
GLOBAL LEADERS IN OUTCOMES, EDUCATION, SAFETY AND DISCOVERY
MEETING GUIDE
OCTOBER 11-15 | NEW ORLEANS, LA
1
Welcome Letter from Mayor of New Orleans .……….………. 2
Welcome Message ….……….……….……….……….………. 3
2014 Committee on Annual Meeting Oversight (AMOC) ... 4
2014 ASA Officers
2014 ASA Board of Directors…….……….……….………. 5
Special Events & Meetings….……….……….……….………. 6
EDUCATION ….……….……….……….……….……….………. 12
Electronic Posters (e-Posters) ….……….……….………. 13
Medically Challenging Cases
Scientific Abstract Sessions
In-Kind Commerical Support …….……….……….………. 14
CME Credit Guide .……….……….……….……….………. 16
Schedule by DAY
Friday, October 10.……….……….……….……….………. 18
Saturday, October 11…….……….……….……….………. 18
Sunday, October 12 …….……….……….……….………. 26
Monday, October 13 …….……….……….……….………. 34
Tuesday, October 14 …….……….……….……….………. 42
Wednesday, October 15 .……….……….……….………. 48
Schedule by LEARNING TRACK
Ambulatory Anesthesia ….……….……….……….………. 50
Cardiac Anesthesia……….……….……….……….………. 54
Critical Care Medicine ….……….……….……….………. 60
Fundamentals of Anesthesiology .……….……….………. 66
Neuroanesthesia .……….……….……….……….………. 80
Obstetric Anesthesia …….……….……….……….………. 84
Pain Medicine ….……….……….……….……….………. 88
Pediatric Anesthesia …….……….……….……….………. 94
Professional Issues ……….……….……….……….………. 98
Regional Anesthesia and Acute Pain …….……….………. 106
Schedule by SESSION TYPE
Subspecialty Panels …….……….……….……….………. 112
Refresher Course Lectures ……….……….……….………. 112
90-Minute Panels .……….……….……….……….………. 117
120-Minute Panels …….……….……….……….………. 120
Clinical Forum ….……….……….……….……….………. 121
Point Counterpoint ……….……….……….……….………. 122
PBLD …….……….……….……….……….……….………. 123
Cadaver Workshops …….……….……….……….………. 131
Hands-on Workshops…….……….……….……….………. 133
Seminar .……….……….……….……….……….………. 133
Residents & Medical Students ….……….……….………. 133
Governance Events ……….……….……….……….………. 134
Special Meetings & Events ……….……….……….………. 134
Corporate Non-CME Educational Events ….……….………. 136
Foundation for Anesthesia Education and Research (FAER) 138
Anesthesia Patient Safety Foundation Donor List (APSF) 140
NETWORK
Run For The Warriors
®
….……….……….……….………. 144
ASA Welcome Reception .……….……….……….………. 144
Connection Center ….……….……….……….……….………. 144
ASA Resource Center
Connection Lounges
Exhibits
Scientific and Educational Exhibits
ASA Bistro.……….……….……….……….……….………. 145
International Connection Lounge ….……….……….………. 145
Online Community ….……….……….……….……….………. 145
Governance….……….……….……….……….……….………. 146
Residents & Medical Student Component….……….………. 152
ATTEND
Registration .……….……….……….……….……….………. 154
Registration Hours
Admission Requirements
Tickets and Name Badges
Ribbons
General Information .……….……….……….……….………. 155
ASA Information Services
Business Services
Email Stations
Emergency Procedures, Medical Care, First-Aid Offices
Exhibitor Information Retrieval Program
Onsite Information and Directional Resources
Future ASA Annual Meetings
Lost and Found
Luggage/Bag Storage
Presenter Ready Room
Press Room/Daily News
Session and Product Locators
SmartTots
WiFi
Worship
Transportation Program …….……….……….……….………. 156
Hotel Shuttle Bus Schedule …….……….……….………. 157
Tours & Activities…….……….……….……….……….………. 158
FLOOR PLANS
Convention Center ……….……….……….……….………. 160
Hotels ….……….……….……….……….……….………. 168
DISCLOSURES & SPEAKER INDEX ….……….……….………. 172
Table of Contents
2014 MEETING GUIDE

2
MITCHELL J. LANDRIEU, MAYOR
CITY OF NEW ORLEANS
1300 PERDIDO STREET | SUITE 2E04 | NEW ORLEANS, LOUISIANA | 70112
PHONE 504-658-4900|FAX 504-558-4938
Dear ASA Attendees, Guests and Exhibitors,
It is my pleasure to welcome the American Society
of Anesthesiologists to New Orleans for
ANESTHESIOLOGY™ 2014, October 11-15. Thank
you for your commitment to our great City.
New Orleans provides the best venue for
discussing the latest technology in anesthesiology
and networking with fellow physicians. Our
research facilities will provide a platform for the
world’s leading experts to conduct symposia and
increase awareness about perioperative medicine.
I encourage you to embrace everything New Orleans has to offer. Take some time to
visit our historic French Quarter, fine restaurants and entertainment venues and
absorb the hospitality that makes New Orleans the most authentic and culturally
rich destination in America.
Again, thank you for choosing New Orleans for this year’s event and we I hope you
enjoy your stay.
Mitchell J. Landrieu
Mayor, City of New Orleans

3
Dear Friends,
We are pleased to invite you to the
ANESTHESIOLOGY™ 2014 annual meeting, the
premier anesthesiology educational event in the
world, to be held this October 11 to 15 in New
Orleans. Each year, more than 15,000 attendees
from over 90 countries gather to learn about the
latest bench and clinical science, technology, and
ground-breaking advances in anesthesiology.
What’s so special about the ANESTHESIOLOGY™ 2014 annual meeting? The wide spectrum
of topics, international focus and the industry professionals representing every facet of the
anesthesiology-related health care industry assembled in one place, at one time.
With more than 500 educational sessions across 10 dedicated learning tracks, including
subspecialty and international panel discussions, there is truly something for everyone. The ASA
continues to transition from paper to electronic program materials, and has the software tools to
help you create a customized education plan that meets your needs. Spouses and guests will, of
course, nd New Orleans an attractive and unique city to explore.
A new ASA initiative, the Perioperative Surgical Home (PSH), is a hot topic in health care and
will be discussed in a variety of sessions, including this year’s Opening Session. To provide
attendees with a global perspective on anesthesiology, we offer three dedicated international
sessions and panel presentations, including an international forum on patient safety and quality
outcomes.
For nearly 70 years, anesthesiologists from around the world have relied on ASA’s annual
meeting for industry-leading education, practice management guidance, technology updates,
networking opportunities and cutting-edge anesthesiology products and services. Experience the
event that will be talked about for the rest of the year.
See you in October!
Jane C.K. Fitch, M.D.
President
Michael F. O’Connor, M.D.
Chair, Committee on Annual Meeting Oversight

4
ASA would like to express appreciation for and recognize the
outstanding efforts of the members of the Committee on Annual
Meeting Oversight in planning the ANESTHESIOLOGY™ 2014
annual meeting.
Chair
Michael F. O’Connor, M.D., FCCM
First Vice Chair
Karen B. Domino, M.D., M.P.H.
Second Vice Chair
Brenda A. Gentz, M.D.
Immediate Past Chair
Audree A. Bendo, M.D.
Committee members:
Asokumar Buvanendran, M.D.
Dean Connors, M.D.
Saundra E. Curry, M.D.
James C. Eisenach, M.D.
Randall P. Flick, M.D.
Joy L. Hawkins, M.D.
David L. Hepner, M.D.
Terese T. Horlocker, M.D.
Girish P. Joshi, M.B.B.S., M.D.
Mary Dale Peterson, M.D.
Beverly K. Philip, M.D.
Scott Reeves, M.D., M.B.A.
Meg A. Rosenblatt, M.D.
Sulpicio G. Soriano, M.D.
Lawrence C. Tsen, M.D.
Avery Tung, M.D., FCCM
President
Jane C.K. Fitch, M.D.
President-Elect
J.P. Abenstein, M.S.E.E., M.D.
First Vice President
Daniel J. Cole, M.D.
Immediate Past President
John M. Zerwas, M.D.
Vice President for Scientic Affairs
Beverly K. Philip, M.D.
Vice President for Professional Affairs
Stanley W. Stead, M.D., M.B.A.
Secretary
Linda J. Mason, M.D.
Treasurer
James D. Grant, M.D.
Assistant Secretary
Jeffrey Plagenhoef, M.D.
Assistant Treasurer
Mary Dale Peterson, M.D.
Speaker, House of Delegates
Steven L. Sween, M.D.
Vice Speaker, House of Delegates
Ronald L. Harter, M.D.
2014 ASA COMMITTEE ON
ANNUAL MEETING OVERSIGHT
2014 ASA OFFICERS

5
Alabama
Michael C. Gosney, M.D.
Jennifer R. Dollar, M.D.
Alaska
Vernon C. Hill, M.D.
Robert J. Pease, M.D.
Arizona
Jeff Mueller, M.D.
Brian J. Cammarata, M.D.
Arkansas
J. Michael Vollers, M.D.
Danny Wilkerson, M.D.
California
Mark A. Singleton, M.D.
Michael Champeau, M.D.
Colorado
Randall M. Clark, M.D.
Kristin T. Woodward, M.D.
Connecticut
Jeffrey B. Gross, M.D.
Kenneth R. Stone, M.D.
Delaware
Chris A. Kittle, M.D.
Nicholas C. Gagliano, M.D.
District of Columbia
John F. Dombrowski, M.D.
Raafat S. Hannallah, M.D.
Florida
David Varlotta, D.O.
Jeffrey S. Jacobs, M.D.
Georgia
Howard Odom, M.D.
Timothy N. Beeson, M.D.
Hawaii
William Montgomery, M.D.
Della M. Lin, M.D.
Idaho
Stephen B. Packer, M.D.
Blake E. Pedersen, D.O.
Illinois
Joseph W. Szokol, M.D.
Asokumar Buvanendran, M.D.
Indiana
Gerard T. Costello, M.D.
Robert W. Brandt, M.D.
Iowa
Joseph F. Cassady, Jr., M.D.
Patrick H. Allaire, M.D.
Kansas
James D. Kindscher, M.D.
Stephen D. Tarver, M.D.
Kentucky
Anjum Bux, M.D.
Heidi M. Koenig, M.D.
Louisiana
David Broussard, M.D.
Kraig S. de Lanzac, M.D.
Maine
Gary E. Palman, D.O.
Allen J. Hayman, M.D.
Maryland
Murray A. Kalish, M.D., M.B.A.
Terry Walman, M.D.
Massachusetts
David L. Hepner, M.D.
Selina A. Long, M.D.
Michigan
Kenneth Elmassian, D.O.
David M. Krhovsky, M.D.
Minnesota
James R. Hebl, M.D.
Mary Ellen Warner, M.D.
Mississippi
Claude Brunson, M.D.
Candace E. Keller, M.D., M.P.H.
Missouri
Donald Arnold, M.D.
James B. Kelly, Jr., M.D.
Montana
Brian E. Harrington, M.D.
Andrew Schmitt, M.D.
Nebraska
Sheila J. Ellis, M.D.
Stephanie L. Randall, M.D.
Nevada
Brett E. Winthrop, M.D.
Dean Polce, D.O.
New Hampshire
Steven Hattamer, M.D.
Sean Hunt, M.D.
New Jersey
Patricia M. Browne, M.D.
Aryeh Shander, M.D., FCCM
New Mexico
John Wills, M.D.
Ruth E. Burstrom, M.D.
New York
Scott B. Groudine, M.D.
Paul H. Willoughby, M.D.
North Carolina
Gerald A. Maccioli, M.D.
Alan Koontz, M.D.
North Dakota
Vijay K. Gaba, M.D.
Ohio
Alan P. Marco, M.D.
Joshua L. Lumbley, M.D.
Oklahoma
Jay D. Cunningham, D.O.
Christopher D. Emerson, M.D.
Oregon
Charles K. Anderson, M.D.,
M.B.A.
Mark A. Gilbert, M.D.
Pennsylvania
Erin A. Sullivan, M.D.
Joseph F. Answine, M.D.
Puerto Rico
Luis Cummings, Jr., M.D.
Edgardo Quintana, M.D.
Rhode Island
Frederick W. Burgess, M.D.,
Ph.D.
Brett L. Arron, M.D.
South Carolina
Christopher A. Yeakel, M.D.
Jennifer Root, M.D.
South Dakota
Robert G. Allen, Jr., M.D.
Richard Russell, M.D.
Tennessee
James M. West, M.D.
W. Bradley Worthington, M.D.
Texas
Scott Kercheville, M.D.
Patrick Giam, M.D.
Utah
Michael K. Cahalan, M.D.
Russell S. Petersen, M.D.
Vermont
Joel H. Mumford, M.D.
Francisco Grinberg, M.D.
Virginia
Byron Work, M.D.
Maxine M. Lee, M.D.
Washington
Peter Dunbar, M.B.,Ch.B.,
M.B.A.
Mark F. Flanery, M.D.
West Virginia
Robert E. Johnstone, M.D.
Paul A. Skaff, M.D.
Wisconsin
James R. Mesrobian, M.D.
Lois A. Connolly, M.D.
Wyoming
Catherine C. Schmidt, M.D.
Harlan R. Ribnik, M.D.
Academic Anesthesiology
Zeev N. Kain, M.D., M.B.A.
Jeffrey R. Kirsch, M.D.
Medical Student Component
Chad R. Greene
Resident Component
Mark C. Bicket, M.D.
Matthew C. Gertsch, M.D.
Uniformed Services Society of
Anesthesiologists (USSA)
Corry J. Kucik, M.D.
John R. Rotruck, M.D.
2014 ASA BOARD OF DIRECTORS

6
Special Events & Meetings
SPE01 Challenges in Anesthesiology: A European Perspective
Saturday, October 11 | 8-10 a.m. | 265-268
Moderator: Daniela Filipescu, M.D.
This symposium will address the challenges for anesthesiology
in the growing eld of evidence-based perioperative medicine.
Upon completion of this learning activity, participants should be
able to identify the interactions between anesthesiologists and
other medical specialties in perioperative medicine, to assess the
importance of guidelines in daily clinical practice and to appreciate
how scientic organizations such as ESA address the issue of
perioperative patient safety.
SPE02 ANESTHESIOLOGY 2014 Opening Session: Are You the
Anesthesiologist of the Future?
Saturday, October 11 | 10:30-11:45 a.m. | Great Hall AD
Lead Speaker: Jason Hwang, M.D.
The 2014 Opening Session will address game-
changing “disruptive innovations” taking place
in medicine that present untold opportunities
for physician anesthesiologists to become
leaders in the coming health care paradigm.
Don’t miss this rare opportunity to hear Louisiana Gov. Bobby
Jindal – one of the freshest, most invigorating minds in the
Republican Party and potential 2016 GOP presidential candidate.
Gov. Jindal’s successes in Louisiana’s education and ethics reform
as well as his transformation of Louisiana’s health care system
have made him a highly respected voice in the GOP today.
At the center of this year’s program – and at the center of this
new paradigm – is the Perioperative Surgical Home (PSH) model
of care, which puts physician anesthesiologists at the head of
a health care system that seeks a better patient experience,
improved outcomes and reduced costs of care.
Jason Hwang, M.D., M.B.A. is coauthor of The Innovator’s
Prescription: A Disruptive Solution for Health Care, which was
the 2010 Book of the Year recipient of the American College of
Healthcare Executives and 2011 winner of the Health Journal
Circle Prize for Inspiring Innovation. Dr. Hwang is an internal
medicine physician and chief medical ofcer and co-founder of
PolkaDoc, a telehealth company that delivers primary care via
smartphone. Mark A. Warner, M.D., 2010 ASA President and
Professor of Anesthesiology and Dean, Mayo School of Graduate
Medical Education, and Zeev Kain, M.D., M.B.A., Associate Dean
for Clinical Operations, UC-Irvine, will present real-world examples
of PSH successes and offer insight into how you can incorporate
the tenets of the PSH in your own practices.
Jason Hwang, M.D., M..B.A., author of The Innovator’s Prescription:
A Disruptive Solution for Health Care
Mark A. Warner, M.D., 2010 ASA President, Professor of
Anesthesiology Mayo Clinic College of Medicine Rochester, MN
Zeev Kain, M.D., M.B.A., Professor and Chair, Department of
Anesthesiology & Perioperative Care, and Associate Dean for
Clinical Operations, UC-Irvine
Featuring Louisiana Governor Bobby Jindal
SPE03 ASA/APSF Ellison C. Pierce, Jr., M.D. Patient Safety Memorial
Lecture: Competence and Teamwork Are Not Enough: The Value of
Cognitive Aids
Saturday, October 11 | 1-2 p.m. | Great Hall B
Lead Speaker: David Gaba, M.D.
Dr. Gaba is Associate Dean for Immersive
and Simulation-based Learning, Co-Director,
Patient Simulation Center of Innovation,
and staff physician, VA Palo, Alto Health
Care System. He is also editor-in-chief of
Simulation in Healthcare. Successful care
of the patient in anesthesia used to be considered solely as
due to the individual knowledge and skill embodied in the single
anesthesiologist. Now we also know the importance of teamwork
– and team management – by the anesthesiologist. Yet for all
other human activities of high intrinsic danger (e.g., aviation,
nuclear power production), these factors alone are known to not
be enough to optimize safety and productivity, in part because
human memory is limited and fallible, especially under stress. A
principle of human factors is to use both knowledge in the head
(memory) and knowledge in the world (presented externally) for
optimal results. Cognitive aids are the variety of physical and
electronic representations of knowledge in the world designed
to assist anesthesiologists and their co-workers in executing
complex decision-making in dynamic settings, such as managing
the anesthetized patient. Examples of such aids include pre-work
checklists (e.g., anesthesia machine check; WHO pre-surgical
checklist); emergency manuals (to be used in real-time to guide
problem solving); tables, nomograms, calculators; and electronic
systems (anesthesia information management systems, and
decision-support software). This lecture will review the rationale for
and the different types of cognitive aids that have been developed
for perioperative settings, with an emphasis on emergency
manuals. It will also discuss how their use can be integrated
with individual competence and knowledge and interprofessional
teamwork to achieve optimal patient safety. The status of adoption
of use of cognitive aids and their likely future evolution will also be
explored.
SPE04 Perioperative Cardiology: Results from VISION, POISE-2,
SIRS and ENIGMA-2
Saturday, October 11 | 2-4 p.m. | Great Hall A
Lead Speaker: Daniel I. Sessler, M.D., POISE-2,
Clonidine
Speakers: Andrea M. Kurz, M.D., VISION
Philip Deveraeaux, M.D., POISE-2, Aspirin
Richard Whitlock, M.D., M.Sc., FRCSC, SIRS Trial
Paul S. Myles, M.B., B.S., ENIGMA-2
Investigators will present the results of four
major studies, totaling 65,000 patients. VISION is a prospective
cross-sectional cohort study that evaluated cardiovascular risk in
patients having non-cardiac surgery. POISE-2 and ENIGMA-2 are
randomized trials that evaluated aspirin, clonidine and nitrous
oxide avoidance for prophylaxis against postoperative myocardial
infarctions. And nally, the SIRS trial evaluated the effect of steroid
administration on mortality and myocardial injury in patients having
cardiac surgery.
SPECIAL EVENTS & MEETINGS

7
SPE05 Anesthesia Patient Safety Foundation Workshop:
Competence and Teamwork Are Not Enough: Implementing
Emergency Manuals and Checklists
Saturday, October 11 | 2-4 p.m. | Great Hall B
Lead Speaker: Jeffrey B. Cooper, Ph.D.
Speakers: David M. Gaba, M.D., Summary of Why Emergency
Manuals are Needed in Perioperative Care
Sara N. Goldhaber-Fiebert,M.D., Basic Principles of Implementation
of Emergency Manuals
Paul G. Preston, M.D., What’s the Right Manual for Your
Organization, Group or Hospital?
William R. Berry, M.D., Getting Over the Culture Barriers
Matthew B. Weinger, M.D.
Based upon the content presented in the Ellison C. Pierce, Jr.,
Memorial Lecture, this workshop will concentrate on the practical
aspects of systematically implementing emergency manuals in
perioperative settings. Experts on the development and production
of emergency manuals will give guidance about key aspects of
how to use emergency manuals with a focus on the process of
implementation. The critical elements of implementation will
be discussed in introductory presentations, followed by a panel
discussion and facilitated breakout groups. The session will
provide an interactive experience for attendees to learn about how
to incorporate emergency manuals rather than on what they are or
why they are needed, which will be covered in the Pierce lecture.
The presentation will include a panel discussion on “When and
How Should the Manual Be Used?”
SPE06 WFSA Panel: Government Funded Healthcare and
Anesthesia – An International Perspective on Successes and
Failures
Sunday, October 12 | 8-10 a.m. | Great Hall B
Lead Speaker: Adrian W. Gelb, M.B., B.Ch.
Speakers: Thomas R. Miller, Ph.D., M.B.A.,
Understanding Access Issues in Anesthesia
Services
Susan O’Leary, M.D., FRCPC, The Canadian
Experience
Jannicke Mellin-Olsen, M.D., Dr.PH, The
Scandinavian Experience
Estela Melman, M.D., The Mexican Experience
Each of the national speakers will cover how health care is
structured and nanced, how anesthesia is reimbursed and their
experiences over the past decade in dealing with government.
SPE27 PQRS Reporting via the QCDR Reporting Channel
Sunday, October 12 | 10-11 a.m. | Room 252-254
Richard P. Dutton, M.D., M.B.A.
This panel will be led by Richard Dutton, Chief Quality Ofcer of
ASA and Executive Director of AQI. For 2014, CMS introduced
Qualied Clinical Data Registry (QCDR) as a new PQRS reporting
mechanism. PQRS reporting via the QCDR will help you avoid the
payment adjustment. Learn about how you can use the NACOR
registry for your quality and regulatory reporting. In this panel
you will learn from experts of both AQI and ASA on how to utilize
the QCDR reporting mechanism to submit your data to CMS. Key
areas: Quality Measures, Quality Reporting, PQRS, QCDR.
SPE08 Society for Airway Management Ovassapian Lecture: The
Airway Approach Algorithm: What Would Andy Say?
Sunday, October 12 | 12:30-1:30 p.m. | Great Hall B
Lead Speaker: William H. Rosenblatt, M.D.
There are only two entry points into the
ASA Difcult Airway Algorithm – awake
intubation and intubation after the induction
of anesthesia. But how does the clinician
choose between the two? Some guidance
is provided by the Difcult Airway Task Force
guidelines. But can the information gleamed
from the recommended preoperative assessment be organized in
a manner that requires the practitioner to assess their own skills
and experience? In the Ovassapian Lecture “What Would Andy
Say?” the speaker will describe the organization of preoperative
information and the clinician’s self- assessment, with the goal of
choosing a safe algorithm entry. The wit and wisdom of late task
force member Andranik Ovassapian, M.D. will be channeled as the
speaker questions the relevance of this approach.
SPE09 ABA Informational Session: Assessment Programs for
Primary Certication in Anesthesiology
Sunday, October 12 | 4-4:30 p.m. | Room 335-336
Lead Speakers: Deborah J. Culley, M.D., Brenda Fahy, M.D., FCCM
The focus will be on certication in anesthesiology, including
the ABA’s transition to Staged Examinations and the new Part
2 (APPLIED) Examination format and content. Part 1 and Part 2
Examinations The focus will be on certication in anesthesiology,
including the ABA’s transition to Staged Examinations and the new
Part 2 (APPLIED) Examination format and content.
• Description of the traditional Part 1 and Part 2 Examinations
• Part 2 Examination: Common candidate problems • Transition to
the new staged examinations; Overview of the BASIC, ADVANCED
and APPLIED Examinations and timeline for residents • Preview
of the new ABA Assessment Center in Raleigh, N.C. • Two-way
communications: Program Director meetings.
SPE10 ABA Informational Session: Maintenance of Certication in
Anesthesiology (MOCA®) Program
Sunday, October 12 | 4:30-5 p.m. | Room 335-336
Lead Speakers: Deborah J. Culley, M.D., Brenda Fahy, M.D., FCCM
The focus will be on the Maintenance of Certication in
Anesthesiology Program (MOCA) and the program for Maintenance
of Certication in Anesthesiology for Subspecialties (MOCA-
SUBS). The focus will be on the Maintenance of Certication in
Anesthesiology Program (MOCA) and the program for Maintenance
of Certication in Anesthesiology for Subspecialties (MOCA-
SUBS). • Review of MOCA requirements/portal account access
• Overview of MOCA Part 4: Practice Performance Assessment
and Improvement • Transition from subspecialty recertication to
maintenance of certication for subspecialties • Simulation for
MOCA video • Future of MOCA; MOCA Survey results and MOCA
Minute Pilot.
SPE11 Best of Abstracts: Basic Science
Monday, October 13 | 8-10 a.m. | Room 265-268
Moderators: James Rathmell, M.D., Jerrold H. Levy, M.D.,
Michael J. Avram, Ph.D.
Anesthesiology editors review submitted abstracts and select
those appropriate for the Best Abstracts in Clinical and Basic
Sciences. Authors of the Best Abstracts are invited to submit their
work to the journal for publication consideration.
Please see the Scientic Abstract Guide for a listing of the Best of
Abstracts: Clinical Science.
EDUCATION

