
1
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
11
The UK immunisation schedule
The routine immunisation schedule
The overall aim of the routine immunisation schedule is to provide protection against the
following vaccine-preventable infections:
●
diphtheria
●
Haemophilus influenzae type b (Hib)
●
hepatitis B
●
human papillomavirus (certain serotypes)
●
influenza
●
measles
●
meningococcal disease (certain serogroups)
●
mumps
●
pertussis (whooping cough)
●
pneumococcal disease (certain serotypes)
●
polio
●
rotavirus
●
rubella
●
shingles
●
tetanus
The schedule for routine immunisations and instructions for how they should be
administered are given in Table 11.1. The relevant chapters on each of these vaccine-
preventable diseases provide detailed information about the vaccines and the immunisation
programmes.

2
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
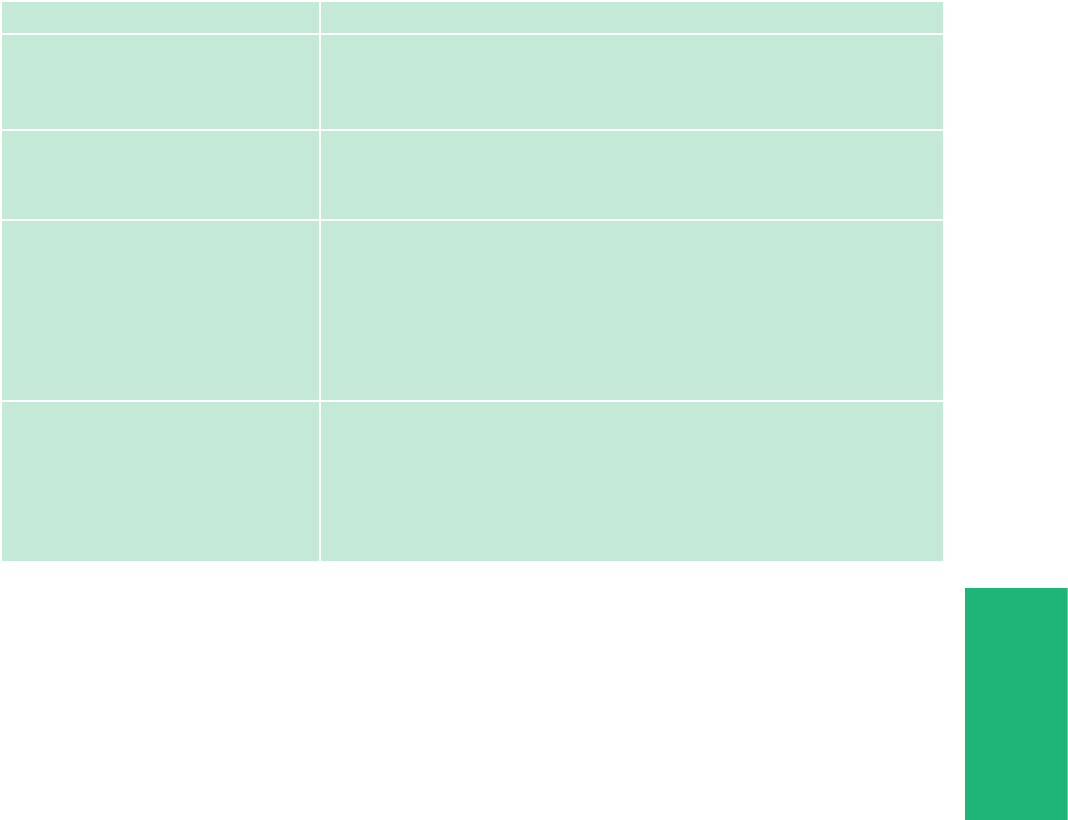
Table 11.1 Schedule for the UK’s routine immunisation programme (excluding catch-
up campaigns)
Age due Vaccine given
How it is given
1
Eight weeks old Diphtheria, tetanus, pertussis, polio,
Haemophilus influenzae type b (Hib) and
hepatitis B (DTaP/IPV/Hib/HepB)
Meningococcal B (MenB)
Rotavirus
One injection
One injection
One oral application
Twelve weeks old Diphtheria, tetanus, pertussis, polio, Hib
and hepatitis B (DTaP/IPV/Hib/HepB)
Rotavirus
Pneumococcal conjugate vaccine (PCV13)
One injection
One oral application
One injection
Sixteen weeks old Diphtheria, tetanus, pertussis, polio, Hib
and hepatitis B (DTaP/IPV/Hib/HepB)
Meningococcal B (MenB)
One injection
One injection
One year old (on or
after the child’s first
birthday)
Hib/MenC
Pneumococcal conjugate vaccine (PCV13)
Meningococcal B (MenB)
Measles, mumps and rubella (MMR)
One injection
2
One injection
2
One injection
2
One injection
2
Eligible paediatric
age groups
Chapter 19)
Live attenuated influenza vaccine (LAIV) Nasal spray, single application
in each nostril
(if LAIV is contraindicated and
child is in a clinical risk group,
give inactivated flu vaccine;
see Chapter 19)
Three years four
months old or soon
after
Diphtheria, tetanus, pertussis and polio
(dTaP/IPV)
Measles, mumps and rubella (MMR)
One injection
One injection
Twelve to thirteen
years old
Human papillomavirus (HPV) Course of two injections at
least six months apart
Fourteen years old
(school year 9)
Tetanus, diphtheria and polio (Td/IPV)
Meningococcal ACWY conjugate
(MenACWY)
One injection
One injection
65 years old Pneumococcal polysaccharide vaccine (PPV) One injection
65 years of age and
older
Inactivated influenza vaccine One injection annually
70 years old Shingles vaccine One injection (live vaccine)
Two injections (inactivated
vaccine)
1 Where two or more injections are required at the same time, these should ideally be given in different
limbs. Where this is not possible, injections in the same limb should be given at least 2.5cm apart.
2 Where injections can only be given in two limbs, it is recommended that the MMR, as the vaccine least
