy, hormone therapy, or other systemic drugs), and/or other pain
management therapy.
Registry Coding Instructions:
Surgical procedures, radiation therapy, or systemic therapy provided to prolong the
patient's life by controlling symptoms, to alleviate pain, or to make the patient
comfortable should be coded palliative care and as first course therapy if that procedure
removes or modifies either primary or metastatic malignant tissue.
Palliative care is not used to diagnose or stage the primary tumor.
Analytic Note:
This data item can be used to distinguish a treatment modality given for curative
treatment from the same modality being used strictly for palliation.
If patients are admitted to a hospital for palliative care other than surgery, radiation or
systemic treatment, the record often does not indicate the underlying reason for the
procedure (for example, other forms of pain care). Therefore, when the initial care
was elsewhere and the care was not one of these three modalities, it is unlikely the
care will be reported in this data item.

331
Palliative Care continued
Code
Definition
0
No palliative care provided
1
Surgery (which may involve a bypass procedure) to alleviate symptoms, but
no attempt to diagnose, stage, or treat the primary tumor is made
2
Radiation therapy to alleviate symptoms, but no attempt to diagnose, stage,
or treat the primary tumor is made
3
Chemotherapy, hormone therapy, or other systemic drugs to alleviate
symptoms, but no attempt to diagnose, stage, or treat the primary tumor
is made
4
Patient received or was referred for pain management therapy with no other
palliative care
5
Any combination of codes 1, 2, and/or 3 without code 4
6
Any combination of codes 1, 2, and/or 3 with code 4
7
Palliative care was performed or referred, but no information on the type of
procedure is available in the patient record. Palliative care was provided
that does not fit the descriptions for codes 1-6
9
It is unknown if palliative care was performed or referred; not stated in
patient record
332
Palliative Care at and this Facility
Data Dictionary Category: Treatment: Other Treatment
PUF Data Item Name: PALLIATIVE_CARE_HOSP
NAACCR Item #: 3280
Diagnosis Years Available: 2004 - 2010
Length: 1
Allowable Values: 0 - 7, 9
Description:
Identifies any care provided in an effort to palliate or alleviate symptoms at the
reporting facility. Palliative care is performed to relieve symptoms and may include
surgery, radiation therapy, systemic therapy (chemotherapy, hormone therapy, or
other systemic drugs), and/or other pain management therapy. This data item was
added to the 2015 PUF (data released in Fall 2017) and does not appear in prior versions
of the PUF data.
Registry Coding Instructions:
Surgical procedures, radiation therapy, or systemic therapy provided to prolong the
patient's life by controlling symptoms, to alleviate pain, or to make the patient
comfortable should be coded palliative care and as first course therapy if that procedure
removes or modifies either primary or metastatic malignant tissue. Palliative care is not
used to diagnose or stage the primary tumor.
Analytic Note:
This data item can be used to distinguish a treatment modality given for curative
treatment from the same modality being used strictly for palliation.
If patients are admitted to a hospital for palliative care other than surgery, radiation or
systemic treatment, the record often does not indicate the underlying reason for the
procedure (for example, other forms of pain care). Therefore, when the initial care
was elsewhere and the care was not one of these three modalities, it is unlikely the
care will be reported in this data item. This item identifies palliative care at the
reporting facility.

333
Palliative Care at this Facility
Code
Definition
0
No palliative care provided
1
Surgery (which may involve a bypass procedure) to alleviate symptoms, but
no attempt to
diagnose, stage, or treat the primary tumor is made
2
Radiation therapy to alleviate symptoms, but no attempt to diagnose, stage,
or treat the
primary tumor is made
3
Chemotherapy, hormone therapy, or other systemic drugs to alleviate
symptoms, but no
attempt to diagnose, stage, or treat the primary tumor is
made
4
Patient received or was referred for pain management therapy with no other
palliative care
5
Any combination of codes 1, 2, and/or 3 without code 4
6
Any combination of codes 1, 2, and/or 3 with code 4
7
Palliative care was performed or referred, but no information on the type of
procedure is
available in the patient record. Palliative care was provided that
does not fit the descriptions
for codes 1-6
9
It is unknown if palliative care was performed or referred; not stated in
patient record
334
Outcomes

335
Thirty Day Mortality
Data Dictionary Category: Outcomes
PUF Data Item Name: PUF_30_DAY_MORT_CD
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 - 2019
Length: 1
Allowable Values: 0, 1, 9, blank
Description:
This item indicates mortality within 30 days of the most definitive primary site surgery.
Registry Coding Instructions: Not applicable.
Analytic Note:
The computation was based on the Date of Most Definitive Surgical Resection of the
Primary Site (NAACCR Item #3170) if that is known. Otherwise, it was based on the
Date of the First Surgical Procedure (NAACCR Item #1200). In either case, the Date of
Last Contact or Death (NAACCR Item #1750) was subtracted from the surgery date and
patient Vital Status (NAACCR Item #1760) indicated whether the latter date referred to
contact or death. Eligible cases are limited to Surgical Procedure of Primary Site codes
20-90 (NAACCR Item #1290). Thirty Day Mortality is blank for patients diagnosed in
2019. Investigators analyzing surgical mortality at the facility level must use the Surgical
Procedure of Primary Site at this Facility (NAACCR Item #670) variable to determine if
the surgery was performed at the facility included in the PUF data. See the Getting
Started document for more information.
Code
Definition
0
Patient alive, or died more than 30 days after surgery
performed
1
Patient died <= 30 days from surgery date
9
Patient alive with fewer than 30 days of follow-up, surgery date
missing,
or last contact date missing
blank
Not eligible; surgical resection unknown or not performed, or
diagnosed in
2019

336
Ninety Day Mortality
Data Dictionary Category: Outcomes
PUF Data Item Name: PUF_90_DAY_MORT_CD
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 - 2019
Length: 1
Allowable values: 0, 1, 9, blank
Description:
This item indicates mortality within 90 days after the most definitive primary site
surgery.