8
SPE12 FAER Academy of Research Mentors: Mentored Research
Training Grants (MRTG): Success Elements for Trainees and Mentors
Monday, October 13 | 8-10 a.m. | Room 342
Lead Speaker: Evan D. Kharasch, M.D., Ph.D.
Speakers: Tamara Willis, Ph.D., M.P.H., AHRQ
Career Development Opportunities
Rebecca Aslakson, M.D., Ph.D., After the MRTG:
Patient-Centered Outcomes Research and
PCORI Creed Stary, M.D., Ph.D., Successful
Career Development Plans
Y.S. Prakash, M.D., Ph.D., MRTG: Successful Mentoring Plans
Roger A. Johns, M.D., Moderator for Q&A
The 2014 FAER Academy of Mentors Workshop will address
Mentored Research Training Grants: Success Elements for
Trainees and Mentors. The audience for this workshop is both
applicants and their mentors. One focus of the workshop will be
the various types of mentored research training grant opportunities
and their application mechanisms, both federal government
and private, including FAER. A second focus will be how best
to formulate and communicate scientic ideas to the specic
audiences for each grant mechanism. A third focus will be on
Individual Development Plans, which are new to the NIH application
process increasingly emphasized by FAER, and often a challenge to
applicants. The workshop will help clarify the purpose, content and
expectations regarding these plans and to help guide applicants.
The last focus will be mentoring plans – the purview of mentors to
craft and write, but of great importance to trainees. The workshop
will help clarify the purpose, content and expectations regarding
these plans to help guide mentors.
SPE13 International Forum on Patient Safety and Quality Outcomes
Monday, October 13 | 8-10 a.m. | Great Hall B
Lead Speaker: Richard P. Dutton, M.D., M.B.A.
Speakers: Sven Staender, M.D., The European
Patient Safety Foundation and OPUS: Optimizing
Patients Undergoing Surgery
Matthew T.V. Chan, M.D., Large International
Trials: What Can We Learn About Patient Safety?
Pedro Ibarra, M.D., M.Sc., National Anesthesia
Practice Standards in Colombia: A Success Story
This special forum will address international issues in
anesthesiology safety, quality and research. The speakers are
experienced leaders of national and regional quality improvement
initiatives, and they will work together to dene the issues
that all providers have in common in promoting high-quality
anesthesiology. Topics will cover national registries and census-
level data collection, development of standards and guidelines,
incident reporting systems and the shared experience of unusual
events and complications, and the necessity for common practices
to support international trials of anesthesia medications, devices
and techniques.
SPE14 Emery A. Rovenstine Lecture: Health Care at the Crossroads:
The Imperative for Change
Monday, October 13 | 10:20-11:35 a.m. | Great Hall AD
Lead Speaker: Karen B. Domino, M.D., M.P.H.
The current health care model in the United
States is unsustainable. Health care
expenditures per capita have increased every
year since 1960, when spending was $147
per citizen. In 2010, $8,402 was spent per
capita. At almost $2.2 trillion, health care
spending in the U.S. is 2.5 times higher than the wealthy nation
average. Health care spending has grown faster than the Gross
Domestic Product (GDP). It is estimated that health care as a
percentage of GDP will sit at 20 percent in 2017. By 2037, health
care spending is estimated to rise to more than 30 percent,
a level that will crowd out funding of other important societal
necessities, including education of our children, transportation,
defense and research funding. The massive health care spending
has not improved outcomes. A recent Institute of Medicine report
ranked the U.S. 17th out of 17 peer nations in life expectancy,
and a JAMA study indicated that the U.S. ranks 27th out of 34
advanced nations in life expectancy. “Business as usual” is clearly
a bad business policy. The funders of health care (e.g., federal and
state governments, businesses and consumers) are responding
to skyrocketing health care costs by focusing on quality, cost-
containment, transparency and performance incentives. These
include no payment for preventable events; no payment for certain
hospital readmissions; payments with positive/negative incentives
based on quality; value-based purchasing; value-based physician
payments; reference pricing; and alternative payment models.
The health care industry is responding with greater consolidation
and potential loss of jobs. Anesthesiologists and other health
care leaders must respond with a greater emphasis on wellness,
prevention, standardization of care, and coordination of care by
physician-led teams. Anesthesiologists are uniquely suited as
perioperative leaders. Future training must emphasize the tenets
of the Perioperative Surgical Home (better health, better delivery of
care, reduced costs), physician-led team-based care, technological
advancements (e.g., Sedasys®, target controlled infusion devices,
robotic anesthesia, decision support systems), and health policy
and regulation changes. Signicant transformations will need
to be made to the residency curricula to meet the demands of
future practice. Anesthesiologists are poised to take leadership
positions across the continuum of perioperative care. The health
care system of the future will embrace perioperative care that is
organized, physician-led, team-based, and driven by quality and
cost-containment. We must commit ourselves to new avenues of
education and training. The future is ours to lead.
ASA Distinguished Service Award (DSA) Recipient: John Neeld, M.D.
Excellence in Research Award Recipient:
Henrik Kehlet, M.D., Ph.D.
Presidential Scholar Award Recipient: Rebecca A. Aslakson, M.D.
Nicholas M. Greene, M.D. Award for Outstanding Humanitarian
Contribution Recipient: Lena E. Dohlman, M.D., M.P.H.
SPECIAL MEETINGS AND EVENTS

9
SPE15 Celebration of Research
Monday, October 13 | 11:45 a.m.-1:15 p.m. | Great Hall B
Lead Speaker: James C. Eisenach, M.D.
Excellence in Research Award Recipient: Henrik
Kehlet, M.D., Ph.D.
Presidential Scholar Recipient: Rebecca
Aslakson, M.D.
The Celebration of Research is a way to
recognize and emphasize the important
research being done in the eld of
anesthesiology as well as a way to honor those who have
advanced the eld of anesthesiology through their research.
A basic tenet of the ASA’s mission is to advance and support
research in anesthesiology. Science and education are the
foundation of progress in the specialty, and we are strengthening
that foundation. The Celebration of Research gives this year’s
research award recipients the opportunity to present overviews
of their work, followed by a panel discussion on research in
anesthesiology.
11:45 a.m. – Welcome, James C. Eisenach, M.D.,
Editor-in-Chief, Anesthesiology
11:50 a.m. – Presentation of FAER Anesthesiology Mentoring
Excellence in Research Award
12 p.m. – Excellence in Research Award Recipient -
Henrik Kehlet, M.D., Ph.D.
12:25 p.m. – Presidential Scholar Award Recipient -
Rebecca A. Aslakson, M.D.
12:55 p.m. – Evan D. Kharasch, M.D., Ph.D., Chair,
ASA Committee on Research Resident
Research Awards:
1st Place: Jennifer Danielsson,M.D.
2nd Place: Andreas Duma, M.D.
3rd Place: Elisha Peterson, M.D.
1:05 p.m. – Foundation for Anesthesia Education
and Research (FAER) Report
James R. Zaidan, M.D., M.B.A., FAER Board Chair
SPE16 FAER-Helrich Research Lecture: The Clinical Neuroscience of
Anesthesia: Research, Education and Patient Care
Monday, October 13 | 2-3 p.m. | Great Hall B
Lead Speaker: Emery N. Brown, M.D., Ph.D.
The FAER Honorary Research Lecture
recognizes outstanding scholarship by a
scientist in an effort to encourage young
anesthesiologists to consider careers in
research and teaching, which are crucial if
anesthesiology is to maintain its reputation
as a medical specialty continuously striving for excellence in
patient care. In the 14th annual Honorary Research Lecture,
Dr. Emery Brown, Warren M. Zapol Professor of Anaesthesia,
Harvard Medical School, will discuss “The Clinical Neuroscience of
Anesthesia: Research, Education and Patient Care.” He will explain
how neuroscience research is rapidly changing our understanding
of anesthesia and how a deeper understanding of neuroscience
can change patient care. He will also describe a neuroscience
education program for anesthesiologists.
SPE17 Patrick Sim Forum: An Afternoon With the WLM Laureates
of the History of Anesthesia
Monday, October 13 | 2-4 p.m. | Room 265-268
Lead Speaker: David B. Waisel, M.D.
Speakers: David J. Wilkinson, M.B.B.S., 2008
WLM Laureate of the History of Anesthesia
Douglas R. Bacon, M.D., M.A., 2012 WLM
Laureate of the History of Anesthesia
The most prestigious award the WLM bestows
is the Laureate of the History of Anesthesia,
which is awarded every four years to an
outstanding scholar and contributor in the eld. To date, six
Laureates have been awarded. We are most fortunate to have
two of the most prominent historians of anesthesia, the 2008
Laureate, David J. Wilkinson, M.B., B.S., FRCA, and the 2012
Laureate, Douglas R. Bacon, M.D., M.A., join us for an intimate
conversation. Through in-depth discussion sparked by moderator
and audience questions, we will explore the arcs of their careers,
their motivation to study anesthesia history, their best and worst
moments, and the advice they would give to aspiring historians.
We will discuss prominent historical controversies, fertile areas
of research and why the study of anesthesia history is important.
This forum is a once-in-a-lifetime opportunity to visit with these
leading historians.
SPE18 FAER Panel: Future of Anesthesiology Research
Monday, October 13 | 3-5 p.m. | Great Hall B
Moderator: Zeljko Bosnjak, Ph.D.
Speakers: Yan Xu, Ph.D., The Benets of Having Ph.D.s in Research
in a Clinical Department
Keith H. Baker, M.D., Ph.D., Research on Education
Charles W. Emala, M.D., Physician-Scientist Faculty Development
Hannah Wunsch, M.D., M.Sc., The Role of Anesthesiologists in
Perioperative Research
The panel will address the future of anesthesiology research from
several viewpoints. First, the role of Ph.D. scientists in anesthesia
departments will be highlighted, as well as the role they play in
mentoring other faculty members. In addition, the importance
of departmental educational programs as they relate to faculty
development and improved patient care will be discussed. Finally,
the panel will elaborate on the advantages of anesthesiologists in
perioperative research and the value of their work to their medical
centers.
EDUCATION

10
SPE19 How Can FAER’s New Education Mentorship Academy Help
Anesthesiology Educators?
Monday, October 13 | 5-6 p.m. | Great Hall B
Lead Speaker: Catherine M. Kuhn, M.D.
An introduction to the recently initiated FAER Academy of Mentors
will be provided. The Academy’s goals and future directions will
be outlined, and the purpose of this and future workshops framed
for attendees. This will be followed by two case presentations
from FAER Research in Education Grant (REG) recipients. They
will briey describe their research theme and describe how the
FAER REG grant t into their education career trajectory; they will
also specically comment on the role of their mentors and any
enhanced opportunities for mentorship. Following these short
presentations, moderators and all participants will be engaged
in an interactive discussion using the previous material as a
springboard. Themes to be explored include 1) elements a good
education grant application, 2) importance of career development
plan, 3) role of mentoring relationships and 4) resources
available for mentors, including opportunities for mentor/mentee
participation in and input into future workshops.
SPE20 Reduce Compliance Risks With Opioid Prescribing
Tuesday, October 14 | 8-10 a.m. | Great Hall B
Lead Speaker: John F. Dombrowski, M.D.
Speaker: Louis Lejarza
Panelists include representatives from the American Society of
Addiction Medicine and the Drug Enforcement Administration.
Panelists will review current literature on opioid addiction and
explain when pain medicine physicians should refer to an
addiction medicine specialist. Panelists will also summarize
federal enforcement actions against physicians for improper opioid
prescribing.
SPE21 Journal Symposium: How to Mechanically Ventilate Patients
in the Operating Room in 2014
Tuesday, October 14 | 8-11 a.m. | Room 275-277
Moderator: Jeanine P. Wiener-Kronish, M.D.
Marcos Vidal-Melo, M.D, Ph.D., Mechanistic Basis for Protective
Intraoperative Mechanical Ventilation
Ana Fernandez-Bustamante, M.D., Ph.D., Intraoperative Ventilation
Practices and Quality Improvement
Paolo Pelosi, M.D.- Protective Ventilation during General
Anesthesia: the PROVHILO Trial
Jean-Francois Pittet, M.D.
Please see the Scientic Abstract Guide for a listing of Journal
Symposium abstracts.
SPE28 AQI Listening Session
Tuesday, October 14 | 10 a.m.-12 p.m. | Room 223
Lead Speaker: Richard P. Dutton, M.D., M.B.A..
We want to hear from you. AQI invites everyone
to join us for a discussion on what you would like
to see AQI work on next. This is your opportunity
to provide input on how AQI can help the
profession – whether it is regulatory reporting,
reimbursement, or changing practice models. Dr.
Richard Dutton will begin the discussion, then we ask the audience
to drive the discussion.
SPE22 John W. Severinghaus Lecture on Translational Science:
Basic Science to Clinical Practice: The Tale of Long-Acting Opioids
Tuesday, October 14 | 10:30-11:30 a.m. | Great Hall AD
Lead Speaker: Evan D. Kharasch, M.D., Ph.D.
Dr. Kharasch is Vice Chancellor for Research, Russell D. and
Mary B. Sheldon Professor of Anesthesiology; Director, Division
of Clinical and Translations Research, Professor of Biochemistry
and Molecular Biophysics at Washington University, St. Louis.
Opioids such as methadone provide long-lasting relief of acute,
perioperative, chronic and cancer pain, and are pivotal to
anesthesia practice. Yet with the increase in methadone use,
there has been a terrifying increase in untoward events. Only
recently has there been a better understanding of methadone
pharmacology, including pharmacokinetics, pharmacodynamics
and pharmacogenetics. This lecture tells the story of how these
clinical problems were studied in the basic science laboratory, how
the insights gained were then veried in clinical trials, and how
this new knowledge can guide clinical practice and improve clinical
outcome and guide practice.
SPE23 Lewis H. Wright Memorial Lecture
Tuesday, October 14 | 12:40-1:50 p.m. |
265-268
Lead Speaker: James P. Bagian, M.D., PE
The Lewis H. Wright Memorial Lecture
of the Wood Library-Museum of
Anesthesiology (WLM) honors Dr. Lewis
Wright, a distinguished pioneer in American
anesthesiology, who gave of himself tirelessly to dignify and
accredit the discipline of anesthesiology as a clinical science and
medical specialty. In 1955, ASA recognized his contributions by
according him its highest honor, the Distinguished Service Award.
This lectureship will serve to remind us now, and in the years to
come, of his honored place in the specialty of anesthesiology.
SPE24 Best of Abstracts: Clinical Science
Tuesday, October 14 | 1-3 p.m. | Room 275-277
Moderators: James Rathmell, M.D., Jerrold H. Levy, M.D.,
Michael J. Avram, Ph.D.
Anesthesiology editors review submitted abstracts and select
those appropriate for the Best Abstracts in Clinical and Basic
Sciences. Authors of the Best Abstracts are invited to submit their
work to the journal for publication consideration.
Please see the Scientic Abstract Guide for a listing of the Best of
Abstracts: Clinical Science.
FEATURED LECTURES

11
11
SPE25 History Panel – Show Me the Money: A Brief History of
Remuneration in Anesthesiology
Tuesday, October 14 | 2-4 p.m. | 265-268
Lead Speaker: Douglas R. Bacon, M.D., M.A.,
An Economic History Lesson: The Creation of
the American Board of Anesthesiology
Speakers: William D. Hammonds, M.D.,
Crawford Long, M.D., The First Anesthetic Fee,
and an Ether Controversy
Christine Ball, M.B., B.S., FANZCA, Paying for
Anesthesia Down Under
David J. Wilkinson, M.B., B.S., From Private
Practice to the National Health Service: The United Kingdom’s
Journey
Mark A. Warner, M.D., The American Dream: Private Practices
versus Employed Physician and an Ongoing Controversy
This panel will trace the history of payment in anesthesiology from
the rst recorded anesthetic fee in 1842 to the current system
in the U.S. Australia and the U.K. are included to contrast U.S.
history and to look at the evolution of other payment systems.
EDUCATION

12
Education Program Overview
The overall scientic program and learning tracks of the
ANESTHESIOLOGY™ 2014 annual meeting address the specialty’s
practice gaps and underlying educational needs in multiple areas,
including Ambulatory Anesthesia, Cardiac Anesthesia, Critical Care
Medicine, Fundamentals of Anesthesiology, Neuroanesthesia,
Obstetric Anesthesia, Pain Medicine, Pediatric Anesthesia,
Professional Issues, and Regional Anesthesia and Acute Pain. The
program reects the diversity of subspecialties and the needs and
interests of the general physician anesthesiologist’s practice.
Target Audience
The ANESTHESIOLOGY™ 2014 annual meeting is intended for
physician anesthesiologists, residents and other health care
professionals interested in expanding their knowledge and
enhancing their skills to improve competency and professional
practice.
Overall Learning Objectives
At the conclusion of this activity, participants should be able to:
• Assess the potential applications of emerging issues and
advances that affect the practice of anesthesia.
• Integrate technical knowledge about state-of-the-art
procedures, advanced therapeutic agents and medical device
uses into practice.
• Apply contemporary practice management skills and knowledge
of regulatory issues to the efcient and safe delivery of patient
care.
• Translate expanded knowledge into improvements in practice,
patient outcomes and patient satisfaction.
Accreditation and Designation Statements
This activity has been planned and implemented in accordance
with the Essential Areas and Policies of the Accreditation Council
for Continuing Medical Education (ACCME) through the joint
sponsorship of the American Society of Anesthesiologists (ASA).
ASA is accredited by the ACCME to provide continuing medical
education for physicians.
ASA designates this live activity for a maximum of 44 AMA PRA
Category 1 Credits
™
. Physicians should claim only the credit
commensurate with the extent of their participation in the activity.
CME Certicates
ANESTHESIOLOGY™ 2014 annual meeting attendees can enter
session attendance information and print their own certicates
from any computer with an Internet connection at the end of each
day of the meeting. Attendees can also print their CME certicates
during the annual meeting at CME computer kiosks in designated
areas. CME credits can be claimed in .25 hour increments.
The deadline for participants to obtain certicates for the
ANESTHESIOLOGY™ 2014 annual meeting is December 31, 2014.
Entry and printing of CME information will be available online at
goanesthesiology.org through December 31, 2014.
Disclosure
ASA adheres to ACCME Essential Areas, Standards and Policies
regarding industry support of CME. Disclosure of the planning
committee and faculty’s commercial relationships will be made
known at the activity. Speakers are required to openly disclose
any limitations of data and/or any discussion of any off-label,
experimental, or investigational uses of drugs or devices in their
presentations.
Resolutions of Conicts of Interest
In accordance with the ACCME Standards for Commercial Support
of CME, ASA has implemented mechanisms, prior to the planning
and implementation of this CME activity, to identify and resolve
conicts of interest for all individuals in a position to control
content of this CME activity.
All faculty and planning committee members are required to
disclose any nancial relationships and will be listed accordingly at
goanesthesiology.org.
For a full listing of all presenters and their sessions, please go to
goanesthesiology.org.
Disclaimer
The information provided at this CME activity is for continuing
education purposes only and is not meant to substitute for the
independent medical judgment of a health care provider relative
to diagnostic and treatment options of a specic patient’s medical
condition.
Special Needs Statement
ASA is committed to making its activities accessible to all
individuals. If you are in need of an accommodation, please do not
hesitate to call and/or submit a description of your needs in writing
in order to receive service.
Commercial Support Acknowledgement
ASA gratefully acknowledges commercial support for the
ANESTHESIOLOGY™ 2014 annual meeting. A list of commercial
supporters will be published in the Meeting Guide and Exhibit
Guide and at goanesthesiology.org.
Attend Select Educational Sessions to Earn Credit
Toward MOCA®
The ANESTHESIOLOGY™ 2014 annual meeting offers several
opportunities to help fulll your Maintenance of Certication in
Anesthesiology (MOCA®) requirements. Sessions marked with the
MOC-PS icon will count toward Part 2 Patient Safety requirements.
Look for the MOC-PS icon to identify designated sessions. Please
note: Name badges must be scanned after the session in order to
claim CME credit for MOCA®.
Ethics Education
Selected sessions have been identied to help meet individual
state and institutional ethics education requirements. Please check
with your regulatory body for qualifying criteria.
Ultrasound-Guided Regional Anesthesia
Ultrasound-guided Regional Anesthesia (UGRA) Education and
Clinical Training Portfolio is a joint ASRA-ASA initiative to provide
applicants with a comprehensive educational and training
experience that fullls current training recommendations for UGRA.
Perioperative Surgical Home
Look for the PSH icon that identies sessions which will address
the Perioperative Surgical Home (PSH) model.
EDUCATION