likely to cause local reactions, is given in the same limb as the MenB with the PCV13 and Hib/MenC doses
given into the other limb.

3
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
The childhood immunisation schedule has been designed to provide early protection
against infections that are most dangerous for the very young. This is particularly important
for diseases such as whooping cough, rotavirus and those due to pneumococcal, Hib and
meningococcal infections. Providing subsequent booster doses as scheduled should ensure
continued protection. Further vaccinations are offered throughout life to provide protection
against infections when eligible individuals reach an age where they can derive most
benefit (such as because of an increased individual risk) or where the programme will
provide optimal control of that disease for the whole population.
Recommendations for the age at which vaccines should be administered are informed by
the age-specific risk for a disease, the risk of disease complications, the ability to respond
to the vaccine and the impact on spread in the population. The schedule should therefore
be followed as closely as possible.
Some individuals may be eligible for additional vaccines due to an underlying medical
condition or circumstances that put them at increased risk of catching a vaccine-
preventable disease or of complications from that disease. These individuals should be
vaccinated in accordance with the recommendations in Chapter 7 and the disease specific
chapters.
Seasonal influenza
Those eligible for influenza vaccine (on the basis of age or clinical risk) should be
vaccinated each winter, usually between October and January, although vaccination may
still be of some benefit if given later. The annual letters on the influenza programme
should be consulted for age eligibility:
England: www.gov.uk/government/collections/annual-flu-programme
Northern Ireland: www.health-ni.gov.uk/topics/professional-medical-and- environmental-
health-advice/hssmd-letters-and-urgent-communications
Scotland:www.sehd.scot.nhs.uk/index.asp
Wales: gweddill.gov.wales/topics/health/nhswales/circulars/public-health/?lang=en

4
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
Schedule flexibility
The schedule recommended by the Joint Committee on Vaccination and Immunisation
(JCVI) incorporates the minimum intervals between subsequent doses of the same vaccine.
As immunological memory from priming dose(s) are likely to be maintained in healthy
individuals, increasing that interval will usually lead to a more pronounced response to the
later dose. Therefore, where any course of immunisation is interrupted, there is
normally no need to start the course again - it should simply be resumed and
completed as soon as possible. Where vaccination was commenced some time
previously however, the product received, or the eligibility may have changed, and the
relevant chapter should therefore be consulted.