Registry Coding Instructions: Not applicable.
Analytic Note:
The computation was based on the Date of Most Definitive Surgical Resection of the
Primary Site (NAACCR #3170) if that was known. Otherwise, it was based on the Date of
First Surgical Procedure (NAACCR Item #1200). In either case, the Date of Last Contact
or Death (NAACCR Item #1750) was subtracted from the surgery date and patient Vital
Status (NAACCR Item #1760) indicated whether the latter date referred to contact or
death. Eligible cases are limited to Surgical Procedure of Primary Site codes 20-90
(NAACCR Item #1290). Ninety Day Mortality is blank for patients diagnosed in 2019.
Investigators analyzing surgical mortality at the facility level must use the Surgical
Procedure of Primary Site at this Facility (NAACCR Item #670) variable to determine if
the surgery was performed at the facility included in the PUF data. See the Getting
Started document for more information.
Code
Definition
0
Patient alive, or died more than 90 days after surgery
performed
1
Patient died <= 90 days from the surgery date
9
Patient alive with fewer than 90 days of follow-up, surgery date
missing,
or last contact date missing
blank
Not eligible; surgical resection unknown or not performed, or
diagnosed in
2019
337
Last Contact or Death, Months from Dx
Data Dictionary Category: Outcomes
PUF Data Item Name: DX_LASTCONTACT_DEATH_MONTHS
NAACCR Item #: Not applicable
Diagnosis Years Available: 2004 - 2019
Length: 8
Allowable Values: 0000.0 - 8887.9, 9999.0, blank
Description:
The number of months between the Date of Initial Diagnosis (NAACCR Item #390) and
the Date of Last Contact or Death (NAACCR Item #1750).
Registry Coding Instructions: Not applicable.
Analytic Note:
Months Elapsed is blank for patients diagnosed in 2020.
Beginning with the 2020 Call for Data, registries will submit annual follow-up for cases
diagnosed within the past 15 years or as of first accredited date, whichever is shorter.
Code
Definition
0000.0 - 8887.9
Number of elapsed months
9999.0
Unknown, number of elapsed months cannot be computed
blank
Not available

338
Vital Status
Data Dictionary Category: Outcomes
PUF Data Item Name: PUF_VITAL_STATUS
NAACCR Item #: 1760
Diagnosis Years Available: 2004 - 2019
Length: 1
Allowable Values: 0, 1, blank
Description:
Records the vital status of the patient as of the date entered in Date of Last Contact or
Death (NAACCR Item #1750), which is the status of the patient at the end of Elapsed
Months - Date of Initial Diagnosis (NAACCR Item #390) to Date of Last Contact or Death
(NAACCR Item #1750) in the PUF.
Registry Coding Instructions: None.
Analytic Note:
Vital Status (NAACCR Item #1760) is blank for cases diagnosed in 2019. See the Getting
Started Guide to Using the Data page 11 for more information on follow-up capture and
approach to survival analysis.
Vital Status (NAACCR Item #1760) is the only item for which SEER and CoC agreed to
retain different codes to mean the same thing. For historic reasons, SEER uses code 4
for deceased patients while CoC uses 0. All 4s in the CoC database were converted to 0
for the PUF file. There is no Vital Status (NAACCR Item #1760) code for "unknown".
Therefore, cases for which the code was not valid are transmitted as blank. They may
have been submitted as blanks, 9s, or any other non-defined value. They can be
analyzed as "unknown" or omitted from analysis, depending on the needs of the study.
Code
Definition
0
Dead
1
Alive
blank
Not available
339
Appendix A: Site-Specific Surgery Codes
Note: The histologies listed in this section apply only to cases diagnosed in 2010 or later. Please consult
FORDS: Revised for 2009 for applicable histologies for cases diagnosed prior to that date at:
https://www.facs.org/quality-programs/cancer/ncdb/call-for-data/fordsolder.