13
13
Many More Opportunities Available at Education Booth
Learn about ASA’s MOCA® offerings, including the Practice
Performance Assessment and Improvement (PPAI) modules,
self-assessment module-pain medicine (SAM-PM), online patient
safety courses, Anesthesiology Continuing Education (ACE), the
Self-Education and Evaluation (SEE) program, and the Simulation
Education Network. Other CME opportunities include practice
management online modules, ethics modules, journal CME and
more. Stop by the Education Booth and visit the ASA Education
Center to discover how to fulll your MOCA® needs.
Learning Track Codes
AM Ambulatory Anesthesia
CA Cardiac Anesthesia
CC Critical Care Medicine
FA Fundamentals of Anesthesiology
NA Neuroanesthesia
OB Obstetric Anesthesia
PN Pain Medicine
PD Pediatric Anesthesia
PI Professional Issues
RA Regional Anesthesia and Acute Pain
Special Designations
E Ethics Session
MOC-PS Maintenance of Certication
UGRA Ultrasound-Guided Regional Anesthesia Portfolio
PSH Perioperative Surgical Home
Session Codes
CF Clinical Forum
OR Oral Presentations
PN Panels (90-Minute and 120-Minute)
PC Point-Counterpoint Sessions
PD Poster Discussions
PO Poster Presentations
L- Problem-Based Learning Discussions
100, 200, 300, 400, 500 series
Refresher Course Lectures
RM Resident and Medical Student Activities
SPE Special Events
600 Series
Subspecialty Panels
800 Series, AW, DW, CA
Workshops
AW: Workshop on Flexible Endoscopy for Lung Isolation
DW: Basic Adult Flexible Fiberoptic Intubation Workshop
CA: Cadaver Workshop
Maintenance of Certication in Anesthesiology Program® and MOCA® are registered
certication marks of the American Board of Anesthesiology®.
This patient safety activity helps fulll the patient safety CME requirement for Part II of
the Maintenance of Certication in Anesthesiology Program (MOCA®) of the American
Board of Anesthesiology (ABA). Please consult the ABA website, www.theABA.org, for
a list of all MOCA® requirements.
Scientic Abstracts, e-posters and Medically Challenging Cases
Enrich your education experience at the ANESTHESIOLOGY™ 2014
annual meeting by attending these offerings:
Electronic Posters (e-posters)
All Poster Discussions and Poster Sessions will be presented in
an electronic format (e-posters) on large, high-denition monitors.
Abstracts will also be available for viewing at your leisure on high-
denition monitors located throughout the convention center. All
Poster Sessions will be available in Hall B1 of the Ernest N. Morial
Convention Center and they will rotate on the large monitors every
30 minutes. Poster Discussions will be held in Rooms 243-245 on
the second level of the convention center. Please note: CME credit
is not provided.
Scientic Abstract Sessions
Scientic abstract sessions consist of Oral Presentations, Poster
Discussions and Poster Sessions. During Oral Presentations and
Poster Discussions, authors present a summary of their studies,
including their hypothesis, methods, data and conclusions.
Questions and comments from the audience are welcome
and encouraged at the conclusion of the presentation. Poster
Sessions are in-depth and informative discussions among authors
and attendees. Poster authors will be available for discussion
during designated times during the meeting. Full text for all
scientic abstracts will be available to view online in August at
goanesthesiology.org.
Late-Breaking Abstracts
Late-Breaking Abstracts focus on signicant and timely ndings
while showcasing late-breaking data and results that affect the
eld of anesthesiology. These abstracts will be presented during
designated periods during the ANESTHESIOLOGY™ 2014 annual
meeting.
Medically Challenging Cases
All Medically Challenging Cases will be presented in electronic
format (e-posters) on high-denition monitors. Interact with
colleagues and hear about the medically challenging cases they
have encountered in their hospital or practice. This area provides
attendees with a forum to share experiences, relate how they
handled a difcult situation and obtain feedback regarding how
other physicians may have proceeded under similar circumstances.
All learning tracks are represented and there is a case for every
medical specialty. Medically Challenging Cases will be located
in Hall B1 of the convention center and will rotate through the
presentations every 10 minutes. CME credit is not provided.
EDUCATION
14
In-Kind Commercial Support Acknowledgement
ASA gratefully acknowledges in-kind commercial support for the
ANESTHESIOLOGY™ 2014 annual meeting. This list is current
as of 9/17/14. For an updated listing, see goanesthesiology.org.
Advanced Ultrasound Guided Pediatric Regional Anesthesia
Workshop
FUJIFILM SonoSite, Inc. – ultrasound systems
Awake Fiberoptic Intubation: A Streamlined Approach with Nerve
Blocks
KARL STORZ Endoscopy-America, Inc. – beroptic bronchoscopes
Basic TEE Workshop
HeartWorks by Inventive Medical Ltd. – TEE simulators
FUJIFILM SonoSite, Inc. – ultrasound systems
Basic/Advanced Flexible Fiberoptic Intubation Workshop
Airtraq, LLC - manikins
Ambu, Inc. – berscopes
KARL STORZ Endoscopy-America, Inc. – exible scopes
Laerdal – manikins
Olympus America Inc. – beroptic bronchoscopes, intubation
manikin, video processors, monitors
Teleex – airway management products
Verathon Medical – videolaryngoscopes
Comprehensive Anatomy-Live Model Ultrasound for Regional
Anesthesia
FUJIFILM SonoSite, Inc. – ultrasound systems
Critical Care Ultrasonography for the Perioperative Physician
HeartWorks by Inventive Medical Ltd. - TEE simulators
FUJIFILM SonoSite, Inc. – ultrasound systems
Philips Healthcare – ultrasound systems
SonoSim, Inc. – two live scan simulators
Difcult Airway Workshop with Simulation
Airtraq, LLC – manikins
Ambu, Inc. – manikins, beroptic laryngoscopes
Intersurgical, Inc. – adult and pediatric mannequins, i-gel airways
KARL STORZ Endoscopy-America, Inc. – exible scopes
Olympus America Inc. – exible beroptic laryngoscopes, intubation
manikin, video processors, monitors
Siemens Healthcare – ultrasound system
Verathon Medical – glidescopes
Head and Neck Blocks (Ultrasound and Fluoroscopy) - Cadaver and
Live Models
FUJIFILM SonoSite, Inc. – ultrasound systems
Introduction to Ultrasound and Fluoroscopic-Guided Techniques for
Chronic Pain Management: Live Models and Cadavers
FUJIFILM SonoSite, Inc. – ultrasound systems
GE Healthcare – ultrasound machine
Must Know Blocks for Ambulatory Anesthesia
eZono AG – ultrasound systems
FUJIFILM SonoSite, Inc. – ultrasound systems
Pacemakers and ICDs
Medtronic – programmers
St. Jude Medical – pacemaker programmers
Pediatric Airway Workshop
Airtraq, LLC – manikins
Clarus Medical, LLC – scopes and mannequins
KARL STORZ Endoscopy-America, Inc. – laryngoscopes and exible
scopes
Mercury Medical – laryngeal airway masks and endotracheal tubes
MPI, Inc. – exible scopes
FUJIFILM SonoSite, Inc. – ultrasound system
Olympus America Inc. – intubation berscopes, intubation manikin,
video processors, monitors
Truphatek Inc. – video laryngoscope, manikins
Verathon Medical – glidescope, manikins
Perioperative ACLS Simulation Workshop
Philips Healthcare – debrillators
Perioperative Pediatric Advanced Life Support Simulation
Draeger Medical Inc. – anesthesia machines
Philips Healthcare – debrillators
Perioperative Resuscitation - What’s New?
Laerdal – manikins
SonoSim, Inc. - live scan simulator
ZOLL Medical Corporation – debrillators
Peripheral Nerve Blocks: Ultrasound, Simulation and Stimulation
Ambu, Inc. – ultrasound machine
Analogic Ultrasound – ultrasound machines
CAE Healthcare – ultrasound training models
eZono AG – ultrasound systems
Pajunk Medical Systems – needles
FUJIFILM SonoSite, Inc. – ultrasound systems
Terason – ultrasound systems
Point of Care: Novel Use of Ultrasonography in Everyday Pediatric
Anesthesia Practice
FUJIFILM SonoSite, Inc. – ultrasound systems
Radiofrequency Ablation of the Spine, Sacrum, and Lumbar Disc
Epimed International, Inc. – variety of needles
Kimberly-Clark Health Care – variety of needles
Resident Regional Anesthesia Workshop
FUJIFILM SonoSite, Inc. – ultrasound systems
Spinal Injections with Fluoroscopy - Cadaver: Basic Techniques
Epimed International, Inc. – variety of needles
Kimberly-Clark Health Care – variety of needles
Spinal Injections with Fluoroscopy-Cadaver: Advanced Techniques
(Cervical/Thoracic)
Epimed International, Inc. – variety of needles
Kimberly-Clark Health Care – variety of needles
The Use of Ultrasound for Vascular Access in Adults and Pediatrics
Ambu, Inc. – ultrasound machine, needles
Analogic Ultrasound – ultrasound machines
FUJIFILM SonoSite, Inc. – ultrasound systems
Mindray North America – ultrasound systems
Simulab Corporation - medical simulation training models
Terason – ultrasound systems
Thoracic Anesthesia Workshop
Laerdal – pediatric intubation trainer
Olympus America Inc. – broncho-videoscopes and berscopes,
intubation manikin, video processors, monitors
Verathon Medical – manikins

15
15
Ultrasound Guided Injections- Live Models: Advanced Techniques
FUJIFILM SonoSite, Inc. – ultrasound systems
Philips Healthcare – ultrasound systems
Ultrasound Guided Injections- Live Models: Basic Techniques
FUJIFILM SonoSite, Inc. – ultrasound systems
Philips Healthcare – ultrasound systems
Ultrasound Guided Musculoskeletal Injections- Live Models: Beyond
Corticosteroids
FUJIFILM SonoSite, Inc. – ultrasound systems
Preferred Medical Systems/Samsung – ultrasound system
Terason – ultrasound machine
Ultrasound-Guided Regional Anesthesia and Clinical Skills
Workshop: Introduction to UGRA for Beginners
FUJIFILM SonoSite, Inc. – ultrasound systems
I-Flow, LLC, a Kimberly-Clark Health Care Company - simulators
Mindray North America – ultrasound systems
Terason – ultrasound machines
Wire-Guided Airway Management
Ambu, Inc. – airway management tools
KARL STORZ Endoscopy - America, Inc. - bronoscopes
Olympus America Inc. - Airway Mobilescopes
Workshop on Emergency Surgical Airway Management Using a Pig
Trachea Model
Pulmodyne – Cric-Key™, Cric-Knives™
VBM Medical Inc. – Quicktrach devices
Workshop on Flexible Endoscopy for Lung Isolation
Olympus America Inc. – broncho-videoscopes and berscopes,
intubation manikin, video processors, monitors
Teleex – airway management products
EDUCATION

16
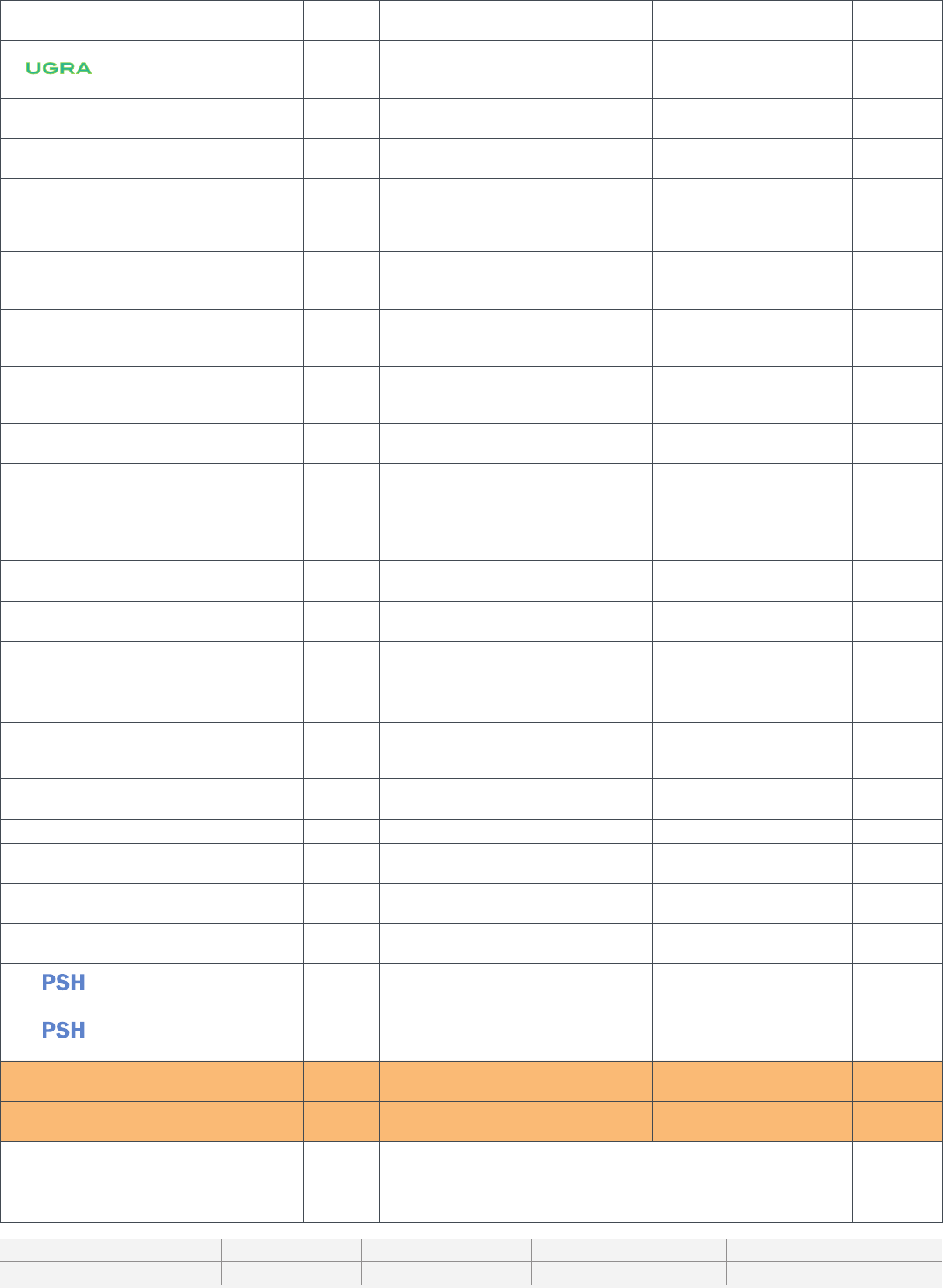
FEE CODE TYPE/NAME OF SESSION CME CREDIT HRS
PN 90-Minute Panels 1.5
PN 120-Minute Panels 2
SPE05 Anesthesia Patient Safety Foundation Workshop: Competence and Teamwork Are Not Enough: Implementing
Emergency Manuals and Checklists
2
SPE02 ANESTHESIOLOGY™ 2014 Opening Session: Are You the Anesthesiologist of the Future 1.25
SPE11 Best of Abstracts: Basic Science 2
SPE24 Best of Abstracts: Clinical 2
SPE15 Celebration of Research 1.5
SPE01 Challenges in Anesthesiology: A European Perspective 2
CF Clinical Forum 1.5
SPE03 Ellison C. Pierce Jr., M.D. Patient Safety Memorial Lecture: Competence and Teamwork Are Not Enough: The Value
of Cognitive Aids
1
SPE14 Emery A. Rovenstine Lecture: Health Care at the Crossroads: The Imperative for Change 1.25
SPE12 FAER Academy of Research Mentors: Mentored Research Training Grants (MRTG): Success Elements for Trainees
and Mentors
2
SPE16 FAER-Helrich Research Lecture: The Clinical Neuroscience of Anesthesia: Research, Education and Patient Care 1
SPE18 FAER Panel: Future of Anesthesiology Research 2
SPE25 History Panel - Show Me the Money: A Brief History of Remuneration in Anesthesiology 2
SPE19 How Can FAER’s New Education Mentorship Academy Help Anesthesiology Educators 1
SPE13 International Forum on Patient Safety and Quality Outcomes 2
SPE22 John W. Severinghaus Lecture on Translational Science: Basic Science to Clinical Practice: The Tale of Long-Acting
Opioids
1
SPE21 Journal Symposium: How to Mechanically Ventilate Patients in the Operating Room in 2014 3
SPE23 Lewis H. Wright Memorial Lecture 1
SPE17 Patrick Sim Forum: An Afternoon With the WLM Laureates of the History of Anesthesia 2
SPE04 Perioperative Cardiology: Results from VISION (n=40,000), POISE-2 (n=10,000), SIRS (n=7,500), and ENIGMA-2
(n=7,000)
2
PC Point-Counterpoint Sessions 1.5
L Problem-Based Learning Discussions (PBLDs) 1.25
SPE20 Reduce Compliance Risks With Opioid Prescribing 2
100s-500s Refresher Course Lectures (See exceptions below) 1
Refresher Course Lectures (exceptions)
121 - Smart Seniors: Avoiding Perioperative Brain Failure
306 - Perioperative Management of Patients Undergoing Spine Surgery
425 - Improving Patient Safety and Communication During Anesthesia and Surgery
2
2
2
RM13 Resident Regional Anesthesia Workshop 2.5
OR Scientic Abstract Oral Presentations 1.5
PD Scientic Abstract Poster Discussions 1.5
SPE08 Society for Airway Management Ovassapian Lecture: The Airway Approach Algorithm: What Would Andy Say? 1
600s Subspecialty Panels 1.25
SPE06 WFSA Panel: Government Funded Healthcare and Anesthesia – An International Perspective on Successes and
Failures
2
CADAVER WORKSHOPS
CA06 Comprehensive Anatomy-Live Model Ultrasound for Regional Anesthesia 4
CA04 Head and Neck Blocks (Ultrasound and Fluoroscopy)-Cadaver and Live Models 4
CA03 Introduction to Ultrasound and Fluoroscopic-Guided Techniques for Chronic Pain Management:
Live Models and Cadavers
4
CA05 Radiofrequency Ablation of the Spine, Sacrum, and Lumbar Disc 4
CA01 Spinal Injections With Fluoroscopy-Cadaver: Basic Techniques 4
CME CREDIT GUIDE
ANESTHESIOLOGY™ 2014 attendees can enter session attendance information and print their own certicates from any computer with
an Internet connection at the end of each day of the meeting. Attendees can also print their CME certicates during the annual meeting
at CME computer kiosks in designated areas. CME credits can be claimed in .25 hour increments. The deadline for participants to
obtain certicates for the ANESTHESIOLOGY™ 2014 annual meeting is December 31, 2014.
Entry and printing of CME information will be available online at goanesthesiology.org through December 31, 2014.

17
CA02 Spinal Injections With Fluoroscopy-Cadaver: Advanced Techniques (Cervical/Thoracic) 4
HANDS-ON-WORKSHOPS
804 Acupuncture Workshop 3
827 Advanced TEE Workshop 3
806 Advanced Ultrasound Guided Pediatric Regional Anesthesia Workshop 3
817 Awake Fiberoptic Intubation: A Streamlined Approach With Nerve Blocks 3
815 Basic TEE Workshop 6
DW Basic/Advanced Flexible Fiberoptic Intubation Workshop 2.5
825 Critical Care Ultrasonography for the Perioperative Physician 3
824 Difcult Airway Workshop With Simulation 3
822 Intermediate Transesophageal Echocardiography (TEE) 3
810 Must Know Blocks for Ambulatory Anesthesia 3
820 Ophthalmic Regional Anesthesia 3
809 Pacemakers and ICDs 3
812 Pediatric Airway Workshop 3
819, 830 Perioperative ACLS Simulation Workshop 3.5
823 Perioperative Pediatric Advanced Life Support Simulation 3
828 Peripheral Nerve Blocks: Ultrasound, Simulation and Stimulation 3
832 Point of Care: Novel Use of Ultrasonography in Everyday Pediatric Anesthesia Practice 3
831 The Use of Ultrasound for Vascular Access in Adults and Pediatrics 3
833 Thoracic Anesthesia Workshop 3
808 Ultrasound Guided Injections-Live Models: Advanced Techniques 4
801 Ultrasound Guided Injections-Live Models: Basic Techniques 4
814 Ultrasound Guided Musculoskeletal Injections-Live Models: Beyond Corticosteroids 4
807 Ultrasound-Guided Regional Anesthesia and Clinical Skills Workshop: Introduction to UGRA for Beginners 3
826 Wire-Guided Airway Management 3
802 Workshop on Emergency Surgical Airway Management Using a Pig Trachea Model 3
AW Workshop on Flexible Endoscopy for Lung Isolation 1.25
807 Practical Stress Management Techniques: A Quest for Physicians’ Well-being 3
813 Providing Effective Feedback to Trainees 3
CA12 Regional Anesthesia: Cadaver and Live Model Ultrasound Workshop 4
RM12 Resident Regional Anesthesia Workshop 4
814 So, You Want to Install an AIMS System? 3
841 Spinal Imaging for the Pain Medicine Physician 2
801 Statistics for Anesthesiologists 3
808 The Art and Science of Interviewing: Finding the Best Candidate for the Position 3
832 The Use of Ultrasound for Vascular Access in Adults and Pediatrics 3
833 Thoracic Anesthesia 3
807 Ultrasound-Guided Regional Anesthesia and Clinical Skills: Introduction to UGRA for Beginners 2
802 Workshop on Emergency Surgical Airway Management Using a Pig Trachea Model 3
AW Workshop on Flexible Endoscopy for Lung Isolation 1.25
SEMINARS
821 Grant Writing and the NIH Study Section for the Uninitiated 3
803 Mastering Perioperative Stress and Burnout: Exploring Methods of Essential Mind-Fitness, Developing Resilience at
Work
3
813 Perioperative Resuscitation - What's New? 3
816 Physical Exam Workshop for Pain Physicians
3
829 Physician Performance Assessment and Improvement: Practice Its Power for Your Own Practice 3
818 Practical Pain Medicine Coding, Compliance and Workow Strategies for 2014 2
811 Spinal Imaging for the Pain Medicine Physician 2
805 Statistics for Anesthesiologists 3
EDUCATION

18
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
FRIDAY, OCT. 10
Time Session Type Fee Code Title Speaker Room
3-7 p.m. Registration Lobby A & D
3-7 p.m. ASA Resource Center Convention Center, Hall B-1
3-7 p.m. International Connection Lounge Lobby A
7:30-9 p.m. Residents and Medical
Students
RM01 Residents and Medical Students
Grassroots Seminar
Jeffrey Plagenhoef, M.D. Hilton
Riverside
9-11 p.m. Residents and Medical
Students
RM02 Resident and Medical Student Welcome
Reception
Mark Bicket, M.D. Hilton
Riverside
SATURDAY, OCT. 11
Time Session Type Track Fee Code Title Speaker Location/
Room
7 a.m.-5 p.m. Registration Lobby A & D
7 a.m.-6:30 p.m. ASA Resource Center Convention Center, Hall B-1
7-8:15 a.m. Subspecialty
Panels
OB 601 (SOAP) Caring for Our Own: Focusing on
the Care Provider to Optimize Safety for
Our Patients
Robert Gaiser, M.D. 231-232
Subspecialty
Panels
PN 602 (ASRA) Advancing Safety and Risk
Management Strategies in Pain Medicine
David Provenzano, M.D. 238-239
7:15-8:30 a.m. PBLD PI L001 A High Risk Patient for Low Risk
Outpatient Surgery: Is There Value in a
Surgical Home for a Patient Going Home?
Jeanna Blitz, M.D. 343-345
PBLD NA L002 Only a Little Sniff of Cocaine; Now an
Aneurysm Coiling Headache!
Jess Brallier, M.D. 343-345
PBLD PI L003 Creating a Culture of Professionalism in
Your Department
Saundra Curry, M.D. 343-345
PBLD CC L005 Surviving Septic Shock in the Operating
Room and Beyond: What Do the
Guidelines Say?
Roman Dudaryk, M.D. 343-345
PBLD RA L006 Numb and Number: Should We Use
Regional Anesthesia in Orthopedic
Trauma?
Nabil Elkassabany, M.D. 343-345
PBLD OB L007 Just Another Day on Labor and Delivery:
Morbid Obesity and Preeclampsia
Regina Fragneto, M.D. 343-345
PBLD RA L008 Nerve Injury/Dysfunction and Peripheral
Nerve Blockade: Fact or Fiction
Thomas Halaszynski, M.D.,
M.B.A.
343-345
PBLD AM L009 Perioperative Anesthetic Issues for
Ambulatory Surgery
Dean Jones, M.D. 343-345
PBLD PN L010 Worsening Back Pain: To Inject or Not to
Inject That Is the Question
Tariq Malik, M.D.
343-345
PBLD FA L011 It’s Only a MAC Case and Now My Patient
is on FIRE!
Mark Phillips, M.D. 343-345
PBLD PD L012 Application of Pediatric Advanced
Life Support for Managing a Patient
With a Debrillator Who Develops an
Intraoperative Cardiac Arrest
David Young, M.D., M.B.A. 343-345
PBLD OB L116 Neurologic Complications Following
Epidural Placement - How to Differentiate
and Manage?
Kelly Elterman, M.D.
David Hepner, M.D.
343-345
PBLD FA L157 The Unanticipated Difcult Airway: A
Dynamic and Dangerous Scenario
Lavinia Kolarczyk, M.D. 343-345
8-9 a.m. RCL CC 101 Sepsis Current Concepts Guidelines and
Perioperative Management
Mark Nunnally, M.D., F.C.C.M. RiverGate
RCL AM 102 Current Controversies in Adult Outpatient
Anesthesia
Jeffrey Apfelbaum, M.D. E-1
RCL FA 103 Arterial Blood-Gas Analysis: Interpretation
and Application
Steven Barker, Ph.D., M.D. E-2
RCL OB 104 Anesthesia for the Morbidly Obese
Parturient
Brenda Bucklin, M.D. E-3
RCL PN 105 Clinical Evaluation and Treatment of
Neuropathic Pain
Timothy Lubenow, M.D. 260-262
EDUCATION