Immunisations should not be given before the scheduled age unless there is a clear clinical
indication for this. The first set of primary immunisations can be given from six weeks of
age if required in certain circumstances such as travel to an endemic country. Administering
the first set of primary immunisations before 6 weeks of age is not recommended, as it
may result in a sub-optimal response to the vaccine which could undermine good control.
MMR vaccine can be given from six months of age, for example during a local outbreak or
if travelling to a high incidence country. Any dose of MMR given below the age of one
year should be discounted as residual maternal antibodies may reduce the response to the
vaccine. Two further doses of MMR will therefore be required at the appropriate ages.
Delaying primary infant immunisations beyond eight weeks risks leaving babies
unprotected against serious infections that can be very severe in the very young, such as
whooping cough. The six to eight week baby check is not required as part of the
assessment for immunisation, and so the eight week primary immunisations should never
be delayed because of any delay in carrying out this examination.
Every effort should be made to ensure that all children and adults are immunised, even if
they are older than the scheduled age; no opportunity to immunise should be missed. The
type of vaccine and number of doses recommended depends on the age of the individual
as some vaccines are not indicated after a certain age. In most instances, this is because
the ability to benefit from vaccination is reduced because of lower risk (e.g. whooping
cough), or lower effectiveness (e.g. for shingles). The exception is rotavirus vaccine, where
vaccination at an older age is more likely to be associated with an adverse event
(intussusception) (see Chapter 27b: Rotavirus for more information).
Recording of immunisation
Following immunisation, all the patient’s clinical records including the GP held record and,
if a child, the record on the Child Health Information System (CHIS) and the Personal Child
Health Record (Red Book) should be updated with all the relevant details (see Chapter 4).
When babies are immunised in special care units, or children and adolescents are
immunised opportunistically in accident and emergency units or inpatient facilities, it is
important that a record of the immunisation is entered onto the relevant CHIS and sent to
the patient’s GP for entry onto the practice-held patient record. Details should also be
recorded in the child’s Personal Child Health Record (Red Book) in a timely manner. Details
of vaccines given in other areas, such as schools/maternity services/pharmacies, should also
be sent to the patient’s GP.

5
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
Where possible, records of immunisation should be requested from children and adults
arriving from overseas and entered onto the GP held record and other clinical records as
appropriate. This will avoid the individual being flagged for vaccination and provide
reassurance during local outbreaks.
A toolkit with information on the vaccines used in several other countries can be
downloaded to facilitate accurate coding at the following:
https://www.gov.uk/government/publications/uk-and-international-immunisation-schedules-
comparison-tool
Childhood immunisation programme
When children attend for any vaccination, it is important to also check that they are up-to-
date for any vaccines that they should have received previously. The table below gives an
example checklist at each key stage; doses of those vaccines that have not been received
but are still indicated at that age should be caught up. Catch-up doses should be
administered as soon as possible but leaving the appropriate intervals as advised in the
relevant chapters.
At a minimum, children’s immunisation status should be checked at these key ages, see
Table 11.2, and the child offered catch-up for any missing vaccinations.
Table 11.2 Routine immunisation schedule vaccination history at key ages
Key age Vaccines child should have had or catch-up with
At the age of
12 months:
Three doses of diphtheria, tetanus, polio, pertussis, Hib and hepatitis B containing
vaccine.
A single dose of PCV vaccine.
Two doses of MenB vaccine.
At the age of
24 months:
Three doses of diphtheria, tetanus, polio, pertussis (and hepatitis B) containing
vaccines.
A single dose of Hib/MenC and PCV13 vaccines after the age of one year.
Either 2 doses of MenB under the age of one and one dose after the age of one
year; or 2 doses of MenB after the age of one year.
A single dose of MMR vaccine after the age of one year.
At school
entry:
Four doses of diphtheria, tetanus, pertussis and polio containing vaccine.
Two doses of MMR vaccine after the age of one year.
A single dose of Hib/MenC conjugate vaccine after the age of one year.
At transfer to
secondary
school:
Four doses of diphtheria, tetanus and polio containing vaccine.
Two doses of MMR vaccine after the age of one year.
A single dose of Hib/MenC conjugate vaccine after the age of one year.
Before
leaving
school:
Five doses of diphtheria, tetanus, polio containing vaccine.
A single dose of MenACWY vaccine after the age of 10 years.