340
Oral Cavity
Lip C00.0-C00.9, Base of Tongue C01.9, Other Parts of Tongue C02.0-C02.9, Gum C03.0-C03.9, Floor of
Mouth C04.0-C04.9, Palate C05.0-C05.9, Other Parts of Mouth C06.0-C06.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Wide excision, NOS
Code 30 includes:
Hemiglossectomy
Partial glossectomy
40 Radical excision of tumor, NOS
41 Radical excision of tumor ONLY
42 Combination of 41 WITH resection in continuity with mandible (marginal, segmental,
hemi-, or total resection)
43 Combination of 41 WITH resection in continuity with maxilla (partial, subtotal, or total
resection)
Codes 40-43 include:
Total glossectomy
Radical glossectomy
341
Oral Cavity continued
Specimen sent to pathology from surgical events 20-43.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 12/4/02, 01/10, 02/10, 01/16
342
Parotid and Other Unspecified Glands
Parotid Gland C07.9, Major Salivary Glands C08.0-C08.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Less than total parotidectomy, NOS; less than total removal of major salivary gland, NOS
31 Facial nerve spared
32 Facial nerve sacrificed
33 Superficial lobe ONLY
34 Facial nerve spared
35 Facial nerve sacrificed
343
Parotid and Other Unspecified Glands continued
36 Deep lobe (Total)
37 Facial nerve spared
38 Facial nerve sacrificed
40 Total parotidectomy, NOS; total removal of major salivary gland, NOS
41 Facial nerve spared
42 Facial nerve sacrificed
50 Radical parotidectomy, NOS; radical removal of major salivary gland, NOS
51 WITHOUT removal of temporal bone
52 WITH removal of temporal bone
53 WITH removal of overlying skin (requires graft or flap coverage)
80 Parotidectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed;
Revised 01/10, 02/10, 01/16
344
Pharynx
Tonsil C09.0-C09.9, Oropharynx C10.0-C10.9, Nasopharynx C11.0-C11.9 Pyriform Sinus C12.9,
Hypopharynx C13.0-C13.9, Pharynx C14.0
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Stripping
No specimen sent to pathology from surgical events 10-15.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
28 Stripping
30 Pharyngectomy, NOS
31 Limited/partial pharyngectomy; tonsillectomy, bilateral tonsillectomy
32 Total pharyngectomy
345
Pharynx continued
40 Pharyngectomy WITH laryngectomy OR removal of contiguous bone tissue, NOS (does NOT
include total mandibular resection)
41 WITH Laryngectomy (laryngopharyngectomy)
42 WITH bone
43 WITH both 41 and 42
50 Radical pharyngectomy (includes total mandibular resection), NOS
51 WITHOUT laryngectomy
52 WITH laryngectomy
Specimen sent to pathology from surgical events 20-52.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
346
Esophagus
C15.0-C15.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Partial esophagectomy
40 Total esophagectomy, NOS
50 Esophagectomy, NOS WITH laryngectomy and/or gastrectomy, NOS
51 WITH laryngectomy
52 WITH gastrectomy, NOS
53 Partial gastrectomy
54 Total gastrectomy
55 Combination of 51 WITH any of 52-54
347
Esophagus continued
80 Esophagectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
348
Stomach
C16.0-C16.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Gastrectomy, NOS (partial, subtotal, hemi-)
31 Antrectomy, lower (distal-less than 40% of stomach)***
32 Lower (distal) gastrectomy (partial, subtotal, hemi-)
33 Upper (proximal) gastrectomy (partial, subtotal, hemi-)
Code 30 includes:
Partial gastrectomy, including a sleeve resection of the stomach
Billroth I: anastomosis to duodenum (duodenostomy)
Billroth II: anastomosis to jejunum (jejunostomy)

349
Stomach continued
40 Near-total or total gastrectomy, NOS
41 Near-total gastrectomy
42 Total gastrectomy
A total gastrectomy may follow a previous partial resection of the stomach.
50 Gastrectomy, NOS WITH removal of a portion of esophagus
51 Partial or subtotal gastrectomy
52 Near total or total gastrectomy
Codes 50-52 are used for gastrectomy resection when only portions of esophagus are
included in procedure.
60 Gastrectomy with a resection in continuity with the resection of other organs, NOS***
61 Partial or subtotal gastrectomy, in continuity with the resection of other organs***
62 Near total or total gastrectomy, in continuity with the resection of other organs***
63 Radical gastrectomy, in continuity with the resection of other organs***
Codes 60-63 are used for gastrectomy resections with organs other than esophagus. Portions
of esophagus may or may not be included in the resection.
80 Gastrectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
*** Incidental splenectomy NOT included
Revised 01/10, 02/10, 01/16
350
Colon
C18.0-C18.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Code removal/surgical ablation of single or multiple liver metastases under the data item Surgical
Procedure/Other Site (NAACCR Item #1294).
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
27 Excisional biopsy
26 Polypectomy, NOS
28 Polypectomy-endoscopic
29 Polypectomy-surgical excision
Any combination of 20 or 26-29 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
Partial colectomy, segmental resection
32 Plus resection of contiguous organ; example: small bowel, bladder
40 Subtotal colectomy/hemicolectomy (total right or left colon and a portion of transverse colon)
41 Plus resection of contiguous organ; example: small bowel, bladder
351
Colon continued
50 Total colectomy (removal of colon from cecum to the rectosigmoid junction; may include a
portion of the rectum)
51 Plus resection of contiguous organ; example: small bowel, bladder
60 Total proctocolectomy (removal of colon from cecum to the rectosigmoid junction, including the
entire rectum)
61 Plus resection of contiguous organ; example: small bowel, bladder
70 Colectomy or coloproctotectomy with resection of contiguous organ(s), NOS (where there is not
enough information to code 32, 41, 51, or 61)
Code 70 includes: Any colectomy (partial, hemicolectomy, or total) WITH a resection of any other
organs in continuity with the primary site. Other organs may be partially or totally removed.
Other organs may include, but are not limited to, oophorectomy, partial proctectomy, rectal
mucosectomy, or pelvic exenteration.
80 Colectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
352
Rectosigmoid
C19.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Code removal/surgical ablation of single or multiple liver metastases under the data item Surgical
Procedure/Other Site (NAACCR Item #1294).
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser ablation
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Wedge or segmental resection; partial proctosigmoidectomy, NOS
31 Plus resection of contiguous organs; example: small bowel, bladder
Procedures coded 30 include, but are not limited to:
Anterior resection
Hartmann operation
Low anterior resection (LAR)
Partial colectomy, NOS
Rectosigmoidectomy, NOS
Sigmoidectomy
40 Pull through WITH sphincter preservation (colo-anal anastomosis)
50 Total proctectomy
353
Rectosigmoid continued
51 Total colectomy
55 Total colectomy WITH ileostomy, NOS
56 Ileorectal reconstruction
57 Total colectomy WITH other pouch; example: Koch pouch
60 Total proctocolectomy, NOS
65 Total proctocolectomy WITH ileostomy, NOS
66 Total proctocolectomy WITH ileostomy and pouch
Removal of the colon from cecum to the rectosigmoid or a portion of the rectum.