19
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
RCL CA 106 New Developments in Cardiopulmonary
Resuscitation
Matthias Riess, M.D., Ph.D. La Nouvelle
Ballroom AB
8-9:30 a.m. 90-Minute Panel CA PN37 Modern Day Concepts in Thoracic
Endovascular Repair (TEVAR) for Aortic
Aneurysms
David Broussard, M.D. 208-210
90-Minute Panel PI PN38 Change Management in Collaborative
Quality Improvement Projects (CQIP)
Mike Schweitzer, M.D., M.B.A. 220-222
90-Minute Panel PI PN39 Leaning In: Women in Leadership Roles Rekha Chandrabose, M.D. 225-227
90-Minute Panel PN PN40 Back Pain and Health Care Redesign:
Preparing for Accountable Care
James Rathmell, M.D. 228-230
90-Minute Panel PI PN103 Quality and Safety Challenges: Raising
the Bar on Oversees Surgical Care Trips
Richard Gillerman, M.D., Ph.D. 206-207
90-Minute Panel PD PN41 What Anesthesiologists Need to Know
About Resuscitating Kids in the OR
Jayant Deshpande, M.D.,
M.P.H.
255-257
Point-
Counterpoint
PI PC01 Life in the Time of Consolidation: Is
Bigger the New Better?
James Grant, M.D. 203-205
Point-
Counterpoint
CC PC02 We Give Too Much Fluid in the OR Ozan Akca, M.D.
Brian Kavanagh, M.B.
211-213
Residents and Medical
Students
RM03 Models of Practice Panel Roy Soto, M.D. R02-03
MCCS MCC01 Medically Challenging Case Presentations Hall B1
Oral
Presentations
CA OR09-1 Experimental Circulation 244
Oral
Presentations
FA OR13-1 Outcomes and Database Research - Cardiac Outcomes & Risk 243
Oral
Presentations
FA OR17-1 Respiration-Ventilation 245
8-10 a.m. Featured Lecture FA SPE01 Challenges in Anesthesiology: A European
Perspective
Daniela Filipescu, M.D. 265-268
120-Minute
Panel
RA PN01 Integrating Regional Anesthesia Into the
Perioperative Surgical Home
James Hebl, M.D. 217-219
120-Minute
Panel
CA PN02 Practice Guidelines in CV Anesthesia:
How Are We Doing as a Specialty?
Martin London, M.D. 252-254
Poster
Presentations
PN PO03-2 Chronic and Cancer Pain Hall B1-Area
A
Poster
Presentations
CC PO06-4 Critical Care Hall B1-Area
B
Poster
Presentations
FA PO08-3 Equipment, Monitoring and Engineering Technology: Circulation Hall B1-Area
C
Poster
Presentations
PI PO14-2 Patient Safety and Practice Management Hall B1-Area
D
Poster
Presentations
PD PO15-1 Pediatric Anesthesia Hall B1-Area
E
8-10:30 a.m. Hands-on
Workshop
FA DW01 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D., Gail
Randel, M.D., David Wong,
M.D.
353-355
8-11 a.m. Residents and Medical
Students
RM04a Medical Student Workshop - Ochsner
Health System
Mack Thomas, M.D. OFF SITE
Residents and Medical
Students
RM04b Medical Student Workshop - Louisiana
State University
Judy Johnson, M.D. OFF SITE
Residents and Medical
Students
RM04c Medical Student Workshop - Tulane
University
Lihua Zhang, M.D. OFF SITE
Hands-on
Workshop
FA 802 Workshop on Emergency Surgical Airway
Management Using a Pig Trachea Model
William Rosenblatt, M.D. 278-279
Seminar PI 803 Mastering Perioperative Stress and
Burnout: Exploring Methods of Essential
Mind-Fitness Developing Resilience at
Work
Kenneth Sapire, M.D. 281-282
Hands-on
Workshop
PN 804 Acupuncture Workshop Yuan-Chi Lin, M.D. 333-334
Seminar FA 805 Statistics for Anesthesiologists Jeffrey Gross, M.D. 335-336
SCHEDULE BY DAY: FRIDAY & SATURDAY
20
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Hands-on
Workshop
PD 806 Advanced Ultrasound Guided Pediatric
Regional Anesthesia Workshop
Amod Sawardekar, M.D. 338-339
Hands-on
Workshop
RA 807A Ultrasound-Guided Regional Anesthesia
and Clinical Skills Workshop: Introduction
to UGRA for Beginners
Adam Jacob, M.D. 346-347
8 a.m.-12 p.m. Cadaver
Workshops
PN CA01 Spinal Injections With Fluoroscopy-
Cadaver: Basic Techniques
Maunak Rana, M.D. 271-273
Hands-on
Workshop
PN 801 Ultrasound Guided Injections-Live Models:
BasicTechniques
Hariharan Shankar, M.B., B.S. 275-277
9-10:15 a.m. PBLD PI L013 Infection Prevention for the Anesthesia
Professional: What is the Least I Should
Know and How Do I Apply It to My
Practice?
Richard Beers, M.D. 343-345
PBLD FA L014 Management of Antiplatelet Therapy
in Patients With Coronary Stents for
Noncardiac Surgery
Davide Cattano, M.D., Ph.D. 343-345
PBLD RA L015 Nerve Injury After Peripheral Nerve
Blockade: Best Practices and Medical-
Legal Protection Strategies
H. David Hardman, M.D.,
M.B.A.
343-345
PBLD PD L016 Trials and Tribulations: Interventional
Management for Recurrent Complex
Regional Pain Syndrome in Children
Stephen Hays, M.D. 343-345
PBLD FA L017 Perioperative Laboratory and Cardiac
Testing: What Is Necessary?
David Hepner, M.D. 343-345
PBLD PI L018 To Coerce or Not to Coerce: What Are the
Questions?
Norma Klein, M.D. 343-345
PBLD FA L019 I Swear It Will Only Take 15 Minutes:
Anesthesia/Sedation for TEE/
Cardioversion
Julia Metzner, M.D. 343-345
PBLD OB L020 Placenta Percreta: Preparation and
Management
Cathleen Peterson-Layne,
Ph.D., M.D.
343-345
PBLD AM L021 It’s Just a Cataract: How a Simple Thing
Can Go Bad
Michael Pilla, M.D. 343-345
PBLD FA L022 Perioperative Management of the Anemic
Patient
Russell Roberson, M.D. 343-346
PBLD RA L023 Analgesic Options for a 68-Year-Old Man
with Multiple Rib Fractures
Mark Leibel, M.D.
Kristopher Schroeder, M.D.
343-345
PBLD PD L024 Tonsillectomy and Adenoidectomy in a
Child With Down Syndrome More to It
Than You Think!
Catherine Seipel, M.D. 343-345
Hands-on
Workshop
FA AW01 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
9:15-10:15 a.m. RCL OB 107 Postpartum Hemorrhage Jill Mhyre, M.D. RiverGate
RCL CC 108 Pulmonary Hypertension and Right
Ventricular Failure
Eric Jacobsohn, M.B.Ch.B. E-1
RCL NA 109 Adult Head Injury: Management Update
and Controversies
Audree Bendo, M.D., Martin
Smith, M.B., B.S.
E-2
RCL RA 110 Upper Extremity Regional Anesthesia:
Essentials for Your Practice
Joseph Neal, M.D. E-3
RCL PN 111 The Role of Perioperative Physicians in
Prevention of Chronic Pain After Surgery
Asokumar Buvanendran, M.D. 260-262
RCL CA 112 Perioperative Management of
Cardiovascular Implantable Electronic
Devices
Annemarie Thompson, M.D. La Nouvelle
Ballroom AB
9:30-11 a.m. Residents and Medical
Students
RM05 Resident Written Board Prep Sajid Shahul, M.D.
Cindy Ku, M.D.
R02-03
Residents and Medical
Students
RM06 Subspecialty Panel Walter Maurer, M.D.
Arthur Calimaran, M.D.
R04-05
10-11:30 a.m. Poster
Discussions
PN PD03-1 Chronic and Cancer Pain 245
Poster
Discussions
FA PD08-1 Equipment, Monitoring and Engineering Technology: Utilizing Technology -
Imaging and Closed Loop Systems
244
EDUCATION
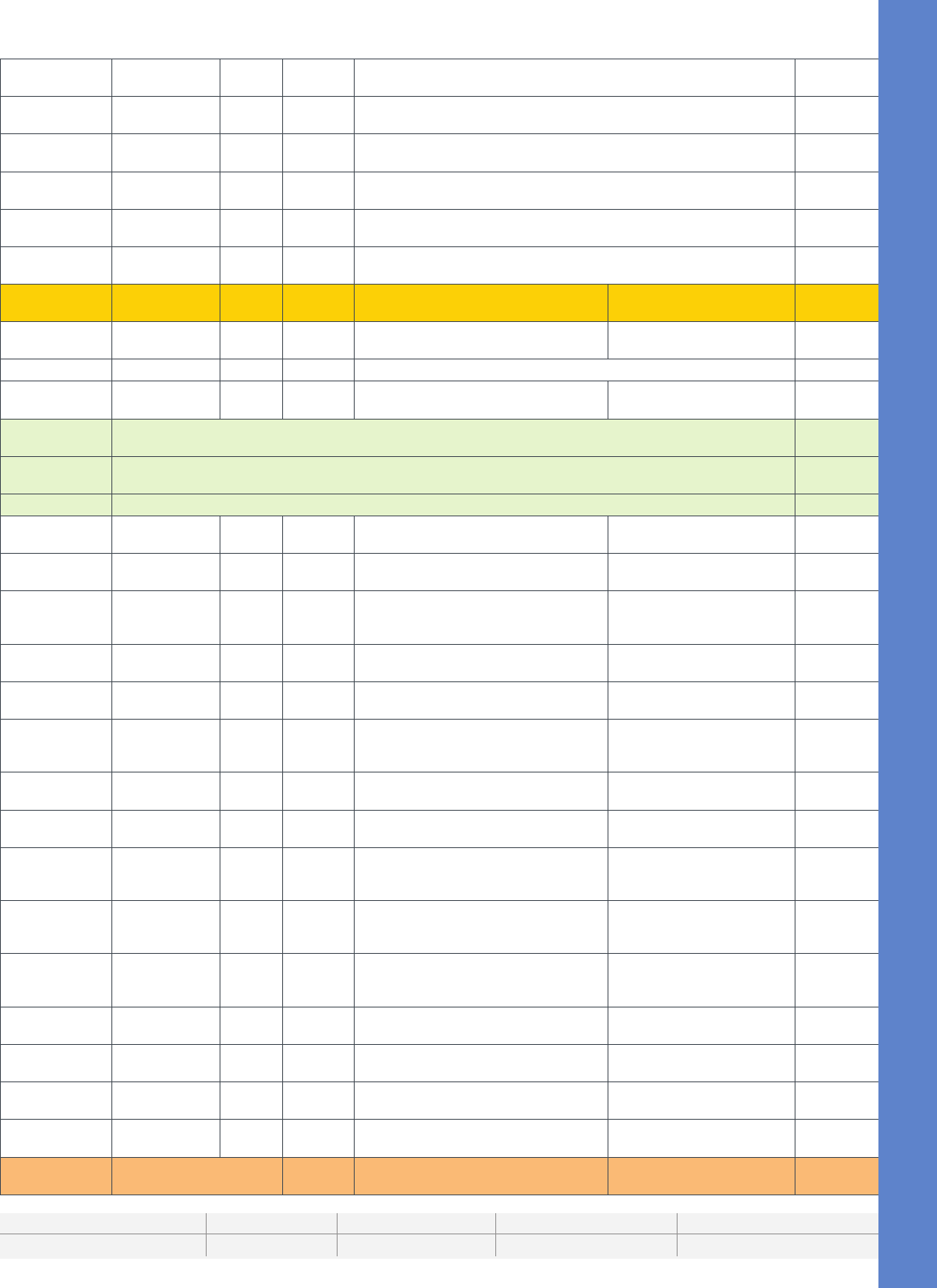
21
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Poster
Discussions
OB PD12-1 Obstetric Anesthesia: Cesarean Delivery 243
10 a.m.-12 p.m. Poster
Presentations
CA PO04-2 Clinical Circulation: Outcomes Hall B1-Area
A
Poster
Presentations
CA PO09-3 Experimental Circulation Hall B1-Area
B
Poster
Presentations
NA PO10-2 Experimental Neurosciences: Mechanisms Hall B1-Area
C
Poster
Presentations
FA PO13-3 Outcomes and Database Research Hall B1-Area
D
Poster
Presentations
RA PO16-1 Regional Anesthesia and Acute Pain Hall B1-Area
E
10:30-11:45
a.m.
Featured Lecture SPE02 ANESTHESIOLOGY™ 2014 Opening
Session
Jason Hwang, M.D., M.B.A. Great Hall
Hands-on
Workshop
FA AW02 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.
William Simmons, M.D.
356-357
10:30-12 p.m. MCCS MCC02 Medically Challenging Case Presentations Hall B1
10:30 a.m.-1
p.m.
Hands-on
Workshop
FA DW02 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D. 353-355
11 a.m.-
4:30 p.m.
Scientic & Educational Exhibits Hall C
11 a.m.-
6:30 p.m.
Afliated Subspecialty Society Pavillion (Connection Center) Booth #111
Exhibits (Connection Center) Hall B2-D
12-1:15 p.m. Hands-on
Workshop
FA AW03 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O., William
Simmons, M.D.
356-357
12:30-1:45 p.m. PBLD NA L025 Delayed Emergence After Craniotomy-No
Delays Accepted
Ra Avitsian, M.D. 343-345
PBLD PD L004 When It Rains, It Pours; Large AVM Heart
Failure Pulmonary HTN and Now There Is
V-tach!
Christina Diaz, M.D. 343-345
PBLD CA L026 Carotid Endarterectomy: Asleep Versus
Awake
Jeffrey Dobyns, D.O. 343-345
12:30-1:45 p.m. PBLD NA L025 Delayed Emergence After Craniotomy-No
Delays Accepted
Ra Avitsian, M.D. 343-345
PBLD PD L004 When It Rains, It Pours; Large AVM Heart
Failure Pulmonary HTN and Now There Is
V-tach!
Christina Diaz, M.D. 343-345
PBLD CA L026 Carotid Endarterectomy: Asleep Versus
Awake
Jeffrey Dobyns, D.O. 343-345
PBLD CC L027 Elderly Man; Going into Shock; Needs
Fluids Now!
Elizabeth Frost, M.B., Ch.B. 343-345
PBLD OB L029 Labor Analgesia and Postpartum Tubal
Ligation in a Patient with a History of
Spinal Instrumentation
Michael Hofkamp, M.D. 343-345
PBLD NA L030 My Ulnar Neuropathy Has Resolved. Now I
Have to Go for Spine Surgery in the Prone
Surrender Position
Ihab Kamel, M.D. 343-345
PBLD NA L031 Why Does My Patient Scheduled for
Endoscopy Sinus Surgery Have Severe
Groin Pain?
Kirk Lalwani, M.D.
ChristineMartin, M.D.
343-345
PBLD AM L032 PONV, PDNV and Long QT Syndrome:
Balancing Risk and Benet
AnujMalhotra, M.D. 343-345
PBLD PI L033 Burned Out Anesthesiologist: Practice
Competence and Colleagues
Sergey Pisklakov, M.D. 343-345
PBLD FA L034 My Patients Never Have Residual
Paralysis in the PACU, or Do They?
Stephan Thilen, M.D., M.S. 343-345
PBLD PI L035 Anesthetic Options for Patients
Undergoing Dialysis Access Procedures
Derek Woodrum, M.D. 343-345
1-2 p.m. Residents and Medical
Students
RM07 Practice Management I Erica Stein, M.D. R02-03
SCHEDULE BY DAY: SATURDAY
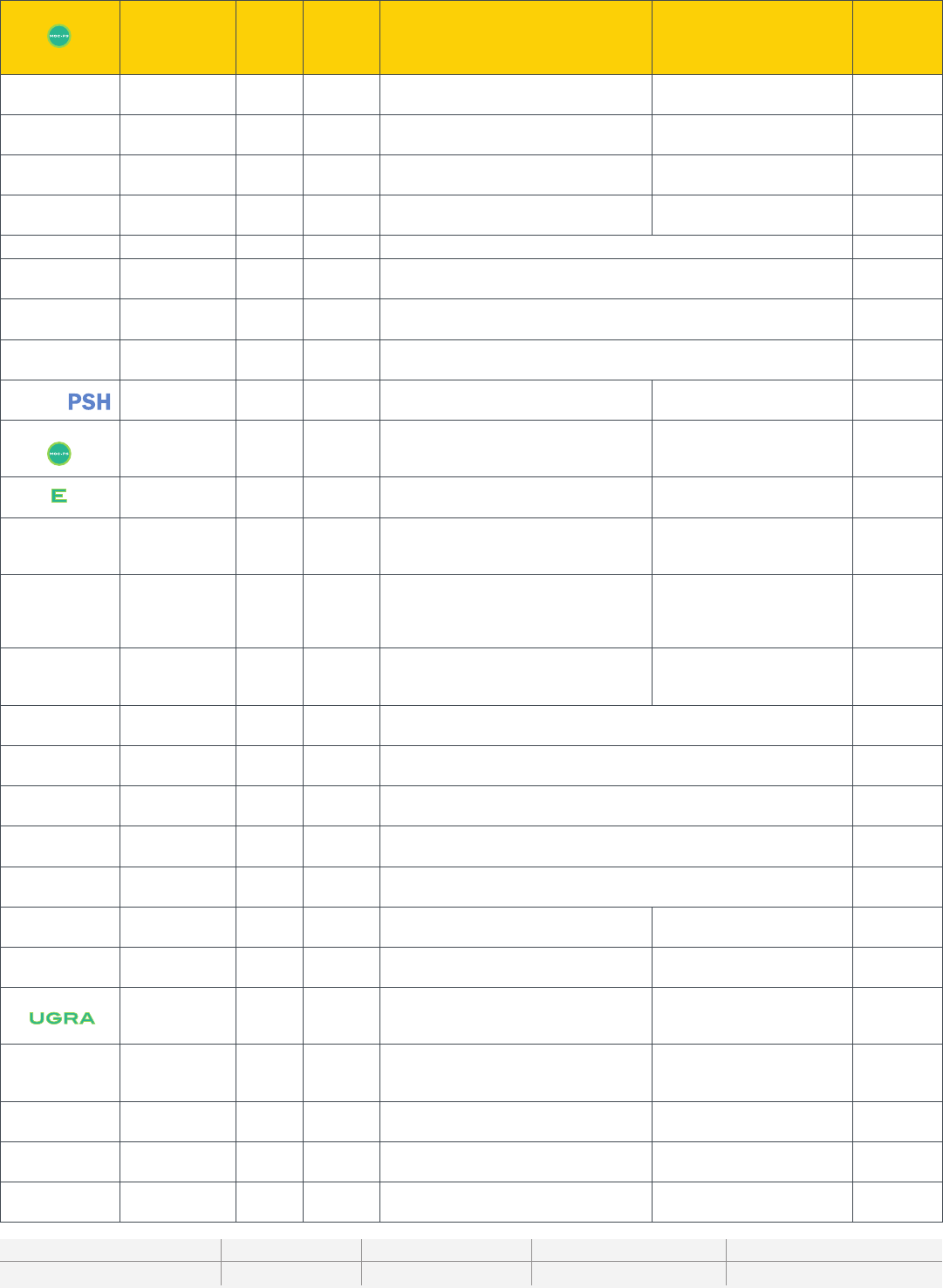
22
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Featured Lecture FA SPE03 ASA/APSF Ellison C. Pierce Jr., M.D.
Patient Safety Memorial Lecture:
Competence and Teamwork Are Not
Enough: The Value of Cognitive Aids
David Gaba, M.D. Great Hall B
1-2:30 p.m. 90-Minute Panel CC PN42 Red Blood Cells: Good, Bad, and Ugly and
Some Solutions
Jonathan Jahr, M.D. 217-219
Clinical Forum AM CF01 Pediatric Ambulatory Anesthesia: Clinical
Forum
Lucinda Everett, M.D. 206-207
Clinical Forum PN CF02 Complications in Pain Medicine and
Preventive Strategies
Hariharan Shankar, M.B., B.S.,
B.S.
211-213
Point-
Counterpoint
CC PC03 Tidal Volumes Don’t Really Matter to the
Anesthesiologist
James Blum, M.D., Daniel
Talmor, M.D., Ph.D.
203-205
MCCS MCC03 Medically Challenging Case Presentations Hall B1
Oral
Presentations
OR04-1 Clinical Circulation: Outcome 244
Oral
Presentations
OR06-1 Critical Care 243
Oral
Presentations
OR14-1 Patient Safety and Practice Management 245
1-3 p.m. 120-Minute
Panel
PI PN03 Setting Up a Perioperative Surgical Home Zeev Kain, M.D., M.B.A. 208-210
120-Minute
Panel
CA PN04 Perioperative Patient Safety in
Cardiovascular Surgery: From Data to
Implementation
Nancy Nussmeier, M.D. 220-222
120-Minute
Panel
PI PN05 Whose Guidelines and Practice
Parameters Apply to Anesthesiologists?
John Butterworth, IV, M.D. 225-227
120-Minute
Panel
NA PN06 Babies Are Not Just Large Rat Pups:
Controveries on the Impact of Anesthetics
on the Developing Brain
Sulpicio Soriano, M.D. 228-230
120-Minute
Panel
PN PN07 Evidenced Based Chronic Pain
Management in Children and
Adolescents:Is There Evidence or Is It
Bias?
Santhanam Suresh, M.D. 252-254
120-Minute
Panel
AM PN08 Anesthesia and Sedation for MRI:
Adapting to Technological Advances and
Demands
Keira Mason, M.D. 255-257
Poster
Presentations
AM PO01-1 Ambulatory Anesthesia: Risk Factors, Outcomes and Recovery Hall B1-Area
A
Poster
Presentations
FA PO08-5 Equipment, Monitoring and Engineering Technology:Ventilation and
Supraglotic Airways
Hall B1-Area
B
Poster
Presentations
PI PO11-1 History and Education:Challenges:Present and Future Hall B1-Area
C
Poster
Presentations
OB PO12-2 Obstetric Anesthesia: Labor Analgesia, Patient Safety and Miscellaneous. Hall B1-Area
D
Poster
Presentations
RA PO16-4 Regional Anesthesia and Acute Pain Hall B1-Area
E
1-4 p.m. Hands-on
Workshop
CA 809 Pacemakers and ICDs Aman Mahajan, M.D., Ph.D. 278-279
Hands-on
Workshop
AM 810 Must Know Blocks for Ambulatory
Anesthesia
David Auyong, M.D. 265-268
Hands-on
Workshop
RA 807B Ultrasound-Guided Regional Anesthesia
and Clinical Skills Workshop: Introduction
to UGRA for Beginners
Adam Jacob, M.D. 352
1-5 p.m. Cadaver
Workshops
PN CA02 Spinal Injections With Fluoroscopy-
Cadaver: Advanced Techniques (Cervical/
Thoracic)
Timothy Lubenow, M.D. 271-273
Hands-on
Workshop
PN 808 Ultrasound Guided Injections-Live Models:
Advanced Techniques
Philip Peng, M.B.B.S. 275-277
1:30-2:30 p.m. RCL PN 113 Complex Regional Pain Syndrome: What’s
New?
Richard Rauck, M.D. E-3
RCL NA 114 Blood Pressure and the Brain: How Low
Can You Go?
John Drummond, M.D. 260-262
EDUCATION