Two doses of MMR vaccine.
Two doses of HPV vaccine (at least 6 months apart)
1
1 All Females remain eligible for HPV vaccine up to their twenty-fifth birthday. All males born on/
after 1 September 2006 are eligible up to their twenty-fifth birthday

6
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
Adult immunisation programme
Five doses of diphtheria, tetanus and polio vaccines at the appropriate interval should
ensure long-term protection through adulthood (although additional doses may be
indicated for travel or following potential exposure to infection). Individuals who have not
completed the five doses should have their remaining doses at the appropriate intervals.
Where there is an unclear history of vaccination, adults should be assumed to be
unimmunised. A full course of diphtheria, tetanus and polio vaccine should be offered to
individuals of any age in line with advice contained in the relevant chapters. It is never too
late in life to start a course of vaccination.
Measles, mumps and rubella vaccine should be offered to all young adults who have not
received two doses as outlined in Chapter 21, Chapter 23 and Chapter 28. In particular,
vaccine status should be checked for all women of child-bearing age who should be
offered MMR to prevent rubella in pregnancy. In addition, up to the age of 25 years,
MenACWY vaccine should be offered to individuals who have never received a MenC-
containing vaccine (see Chapter 22) and HPV should be offered to eligible unvaccinated
individuals (see Chapter 18a for eligibility).
Older adults (65 years and older) should routinely be offered a single dose of
pneumococcal polysaccharide vaccine if they have not previously received it. Annual
influenza vaccination should be offered from 65 years of age. Adults aged 70 years
become eligible for shingles vaccine and remain eligible until their 80th birthday. More
information on shingles vaccine eligibility is available at: https://www.gov.uk/government/
collections/shingles- vaccination-programme
Vaccination of individuals with unknown or incomplete immunisation status
For a variety of reasons, some individuals may present not having received some or all their
immunisations or may have an unknown immunisation history. Where an individual born in
the UK presents with an inadequate immunisation history, every effort should be made to
clarify what immunisations they may have had. Anyone who has not completed the
routine immunisation programme as appropriate for their age should have the outstanding
doses as described in the relevant chapters.
If children and adults coming to the UK do not have a documented or reliable verbal
history of immunisation, they should be assumed to be unimmunised and a full course of
required immunisations should be planned.
Individuals coming from areas of conflict or from population groups who may have been
marginalised in their country of origin (such as refugees, gypsy or other nomadic travellers)
may not have had good access to immunisation services. In particular, older children and
adults may also have been raised during periods before immunisation services were well
developed or when vaccine quality was sub-optimal. Where there is no reliable history of
previous immunisation, it should be assumed that any undocumented doses are missing
and the UK catch-up recommendations for that age should be followed.
An algorithm for vaccinating individuals with uncertain or incomplete immunisation status
is available at https://www.gov.uk/government/publications/vaccination-of-individuals-with-
uncertain-or-incomplete-immunisation-status

7
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
Individuals coming to the UK who have a history of completing immunisation in their
country of origin may not have been offered protection against all the antigens currently
offered in the UK. Most countries have offered protection against diphtheria, tetanus, polio
and whooping cough for many years, but do not currently include MenC or MenB in the
schedule and may have introduced PCV and Hib vaccine relatively recently. Many countries
worldwide only offer single measles vaccines, rather than MMR, or have only recently
started to offer a rubella containing vaccine. Measles vaccine is also given below the age
of one year in many lower income countries. Doses of measles-containing vaccine given
below the age of one should be discounted and two further doses of MMR vaccine given
to ensure adequate protection against both measles and rubella.
Current country-specific schedules are available on the WHO website (http://apps.who.int/
immunization_monitoring/globalsummary).
Children coming to the UK may have received a fourth dose of a diphtheria/tetanus/
pertussis-containing vaccine that is given at around 18 months in many countries. Booster
doses given before three years of age should be discounted, as they may not provide
continued satisfactory protection until the time of the teenage booster. The routine pre-
school and subsequent boosters should be given according to the UK schedule.
Premature infants
It is
important that premature infants have their immunisations at the appropriate
chronological age (counted from their date of birth), in accordance with the national
routine immunisation schedule. As the benefit of vaccination is high in this group of
infants, vaccination should not be withheld or delayed.