70 Colectomy or proctocolectomy resection in continuity with other organs; pelvic exenteration
80 Colectomy, NOS; Proctectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
354
Rectum
C20.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Code removal/surgical ablation of single or multiple liver metastases under the data item Surgical
Procedure/Other Site (NAACCR Item #1294).
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
27 Excisional biopsy
26 Polypectomy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
28 Curette and fulguration
30 Wedge or segmental resection; partial proctectomy, NOS
Procedures coded 30 include, but are not limited to:
Anterior resection
Hartmann’s operation
Low anterior resection (LAR)
Transsacral rectosigmoidectomy
Total mesorectal excision (TME)
40 Pull through WITH sphincter preservation (coloanal anastomosis)
50 Total proctectomy
Procedure coded 50 includes, but is not limited to:
Abdominoperineal resection (Miles Procedure)
355
Rectum continued
60 Total proctocolectomy, NOS
70 Proctectomy or proctocolectomy with resection in continuity with other organs; pelvic
exenteration
80 Proctectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 05/10, 01/16
356
Anus
C21.0-C21.8
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Thermal Ablation
No specimen sent to pathology from surgical events 10-15.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
60 Abdominal perineal resection, NOS (APR; Miles procedure)
61 APR and sentinel node excision
62 APR and unilateral inguinal lymph node dissection
63 APR and bilateral inguinal lymph node dissection
357
Anus continued
The lymph node dissection should also be coded under Scope of Regional Lymph Node Surgery
(NAACCR Item #1292) or Scope of Regional Lymph Node Surgery at this Facility (NAACCR Item
#672).
Specimen sent to pathology from surgical events 20-63.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
358
Liver and Intrahepatic Bile Ducts
C22.0-C22.1
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Alcohol (Percutaneous Ethanol Injection-PEI)
16 Heat-Radio-frequency ablation (RFA)
17 Other (ultrasound, acetic acid)
No specimen sent to pathology from surgical events 10-17.
20 Wedge or segmental resection, NOS
21 Wedge resection
22 Segmental resection, NOS
23 One
24 Two
25 Three
26 Segmental resection AND local tumor destruction
30 Lobectomy, NOS
36 Right lobectomy
37 Left lobectomy
38 Lobectomy AND local tumor destruction
50 Extended lobectomy, NOS (extended: resection of a single lobe plus a segment of another lobe)
359
Liver and Intrahepatic Bile Ducts continued
51 Right lobectomy
52 Left lobectomy
59 Extended lobectomy AND local tumor destruction
60 Hepatectomy, NOS
61 Total hepatectomy and transplant
65 Excision of a bile duct (for an intra-hepatic bile duct primary only)
66 Excision of an intrahepatic bile duct PLUS partial hepatectomy
75 Extrahepatic bile duct and hepatectomy WITH transplant
Specimen sent to pathology from surgical events 20-75.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/11, 01/16
360
Pancreas
C25.0-C25.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
25 Local excision of tumor, NOS
30 Partial pancreatectomy, NOS; example: distal
35 Local or partial pancreatectomy and duodenectomy
36 WITHOUT distal/partial gastrectomy
37 WITH partial gastrectomy (Whipple)
40 Total pancreatectomy
60 Total pancreatectomy and subtotal gastrectomy or duodenectomy
70 Extended pancreatoduodenectomy
80 Pancreatectomy, NOS
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
361
Larynx
C32.0-C32.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Stripping
No specimen sent to pathology from surgical events 10-15.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
28 Stripping
30 Partial excision of the primary site, NOS; subtotal/partial laryngectomy NOS; hemilaryngectomy
NOS
31 Vertical laryngectomy
32 Anterior commissure laryngectomy
33 Supraglottic laryngectomy
362
Larynx continued
40 Total or radical laryngectomy, NOS
41 Total laryngectomy ONLY
42 Radical laryngectomy ONLY
50 Pharyngolaryngectomy
80 Laryngectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
363
Lung
C34.0-C34.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
19 Local tumor destruction or excision, NOS
Unknown whether a specimen was sent to pathology for surgical events coded 19 (principally
for cases diagnosed prior to January 1, 2003).
15 Local tumor destruction, NOS
12 Laser ablation or cryosurgery
13 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
No specimen sent to pathology from surgical events 12-13 and 15.
20 Excision or resection of less than one lobe, NOS
23 Excision, NOS
24 Laser excision
25 Bronchial sleeve resection ONLY
21 Wedge resection
22 Segmental resection, including lingulectomy
30 Resection of lobe or bilobectomy, but less than the whole lung (partial pneumonectomy, NOS)
33 Lobectomy WITH mediastinal lymph node dissection
The lymph node dissection should also be coded under Scope of Regional Lymph Node Surgery
(NAACCR Item #1292) or Scope of Regional Lymph Node Surgery at this Facility (NAACCR Item #672).
45 Lobe or bilobectomy extended, NOS
46 WITH chest wall
47 WITH pericardium
48 WITH diaphragm
55 Pneumonectomy, NOS
364
Lung continued
56 WITH mediastinal lymph node dissection (radical pneumonectomy)
The lymph node dissection should also be coded under Scope of Regional Lymph Node Surgery
(NAACCR Item #1292) or Scope of Regional Lymph Node Surgery at this Facility (NAACCR Item
#672).
65 Extended pneumonectomy
66 Extended pneumonectomy plus pleura or diaphragm
70 Extended radical pneumonectomy
The lymph node dissection should also be coded under Scope of Regional Lymph Node Surgery
(NAACCR Item #1292) or Scope of Regional Lymph Node Surgery at this Facility (NAACCR Item
#672).
80 Resection of lung, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
365
Hematopoietic/Reticuloendothelial/Immunoproliferative/Myeloprolifer
ative Disease
C42.0, C42.1, C42.3, C42.4 (with any histology)
OR
Any site (with M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-
9992)
Code
98 All hematopoietic/reticuloendothelial/immunoproliferative/myeloproliferative disease sites
and/or histologies, WITH or WITHOUT surgical treatment.