23
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
SCHEDULE BY DAY: SATURDAY
RCL CA 115 Perioperative Lung Protective Strategies in
One-Lung and Two-Lung Ventilation
Peter Slinger, M.D. La Nouvelle
Ballroom AB
RCL FA 127 Hospital System Failures and Hazard
Management in the Operating Room
P. Allan Klock, Jr., M.D. E-1
RCL FA 128 Human Errors IU Medicine: What They
Should Mean to Patients, Providers and
the Public
Robert Lagasse, M.D. E-2
1:30-2:45 p.m. Hands-on
Workshop
FA AW04 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O., William
Simmons, M.D.
356-357
2-3 p.m. Residents and Medical
Students
RM08 Practice Management II Judith Jurin Semo, J.D., Esq. R02-03
2-4 p.m. Featured Lecture CA SPE04 Perioperative Cardiology: Results from
VISION, POISE-2, SIRS and ENIGMA-2
Daniel Sessler, M.D. Great Hall A
Featured Lecture FA SPE05 Anesthesia Patient Safety Foundation
Workshop: Competence and Teamwork
Are Not Enough: Implementing Emergency
Manuals and Checklists
Jeffrey B. Cooper, Ph.D. Great Hall B
Seminar PN 811 Spinal Imaging for the Pain Medicine
Physician
Wyndam Strodtbeck, M.D. 338-339
2:30-5 p.m. Hands-on
Workshop
FA DW03 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D. 353-355
2:45-3:45 p.m. RCL OB 116 Anesthetic Management of the
Preeclamptic Patient
Joy Hawkins, M.D. RiverGate
RCL RA 117 Making Regional Anesthesia Work in the
Real World
Francis Salinas, M.D. E-1
RCL FA 118 Anesthesia for Major Orthopedic Surgery Andrew Rosenberg, M.D. E-2
RCL CC 119 Mechanical Ventilatory Support: What
Every Anesthesiologist Should Know
Michael Gropper, M.D., Ph.D. E-3
RCL FA 120 Operating Room Fire Safety William Culp, Jr., M.D. 260-262
3-4:15 p.m. Hands-on
Workshop
FA AW05 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O., William
Simmons, M.D.
356-357
3-4:30 p.m. MCCS MCC04 Medically Challenging Case Presentations Hall B1
Poster
Discussions
PD PD15-1 Pediatric Anesthesia: Cardiac 244
Poster
Discussions
RA PD16-1 Regional Anesthesia and Acute Pain 245
Oral
Presentations
PI OR11-1 History and Education: Novel Ways to Teach and Learn 243
3-5 p.m. RCL NA 121 Smart Seniors: Avoiding Perioperative
Brain Failure
Gregory Crosby, M.D. La Nouvelle
Ballroom AB
3:30-4:45 p.m. PBLD RA L037 Postoperative Ulnar Neuropathy - Could I
Have Done Something to Prevent It?
Sanjay Bhananker, M.B., B.S. 343-345
PBLD FA L036 Anesthetic Management of a Patient With
Penetrating Chest Trauma
Charles Smith, M.D. 343-345
PBLD AM L038 Is Ambulatory Shoulder Surgery Safe in a
Patient With Obstructive Sleep Apnea?
Christopher Canlas, M.D. 343-345
PBLD PD L039 Wake Up Your Surgery Is Not Over Prabhakar Devavaram, M.B.,
B.S
343-345
PBLD NA L040 Ah! I Can’t Bear It! This Is the Worst
Headache of My Life!
Stanlies D’Souza, M.D.,
F.R.C.A
343-345
PBLD PD L041 I Passed Gas in the Operating Room. Are
Volatile Agents Really Silent and Deadly to
Patients With Muscular Dystrophy?
Matthew Green, M.D. 343-345
PBLD CA L042 I Thought Three Pump Runs Were Bad but
This Pulmonary Edema is Even Worse!
What is Going On?
Marcellene Franzen, M.D.
Lindsey Loveland-Baptist, M.D.
343-345
PBLD OB L043 Anesthesia for an Hypoplastic Left Heart
Syndrome Parturient
David Mann, M.D. 343-345
SCHEDULE BY DAY: SATURDAY

24
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
PBLD OB L044 Anesthetic Management of Cesarean
Delivery for a Parturient With Previous
Myocardial Infarction and Coronary Artery
Stents
Daria Moaveni, M.D. 343-345
PBLD FA L045 Blood IS Thicker Than Water: Anesthetic
Concerns of Hypercoagulability
Gregory Rose, M.D. 343-345
PBLD FA L046 Prevention and Management of
Intraoperative Awarenessin High Risk
Patients
Kathleen Smith, M.D. 343-345
PBLD PI L047 Hold My Compass: Tools and Tips so
YOU Don’t Get Lost in the EP Lab
Mark Weiss, M.D. 343-345
3:30-5 p.m. 90-Minute Panel AM PN43 Advanced Diagnostic Bronchoscopy:
Coming Soon to an ASC near You
Basem Abdelmalak, M.D. 208-210
90-Minute Panel CA PN44 Thoracic Surgery 2014 Nathaen Weitzel, M.D. 217-219
90-Minute Panel CC PN45 Optimizing Perioperative Hepatic Function Randolph Steadman, M.D.,
M.S.
220-222
90-Minute Panel PN PN46 Radiofrequency Ablation for Spinal Pain:
Techniques to Optimize Success
Kevin Vorenkamp, M.D. 225-227
90-Minute Panel NA PN47 Management of Neurological Events After
Anesthesia
Deborah Rusy, M.D. 228-230
90-Minute Panel RA PN48 Regional Anesthesia in Children: What
Have We Learned From Large Prospective
Databases?
Santhanam Suresh, M.D. 252-254
90-Minute Panel PI PN49 Governmental Inuences Over Health
Care: Lessons Learned From Working on
Capitol Hill
Andrew Gettinger, M.D. 255-257
Clinical Forum CA CF03 Circulatory Assist: The Coming Tidal Wave Roman Sniecinski, M.D. 206-207
Point-
Counterpoint
CC PC04 Do We Really Need Risk Adjustment to
Measure Outcomes?
Avery Tung, M.D., Laurent
Glance, M.D.
203-205
Point-
Counterpoint
RA PC05 Ultrasound-Guided Regional Anesthesia--
Pushing the Limits or Over the Edge
Meg Rosenblatt, M.D., Anahi
Perlas, M.D.
211-213
3:30-5:30 p.m. Residents and Medical
Students
RM09 Residency Meet and Greet Chad Greene La Nouvelle
Ballroom C
4-5 p.m. RCL FA 122 Mastering Anesthesia for the Elderly
Patient
Jeffrey Silverstein, M.D. RiverGate
RCL OB 123 Dural Puncture and Headache: Let’s Keep
It the Patient’s Headache
Robert Gaiser, M.D. E-1
RCL CC 124 Transfusion Therapy: Optimal Use of
Blood Products
Stephen Surgenor, M.B.A.,
M.D.
E-2
RCL PD 125 Pediatric Ambulatory Anesthesia:
Challenges and Controversies
Linda Mason, M.D. E-3
RCL RA 126 Regional Anesthesia to Improve Long
Term Outcomes After Surgery
Michael Andreae, M.D., M.S. 260-262
5-6:30 p.m. ASA Welcome Reception (Exhibit Hall) Connection Center
EDUCATION

25
Did you know NACOR* is the only anesthesia
QCDR and can help your practice avoid
payment penalties by meeting PQRS
requirements?
Sound like alphabet soup to you?
Need clarication?
Visit AQI in the Resource Center to learn how ASA
has partnered with AQI to offer your group practice this
exciting new member benet.
*The National Anesthesia Clinical Outcomes Registry, maintained by the Anesthesia Quality Institute, has been designated as a Qualied Clinical Data
Registry by the Centers for Medicare and Medicaid Services for PQRS reporting.
HOT TOPIC
PQRS Reporting via the
QCDR Reporting Channel
Sunday, October 12,
10-11 a.m., Room 252-254
Lead speaker:
Richard Dutton,
M.D., M.B.A.

26
EDUCATION
SUNDAY, OCT. 12
Time Session Type Track Fee Code Title Speaker Location
6 a.m. Hope For The Warriors® - Run For The Warriors®
Check in at the Run For The Warriors
Booth for details on the race
7 a.m.-5 p.m. Registration Lobby A & D
7 a.m.-5 p.m. ASA Resource Center Convention Center, Hall B-1
7 a.m.-5 p.m. International Connection Lounge Lobby A
7-8:15 a.m. Subspecialty
Panels
FA 603 (STA) How Can Mobile Technology Help
Me Help My Patients?
Maxime Cannesson, M.D.,
Ph.D.
228-230
Subspecialty
Panels
CC 604 (SOCCA) Trauma and Critical Care Pearls
for the Non-Intensivists
Daniel Brown, M.D., Ph.D. 231-232
Subspecialty
Panels
AM 605 (SAMBA) TIVA in 2014 Steven Butz, M.D. 238-239
7:15-8:30 a.m. PBLD OB L048 Cesarean Delivery in a Patient With
Hypertrophic Obstructive Cardiomyopathy
Jaime Aaronson, M.D.
Stephanie Goodman, M.D.
343-345
PBLD NA L049 Delayed Emergence After Craniotomy-No
Delays Accepted
Ra Avitsian, M.D. 343-345
PBLD RA L050 Perioperative Management of the Patient
on Anticoagulant Therapy: A Fresh Look at
an Old Problem
Richard Beers, M.D. 343-345
PBLD FA L051 Beyond Swiss Cheese - Cases for the
Anesthesia Patient Safety Ofcer
Jonathan Cohen, M.D. 343-345
PBLD FA L052 A Patient With a Temperature of 102.5 F
and Rigors 3 hours after Surgery
Theresa Gelzinis, M.D. 343-345
PBLD RA L053 Antibrinolytic Use in Major Orthopedic
Procedures: What’s the Bloody
Controversy?
Yan Lai, M.D. 343-345
PBLD CA L054 I Thought Three Pump Runs Were Bad but
This Pulmonary Edema is Even Worse!
What is Going On?
Marcellene Franzen, M.D.,
Lindsey Loveland-Baptist, M.D.
343-345
PBLD NA L055 Deep Brain Stimulation for Parkinson’s
Disease: What Is the Role of the
Anesthesiologist?
Julia Metzner, M.D. 343-345
PBLD AM L056 It’s Just a Cataract: How a Simple Thing
Can Go Bad
Michael Pilla, M.D. 343-345
PBLD PI L057 Burned Out Anesthesiologist: Practice
Competence and Colleagues
Sergey Pisklakov, M.D. 343-345
PBLD PI L058 The Impaired Anesthesiologist: More Than
Just Drugs and Alcohol
Gregory Rose, M.D. 343-345
PBLD PI L060
Anesthetic Options for Patients
Undergoing Dialysis Access Procedures
Derek Woodrum, M.D. 343-345
8-9 a.m. RCL CC 202 Respiratory Physiology and Perioperative
Gas Exchange
Luca Bigatello, M.D. E-1
RCL PD 203 Current Controversies in Pediatric
Anesthesia
Lena Sun, M.D. E-2
RCL CA 204 Rethinking Acute Blood Pressure
Management in the Perioperative Setting
Solomon Aronson, M.D.,
M.B.A., FACC, FCCP, FAHA,
FASE
E-3
RCL AM 205 Anesthesia for Outpatient Diagnostic and
Therapeutic Radiology
Thomas Cutter, M.D. 260-262
RCL CA 206 Preoperative Cardiac Evaluation for
Noncardiac Surgery
Lee Fleisher, M.D. La Nouvelle
Ballroom AB
8-9:30 a.m. 90-Minute Panel PN PN101 Neuropathic Pain: From Mechanisms to
Outcomes
Jianguo Cheng, M.D. 252-254
90-Minute Panel FA PN50 Airway Management Training: Are We
Keeping Up With Technology?
Nicholas Nedeff, M.D. 208-210
90-Minute Panel CA PN51 Heart Failure in Adults Undergoing Non-
Cardiac Surgery
Amanda Fox, M.D., M.P.H. 217-219
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain

27
90-Minute Panel CC PN52 Simulation Education in Competency-
Based Training and Assessment: Present
and Future
Randall Schell, M.D., M.Ed. 220-222
90-Minute Panel NA PN53 The Yin and Yang of Anesthetic Drugs: Are
They Neuroprotective or Neurotoxic?
Piyush Patel, M.D. 225-227
Clinical Forum FA CF04 Evidence-Informed Anesthesia for the
Severely Obese; Example Obstetrics and
Gynecology - Does It Exist ?
Roman Schumann, M.D. 206-207
Point-
Counterpoint
PN PC06 Long-Term Opioid Treatment for Chronic
Non-Malignant Pain
Gary Brenner, M.D., Ph.D.,
Rene Przkora, M.D., Ph.D.
203-205
Point-
Counterpoint
OB PC07 Combined Spinal-Epidural Labor
Analgesia: Forevermore or Nevermore?
Cynthia Wong, M.D. 211-213
MCCS MCC05 Medically Challenging Case Presentations Hall B1
Oral
Presentations
PN OR03-1 Chronic and Cancer Pain 243
Oral
Presentations
PI OR14-2 Patient Safety and Practice Management 245
Poster
Discussions
NA PD05-2 Clinical Neurosciences 244
8-10 a.m. Featured Lecture PI SPE06 WFSA Panel: Government Funded
Healthcare and Anesthesia – An
International Perspective on Successes
and Failures
Adrian Gelb, M.B., B.Ch.,
FRCPC
Great Hall B
Poster
Presentations
FA PO02-1 Anesthetic Action and Biochemistry: Efcacy and Safety of Current and
Emerging Anesthetics and Analgesics
Hall B1-Area
C
Poster
Presentations
CA PO04-1 Clinical Circulation: Echo/Monitoring Hall B1-Area
E
Poster
Presentations
NA PO10-1 Experimental Neurosciences: Neurotoxicity Hall B1-Area
D
Poster
Presentations
FA PO13-1 Outcomes and Database Research Hall B1-Area
A
8-10:30 a.m. Hands-on
Workshop
FA DW04 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D. 353-355
8-11 a.m. Hands-on
Workshop
PD 812 Pediatric Airway Workshop Narasimhan Jagannathan,
M.D.
346-347
Seminar CC 813 Perioperative Resuscitation - What’s New? Steven Robicsek, M.D., Ph.D. 348-349
8 a.m.-12 p.m. Cadaver
Workshops
PN CA03 Introduction to Ultrasound and
Fluoroscopic-Guided Techniques for
Chronic Pain Management: Live Models
and Cadavers
David Provenzano, M.D. 271-273
Cadaver
Workshops
PN CA04 Head and Neck Blocks (Ultrasound and
Fluoroscopy) - Cadaver and Live Models
Miles Day, M.D. 275-277
House of Delegates SPE07 House of Delegates: Session I Jane C.K. Fitch, M.D. Grand
Ballroom
Hilton
Riverside
8 a.m.-4 p.m. Hands-on
Workshop
CA 815 Basic TEE Workshop Sasha Shillcutt, M.D. 338-339
9-10:15 a.m. PBLD FA L061 Anesthetic Management of a Patient With
Penetrating Chest Trauma
Charles Smith, M.D. 343-345
PBLD CC L062 Surviving Septic Shock in the Operating
Room and Beyond: What Do the
Guidelines Say?
Roman Dudaryk, M.D. 343-345
PBLD OB L063 Just Another Day on Labor and Delivery:
Morbid Obesity and Preeclampsia
Regina Fragneto, M.D. 343-345
PBLD NA L064 Just Another Subarachnoid Hemorrhage?
Or Am I Really Up-to-date on What to Do?
Eduardo Galeano, M.D. 343-345
PBLD PD L065 I Passed Gas in the Operating Room. Are
Volatile Agents Really Silent and Deadly to
Patients With Muscular Dystrophy?
Matthew Green, M.D. 343-345
PBLD RA L066 Nerve Injury/Dysfunction and Peripheral
Nerve Blockade: Fact or Fiction
Thomas Halaszynski, M.D.,
M.B.A.
343-345
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
SCHEDULE BY DAY: SUNDAY

28
PBLD OB L067 Labor Analgesia and Postpartum Tubal
Ligation in a Patient With a History of
Spinal Instrumentation
Michael Hofkamp, M.D. 343-345
PBLD CA L068 Patient With a Failing Fontan for
Emergency Exploratory Laparotomy
Galina Leyvi, M.D. 343-345
PBLD FA L069 Prevention and Management of
Intraoperative Awareness in High Risk
Patients
Kathleen Smith, M.D. 343-345
PBLD FA L070 Airway Management of a Patient With
Penetrating Neck Injury
Albert Varon, M.D. 343-345
PBLD PI L071 Anesthesiologists and Terminal Live Organ
Donation: You Want Me to Do What?
Richard Wolman, M.D., M.A. 343-345
PBLD PD L072 Application of Pediatric Advanced
Life Support for Managing a Patient
With a Debrillator Who Develops an
Intraoperative Cardiac Arrest
David Young, M.D., M.Ed 343-345
Hands-on
Workshop
FA AW06 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
9 a.m.-4 p.m. Scientic and Educational Exhibits (Connection Center) Hall C
Exhibits (Connection Center) Hall B2-D
Afliated Subspecialty Soceity Pavillion (Connection Center) Booth #111
9:15-10:15 a.m. RCL OB 207 Neurologic Complications of Neuraxial
Anesthesia in Obstetrics
David Wlody, M.D. RiverGate
RCL PI 208 Decision Making Errors in Anesthesiology Marjorie Stiegler, M.D. E-1
RCL CA 209 Congenital Heart Disease in the Adult
Presenting for Non-Cardiac Surgery
Ilka Theruvath, M.D. E-2
RCL PN 210 Modern Concepts in Spinal Cord
Stimulation
Timothy Deer, M.D. E-3
RCL FA 211 Perioperative Management of Patients
With Left Ventricular Assist Devices
Undergoing Noncardiac Surgery
Michael O’Connor, M.D. 260-262
RCL PD 212 New Guidelines: Pediatric Advanced Life
Support for the Anesthesiologist
Eugenie Heitmiller, M.D. La Nouvelle
Ballroom AB
10-11 a.m. Featured Lecture SPE27 PQRS Reporting Via the QCDR Reporting
Channel
Richard Dutton, M.D., M.B.A. 252-254
10-11:30 a.m. 90-Minute Panel OB PN54 Cutting-Edge, Technologies and Point-
of-Care Devices to Improve Care of the
Obstetric Patient
Brendan Carvalho, F.R.C.A. 208-210
90-Minute Panel PD PN55 Pediatric Adenotonsillectomy: Enhancing
Quality and Efciency; Ensuring Safety
LynneMaxwell, M.D. 217-219
90-Minute Panel PI PN56 Beating Back Burnout: Strategies for
Career Longevity and Improved Patient
Care
Mary AnnVann, M.D. 220-222
90-Minute Panel PI PN57 Not All That Glitters is Gold-How Do I
Judge Quality from My Experience as a
Surgical Outpatient?
Armin Schubert, M.D. 225-227
90-Minute Panel RA PN58 Nerve Injury Following Regional
Anesthesia
Vincent Chan, M.D. 228-230
90-Minute Panel PI PN59 Professionalism - An International
Perspective
Saundra Curry, M.D. 255-257
Clinical Forum CA CF05 Adult Congenital Heart Disease
(ACHD):Special Considerations for
Patients With CHD Surviving Into
Adulthood
James DiNardo, M.D. 206-207
Point-
Counterpoint
FA PC08 Perioperative Colloid Administration -
Should it be Abandoned?
Marc Rozner, Ph.D., M.D.,
John Drummond, M.D.
211-213
Poster
Presentations
CC PO06-1 Critical Care Hall B1-Area
D
Poster
Presentations
FA PO08-1 Equipment, Monitoring and Engineering Technology: Securing the Airway Hall B1-Area
C
Poster
Presentations
PI PO14-1 Patient Safety and Practice Management Hall B1-Area
B
EDUCATION
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain

29
Poster
Presentations
PD PO15-2 Pediatric Anesthesia Hall B1-Area
E
Poster
Presentations
RA PO16-2 Regional Anesthesia and Acute Pain: Ultrasound Guided RA Hall B1-Area
A
10 a.m.-12 p.m. Residents and Medical
Students
RM10 Medical Resident Component House of
Delegates
Mark Bicket, M.D. R02-03
10 a.m.-1 p.m. Residents and Medical
Students
RM11 Medical Student Component House of
Delegates
Chad Greene R04-05
10:30-11:30
a.m.
RCL AM 213 Adult Patient With Morbid Obesity and
OSA for Ambulatory Surgery: An Update
Girish Joshi, M.B.B.S., M.D.,
FFARCSI
RiverGate
RCL OB 214 Hail Caesar: Anesthesia for Cesarean
Delivery
Lawrence Tsen, M.D. E-1
RCL CA 215 Catheter Based Cardiac Surgery:
Anesthesia in the Hybrid Suite and Cath
Lab
Nathaen Weitzel, M.D. E-2
RCL PN 216 Head and Neck Pain: A Clinical Approach Samer Narouze, M.D., Ph.D. E-3
RCL PD 217 Anesthesia for the Patient With Congenital
Heart Disease for Emergent Non-Cardiac
Surgery: Are You Well Equipped?
Dean Andropoulos, M.D. 260-262
RCL CC 218 The Evidence Behind Evidence-Based
Medicine
Brian Kavanagh, M.B. La Nouvelle
Ballroom AB
Oral
Presentations
FA OR13-2 Outcomes and Database Research - Evaluation of Risk 244
Poster
Discussions
CA PD04-2 Clinical Circulation: Blood, Other 243
10:30-11:45
a.m.
Hands-on
Workshop
FA AW07 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
10:30 a.m.-
12 p.m.
MCCS MCC06 Medically Challenging Case Presentations Hall B1
10:30 a.m.-
1 p.m.
Hands-on
Workshop
FA DW05 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D. 353-355
12-1:15 p.m. Hands-on
Workshop
FA AW08 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
12:30-1:30 p.m. RCL PD 219 Anesthetic Induced Neurotoxicity in
Pediatric Patients: A Status Update
Randall Flick, M.D., M.P.H. E-2
RCL PN 220 Radiofrequency Ablation for the Treatment
of Spine Pain: Understanding the Basic
Principles and Clinical Applications
David Provenzano, M.D. E-3
RCL PD 221 Neonatal Emergencies: Simple Approach
to Success
Samuel Wald, M.D. 260-262
RCL RA 222 Hemorrhagic and Infectious Complications
of Neuraxial Anesthesia
Terese Horlocker, M.D. La Nouvelle
Ballroom AB
Featured Lecture FA SPE08 Society for Airway Management Lecture:
The Airway Approach Algorithm: What
Would Andy Say?
William Rosenblatt, M.D. Great Hall B
12:30-1:45 p.m. PBLD PI L073 Do You Want to Present a PBLD at the
2015 ASA Meeting? This PBLD Session
Could Help You
Sanjay Bhananker, M.B., B.S. 343-345
PBLD NA L074 Ah! I Can’t Bear It! This Is the Worst
Headache of My Life!
Stanlies D’Souza, M.D.,
F.R.C.A
343-345
PBLD PN L075 Opioid-Induced Hyperalgesia Tolerance
and Chronic Postsurgical Pain; a
Dilemma Complicating Postoperative Pain
Management
Dalia Elmofty, M.D. 343-345
PBLD RA L076 Nerve Injury After Peripheral Nerve
Blockade: Best Practices and Medical-
Legal Protection Strategies
H. David Hardman, M.D.,
M.B.A.
343-345
PBLD PI L077 To Coerce or Not to Coerce: What Are the
Questions?
Norma Klein, M.D. 343-345
PBLD OB L078 Anesthesia for an Hypoplastic Left Heart
Syndrome Parturient
David Mann, M.D. 343-345
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
SCHEDULE BY DAY: SUNDAY