As the occurrence of apnoea following vaccination is especially increased in infants who
were born very prematurely, specific guidance on the immunisation of premature infants in
Chapter 7 and the disease specific chapters should be followed.
Selective immunisation programmes
There are a number of selective immunisation programmes that target children and adults
at particular risk of serious complications from certain infections, such as hepatitis B,
hepatitis A, influenza, Hib, meningococcal and pneumococcal infection. Other vaccines,
including BCG, HPV, hepatitis B and hepatitis A, are also recommended for individuals at
higher risk of exposure to infection, due to lifestyle factors, close contact or recent
outbreaks in their community.
Individuals at risk of exposure through their work should be advised about any required
vaccinations by their employer or their occupational health service (Chapter 12). For more
information, please see Chapter 7 and the disease specific chapters.
Vaccination during and after pregnancy
In 2010, routine influenza immunisation of individuals was extended to include all
pregnant women. This was based on evidence of the increased risk from influenza to the

8
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
mother and to infants in the first few months of life. Vaccination therefore protects the
woman herself and provides passive immunity to the infant following birth. Preventing
infection in the mother will also reduce the risk of her transmitting influenza to her
newborn baby. Inactivated influenza vaccine should therefore be offered to pregnant
women at any stage of pregnancy (first, second or third trimesters), ideally before influenza
viruses start to circulate. Influenza vaccination is usually carried out between October and
January, but clinical judgement should be used to assess whether a pregnant woman
should be vaccinated after this period. The current level and severity of influenza activity,
the presence of other risk factors and the availability of inactivated influenza vaccine may
form part of the consideration for late vaccination.
A programme for the vaccination of pregnant women against pertussis was introduced in
October 2012. The purpose of the programme is to boost antibodies in these women so
that high levels of passive antibody are transferred from mother to baby. This should
protect the infant against pertussis infection until they can be vaccinated at eight weeks of
age. Pregnant women should be offered dTaP/IPV vaccine from week 16 of each pregnancy
(for operational reasons, vaccination is probably best offered at, or after the foetal anomaly
scan at around 20 weeks). This programme is described in more detail in Chapter 24.
Influenza vaccine can be given at the same time as pertussis vaccine, but influenza
vaccination should not be delayed in order to administer the two vaccines together.
Inactivated influenza vaccines are preferred to the live attenuated vaccine for pregnant
women (see Chapter 19). Pertussis vaccine can be given at the same time as influenza
vaccine but, to avoid compromising the passive protection to the infant, this should not be
used as a reason to give pertussis vaccination outside of the recommended period.
From 2016, the routine antenatal testing of women for rubella susceptibility ceased.
Pregnant women should have their vaccine status checked during or after pregnancy, for
example at the post-natal check, and be offered any outstanding doses of MMR soon after
delivery. MMR vaccine should not be offered in pregnancy.
Intervals between vaccines
Doses of different inactivated vaccines can be administered at any time before, after, or at
the same time as each other. Doses of inactivated vaccines can also be given at any interval
before, after, or at the same time as a live vaccine and vice versa.
A minimum four-week interval is normally recommended between successive doses of the
same vaccine - for example between each of the three doses of DTaP-containing vaccine in
the primary schedule. A better response is made to some vaccines when an eight-week
interval is observed between infant doses. Although shorter intervals may be advised to
achieve more rapid protection, e.g. for travel or during an outbreak, this may lead to a lower
immune response, particularly in infants, and may therefore provide less durable protection. If
one of the infant primary immunisation DTaP-containing vaccine doses is inadvertently or
deliberately given up to a week early (such as for travel) however, the impact on the final
response is minimal. If more than one dose in the three-dose schedule is given early, or one
of the doses is given at less than a three week interval, then that dose should be repeated at
least four weeks after the final dose. Where an infant dose of MenB is inadvertently given at
an interval of less than eight weeks, an additional dose should be administered four weeks
after the second dose to ensure adequate protection whilst still at a vulnerable age.
9
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
For other multiple dose schedules with inactivated vaccines e.g. hepatitis B, giving
subsequent doses at a slightly shorter than the recommended interval is unlikely to be
highly detrimental to the overall immune response. However, early vaccination should be
avoided unless necessary to ensure rapid protection or to improve compliance, and
additional doses may be recommended to ensure longer term protection.