Surgical procedures for hematopoietic/reticuloendothelial/immunoproliferative/
myeloproliferative primaries are to be recorded using the data item Surgical Procedure/Other
Site (NAACCR Item #1294) or Surgical Procedure/Other Site at this Facility (NAACCR Item #674).
Revised 01/04, 01/10, 02/10, 01/16
366
Bones, Joints and Articular Cartilage, Peripheral Nerves and Autonomic
Nervous System, and Connective, Subcutaneous and Other Soft Tissues
Bones, Joints and Articular Cartilage C40.0-C41.9, Peripheral Nerves and Autonomic Nervous System
C47.0-C47.9, Connective, Subcutaneous and Other Soft Tissues C49.0-C49.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
19 Local tumor destruction or excision, NOS
Unknown whether a specimen was sent to pathology for surgical events coded 19 (principally for
cases diagnosed prior to January 1, 2003).
15 Local tumor destruction
No specimen sent to pathology from surgical event 15.
25 Local excision
26 Partial resection
30 Radical excision or resection of lesion WITH limb salvage
40 Amputation of limb
41 Partial amputation of limb
42 Total amputation of limb
50 Major amputation, NOS
51 Forequarter, including scapula
52 Hindquarter, including ilium/hip bone
53 Hemipelvectomy, NOS
54 Internal hemipelvectomy
Specimen sent to pathology from surgical events 25-54.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 8/17/02, 01/10, 02/10, 01/16
367
Spleen
C42.2
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
19 Local tumor destruction or excision, NOS
Unknown whether a specimen was sent to pathology for surgical events coded 19 (principally for
cases diagnosed prior to January 1, 2003).
21 Partial splenectomy
22 Total splenectomy
80 Splenectomy, NOS
Specimen sent to pathology for surgical events 21-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
368
Skin
C44.0-C44.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser ablation
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Biopsy of primary tumor followed by a gross excision of the lesion (does not have to be done
under the same anesthesia)
31 Shave biopsy followed by a gross excision of the lesion
32 Punch biopsy followed by a gross excision of the lesion
33 Incisional biopsy followed by a gross excision of the lesion
34 Mohs surgery, NOS

369
Skin continued
35 Mohs with 1-cm margin or less
36 Mohs with more than 1-cm margin
45 Wide excision or reexcision of lesion or minor (local) amputation with margins more than 1 cm,
NOS. Margins MUST be microscopically negative.
46 WITH margins more than 1 cm and less than or equal to 2 cm
47 WITH margins greater than 2 cm
If the excision or reexcision has microscopically confirmed negative margins less than 1 cm OR
the margins are more than 1 cm but are not microscopically confirmed; use the appropriate
code, 20-36.
60 Major amputation
Specimen sent to pathology from surgical events 20-60.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/15, 01/16
370
Breast
C50.0-C50.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
19 Local tumor destruction, NOS
No specimen was sent to pathology for surgical events coded 19 (principally for cases diagnosed prior
to January 1, 2003).
20 Partial mastectomy, NOS; less than total mastectomy, NOS
21 Partial mastectomy WITH nipple resection
22 Lumpectomy or excisional biopsy
23 Reexcision of the biopsy site for gross or microscopic residual disease
24 Segmental mastectomy (including wedge resection, quadrantectomy, tylectomy)
Procedures coded 20-24 remove the gross primary tumor and some of the breast tissue
(breast-conserving or preserving). There may be microscopic residual tumor.
30 Subcutaneous mastectomy
A subcutaneous mastectomy, also called a nipple sparing mastectomy, is the removal of breast
tissue without the nipple and areolar complex or overlying skin. It is performed to facilitate
immediate breast reconstruction. Cases coded 30 may be considered to have undergone breast
reconstruction.
40 Total (simple) mastectomy
41 WITHOUT removal of uninvolved contralateral breast
43 With reconstruction NOS
44 Tissue
45 Implant
46 Combined (Tissue and Implant)
42 WITH removal of uninvolved contralateral breast
371
Breast continued
47 With reconstruction NOS
48 Tissue
49 Implant
75 Combined (Tissue and Implant)
A total (simple) mastectomy removes all breast tissue, the nipple, and areolar complex. An
axillary dissection is not done, but sentinel lymph nodes may be removed.
For single primaries only, code removal of the involved contralateral breast under the data
item Surgical Procedure/Other Site (NAACCR Item #1294) and/or Surgical Procedure/Other
Site at this Facility (NAACCR Item #674).
If the contralateral breast reveals a second primary, each breast is abstracted separately. The
surgical procedure is coded 41 for the first primary. The surgical code for the contralateral
breast is coded to the procedure performed on that site.
Reconstruction that is planned as part of first course treatment is coded 43-49 or 75, whether it
is done at the time of mastectomy or later.
76 Bilateral mastectomy for a single tumor involving both breasts, as for bilateral inflammatory
carcinoma.
50 Modified radical mastectomy
51 WITHOUT removal of uninvolved contralateral breast
53 Reconstruction, NOS
54 Tissue
55 Implant
56 Combined (Tissue and Implant)
52 WITH removal of uninvolved contralateral breast
57 Reconstruction, NOS
58 Tissue
59 Implant
63 Combined (Tissue and Implant)
Removal of all breast tissue, the nipple, the areolar complex, and variable amounts of breast
skin in continuity with the axilla. The specimen may or may not include a portion of the
pectoralis major muscle
372
Breast continued
If contralateral breast reveals a second primary, it is abstracted separately. The surgical
procedure is coded 51 for the first primary. The surgical code for the contralateral breast is
coded to the procedure performed on that site.