30
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
PBLD OB L079 Anesthetic Management of Cesarean
Delivery for a Parturient With Previous
Myocardial Infarction and Coronary Artery
Stents
Daria Moaveni, M.D. 343-345
PBLD FA L080 It’s Only a MAC Case and Now My Patient
is on FIRE!
Mark Phillips, M.D. 343-345
PBLD OB L081 Critical Management of a Parturient With
Inuenza Progressing to ARDS
Vernon Ross, M.D. 343-345
PBLD RA L082 Analgesic Options for a 68-Year-Old Man
with Multiple Rib Fractures
Mark Leibel, M.D.
Kristopher Schroeder, M.D.
343-345
PBLD CA L083 Hold My Compass: Tools and Tips So That
YOU Don’t Get Lost in the EP Lab
Mark Weiss, M.D. 343-345
PBLD CC L084 Management of Acute Pulmonary
Embolism: Anticipating and Responding to
Complexity
Ahmed Zaky, M.D. 343-345
12:30-2:30 p.m. 120-Minute
Panel
PI PN09 Patients Do the Darndest Things: Tales
From the Anesthesia Incident Reporting
System
Richard Dutton, M.D., M.B.A. 211-213
1-2:30 p.m. 90-Minute Panel FA PN102 Perioperative Management of Patients
With Endocrine Disease: A Global
Perspective
Karen Domino, M.D., M.P.H. 255-257
Clinical Forum AM CF06 Ambulatory Non-Operating Room
Anesthesia (NORA): It Ain’t That Simple
Thomas Cutter, M.D. 206-207
Point-
Counterpoint
CC PC09 A Structured Handoff Protocol Improves
the Care of Patients Going to the ICU
After Surgery
Steven Greenberg, M.D. 203-205
MCCS MCC07 Medically Challenging Case Presentations Hall B1
Poster
Discussions
FA PD08-2 Equipment, Monitoring and Engineering Technology: Enhancing Patient
Safety and Environmentally Sound Practices
243
Poster
Discussions
CA PD09-1 Experimental Circulation 245
Poster
Discussions
PI PD11-1 History and Education:Pioneers of Anesthesia 244
1-3 p.m. 120-Minute
Panel
CC PN10 Minimizing Postoperative ICU
Complications in a Surgical Home
Trung Vu, M.D. 217-219
120-Minute
Panel
FA PN11 Intravenous Anesthesia Beyond Propofol Keira Mason, M.D. 220-222
120-Minute
Panel
OB PN12 Perioperative Considerations for Ex
Utero Intrapartum Treatment Procedures:
Principles, Pitfalls and Progress
Mark Rollins, M.D., Ph.D. 225-227
120-Minute
Panel
PD PN13 They Walk Among Us: Anesthesia for
Adults With Pediatric Disease
Debra Morrison, M.D. 228-230
120-Minute
Panel
RA PN14 Controversies and Challenges in
Perioperative Pain Management
Eugene Viscusi, M.D. 252-254
Poster
Presentations
PN PO03-1 Chronic and Cancer Pain Hall B1-Area
B
Poster
Presentations
NA PO05-1 Clinical Neurosciences Hall B1-Area
E
Poster
Presentations
PI PO11-2 History and Education:Evaluation: Strategies and Resources Hall B1-Area
D
Poster
Presentations
FA PO13-5 Outcomes and Database Research Hall B1-Area
A
1-4 p.m. Seminar PN 816 Physical Exam Workshop for Pain
Physicians
Brian Starr, M.D. 346-347
Hands-on
Workshop
FA 817 Awake Fiberoptic Intubation: A
Streamlined Approach With Nerve Blocks
Scott Miller, M.D. 348-349
Hands-on
Workshop
PD 823 Perioperative Pediatric Advanced Life
Support Simulation
Scott Watkins, M.D. 281
1-5 p.m. Cadaver
Workshops
PN CA05 Radiofrequency Ablation of the Spine,
Sacrum and Lumbar Disc
Maxim Eckmann, M.D. 275-277
EDUCATION

31
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Hands-on
Workshop
PN 814 Ultrasound Guided Musculoskeletal
Injections - Live Models: Beyond
Corticosteroids
James Modir, M.D. 271-273
1:30-2:45 p.m. Hands-on
Workshop
FA AW09 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
1:45-2:45 p.m. RCL FA 223 Perioperative Management of Pulmonary
Hypertension
Ronald Pearl, M.D., Ph.D. RiverGate
RCL FA 224 Obstructive Sleep Apnea - What an
Anesthesiologist Should Know
Frances Chung, M.B.B.S.
F.R.C.P.C.
E-1
RCL OB 225 State of the Art Labor Analgesia Kenneth Nelson, M.D. E-2
RCL CC 226 Heart Failure and Perioperative Care Gareth Ackland, M.D. E-3
RCL AM 227 Effective Management of Pain, PONV and
Common Adverse Effects in Ambulatory
Surgical Patients
Tong Gan, M.D. 260-262
RCL PI 228 Building a Quality Management System
for Meaningful Use
John Allyn, M.D. La Nouvelle
Ballroom AB
2-5 p.m. Residents
and Medical
Students
FA RM12 FAER Medical Student Anesthesia
Research Fellowship Symposium
Paloma Toledo, M.D., M.P.H. R08-09
2:30-5 p.m. Residents
and Medical
Students
FA RM13 Resident Regional Anesthesia Workshop Julia Pollock, M.D. R06-07
Hands-on
Workshop
FA DW06 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil, M.D. 353-355
3-4 p.m. RCL NA 229 The Impact of Anesthesia on the Young
and Old Brain
Audree Bendo, M.D. RiverGate
RCL CC 230 Perioperative Coagulation and
Coagulopathy
Linda Liu, M.D. E-1
RCL FA 231 Neuromuscular Management and Patient
Outcomes
Glenn Murphy, M.D. E-2
RCL RA 232 The Economics of Regional Anesthesia Brian Williams, M.D., M.B.A. E-3
RCL CA 233 New Developments in Thoracic
Anesthesia
Edmond Cohen, M.D. 260-262
RCL OB 234 Anesthesia for Nonobstetric Surgery and
Procedures
Yaakov Beilin, M.D. La Nouvelle
Ballroom AB
3-4:15 p.m.
Hands-on
Workshop
FA AW10 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel, D.O.,
William Simmons, M.D.
356-357
3-4:30 p.m. Clinical Forum FA CF07 A 65-Year-Old Male; Preoperative
Evaluation and Management of CAD for
Robotic Prostate Surgery
Paul Kempen, M.D., Ph.D. 206-207
MCCS MCC08 Medically Challenging Case Presentations Hall B1
Oral
Presentations
AM OR01-2 Ambulatory Anesthesia: Ambulatory Anesthesia Practice and Outcomes 245
Oral
Presentations
FA OR07-2 Drug Disposition, Metabolism and Elimination 243
3-5 p.m. 120-Minute
Panel
FA PN15 Fluid Administration in the Operating
Room: An Update Focusing on Recent
Literature
Andrew Leibowitz, M.D. 203-205
120-Minute
Panel
RA PN16 Transversus Abdominis Plane Block
Paravertebral Block or Thoracic Epidural:
Is There an Ideal Truncal Block?
Steven Clendenen, M.D. 211-213
Oral
Presentations
FA OR17-2 Respiration-Respiration-Respiration-Basic Mechanisms, Animal Models and
Clinical Science
244
3:30-4:45 p.m. PBLD PI L059 When the Patient Just Says No Sarah Smith, M.D. 343-345
PBLD PI L085 A High Risk Patient for Low Risk
Outpatient Surgery: Is There Value in a
Surgical Home for a Patient Going Home?
Jeanna Blitz, M.D. 343-345
PBLD NA L086 Only a Little Sniff of Cocaine; Now an
Aneurysm Coiling Headache!
Jess Brallier, M.D. 343-345
SCHEDULE BY DAY: SUNDAY

32
PBLD CC L087 Transfusion Goals and Hemostatic
Management of the Anticoagulated
Trauma Patient: Can You Plug a Hole in
the Dam?
Louanne Carabini, M.D. 343-345
PBLD RA L088 This Epidural Catheter Is Not Working
Well. What Should I Do?
Miguel Cruz, M.D. 343-345
PBLD CC L089 Elderly Man; Going into Shock; Needs
Fluids Now!
Elizabeth Frost, M.B., Ch.B. 343-345
PBLD AM L090 It’s Just a Quick EGD in the Ofce...but
Can I Safely Anesthetize My Patient Here?
Jeena Jacob, M.D. 343-345
PBLD PD L091 Why Does My Patient Scheduled for
Endoscopic Sinus Surgery Have Severe
Groin Pain?
Kirk Lalwani, M.D.
Christine Martin, M.D.
343-345
PBLD RA L092 Thoracic Epidural Analgesia in the
Recently Anticoagulated Patient: Is This a
Good Idea?
Anuj Malhotra, M.D. 343-345
PBLD PN L093 Worsening Back Pain: To Inject or Not to
Inject That Is the Question
Tariq Malik, M.D. 343-345
PBLD OB L094 Anesthetic Considerations for the
Jehovah’s Witness Patient Undergoing
Trial of Labor After Cesarean Delivery
(TOLAC)
Chawla LaToya Mason, M.D. 343-345
PBLD OB L095 Placenta Percreta: Preparation and
Management
Cathleen Peterson-Layne,
Ph.D., M.D.
343-345
PBLD PD L096 Tonsillectomy and Adenoidectomy in a
Child With Down Syndrome More to It
Than You Think!
Catherine Seipel, M.D. 343-345
3:30-5 p.m. 90-Minute Panel AM PN60 Crisis Management in Ofce-Based
Anesthesia
Michael Walsh, M.D. 208-210
90-Minute Panel CA PN61 Cerebral Oximetry Monitoring: Does It
Affect Neurologic Outcome?
John Murkin, M.D. 217-219
90-Minute Panel CC PN62 ACLs for the Anesthesiologist: An Update Vivek Moitra, M.D. 220-222
90-Minute Panel AM PN63 Ambulatory Surgery Airway Challenges Raafat Hannallah, M.D. 225-227
90-Minute Panel PI PN64 Limits of Care: Ethical Issues in the
Current Technological Environment
Paul Barash, M.D. 228-230
90-Minute Panel FA PN65 Optimization of the High-Risk Surgery
Patient in the Era of Enhanced Recovery
After Surgery and Perioperative Surgical
Home
Maxime Cannesson, M.D.,
Ph.D.
255-257
3:30-5:30 p.m. 120-Minute
Panel
FA PN17 Preoperative Assessment and
Management
David Hepner, M.D. 252-254
4-4:30 p.m. Featured Lecture
SPE09 ABA Informational Session: Assessment
Programs for Primary Certication in
Anesthesiology
Deborah Culley, M.D. 335-336
4:15-5:15 p.m. RCL PN 235 Cancer Pain Management in 2014 Oscar A. De Leon-Casasola,
M.D.
RiverGate
RCL RA 236 Ultrasound Guided Regional Anesthesia
in Infants, Children and Adolescents:
Guiding You to Success
Santhanam Suresh, M.D. E-1
RCL PI 237 Mythbusters Episode: Economic Issues of
Anesthesia Care
Amr Abouleish, M.D., M.B.A. E-2
RCL FA 238 Weapons of Mass Destruction: Improvised
Explosive Devices
Michael Murray, M.D., Ph.D. E-3
RCL CC 239 Understanding Clinical Hemodynamics Jeffery Vender, M.D., F.C.C.M. 260-262
RCL FA 240 What’s New in Airway Management Lauren Berkow, M.D. La Nouvelle
Ballroom AB
4:30-5 p.m. Featured Lecture SPE10 ABA Informational Session: Maintenance
of Certication in Anesthesiology Program
(MOCA)
Deborah Culley, M.D. 335-336
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain

33
33
SCHEDULE BY DAY: SUNDAY
NOTES

34
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
MONDAY, OCT. 13
Time Session Type Track Fee Code Title Speaker Location
7 a.m.-5 p.m. Registration Lobby A & D
7 a.m.-5 p.m. ASA Resource Center (Connection Center) Convention Center, Hall B-1
7 a.m.-5 p.m. International Connection Lounge Lobby A
7-8:15 a.m. Subspecialty
Panels
NA 606 (SNACC) Anesthesia for Acute Stroke
Management: Method, Timing and
Hemodynamics
Ra Avitsian, M.D. 231-232
Subspecialty
Panels
PI 607 (SEA) Technology Today: Testing, Training
and Learning
Ira Todd Cohen, M.D., M.Ed. 238-239
Subspecialty
Panels
RA 608 (ASRA) In-Hospital Falls: What Causes
Them and How Can We Prevent Them?
Sandra Kopp, M.D. 243
7:15-8:30 a.m. PBLD FA L097 Help - My Patient Is on a Multi-
Chemotherapeutic Regiment and Is
Coming for a Laparotomy! What Do I Need
to Know?
Anoushka Afonso, M.D. 343-345
PBLD CA L098 Carotid Endarterectomy: Asleep Versus
Awake
Jeffrey Dobyns, D.O. 343-345
PBLD PI L100 Giving Feedback: How to Support the
Defensive Learner
Yulia Ivashkov, M.D. 343-345
PBLD NA L101 My Ulnar Neuropathy Has Resolved. Now I
Have to Go for Spine Surgery in the Prone
Surrender Position
Ihab Kamel, M.D. 343-345
PBLD FA L102 Malignant Hyperthermia in a Child Having
a Tethered Cord Release
Tae Kim, M.D. 343-345
PBLD OB L104 She was Advised Not to Get Pregnant and
She Did: Pulmonary Hypertension and
Pregnancy
Tanya Lucas, M.D. 343-345
PBLD AM L105 PONV, PDNV and Long QT Syndrome:
Balancing Risk and Benet
Anuj Malhotra, M.D. 343-345
PBLD PD L106 A Child With Mitochondrial Disease and
Propofol Allergy Who May be Susceptible
to Malignant Hyperthermia
Jayant Pratap, M.B., B.Ch. 343-345
PBLD RA L107 A 40-Year-Old Woman With Multiple
Sclerosis Consulting for Postoperative
Epidural Following Laparoscopic
Converted to Open Colectomy
John Shepler, M.D.
Kristopher Schroeder, M.D.
343-345
PBLD FA L108 Airway Management of a Patient With
Penetrating Neck Injury
Albert Varon, M.D. 343-345
PBLD CC L109 Management of Acute Pulmonary
Embolism:Anticipating and Responding to
Complexity
Ahmed Zaky, M.D. 343-345
PBLD NA L133 Awake Craniotomy in a Patient With
Obstructive Sleep Apnea
Karl Willmann, M.D. 343-345
PBLD PD L140 When It Rains It Pours; Large AVM Heart
Failure Pulmonary HTN and Now There Is
V-tach!
Christina Diaz, M.D. 343-345
8-9 a.m. RCL FA 301 Positioning Problems You Hope to Never
Encounter
Mark Warner, M.D. RiverGate
RCL PN 302 Therapeutic Epidural Injections: Safety
Considerations and Evidence Basis
Marc Huntoon, M.D. E-1
RCL RA 303 Current Concepts and Controversies in
Acute Pain Management
Eugene Viscusi, M.D. E-2
RCL PI 304 Tired of Not Being Taken Seriously? How
Professionalism Affects You
Saundra Curry, M.D. E-3
RCL CA 305 Synthetic Colloids in Cardiac Surgery
What Are the Indications?
Roman Sniecinski, M.D. 260-262
8-9:30 a.m. 90-Minute Panel OB PN66 Basic Considerations for the Occasional
Obstetric Anesthesiologist
Yaakov (Jake) Beilin, M.D. 208-210
Clinical Forum RA CF08 EXPAREL: A Novel Liposomal Extended-
Release Bupivacaine Formulation
John Rowlingson, M.D. 203-205
EDUCATION

35
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Clinical Forum CC CF09 Critical Care Forum: Challenges
and Controversies in Critical Care
Anesthesiology
Avery Tung, M.D., F.C.C.M. 206-207
Point-
Counterpoint
CC PC10 Should We Perform CPR When We Know
That It Is Futile?
Neal Cohen, M.D., M.P.H.,
M.S.
211-213
MCCS MCC09 Medically Challenging Case Presentations Hall B1
Oral
Presentations
AM OR01-1 Ambulatory Anesthesia: Anesthesia Outcomes, Delirium and Cognitive
Dysfunction
243
Oral
Presentations
FA OR13-3 Outcomes and Database Research 245
Poster
Discussions
PD PD15-2 Pediatric Anesthesia: Miscellaneous 244
8-10 a.m. 120-Minute
Panel
CC PN18 Perioperative Hemodynamic Optimization
and Goal Directed Therapy
Jeffery Vender, M.D., F.C.C.M. 217-219
120-Minute
Panel
FA PN19 ACUTE Care Anesthesiology: Strategies
for the Management of Trauma,
Emergencies and Disasters
Maureen McCunn, M.D., MIPP 220-222
120-Minute
Panel
OB PN20 Maternal Mortality in the Developed
World: What Should the Anesthesiologist
Know?
Robert D’Angelo, M.D. 225-227
120-Minute
Panel
FA PN21 Neuromuscular Blockade and Reversal Francois Donati, M.D., Ph.D. 228-230
120-Minute
Panel
PN PN22 Palliative Care and the Anesthesiologist Mihir KaM.D.ar, M.D. 252-254
120-Minute
Panel
PI PN23 Embracing Quality Improvement: Key
Steps You Can Take Today to Improve
Yourself Your Department and Your
Hospital
David Zvara, M.D. 255-257
RCL NA 306 Perioperative Management of Patients
Undergoing Spine Surgery
Susan Black, M.D. La Nouvelle
Ballroom AB
Featured Lecture SPE11 Best of Abstracts: Basic Science James Rathmell, M.D. 265-268
Featured Lecture FA SPE12 FAER Academy of Research Mentors Evan Kharasch, M.D., Ph.D. 342
Featured Lecture FA SPE13 International Forum on Patient Safety and
Quality Outcomes
Richard Dutton, M.D., M.B.A. Great Hall B
Poster
Presentations
PN PO03-3 Chronic and Cancer Pain Hall B1-Area
B
Poster
Presentations
FA PO08-2 Equipment, Monitoring and Engineering Technology: Coagulation,
Hemoglobin, and Glucose
Hall B1-Area
C
Poster
Presentations
NA PO10-3 Experimental Neurosciences: Cerebral Blood Flow and CNS Ischemia Hall B1-Area
E
Poster
Presentations
PI PO11-3 History and Education: How Far We Have Come Hall B1-Area
D
Poster
Presentations
PI PO14-5 Patient Safety and Practice Management Hall B1-Area
A
8-11 a.m. Hands-on
Workshop
AM 820 Ophthalmic Regional Anesthesia Marc Feldman, M.D., MHS 333-334
Seminar FA 821 Grant Writing and the NIH Study Section
for the Uninitiated
Michael Andreae, M.D. 348
Hands-on
Workshop
CA 822 Intermediate Transesophageal
Echocardiography (TEE)
James Abernathy, III, M.D.,
M.P.H.
338-339
Hands-on
Workshop
CC 825 Critical Care Ultrasonography for the
Perioperative Physician
Steven Venticinque, M.D. 356-357
Hands-on
Workshop
FA 824A Difcult Airway Workshop With Simulation Allan Reed, M.D. 353-355
8-11:30 a.m. Hands-on
Workshop
CC 819A Perioperative ACLS Simulation Workshop Matthew McEvoy, M.D. 281
9-10:15 a.m. PBLD FA L110 Trauma Induced Coagulopathy Maged Andrews, M.Sc., M.B.,
B.Ch.
343-345
PBLD NA L111 Crisis in the Neuro-Muscular Junction.
Anesthetic Implications
Cristina Barboi, M.D. 343-345
SCHEDULE BY DAY: MONDAY

36
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
PBLD AM L112 Is Ambulatory Shoulder Surgery Safe in a
Patient With Obstructive Sleep Apnea?
Christopher Canlas, M.D. 343-345
PBLD RA L113 This Epidural Catheter Is Not Working
Well. What Should I Do?
Miguel Cruz, M.D. 343-345
PBLD RA L114 Numb and Number: Should We Use
Regional Anesthesia in Orthopedic
Trauma?
Nabil Elkassabany, M.D. 343-345
PBLD PN L115 Opioid-Induced Hyperalgesia, Tolerance
and Chronic Postsurgical Pain; a
Dilemma Complicating Postoperative Pain
Management
Dalia Elmofty, M.D. 343-345
PBLD CC L117 Management of Severe ARDS in the ICU
With ECMO
Jacob Gutsche, M.D. 343-345
PBLD FA L118 A Patient With End-Stage Liver Disease for
Elective Surgery
Christopher Darling, D.O.
Michael Hannaman, M.D.
343-345
PBLD PI L119 My Patient With a DNR Order Arrested in
the OR! Now What?!
Juliann Hobbs, M.D., M.P.H. 343-345
PBLD PI L120 When the Patient Just Says No Sarah Smith, M.D. 343-345
PBLD PD L121 It Is Just a Nosebleed Isn’t It? Anesthetic
Considerations for Unsuspected
Pulmonary Hypertension
Shu-Ming Wang, M.D. 343-345
PBLD FA L122 Oh No! Both Arteries in My Neck Are
Blocked! Now What?
Stanlies D’Souza, M.D.,
F.R.C.A
343-345
9-11 a.m. Seminar PN 818 Practical Pain Medicine Coding:
Compliance and Workow Strategies for
2014
Kevin Vorenkamp, M.D. 276-277
9 a.m.-3 p.m. Scientic and Educational Exhibits (Connection Center) Hall C
Exhibits (Connection Center) Hall B2-D
Afliated Subspecialty Society Pavilion (Connection Center) Booth #111
9:15-10:15 a.m. RCL PI 307 Ethics in the Real World Jeffrey Jacobs, M.D. RiverGate
RCL PN 308 The Strain in Pain Lies Mainly in the
Brain: Lessons Learned from the
Neuroimaging of Pain
Sean Mackey, M.D., Ph.D. E-1
RCL FA 309 A Few New Papers From Outside
Anesthesia Which Can Affect Your Pactice
James Eisenach, M.D. E-2
RCL CA 310 Cerebral Protection During Cardiac
Surgery
Charles Hogue, M.D. E-3
RCL RA 311 Clinical Pathways for Total Joint
Arthroplasty: Essential Components for
Success
James Hebl, M.D. 260-262
10 a.m.-12 p.m. Poster
Presentations
AM PO01-2 Ambulatory Anesthesia: Sedation, Pharmacokinetics and Recovery
Outcomes
Hall B1-Area
E
Poster
Presentations
FA PO13-2 Outcomes and Database Research Hall B1-Area
B
Poster
Presentations
PI PO14-3 Patient Safety and Practice Management Hall B1-Area
C
Poster
Presentations
PD PO15-3 Pediatric Anesthesia Hall B1-Area
D
Poster
Presentations
FA PO17-1 Respiration-Clinical and Basic Science Hall B1-Area
A
10:20-11:35
a.m.
Featured Lecture SPE14 Rovenstine Lecture: Health Care at the
Crossroads: The Imperative for Change
Karen Domino, M.D., M.P.H. Great Hall
AD
10:30-12 p.m. MCCS MCC10 Medically Challenging Case Presentations Hall B1
11:45 a.m.-1:15
p.m.
Featured Lecture SPE15 Celebration of Research James Eisenach, M.D. Great Hall B
12:30-1:30 p.m. RCL PI 312 Chemical Dependency and Anesthesiology John Tetzlaff, M.D. RiverGate
RCL CC 313 (A)ACLS in the Perioperative Period Gerald Maccioli, M.D. E-1
RCL FA 314 Perioperative Glycemic Management: A
Practical Guide
Basem Abdelmalak, M.D. E-2
EDUCATION