Advice on intervals between different live vaccines is based on existing specific evidence of
interference between vaccines. The current advice is detailed in Table 11.3. Recommended
intervals between subsequent doses of the same live vaccine will depend upon the specific
incubation period of the vaccine virus, and other factors, such as decline in maternally
derived antibody. Please refer to the relevant chapters.
Table 11.3 Recommended time intervals when giving more than one live attenuated
vaccine
Vaccine combinations Recommendations
Yellow Fever and MMR A four week minimum interval period should be observed
between the administration of these two vaccines. Yellow Fever
and MMR should not be administered on the same day.
1
Varicella (and zoster) vaccine
and MMR
If these vaccines are not administered on the same day, then a
four week minimum interval should be observed between
vaccines.
2
Tuberculin skin testing
(Mantoux) and MMR
MMR vaccination and tuberculin skin testing can be performed
on the same day (Kroeger et al 2019). However, if a tuberculin
skin test has already been initiated, then MMR should be
delayed until the skin test has been read unless protection
against measles is required urgently. If a child has had a recent
MMR, and requires a tuberculin test, then a four week interval
should be observed.
3
All currently used live vaccines
(BCG, rotavirus, live attenuated
influenza vaccine (LAIV), oral
typhoid vaccine, yellow fever,
varicella, zoster and MMR).
Apart from those combinations listed above, these vaccines
can be administered at any time before or after each other.
This includes tuberculin (Mantoux) skin testing.
4
1 Co-administration of these two vaccines can lead to sub-optimal antibody responses to yellow fever,
mumps and rubella antigens (Nascimento et. al, 2011). Where protection is required rapidly then the
vaccines should be given at any interval; an additional dose of MMR should be considered.
2 A study in the US (Mullooley & Black, 2001) showed a significant increase in breakthrough infections when
varicella vaccine was administered within 30 days of MMR vaccine; suggesting that MMR vaccine caused
an attenuation of the response to varicella vaccine. When the vaccines are given on the same day, however
the responses have been shown to be adequate (Plotkin, 2018.) As the zoster (shingles) vaccine contains
the same virus as varicella (chicken pox) vaccine, this recommendation has been extrapolated to MMR and
zoster. Where protection from either vaccine is required rapidly then the vaccines can be given at any
interval and an additional dose of the vaccine given second should be considered.
3 Administering tuberculin (Mantoux) within 28 days of MMR vaccine may result in decreased reactivity of
the tuberculin and the false negative reporting of results. If tuberculin testing has already been initiated,
MMR should be delayed until the skin test has been read. If protection against measles is urgently
required, then the benefit of protection from the vaccine outweighs the potential interference with the
tuberculin test. In this circumstance, the individual interpreting the negative tuberculin test should be
aware of the recent MMR vaccination when considering how to manage that individual.
4 Whilst there is no evidence of decreased reactivity or interference from other live vaccines, those
interpreting the results of the tuberculin skin test should be aware of any recently administered live
injectable vaccines.

10
Chapter 11 -
The UK
immunisation
schedule
Chapter 11: The UK immunisation schedule 11 March 2022
References
Kroger AT, Duchin J, Vázquez M. General Best Practice Guidelines for Immunization. Best Practices Guidance
of the Advisory Committee on Immunization Practices (ACIP). https://www.cdc.gov/vaccines/hcp/acip-recs/
general-recs/index.html. Accessed on January 10, 2019.
Mullooly, J and Black, S (2001). Simultaneous administration of varicella vaccine and other recommended
childhood vaccines – United States, 1995-1999. MMWR Weekly. Nov 30, 2001 / 50(47); 1058 -1061. http://
www.cdc.gov/mmwr/preview/mmwrhtml/mm5047a4.htm
Nascimento Silva JR, Camacho LA, Freire Mde S et al (2011). Mutual interference on the immune response to
yellow fever vaccine and a combined vaccine against measles, mumps and rubella. Vaccine 29(37): 6327- 6334
Plotkin SA, Orenstein WA, Offit PA and Edwards KM, (eds) (2018) Vaccines, 7th edition. Philadelphia, PA:
Elsevier, [2018]