For single primaries only, code removal of involved contralateral breast under the data item
Surgical Procedure/Other Site (NAACCR Item #1294) or Surgical Procedure/Other Site at this
Facility (NAACCR Item #674).
60 Radical mastectomy, NOS
61 WITHOUT removal of uninvolved contralateral breast
64 Reconstruction, NOS
65 Tissue
66 Implant
67 Combined (Tissue and Implant)
62 WITH removal of uninvolved contralateral breast
68 Reconstruction, NOS
69 Tissue
73 Implant
74 Combined (Tissue and Implant)
70 Extended radical mastectomy
71 WITHOUT removal of uninvolved contralateral breast
72 WITH removal of uninvolved contralateral breast
80 Mastectomy, NOS
Specimen sent to pathology for surgical events coded 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 05/10, 01/11, 01/13, 01/16
373
Cervix Uteri
C53.0-C53.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
For invasive cancers, dilation and curettage is coded as an incisional biopsy (02) under the data item
Surgical Diagnostic and Staging Procedure (NAACCR Item #1350).
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Loop Electrocautery Excision Procedure (LEEP)
16 Laser ablation
17 Thermal ablation
No specimen sent to pathology from surgical events 10-17.
20 Local tumor excision, NOS
26 Excisional biopsy, NOS
27 Cone biopsy
24 Cone biopsy WITH gross excision of lesion
29 Trachelectomy; removal of cervical stump; cervicectomy
Any combination of 20, 24, 26, 27 or 29 WITH
21 Electrocautery
22 Cryosurgery
23 Laser ablation or excision
25 Dilatation and curettage; endocervical curettage (for in situ only)
28 Loop electrocautery excision procedure (LEEP)
374
Cervix Uteri continued
30 Total hysterectomy (simple, pan-) WITHOUT removal of tubes and ovaries
Total hysterectomy removes both the corpus and cervix uteri and may also include a portion of
vaginal cuff.
40 Total hysterectomy (simple, pan-) WITH removal of tubes and/or ovary
Total hysterectomy removes both the corpus and cervix uteri and may also include a portion of
vaginal cuff.
50 Modified radical or extended hysterectomy; radical hysterectomy; extended radical hysterectomy
51 Modified radical hysterectomy
52 Extended hysterectomy
53 Radical hysterectomy; Wertheim procedure
54 Extended radical hysterectomy
60 Hysterectomy, NOS, WITH or WITHOUT removal of tubes and ovaries
61 WITHOUT removal of tubes and ovaries
62 WITH removal of tubes and ovaries
70 Pelvic exenteration
71 Anterior exenteration
Includes bladder, distal ureters, and genital organs WITH their ligamentous attachments and
pelvic lymph nodes.
72 Posterior exenteration
Includes rectum and rectosigmoid WITH ligamentous attachments and pelvic lymph nodes.
73 Total exenteration
Includes removal of all pelvic contents and pelvic lymph nodes.
74 Extended exenteration
Includes pelvic blood vessels or bony pelvis.
Specimen sent to pathology from surgical events 20-74.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
375
Corpus Uteri
C54.0-C55.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
For invasive cancers, dilation and curettage is coded as an incisional biopsy (02) under the data item
Surgical Diagnostic and Staging Procedure (NAACCR Item #1350).
Codes
00 None; no surgery of primary site
19 Local tumor destruction or excision, NOS
Unknown whether a specimen was sent to pathology for surgical events coded 19 (principally for
cases diagnosed prior to January 1, 2003).
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Loop Electocautery Excision Procedure (LEEP)
16 Thermal ablation
No specimen sent to pathology from surgical events 10-16.
20 Local tumor excision, NOS; simple excision, NOS
24 Excisional biopsy
25 Polypectomy
26 Myomectomy
Any combination of 20 or 24-26 WITH
21 Electrocautery
22 Cryosurgery
23 Laser ablation or excision
30 Subtotal hysterectomy/supracervical hysterectomy/fundectomy WITH or WITHOUT removal of
tube(s) and ovary(ies).
376
Corpus Uteri continued
31 WITHOUT tube(s) and ovary(ies)
32 WITH tube(s) and ovary(ies)
40 Total hysterectomy (simple, pan-) WITHOUT removal of tube(s) and ovary(ies)
Removes both the corpus and cervix uteri. It may also include a portion of the vaginal cuff.
50 Total hysterectomy (simple, pan-) WITH removal of tube(s) and/or ovary(ies)
Removes both the corpus and cervix uteri. It may also include a portion of the vaginal cuff.
60 Modified radical or extended hysterectomy; radical hysterectomy; extended radical hysterectomy
61 Modified radical hysterectomy
62 Extended hysterectomy
63 Radical hysterectomy; Wertheim procedure
64 Extended radical hysterectomy
65 Hysterectomy, NOS, WITH or WITHOUT removal of tube(s) and ovary(ies)
66 WITHOUT removal of tube(s) and ovary(ies)
67 WITH removal of tube(s) and ovary(ies)
75 Pelvic exenteration
76 Anterior exenteration
Includes bladder, distal ureters, and genital organs WITH their ligamentous attachments and
pelvic lymph nodes.
77 Posterior exenteration
Includes rectum and rectosigmoid WITH ligamentous attachments and pelvic lymph nodes.
78 Total exenteration
Includes removal of all pelvic contents and pelvic lymph nodes.
79 Extended exenteration
Includes pelvic blood vessels or bony pelvis.
Specimen sent to pathology from surgical events 20-79.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
377
Ovary
C56.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
17 Local tumor destruction, NOS
No specimen sent to pathology from surgical event 17.