37
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
RCL CA 315 Preconditioning the Heart: How It Works
and Does It Matter?
Judy Kersten, M.D. E-3
RCL RA 316 Lipid Resuscitation for Local Anesthetic
and Other Toxic Overdoses
Guy Weinberg, M.D. 260-262
RCL PN 317 Improving Safety Through Use of
Diagnostic Imaging and Image Guidance
in Pain Medicine
James Rathmell, M.D. La Nouvelle
Ballroom AB
PBLD PI L103 How to Create and Moderate a Great
Problem Based Learning Discussion
(PBLD)
Kirk Lalwani, M.D. 343-345
12:30-1:45 p.m. PBLD PD L123 Cardiovascular Collapse During
Thoracoscopic Tracheoesophageal Fistula
Repair
Kimberly Blasius, M.D. 343-345
PBLD PI L124 Do You Want to Present a PBLD at the
2015 ASA Meeting? This PBLD Session
Could Help You
Sanjay Bhananker, M.B., B.S. 343-345
PBLD FA L125 Can the Adult Patient With Morbid Obesity
and Obstructive Sleep Apnea Safely
Undergo Outpatient Surgery?
Kenneth Hiller, M.D. 343-345
PBLD PI L126 How Not to End Up on the Nightly News:
Safe Injection Practices
Vilma Joseph, M.D. 343-345
PBLD FA L127 The Unanticipated Difcult Airway: A
Dynamic and Dangerous Scenario
Lavinia Kolarczyk, M.D. 343-345
PBLD OB L128 A Parturient With Scoliosis and Harrington
Rods
Allison Lee, M.D. 343-345
PBLD OB L129 Anesthetic Considerations for the
Jehovah’s Witness Patient Undergoing
Trial of Labor After Cesarean Delivery
(TOLAC)
Chawla LaToya Mason, M.D. 343-345
PBLD FA L130 I Swear It Will Only Take 15 Minutes:
Anesthesia/Sedation for TEE/
Cardioversion
Julia Metzner, M.D. 343-345
PBLD FA L131 Blood IS Thicker Than Water: Anesthetic
Concerns of Hypercoagulability
Gregory Rose, M.D. 343-345
PBLD AM L132 A Slip and Fall in the Post Warfarin Era Mercy Udoji, M.D. 343-345
PBLD PI L134 Anesthesiologists and Terminal Live Organ
Donation: You Want Me to Do What?
Richard Wolman, M.D., M.A. 343-345
PBLD PD L135 Using Advanced Trauma Life Support to
Manage a Pediatric Trauma Patient With
Traumatic Brain Injury and Disclosure of
Difcult News After a Poor Outcome
David Young, M.D., M.Ed 343-345
12:30-2:30 p.m. 120-Minute
Panel
PI PN24 Milestones: Setting a High Bar or Barely
Clearing the Hurdle?
Randall Schell, M.D., M.Ed. 203-205
1-2:30 p.m. 90-Minute Panel
CA PN67 Understanding the Role of Anemia
on Patient Outcomes: An Innocent
Bystander?
Colleen Koch, M.D., M.S.,
M.B.A.
208-210
90-Minute Panel CC PN68 Quality Improvement in Critical Care Gregory Botz, M.D. 217-219
90-Minute Panel PN PN69 Management of Chronic Pain: A Review of
Treatment Modalities
Magdalena Anitescu, M.D. 220-222
90-Minute Panel NA PN70 Life-Death Transition George Mashour, M.D., Ph.D. 225-227
90-Minute Panel PD PN71 TIVA for TOTS Zulqar Ahmed, M.D., F.A.A.P. 228-230
90-Minute Panel FA PN72 Morbid and Ultra Obesity: Growing
Challenge in Anesthesiology
Ashish Sinha, M.D., Ph.D. 252-254
90-Minute Panel FA PN73 How Do We Decide When Not to Operate?
Facing Challenges in Surgical Decision-
Making for Older Adults
Mark Neuman, M.D., M.Sc. 255-257
Clinical Forum PD CF10 Anesthetic Safety in Newborns Can Be
Achieved by Sticking to Little Details
Susan Verghese, M.D. 206-207
Point-
Counterpoint
FA PC11 Computer-Assisted Personalized Sedation
(CAPS) - Is the Coming Technology of
CAPS a Friend or Foe?
Walter Maurer, M.D. 211-213
SCHEDULE BY DAY: MONDAY

38
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
MCCS MCC11 Medically Challenging Case Presentations Hall B1
Oral
Presentations
FA OR02-1 Anesthetic Action and Biochemistry: Off Target Effects of Anesthetics to
Improve Patient Safety
231-232
Oral
Presentations
NA OR10-2 Experimental Neurosciences 238-239
Oral
Presentations
PI OR11-2 History and Education: How Do Know What We Teach 245
Oral
Presentations
PI OR14-3 Patient Safety and Practice Management 243
Poster
Discussions
PN PD03-2 Chronic and Cancer Pain 244
1-3 p.m. Poster
Presentations
CA PO04-3 Clinical Circulation: Physiology/Pharmacology Hall B1-Area
E
Poster
Presentations
CC PO06-2 Critical Care Hall B1-Area
D
Poster
Presentations
FA PO07-1 Drug Disposition, Metabolism and Elimination Hall B1-Area
A
Poster
Presentations
CA PO09-1 Experimental Circulation Hall B1-Area
C
Poster
Presentations
RA PO16-3 Regional Anesthesia and Acute Pain: Basic sciences Hall B1-Area
B
1-4 p.m. Hands-on
Workshop
FA 826 Wire-Guided Airway Management Richard Galgon, M.D. 333-334
Hands-on
Workshop
CA 827 Advanced TEE Workshop Sajid Shahul, M.D., M.P.H. 338-339
Seminar PI 829 Physician Performance Assessment and
Improvement: Practice Its Power for Your
Own Practice
Leslie Jameson, M.D. 356-357
Hands-on
Workshop
FA 824B Difcult Airway Workshop With Simulation Allan Reed, M.D. 353-355
Hands-on
Workshop
RA 828A Peripheral Nerve Blocks: Ultrasound,
Simulation and Stimulation
Andrew Rosenberg, M.D. 352
1-4:30 p.m. Hands-on
Workshop
CC 819B Perioperative ACLS Simulation Workshop Matthew McEvoy, M.D. 281
1-5 p.m. Cadaver
Workshops
RA CA06 Comprehensive Anatomy-Live Model
Ultrasound for Regional Anesthesia
Carlo Franco, M.D. 271-273
1:45-2:45 p.m. RCL FA 318 How to Establish a Perioperative Surgical
Home in Your Institution
Zeev Kain, M.D., M.B.A. RiverGate
RCL PN 319 Interventional Pain Procedures in Patients
on Anticoagulants
Honorio BenzonM. D. E-1
RCL AM 320 Malignant Hyperthermia in the Ambulatory
Setting
Ronald Litman, D.O. E-2
RCL FA 321 My Pharmacy Is Out of Fentanyl, What Do
I Do Now? Rational Perioperative Opioid
Substitutions
Dhanesh Gupta, M.D. E-3
RCL RA 322 Lower Extremity Nerve Blocks: Update Admir Hadzic, M.D., Ph.D. 260-262
RCL CC 323 Controversies and Best Practices in
Central Line Insertion
Avery Tung, M.D., F.C.C.M. La Nouvelle
Ballroom AB
2-3 p.m. Featured Lecture FA SPE16 FAER Honorary Research Lecture: The
Clinical Neuroscience of Anesthesia:
Research Education and Patient Care
Emery Brown, M.D., Ph.D. Great Hall B
2-4 p.m. Featured Lecture FA SPE17 Patrick Sim Forum: An Afternoon With
the WLM Laureates of the History of
Anesthesia
David Waisel, M.D. 265-268
3-4 p.m. RCL PN 324 Algorithmic Approach to Back Pain Nagy Mekhail, M.D., Ph.D. RiverGate
RCL AM 325 Ultrasound Guided Regional Anesthesia
for Ambulatory Surgery
Meg Rosenblatt, M.D. E-1
RCL RA 326 Multimodal Analgesics for Perioperative
Pain Control
May Chin, M.D. E-2
EDUCATION

39
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
RCL FA 327 Top 10 Respiratory Anesthesia Practices
That Drive Me Crazy
David Warner, M.D. E-3
RCL PD 328 Airway Management in Pediatric
Emergencies: The Tricks of the Trade
Paul Reynolds, M.D. 260-262
RCL FA 329 Hazards of the Anesthesia Workstation James Eisenkraft, M.D. La Nouvelle
Ballroom AB
3-4:30 p.m. Clinical Forum PI CF11 What Should You Do When You Don’t
Think the Patient Should Have Surgery
at All?
Nancy Glass, M.D., M.B.A. 206-207
Point-
Counterpoint
PN PC12 Should We Discontinue the Use of
Opioids for the Treatment of Chronic Pain?
Rafael Miguel, M.D.,
Oscar De Leon Casasola,
M.D.
203-205
Point-
Counterpoint
CA PC13 Current Controversies in Cardiac
Anesthesia
Gregory Janelle, M.D., F.A.S.E. 211-213
MCCS MCC12 Medically Challenging Case Presentations Hall B1
Oral
Presentations
FA OR07-1 Drug Disposition, Metabolism and Elimination 245
Oral
Presentations
NA OR10-1 Experimental Neurosciences: Mechanisms 243
Oral
Presentations
RA OR16-1 Regional Anesthesia and Acute Pain 231-232
3-5 p.m. Featured Lecture FA SPE18 FAER Panel: Future of Anesthesiology
Research
Zeljko Bosnjak, Ph.D. Great Hall B
3:30-4:45 p.m. PBLD CA L136 Descending Thoracic Aortic Repair - Spinal
Cord Protection Strategies
Harendra Arora, M.D. 343-345
PBLD NA L137 An Acute Ischemic Stroke Coming to Your
Neuroangiography Suite
Ra Avitsian, M.D. 343-345
PBLD PI L138 Infection Prevention for the Anesthesia
Professional: What is the Least I Should
Know and How Do I Apply It to My
Practice?
Richard Beers, M.D. 343-345
PBLD PI L139 Creating a Culture of Professionalism in
Your Department
Saundra Curry, M.D. 343-345
PBLD CC L141 Management of Co-Intoxications in the
ICU Patient
Robert Gould, M.D. 343-345
PBLD AM L142 Perioperative Anesthetic Issues for
Ambulatory Surgery
Dean Jones, M.D. 343-345
PBLD RA L143 Tough Choices: Regional or General
Anesthesia in a Very Elderly Patient
Jason Lane, M.D., M.P.H. 343-345
PBLD PI L144
He’s 15 Needs This Operation and He’s
DNR!
David Mann, M.D. 343-345
PBLD NA L145 Deep Brain Stimulation for Parkinson’s
Disease: What Is the Role of the
Anesthesiologist?
Julia Metzner, M.D. 343-345
PBLD FA L146 Cardiopulmonary Collapse During
Laparoscopic Nissen Fundoplication
Govind Rajan, M.B., B.S. 343-345
PBLD OB L147 Critical Management of a Parturient With
Inuenza Progressing to ARDS
Vernon Ross, M.D. 343-345
PBLD OB L148 A Parturient Presenting in Premature
Labor With Single-Ventricle Physiology
Complicated by Breech Presentation and
Paroxysmal Supraventricular Tachycardia:
What’s Your Labor Management Plan?
Manuel Vallejo, M.D., D.M.D. 343-345
PBLD OB L187 Neurologic Complications Following
Epidural Placement - How to Differentiate
and Manage?
Kelly Elterman, M.D.
David Hepner, M.D.
343-345
3:30-5 p.m. 90-Minute Panel AM PN74 Non-Operating Room Anesthesia:
Techniques
Basavana Goudra, M.D.,
F.R.C.A., FCARCSI
208-210
90-Minute Panel CA PN75 Guidelines for Blood Management - What
Do They Tell Us?
C. Mazer, M.D. 217-219
SCHEDULE BY DAY: MONDAY

40
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
90-Minute Panel CC PN76 Optimizing Perioperative Pulmonary
Function
Steven Lisco, M.D. 220-222
90-Minute Panel OB PN77 What Are They Doing and Why? Obstetrics
for the Anesthesiologist
Barbara Scavone, M.D. 225-227
90-Minute Panel RA PN78 Regional Anesthesia for Total Shoulder
Arthoplasty: Outcomes, Complications,
Techniques, and Use in Ambulatory
Surgery
Maxim Eckmann, M.D. 228-230
90-Minute Panel PI PN79 Physician Impairment: Incidence
Identication and Intervention
Keith Berge, M.D. 252-254
90-Minute Panel RA PN80 Regional Anesthesia Dilemmas Due to
Medical Disease
Steven Clendenen, M.D. 255-257
4:15-5:15 p.m. RCL CC 330 Perioperative Delirium Pratik Pandharipande, M.D. RiverGate
RCL FA 331 Obesity and Anesthesia: Crossroads of a
Challenge
Ashish Sinha, M.D., Ph.D. E-1
RCL PI 332 Advanced Teaching Skills for the Fast-
Paced OR: How to Successfully Educate
When Faced With High Clinical Workload,
Lack of Protected Time, and Limited
Funding?
Marek Brzezinski, M.D., Ph.D. E-2
RCL CA 334 Heparin Sensitivity and Resistance:
Management During Cardiopulmonary
Bypass
Alan Finley, M.D. 260-262
RCL PI 335 The Art and Science of Disclosing
Unanticipated Outcomes to Patients: An
Anesthesiologist’s Perspective
Allen Gustin, M.D. La Nouvelle
Ballroom AB
5-6 p.m. Featured Lecture PI SPE19 How Can FAER’s New Education
Mentorship Academy Help Anesthesiology
Educators
Catherine Kuhn, M.D. Great Hall B
EDUCATION
41
Claim your
CME credit
online!
Earn a chance
to win an iPad
®
Claim your CME credit and access session
evaluations via the following 3 options:
1. ANESTHESIOLOGY
™
2014 Online Community
2. asahq.org/evals
3. Scan the QR code

42
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
EDUCATION
TUESDAY, OCT. 14
Time Session Type Track Fee Code Title Speaker Location
7 a.m.-5 p.m. Registration Lobby A & D
7 a.m.-5 p.m. ASA Resource Center (Connection Center) Convention Center, Hall B-1
7 a.m.-5 p.m. International Connection Lounge Lobby A
7-8:15 a.m. Subspecialty
Panels
CA 609 (SCA) Cardiac Anesthesia Colleen Koch, M.D., M.S.,
M.B.A.
231-232
Subspecialty
Panels
PD 610 (SPA) The Child With Congenital Heart
Disease Presenting for Non-Cardiac
Surgery
Shobha Malviya, M.D. 238-239
7:15-8:30 a.m. PBLD FA L149 Trauma Induced Coagulopathy Maged Andrews, M.Sc., M.B.
B.Ch.
343-345
PBLD NA L150 An Acute Ischemic Stroke Coming to Your
Neuroangiography Suite
Ra Avitsian, M.D. 343-345
PBLD RA L151 Postoperative Ulnar Neuropathy - Could I
Have Done Something to Prevent It?
Sanjay Bhananker, M.B., B.S. 343-345
PBLD CC L152 Transfusion Goals and Hemostatic
Management of the Anticoagulated
Trauma Patient: Can You Plug a Hole in
the Dam?
Louanne Carabini, M.D. 343-345
PBLD FA L153 Oh No! Both Arteries in My Neck Are
Blocked! Now What?
Stanlies D’Souza, M.D.,
F.R.C.A
343-345
PBLD CC L154 Management of Co-Intoxications in the
ICU Patient
Robert Gould, M.D. 343-345
PBLD PI L155 My Patient With a DNR Order Arrested in
the OR! Now What?!
Juliann Hobbs, M.D., M.P.H. 343-345
PBLD AM L156 It’s Just a Quick EGD in the Ofce...but
Can I Safely Anesthetize My Patient Here?
Jeena Jacob, M.D. 343-345
PBLD OB L158 A Parturient With Scoliosis and Harrington
Rods
Allison Lee, M.D. 343-345
PBLD FA L159 My Patients Never Have Residual
Paralysis in the PACU, or Do They?
Stephan Thilen, M.D., M.S. 343-345
PBLD NA L160 Awake Craniotomy in a Patient With
Obstructive Sleep Apnea
Karl Willmann, M.D. 343-345
8-9 a.m. RCL PI 401 Compensation for Service - When the
Revenues Don’t Support the Expectations
Asa Lockhart, M.D., M.B.A. RiverGate
RCL AM 402 The Geriatric Outpatient: Postoperative
Cognitive Dysfunction and Other Concerns
Kathryn McGoldrick, M.D. E-1
RCL OB 403
Neuraxial Labor Analgesia and Pregnancy
Outcome: Fact and Fiction
Cynthia Wong, M.D. E-2
RCL RA 404 The Age of HCAHPS: The Need for Acute
Pain Services Revisited
Michael Bottros, M.D. E-3
RCL CA 405 The Pulmonary Artery Catheter in 2014:
Past, Present, and Is There a Future?
Jonathan Mark, M.D. 260-262
RCL FA 406 ATLS Update: What Every Anesthesiologist
Needs to Know...BEFORE Going to the OR!
Maureen McCunn, M.D.,
M.I.P.P.
La Nouvelle
Ballroom AB
8-9:30 a.m. 90-Minute Panel AM PN81 Pediatric Ambulatory Challenges Raafat Hannallah, M.D. 208-210
90-Minute Panel AM PN82 Management of Patients at Risk of Sleep
Apnea in Ambulatory Anesthesia
Matthias Eikermann, M.D.,
Ph.D.
217-219
90-Minute Panel FA PN84 Beyond Smoke and Mirrors: Panel on
Surgical Fire Prevention Including Laser
Safety
Charles Cowles, M.D., M.B.A. 225-227
90-Minute Panel PI PN85 What Is the Role of the Anesthesiologist
Asked to Participate in a Procedure He/
She Believes Will Not Benet the Patient?
Nicholas Sadovnikoff, M.D.,
F.C.C.M.
228-230
90-Minute Panel PI PN86 Professionalism - Who Needs It? Why
Professionalism Matters No Matter Where
You Work
Saundra Curry, M.D. 252-254
Clinical Forum PD CF12 In a Land Far Away From Home ... Remote
Anesthetic Care for the Medically Complex
Pediatric Patient
Inger Aliason, M.D. 206-207

43
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Point-
Counterpoint
CA PC14 Volatile Anesthetics for Cardioprotection:
Is Preconditioning a Bust?
Stefan De Hert, M.D. 203-205
Point-
Counterpoint
PI PC15 Anesthesia Information Management
Systems Should Be the Standard of Care
for All Patients Receiving an Anesthetic
Joseph Szokol, M.D., J.D.,
M.B.A.
211-213
Oral
Presentations
FA OR02-2 Anesthetic Action and Biochemistry: Emerging Anesthetics and Analgesics 245
Oral
Presentations
CC OR06-2 Critical Care 244
Oral
Presentations
FA OR13-5 Outcomes and Database Research - Blood & Transfusions 245
Oral
Presentations
PI OR14-4 Patient Safety and Practice Management 244
Poster
Discussions
RA PD16-2 Regional Anesthesia and Acute Pain 243
8-10 a.m. Poster
Presentations
NA PO05-2 Clinical Neurosciences Hall B1-Area
E
Poster
Presentations
CA PO09-2 Experimental Circulation Hall B1-Area
C
Poster
Presentations
FA PO13-6 Outcomes and Database Research Hall B1-Area
A
Poster
Presentations
PI PO14-4 Patient Safety and Practice Management Hall B1-Area
B
Featured Lecture PN SPE20 Reduce Compliance Risks With Opioid
Prescribing
John Dombrowski, M.D. Great Hall B
8-11 a.m. Featured Lecture SPE21 Journal Symposium: How to Mechanically
Ventilate Patients in the Operating Room
in 2014
Jeanine Wiener-Kronish, M.D. 275-277
Hands-on
Workshop
PD 832 Point of Care: Novel Use of
Ultrasonography in Everyday Pediatric
Anesthesia Practice
Santhanam Suresh, M.D. Room 353-
354
Hands-on
Workshop
RA 828B Peripheral Nerve Blocks: Ultrasound,
Simulation and Stimulation
Andrew Rosenberg, M.D. Room 352
Hands-on
Workshop
FA 831A The Use of Ultrasound for Vascular
Access in Adults and Pediatrics
Ehab Farag, M.D., F.R.C.A. 338-339
Hands-on
Workshop
CA 833A Thoracic Anesthesia Workshop Edmond Cohen, M.D. 356-357
8-11:30 a.m. Hands-on
Workshop
CC 830A Perioperative ACLS Simulation Workshop Matthew McEvoy, M.D. Room 281
9-10:15 a.m.
PBLD CA L161 Descending Thoracic Aortic Repair - Spinal
Cord Protection Strategies
Harendra Arora, M.D. 343-345
PBLD FA L162 Beyond Swiss Cheese - Cases for the
Anesthesia Patient Safety Ofcer
Jonathan Cohen, M.D. 343-345
PBLD PD L163 Wake Up Your Surgery Is Not Over Prabhakar Devavaram,
M.B.B.S
343-345
PBLD CC L164 Management of Severe ARDS in the ICU
With ECMO
Jacob Gutsche, M.D. 343-345
PBLD FA L165 Malignant Hyperthermia in a Child Having
a Tethered Cord Release
Tae Kim, M.D. 343-345
PBLD RA L166 Antibrinolytic Use in Major Orthopedic
Procedures: What’s the Bloody
Controversy?
Yan Lai, M.D. 343-345
PBLD OB L167 She was Advised Not to Get Pregnant and
She Did: Pulmonary Hypertension and
Pregnancy
TanyaLucas, M.D. 343-345
PBLD RA L168 Thoracic Epidural Analgesia in the
Recently Anticoagulated Patient: Is This a
Good Idea?
Anuj Malhotra, M.D. 343-345
PBLD FA L169 Cardiopulmonary Collapse During
Laparoscopic Nissen Fundoplication
Govind Rajan, M.B., B.S. 343-345
PBLD PI L170 The Impaired Anesthesiologist: More Than
Just Drugs and Alcohol
Gregory Rose, M.D. 343-345
SCHEDULE BY DAY: TUESDAY

44
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
PBLD AM L171 A Slip and Fall in the Post Warfarin Era Mercy Udoji, M.D. 343-345
PBLD OB L172 A Parturient Presenting in Premature
Labor With Single-Ventricle Physiology
Complicated by Breech Presentation and
Paroxysmal Supraventricular Tachycardia:
What’s Your Labor Management Plan?
Manuel Vallejo, M.D., D.M.D. 343-345
9:15-10:15 a.m. RCL RA 407 Virtual Cadaver Lab - Anatomy Pearls in
Regional Anesthesia to Improve Clinical
Success
David Auyong, M.D. RiverGate
RCL OB 408 Strategies to Optimize Cesarean Delivery
Analgesia
Brendan Carvalho, F.R.C.A. E-1
RCL PD 409 Acute Postoperative Pain Management in
Infants and Children: Size Does Matter!
Patrick Birmingham, M.D. E-2
RCL CA 410 Patient Safety in the Cardiac Operating
Room: What Can, Will and Might Make
Patients Safer and You Happier
James Abernathy, III, M.D.,
M.P.H.
E-3
RCL FA 411 Anesthetics and the Brain - Less
Mysterious Than You May Think
Misha Perouansky, M.D. 260-262
RCL PI 412 Safety and Human Factors in Anesthetic
Practice
Keith Ruskin, M.D. La Nouvelle
Ballroom AB
10-11:30 a.m. 90-Minute Panel RA PN83 Acute Pain Management in the Patient
With Opioid Tolerance Dependance or
Addiction
David Provenzano, M.D. 252-254
90-Minute Panel CC PN87 Fluid Administration During the
Perioperative Period: Does It Make a
Difference What and How Much You
Give?
Matthias Jacob, M.D., Ph.D. 208-210
90-Minute Panel NA PN88 Sleeping and Waking Is Hard to Do:
Mechanisms of Induction and Emergence
From General Anesthesia
Peter Goldstein, M.D. 220-222
90-Minute Panel PI PN89 Clean Versus Green: Are Optimized
Patient Care and Community Health/
Safety Initiatives Mutually Exclusive?
Brian Rothman, M.D. 225-227
90-Minute Panel FA PN90 Clinical Pearls: Anesthesia for Adult ENT
Surgery
Basem Abdelmalak, M.D. 228-230
Clinical Forum PI CF13 Controversial Cases in Organ Donation
and End-of-Life Care: Terminal Live Organ
Donation and the Sale of Human Organs
Richard Wolman, M.D., M.A. 206-207
Point-
Counterpoint
CC PC16 Can Post-Operative Delirium Really Be
Managed?
Pratik Pandharipande, M.D. 203-205
Point-
Counterpoint
RA PC17 Should I Be Using More Than One Local
Anesthetic Additive During Peripheral
Nerve Blockade?
Anahi Perlas, M.D. 211-213
Oral
Presentations
FA OR13-4 Outcomes and Database Research - Airway & Sleep Apnea
245
Poster
Discussions
CA PD04-1 Clinical Circulation: Echo 243
Poster
Discussions
NA PD10-1 Experimental Neurosciences: Neurotoxicity 243
Poster
Discussions
PD PD15-3 Pediatric Anesthesia: General 244
10 a.m.-12 p.m. Featured Lecture SPE28 AQI Listening Session Richard P. Dutton, M.D., M.B.A. 223
120-Minute
Panel
RA PN25 ASRA Practice Advisories: Review and
Update
Terese Horlocker, M.D. 217-219
Poster
Presentations
CC PO06-3 Critical Care Hall B1-Area
D
Poster
Presentations
FA PO07-2 Drug Disposition, Metabolism and Elimination Hall B1-Area
A
Poster
Presentations
NA PO10-4 Experimental Neurosciences: Inammation, Cognitive Dysfunction and
Neuroprotection
Hall B1-Area
E
Poster
Presentations
OB PO12-1 Obstetric Anesthesia: Cesarean Delivery Hall B1-Area
C
EDUCATION