25 Total removal of tumor or (single) ovary, NOS
26 Resection of ovary (wedge, subtotal, or partial) ONLY, NOS; unknown if hysterectomy
done
27 WITHOUT hysterectomy
28 WITH hysterectomy
35 Unilateral (salpingo-)oophorectomy; unknown if hysterectomy done
36 WITHOUT hysterectomy
37 WITH hysterectomy
50 Bilateral (salpingo-)oophorectomy; unknown if hysterectomy done
51 WITHOUT hysterectomy
52 WITH hysterectomy
55 Unilateral or bilateral (salpingo-)oophorectomy WITH OMENTECTOMY, NOS; partial or total;
unknown if hysterectomy done
56 WITHOUT hysterectomy
57 WITH hysterectomy
60 Debulking; cytoreductive surgery, NOS
61 WITH colon (including appendix) and/or small intestine resection (not incidental)
62 WITH partial resection of urinary tract (not incidental)
63 Combination of 61 and 62
378
Ovary continued
Debulking is a partial or total removal of the tumor mass and can involve the removal of
multiple organ sites. It may include removal of ovaries and/or the uterus (a hysterectomy). The
pathology report may or may not identify ovarian tissue. A debulking is usually followed by
another treatment modality such as chemotherapy.
70 Pelvic exenteration, NOS
71 Anterior exenteration
Includes bladder, distal ureters, and genital organs WITH their ligamentous attachments and
pelvic lymph nodes.
72 Posterior exenteration
Includes rectum and rectosigmoid WITH ligamentous attachments and pelvic lymph nodes.
73 Total exenteration
Includes removal of all pelvic contents and pelvic lymph nodes.
74 Extended exenteration
Includes pelvic blood vessels or bony pelvis
80 (Salpingo-)oophorectomy, NOS
Specimen sent to pathology from surgical events 25-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
379
Prostate
C61.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Do not code an orchiectomy in this field. For prostate primaries, orchiectomies are coded in the data
item Hematologic Transplant and Endocrine Procedures (NAACCR Item #3250).
Codes
00 None; no surgery of primary site
18 Local tumor destruction or excision, NOS
19 Transurethral resection (TURP), NOS, and no specimen sent to pathology or unknown if sent
Unknown whether a specimen was sent to pathology for surgical events coded 18 or 19 (principally
for cases diagnosed prior to January 1, 2003).
10 Local tumor destruction, NOS
14 Cryoprostatectomy
15 Laser ablation
16 Hyperthermia
17 Other method of local tumor destruction
No specimen sent to pathology from surgical events 10-17.
20 Local tumor excision, NOS
21 Transurethral resection (TURP), NOS, with specimen sent to pathology
22 TURP-cancer is incidental finding during surgery for benign disease
23 TURP-patient has suspected/known cancer
Any combination of 20-23 WITH
24 Cryosurgery
25 Laser
26 Hyperthermia
30 Subtotal, segmental, or simple prostatectomy, which may leave all or part of the capsule intact
50 Radical prostatectomy, NOS; total prostatectomy, NOS
Excised prostate, prostatic capsule, ejaculatory ducts, seminal vesicle(s) and may include a
narrow cuff of bladder neck.
380
Prostate continued
70 Prostatectomy WITH resection in continuity with other organs; pelvic exenteration
Surgeries coded 70 are any prostatectomy WITH resection in continuity with any other organs.
The other organs may be partially or totally removed. Procedures may include, but are not
limited to, cystoprostatectomy, radical cystectomy, and prostatectomy.
80 Prostatectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 12/4/02, 01/10, 02/10, 1/11, 01/16
381
Testis
C62.0-C62.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
12 Local tumor destruction, NOS
No specimen sent to pathology from surgical event 12.
20 Local or partial excision of testicle
30 Excision of testicle WITHOUT cord
40 Excision of testicle WITH cord or cord not mentioned (radical orchiectomy)
80 Orchiectomy, NOS (unspecified whether partial or total testicle removed)
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
382
Kidney, Renal Pelvis, and Ureter
Kidney C64.9, Renal Pelvis C65.9, Ureter C66.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Thermal ablation
No specimen sent to pathology from this surgical event 10-15.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Partial or subtotal nephrectomy (kidney or renal pelvis) or partial ureterectomy (ureter)
Procedures coded 30 include, but are not limited to:
Segmental resection
Wedge resection
383
Kidney, Renal Pelvis, and Ureter continued
40 Complete/total/simple nephrectomy-for kidney parenchyma
Nephroureterectomy
Includes bladder cuff for renal pelvis or ureter.
50 Radical nephrectomy
May include removal of a portion of vena cava, adrenal gland(s), Gerota’s fascia, perinephric
fat, or partial/total ureter.
70 Any nephrectomy (simple, subtotal, complete, partial, simple, total, radical) in continuity with the
resection of other organ(s) (colon, bladder)
The other organs, such as colon or bladder, may be partially or totally removed.
80 Nephrectomy, NOS
Ureterectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/16
384
Bladder
C67.0-C67.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
15 Intravesical therapy
16 Bacillus Calmette-Guerin (BCG) or other immunotherapy
Also code the introduction of immunotherapy in the immunotherapy items. If immunotherapy
is followed by surgery of the type coded 20-80 code that surgery instead and code the
immunotherapy only as immunotherapy.
No specimen sent to pathology from surgical events 10-16.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Partial cystectomy
50 Simple/total/complete cystectomy
60 Complete cystectomy with reconstruction
61 Radical cystectomy PLUS ileal conduit
385
Bladder continued
62 Radical cystectomy PLUS continent reservoir or pouch, NOS
63 Radical cystectomy PLUS abdominal pouch (cutaneous)
64 Radical cystectomy PLUS in situ pouch (orthotopic)
When the procedure is described as a pelvic exenteration for males, but the prostate is not
removed, the surgery should be coded as a cystectomy (code 60-64).
70 Pelvic exenteration, NOS
71 Radical cystectomy including anterior exenteration
For females, includes removal of bladder, uterus, ovaries, entire vaginal wall, and entire
urethra. For males, includes removal of the prostate. When a procedure is described as a
pelvic exenteration for males, but the prostate is not removed, the surgery should be coded as
a cystectomy (code 60-64).
72 Posterior exenteration
For females, also includes removal of vagina, rectum and anus. For males, also includes
prostate, rectum and anus.
73 Total exenteration
Includes all tissue and organs removed for an anterior and posterior exenteration.
74 Extended exenteration
Includes pelvic blood vessels or bony pelvis.
80 Cystectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/12, 01/16
386
Brain
Meninges C70.0-C70.9, Brain C71.0-C71.9,
Spinal Cord, Cranial Nerves and Other Parts of Central Nervous System C72.0-C72.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Do not code laminectomies for spinal cord primaries.
Codes
00 None; no surgery of primary site
10 Tumor destruction, NOS
No specimen sent to pathology from surgical event 10.
Do not record stereotactic radiosurgery (SRS), Gamma knife, Cyber knife, or Linac radiosurgery as
surgical tumor destruction. All of these modalities are recorded in the radiation treatment fields.
20 Local excision of tumor, lesion or mass; excisional biopsy
21 Subtotal resection of tumor, lesion or mass in brain
22 Resection of tumor of spinal cord or nerve
30 Radical, total, gross resection of tumor, lesion or mass in brain
40 Partial resection of lobe of brain, when the surgery can not be coded as 20-30.
55 Gross total resection of lobe of brain (lobectomy)
Codes 30 - 55 are not applicable for spinal cord or spinal nerve primary sites.
Specimen sent to pathology from surgical events 20-55.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
387
Thyroid Gland
C73.9
(Except for M9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
13 Local tumor destruction, NOS
No specimen sent to pathology from surgical event 13.
25 Removal of less than a lobe, NOS
26 Local surgical excision
27 Removal of a partial lobe ONLY
20 Lobectomy and/or isthmectomy
21 Lobectomy ONLY
22 Isthmectomy ONLY
23 Lobectomy WITH isthmus
30 Removal of a lobe and partial removal of the contralateral lobe
40 Subtotal or near total thyroidectomy
50 Total thyroidectomy
80 Thyroidectomy, NOS
Specimen sent to pathology from surgical events 20-80.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/10, 02/10, 01/15, 01/16
388
Lymph Nodes
C77.0-C77.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
19 Local tumor destruction or excision, NOS
Unknown whether a specimen was sent to pathology for surgical events coded to 19 (principally for
cases diagnosed prior to January 1, 2003).
15 Local tumor destruction, NOS
No specimen sent to pathology from surgical event 15.
25 Local tumor excision, NOS
Less than a full chain, includes an excisional biopsy of a single lymph node.
30 Lymph node dissection, NOS
31 One chain
32 Two or more chains
40 Lymph node dissection, NOS PLUS splenectomy
41 One chain
42 Two or more chains
50 Lymph node dissection, NOS and partial/total removal of adjacent organ(s)
51 One chain
52 Two or more chains
60 Lymph node dissection, NOS and partial/total removal of adjacent organ(s) PLUS splenectomy
(Includes staging laparotomy for lymphoma.)
61 One chain
62 Two or more chains
Specimen sent to pathology for surgical events 25-62.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 09/04, 01/10, 02/10, 01/16
389
All Other Sites
C14.2-C14.8, C17.0-C17.9, C23.9, C24.0-C24.9, C26.0-C26.9, C30.0-C 30.1, C31.0-C31.9, C33.9, C37.9,
C38.0-C38.8, C39.0-C39.9, C48.0-C48.8, C51.0-C51.9, C52.9, C57.0-C57.9, C58.9, C60.0-C60.9, C63.0-
C63.9, C68.0-C68.9, C69.0-C69.9, C74.0-C74.9, C75.0-C75.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Codes
00 None; no surgery of primary site
10 Local tumor destruction, NOS
11 Photodynamic therapy (PDT)
12 Electrocautery; fulguration (includes use of hot forceps for tumor destruction)
13 Cryosurgery
14 Laser
No specimen sent to pathology from surgical events 10-14.
20 Local tumor excision, NOS
26 Polypectomy
27 Excisional biopsy
Any combination of 20 or 26-27 WITH
21 Photodynamic therapy (PDT)
22 Electrocautery
23 Cryosurgery
24 Laser ablation
25 Laser excision
30 Simple/partial surgical removal of primary site
40 Total surgical removal of primary site; enucleation
41 Total enucleation (for eye surgery only)
50 Surgery stated to be “debulking”
60 Radical surgery
390
All Other Sites, continued
Partial or total removal of the primary site WITH a resection in continuity (partial or total
removal) with other organs.
Specimen sent to pathology from surgical events 20-60.
90 Surgery, NOS
99 Unknown if surgery performed
Revised 01/04, 01/10, 02/10, 01/16
391
Unknown and Ill-Defined Primary Sites
C76.0-C76.8, C80.9
(Except for M-9727, 9732, 9741-9742, 9762-9809, 9832, 9840-9931, 9945-9946, 9950-9967, 9975-9992)
Code
98 All unknown and ill-defined disease sites, WITH or WITHOUT surgical treatment.
Surgical procedures for unknown and ill-defined primaries are to be recorded using the data
item Surgical Procedure/Other Site (NAACCR Item #1294) or Surgical Procedure/Other Site at
this Facility (NAACCR Item #674).
Revised 01/04, 01/10, 02/10, 01/16