45
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
45
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
Poster
Presentations
RA PO16-5 Regional Anesthesia and Acute Pain Hall B1-Area
B
10:30-11:30
a.m.
Featured Lecture PN SPE22 John W. Severinghaus Lecture on
Translational Science: Basic Science to
Clinical Practice: The Tale of Long-Acting
Opioids
Evan Kharasch, M.D., Ph.D. Great Hall
AD
11:45 a.m.-
12:45 p.m.
RCL PI 413 Mindfulness in Anesthesia: A Safety and
Satisfaction Initiative
Neil Farber, M.D., Ph.D. RiverGate
RCL OB 414 Improving Patient Safety on the Labor and
Delivery Suite through Changes in Culture,
Education, and Communication
David Birnbach, M.D., M.P.H. E-1
RCL RA 415 Continuous Peripheral Nerve Blocks in
2014: Techniques, Management, Benets,
and Avoiding Complications
Brian Ilfeld, M.D., M.S. E-2
RCL FA 416 Anesthesia for Head and Neck Surgery David Healy, M.D., M.R.C.P.,
F.R.C.A.
E-3
RCL FA 417 Preoperative Identication, Evaluation,
and Optimization of the Highest Risk
Patients
Bobbie Jean Sweitzer, M.D. 260-262
RCL CA 418 TEE for the Occasional Cardiac
Anesthesiologist
Michael Cahalan, M.D. La Nouvelle
Ballroom AB
12:30-1:45 p.m. PBLD FA L099 Perioperative Laboratory and Cardiac
Testing: What is Necessary?
David Hepner, M.D. 343-345
PBLD OB L173 Cesarean Delivery in a Patient With
Hypertrophic Obstructive Cardiomyopathy
Jaime Aaronson, M.D.
Stephanie Goodman, M.D.
343-345
PBLD RA L174 Perioperative Management of the Patient
on Anticoagulant Therapy: A Fresh Look at
an Old Problem
Richard Beers, M.D. 343-345
PBLD FA L175 Management of Antiplatelet Therapy
in Patients With Coronary Stents for
Noncardiac Surgery
Davide Cattano, M.D., Ph.D. 343-345
PBLD NA L176 Just Another Subarachnoid Hemorrhage?
Or Am I Really Up-to-date on What to Do?
Eduardo Galeano, M.D. 343-345
PBLD PD L177 Trials and Tribulations: Interventional
Management for Recurrent Complex
Regional Pain Syndrome in Children
Stephen Hays, M.D. 343-345
PBLD PI L178 How to Create and Moderate a Great
Problem Based Learning Discussion
(PBLD)
Kirk Lalwani, M.D. 343-345
PBLD RA L179 Tough Choices: Regional or General
Anesthesia in a Very Elderly Patient
Jason Lane, M.D., M.P.H. 343-345
PBLD CA L180 Patient With a Failing Fontan for
Emergency Exploratory Laparotomy
Galina Leyvi, M.D. 343-345
PBLD PI L181 He’s 15, Needs This Operation and He’s
DNR!
David Mann, M.D. 343-345
PBLD PD L182 A Child With Mitochondrial Disease and
Propofol Allergy Who May be Susceptible
to Malignant Hyperthermia
Jayant Pratap, M.B., B.Ch. 343-345
PBLD FA L183 Perioperative Management of the Anemic
Patient
Russell Roberson, M.D. 343-345
12:40-1:50 p.m. Featured Lecture FA SPE23 Lewis H. Wright Memorial Lecture James Bagian, M.D., PE 265-268
1-2 p.m. RCL PI 419 Five Years of the AQI: What Do We Know
About Ourselves Now?
Richard Dutton, M.D., M.B.A. RiverGate
RCL NA 420 Perioperative Management of
Cerebrovascular Diseases
Adrian Gelb, M.B, B.Ch.,
FRCPC
E-1
RCL RA 421 Local Anesthetics: Mechanisms, Toxicities
and Controversies From a Clinical
Perspective
John Butterworth, M.D. E-2
RCL CA 422 Massive Post-Cardiopulmonary
Hemorrhage: A Rational Approach to
Management
Edwin Avery, IV, M.D. E-3
SCHEDULE BY DAY: TUESDAY

46
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
RCL PI 423 Do the Right Thing: Resolving Ethical
Dilemmas in the OR
Sarah Smith, M.D. 260-262
RCL FA 424 Massive Transfusion Protocol in Trauma Charles Smith, M.D. La Nouvelle
Ballroom AB
1-2:30 p.m. 90-Minute Panel CC PN91 The Evolving Goals of the ICU: Critical
Care, Palliative Care, or Patient-Centered
Care
Neal Cohen, M.D., M.P.H. 217-219
Clinical Forum FA CF14 Dogma and Controversies in Acute and
Perioperative Burn Care
Sam Sharar, M.D. 206-207
Point-
Counterpoint
FA PC18 Hypotensive Resuscitation Joshua Tobin, M.D. 203-205
Point-
Counterpoint
PI PC19 Simulation in Medical Education: Boon or
Boondoggle?
Amanda Burden, M.D. 211-213
Oral
Presentations
CA OR09-2 Experimental Circulation 244
Poster
Discussions
FA PD17-1 Respiration-Upper Airway and Sleep Apnea 245
1-3 p.m. 120-Minute
Panel
PI PN26 The Economics of the Perioperative
Surgical Home; We Know Where We Are
and Where We Want to Go, But How Do
We Get There?
Peter Dunbar, M.B., Ch.B.,
M.B.A
208-210
120-Minute
Panel
AM PN27 Novel Drugs in Ambulatory Practice. How
Would They Change Your Practice?
Tong Gan, M.D. 220-222
120-Minute
Panel
CA PN28 Percutaneous Approaches to Aortic and
Mitral Pathology
Michael Fitzsimons, M.D. 225-227
120-Minute
Panel
PI PN29 Everything You Need to Know About
Lawsuits, But Didn’t Know Whom to Ask
Aparna Ananth, M.D. 228-230
120-Minute
Panel
FA PN30 Computer-Assisted Personalized Sedation
(CAPS) - the Future of Moderate Sedation
Walter Maurer, M.D. 252-254
120-Minute
Panel
PD PN31 Editor’s Picks in Pediatric
ANESTHESIOLOGY™ 2014
Constance Houck, M.D. 255-257
Poster
Presentations
FA PO02-2 Anesthetic Action and Biochemistry: Molecular Insights into Anesthetic
Mechanism of Action,Safety and Toxicity
Hall B1-Area
C
Poster
Presentations
CA PO04-4 Clinical Circulation: Blood/Coagulation Hall B1-Area
D
Poster
Presentations
FA PO08-4 Equipment, Monitoring and Engineering Technology: Anesthesia Depth and
Eclectic Assortment of Cool Stuff
Hall B1-Area
B
Poster
Presentations
FA PO13-4 Outcomes and Database Research Hall B1-Area
A
Poster
Presentations
PD PO15-4 Pediatric Anesthesia Hall B1-Area
E
Featured Lecture SPE24 Best of Abstracts: Clinical James Rathmell, M.D. 275-277
1-4 p.m. Hands-on
Workshop
RA 828C Peripheral Nerve Blocks: Ultrasound,
Simulation and Stimulation
Andrew Rosenberg, M.D. Room 352
Hands-on
Workshop
FA 831B The Use of Ultrasound for Vascular
Access in Adults and Pediatrics
Ehab Farag, M.D., F.R.C.A. 338-339
Hands-on
Workshop
CA 833B Thoracic Anesthesia Workshop Edmond Cohen, M.D. 356-357
1-4:30 p.m. Hands-on
Workshop
CC 830B Perioperative ACLS Simulation Workshop Matthew McEvoy, M.D. Room 281
2-4 p.m. Featured Lecture PI SPE25 History Panel - Show Me the Money:
A Brief History of Remuneration in
Anesthesiology
Douglas Bacon, M.D., M.A. 265-268
2:15-3:15 p.m. RCL PD 426 Anesthetic Management of Common
Pediatric Emergencies
Franklyn Cladis, M.D. E-1
RCL PN 427 Healthcare Reform and Pain Medicine
-Impact and Strategies for Future Success
Richard Rosenquist, M.D. E-2
RCL FA 428 Strategies for Success in Anesthesia
During One-Lung Ventilation
Gregory Fischer, M.D. E-3
RCL CA 429 Update on Strategies for Blood
Conservation and Hemostasis in Cardiac
Surgery
C. Mazer, M.D. 260-262
EDUCATION

47
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain
RCL FA 430 Electrical Safety in the Operating Room Jeffrey Gross, M.D. La Nouvelle
Ballroom AB
2:15-4:15 p.m. RCL PI 425 Improving Patient Safety and
Communication During Anesthesia and
Surgery
Richard Cook, M.D. RiverGate
3-4:30 p.m. Point-
Counterpoint
CC PC20 Electronic Health Records Improve Patient
Safety - or Do They?
David Feinstein, M.D. 203-205
Poster
Discussions
CC PD06-1 Critical Care 243
Poster
Discussions
FA PD08-4 Equipment, Monitoring and Engineering Technology: Advances in
Noninvasive Monitoring
245
Poster
Discussions
OB PD12-2 Obstetric Anesthesia: Labor Analgesia, Outcomes, Hemorrhage and
Miscellaneous
244
3-5 p.m. 120-Minute
Panel
FA PN32 Creating the Safe Non-Operating Room
Anesthesia (NORA) Experience
Brenda Gentz, M.D. 211-213
Clinical Forum NA CF15 You Want to Test What?: Anesthetic
Challenges During Functional
Neurosurgery
Antoun Koht, M.D. 206-207
3:30-4:30 p.m. RCL FA 431 Trauma Anesthesia and Operative
Resuscitation
Joshua Tobin, M.D. E-1
RCL FA 432 Different Strokes for Operative Folks:
Prevention of the Perioperative
Cerebrovascular Accident
Georgte Williams, II, M.D. E-2
RCL FA 433 Current Controversies of Perioperative
Fluid Management
Roman Dudaryk, M.D. E-3
3:30-4:45 p.m. PBLD FA L184 Help! My Patient Is on a Multi-
Chemotherapeutic Regiment and Is
Coming for a Laparotomy! What Do I Need
to Know?
Anoushka Afonso, M.D. 343-345
PBLD PD L185 Cardiovascular Collapse During
Thoracoscopic Tracheoesophageal Fistula
Repair
Kimberly Blasius, M.D. 343-345
PBLD NA L186 Crisis in the Neuro-Muscular Junction.
Anesthetic Implications
Cristina Barboi, M.D. 343-345
PBLD FA L188 A Patient With End-Stage Liver Disease for
Elective Surgery
Christopher Darling, D.O.
Michael Hannaman, M.D.
343-345
PBLD FA L189 Can the Adult Patient With Morbid Obesity
and Obstructive Sleep Apnea Safely
Undergo Outpatient Surgery?
Kenneth Hiller, M.D. 343-345
PBLD PI L190 Giving Feedback: How to Support the
Defensive Learner
YuliaIvashkov, M.D. 343-345
PBLD
PI L191 How Not to End Up on the Nightly News:
Safe Injection Practices
Vilma Joseph, M.D. 343-345
PBLD RA L192 A 40-Year -Old Woman With Multiple
Sclerosis Consulting for Postoperative
Epidural Following Laparoscopic
Converted to Open Colectomy
John Shepler, M.D.
Kristopher Schroeder, M.D.
343-345
PBLD PD L193 It Is Just a Nosebleed, Isn’t It? Anesthetic
Considerations for Unsuspected
Pulmonary Hypertension
Shu-Ming Wang, M.D. 343-345
PBLD PD L194 Using Advanced Trauma Life Support to
Manage a Pediatric Trauma Patient With
Traumatic Brain Injury and Disclosure of
Difcult News After a Poor Outcome
David Young, M.D., M.Ed 343-345
3:30-5 p.m. 90-Minute Panel CA PN92 Perioperative 3D TEE: Innovative Imaging
or Just Pretty Pictures?
Stanton Shernan, M.D.,
F.A.H.A., F.A.S.E.
208-210
90-Minute Panel FA PN93 Sugammadex: Are We Finally There?
Update on Unmet Medical Need Clinical
Use in Europe and Regulatory Progress
Jonathan Jahr, M.D. 217-219
90-Minute Panel CC PN94 Optimizing Perioperative Renal Function Robert Sladen, M.B., Ch.B.,
F.C.C.M.
220-222
90-Minute Panel PI PN95 Responding to Human Errors: The Good,
the Bad, and the Ugly
Robert Lagasse, M.D. 225-227
SCHEDULE BY DAY: TUESDAY

48
90-Minute Panel AM PN96 Identifying Triage Decisions in Ambulatory
Anesthesia: Right Patient, Place,
Technique and Time
Mary Ann Vann, M.D. 228-230
3:30-5:30 p.m. 120-Minute
Panel
CC PN33 Anesthesia for the Patient Too Sick for
Anesthesia
Daniel Brown, M.D., Ph.D. 252-254
WEDNESDAY, OCT. 15
Time Session Type Track Fee Code Title Speaker Location
7 a.m.-12 p.m. Registration Lobby A & D
8-9 a.m. RCL CC 501 Emergent Airway Management: Tips,
Tricks, and Evidence
Aaron Joffe, D.O. E-1
RCL CA 502 Postoperative Acute Kidney Injury in
Cardiac Surgery
Madhav Swaminathan, M.D. E-2
RCL FA 503 Recent Advances in Perioperative Fluid
Management and the Patients’ Outcomes
Ehab Farag, M.D., F.R.C.A. E-3
8-9:30 a.m. 90-Minute Panel CA PN100 Protecting the Lung During Cardiac
Surgery: An Interdisciplinary Approach
Eric Nelson, D.O. 208-210
90-Minute Panel AM PN97 Challenges in Ambulatory Out-of-OR
Anesthesia Practice
Radha Arunkumar, M.B., B.S.,
M.D.
208-210
90-Minute Panel CC PN98 FFP: A Critical Appraisal in 2014 Aryeh Shander, M.D. 217-219
90-Minute Panel FA PN99 Big Data, Big Opportunity: Anesthesiology
2.0
Jesse Ehrenfeld, M.D., M.P.H. 220-222
Poster
Discussions
FA PD08-3 Equipment, Monitoring and Engineering Technology: Monitoring Sedation
and Cerebral Effects of Anesthesia
243
Oral
Presentations
FA OR13-5 Outcomes and Database Research - Blood & Transfusions 245
Oral
Presentations
PI OR14-4 Patient Safety and Practice Management 244
8-10 a.m. 120-Minute
Panel
FA PN34 Aortic Surgery in the 21st Century Rae Allain, M.D. 228-230
120-Minute
Panel
PI PN35 Grading the Graders - How Do We Get to
Better Performance Measures?
Laurent Glance, M.D. 252-254
120-Minute
Panel
RA PN36 Regional Anesthesia Adjuncts: Helpful or
Harmful?
Brian Williams, M.D., M.B.A. 255-257
8 a.m.-12 p.m. House of Delegates SPE26 House of Delegates: Session II Jane C.K. Fitch, M.D. Grand
Ballroom,
Hilton
Riverside
9:15-10:15 a.m. RCL CC
504 Perioperative Renal Protection Michael Hutchens, M.D. E-1
RCL RA 505 Perioperative Analgesia and Effect on
Patient Outcomes
Spencer Liu, M.D. E-2
10-11:30 a.m. Poster
Discussions
NA PD05-1 Clinical Neurosciences: Intraoperative Monitoring 245
Poster
Discussions
RA PD16-3 Regional Anesthesia and Acute Pain 244
EDUCATION
AM Ambulatory Anesthesia CA Cardiac Anesthesia CC Critical Care Medicine FA Fund. of Anesthesiology NA Neuroanesthesia
OB Obstetric Anesthesia PN Pain Medicine PD Pediatric Anesthesia PI Professional Issues RA Regional Anesthesia and Acute Pain

49
SCHEDULE BY DAY: TUESDAY & WEDNESDAY
NOTES
50
Ambulatory Anesthesia
Saturday, October 11
Problem-Based Learning Discussions | L009
Perioperative Anesthetic Issues for Ambulatory Surgery
7:15-8:30 a.m. | Room 343-345
Dean Jones, M.D., FRCPC
Refresher Course Lecture | 102
Current Controversies in Adult Outpatient Anesthesia
8-9 a.m. | Room E-1
Jeffrey Apfelbaum, M.D.
This presentation will involve a discussion of areas of current
controversy in ambulatory anesthesia and suggestions on
resolution. In the past, topics have included breaking news such
as changes to the CMS Interpretative Guidelines, drug shortages,
the use of computer assisted personalized sedation, and acute
changes to standards from accrediting bodies.
Problem-Based Learning Discussions | L021
It’s Just a Cataract: How a Simple Thing Can Go Bad
9-10:15 a.m. | Room 343-345
Michael Pilla, M.D.
Problem-Based Learning Discussions | L032
PONV, PDNV and Long QT Syndrome: Balancing Risk and Benet
12:30-1:45 p.m. | Room 343-345
Anuj Malhotra, M.D.
Clinical Forum | CF01
Pediatric Ambulatory Anesthesia: Clinical Forum
1-2:30 p.m. | Room 206-207
Lucinda Everett M.D.
This forum will explore topics related to pediatric ambulatory
anesthesia in the O.R. and beyond. Topics include the former
premature infant, airway issues, sleep apnea, anesthetic
considerations for MRI, anesthetic implications of GI diseases, and
cardiac dysrhythmias. T. Anderson M.D., Ph.D., Sally Rampersad
M.B., FRCA, Joshua Uffman, M.D.
120 Minute Panel | PN08
Anesthesia and Sedation for MRI: Adapting to Technological
Advances and Demands
1-3 p.m. | Room 255-257
Keira Mason M.D.
Safety and the American Society of Anesthesiologist Practice
Advisory
In clinical use for approximately 20 years, MRI is an emerging
and developing area of growth. Not only limited to diagnostic
imaging, MRI is a modality which is now being incorporated
into the operating room. As the MRI technology advances and
the imaging techniques and exams become more complex, the
demands on the anesthesiologist can become equally challenging.
The anesthesiologist must understand the American College of
Radiology and American Society of Anesthesiologists guidelines
and recommendations regarding both MRI safety and the delivery
of anesthesia and sedation in the MRI environment. Emergency
preparedness is critical in this off-site and often, remote location.
A thorough understanding of the MRI environment and the imaging
requirements needed for the complex imaging studies of the
airway, heart and brain are critical to providing safe anesthesia
care for obtaining quality imaging.
Dean Andropoulos, M.D., Tackling the Challenge of Anesthesia
for Cardiac Imaging, Mohamed Mahmoud, M.B.,B.Ch., Anesthesia
Considerations for Dynamic Airway Imaging, Anthony Absalom,
M.D., Keeping the Brain Intact for Functional Imaging, Craig
McClain, M.D., Keeping it Safe in the MRI Operating Room
Poster Presentations | PO01-1
Ambulatory Anesthesia: Risk Factors, Outcomes and Recovery
1-3 p.m. | Hall B1-Area A
Hands-on Workshop | 810
Must Know Blocks for Ambulatory Anesthesia
1-4 p.m. | Room 265-268
David Auyong M.D.
Clinical Tips for Ultrasound Success in Ambulatory Surgery
This workshop will consist of an initial lecture that includes 7
clinical keys for success with ultrasound, out-of-plane ultrasound
technique, and a 3-step process for ultrasound guided in-plane
needle visualization. We will then discuss appropriate nerve blocks
for specic surgeries, especially in the context of ambulatory
anesthesia. Next, the participants will rotate through 5 different
ultrasound stations covering the upper extremity, lower extremity,
and truncal nerve blocks. Specic nerve blocks that will be covered
include interscalene, supraclavicular, infraclavicular, axillary,
femoral, adductor canal, saphenous, popliteal sciatic, transversus
abdominis plane (TAP), rectus sheath, and paravertebral. We will
have available two stations for open scanning to provide additional
hands-on practice with experts in ambulatory nerve blocks.
James Benonis M.D., Christina DeLucca M.D., Ryan Derby M.D.,
M.P.H., Jeffrey Gonzales, M.D., Stuart Grant, M.D., Neil Hanson, M.D.,
David Hardman M.D., Raymond Joseph, M.D., David MacLeod, M.D.,
Gavin Martin M.B.,Ch.B., Ryan Nagy, M.D., Kristie Osteen, M.D.,
Leslie Thomas, M.D., Lisa Warren M.D.
Problem-Based Learning Discussions | L038
Is Ambulatory Shoulder Surgery Safe in a Patient With Obstructive
Sleep Apnea?
3:30-4:45 p.m. | Room 343-345
Christopher Canlas M.D.
90 Minute Panel | PN43
Advanced Diagnostic Bronchoscopy: Coming Soon to an ASC near
You
3:30-5 p.m. | Room 208-210
Basem Abdelmalak M.D.
Advanced Diagnostic Bronchoscopy: Anesthetic Considerations
and Techniques
There is an increasing demand for anesthesia services in
connection with the ever increasing use of interventional
pulmonology for mediastinal staging, biopsy, and diagnosis
of central and peripheral lung lesions. These procedures are
performed using endobronchial ultrasound bronchoscopy (EBUS)
and electromagnetic navigation bronchoscopy(ENB). Both of these
techniques are typically outpatient procedures, and as a result of
pulmonologists’ increasing levels of experience and familiarity with
them, they are being performed more often at out of the operating
room bronchoscopy suites as well as ambulatory surgery centers.
The patients who present for these procedures represent a
challenge for anesthesiologists, who must simultaneously consider
the severity of patients’ lung disease and comorbidities. Other
complicating factors may stem from the nature of the procedure,
as anesthesiologists must share the patient’s airway with
pulmonologists; the dynamic nature of the procedure; the airway
choice; and the ventilation mode used to accommodate these
procedures. This panel will discuss the above issues with the goal
of improving awareness, knowledge, and patient safety. Thomas
Gildea M.D., Advanced Diagnostic Bronchoscopy: Procedures,
Mona Sarkiss M.D., Advanced Diagnostic Bronchoscopy:
Complications
EDUCATION

51
Sunday, October 12
Subspecialty Panels | 605 (SAMBA) TIVA in 2014
7-8:15 a.m. | Room 238-239
Steven Butz M.D.
Learn why TIVA has become such a popular way of administering a
general anesthetic. In this panel, we will be reviewing the benets
of TIVA as well as recipes that have been successful. There will
be particular emphasis on ketamine and a case-study review of
appropriate use for all the IV drugs and settings. Richard Urman
M.D., M.B.A., TIVA: The Evolution of General Anesthesia, David
Dickerson M.D., TIVA and Ketamine, Niraja Rajan M.B., TIVA in the
Real World
Problem-Based Learning Discussions | L056
It’s Just a Cataract: How a Simple Thing Can Go Bad
7:15-8:30 a.m. | Room 343-345
Michael Pilla M.D.
Refresher Course Lecture | 205
Anesthesia for Outpatient Diagnostic and Therapeutic Radiology
8-9:00 a.m. | Room 260-262
Thomas Cutter M.D.
This RCL will cover various contrast formulations and how to
best manage the patient receiving them. It will include the
hazards to the patient and the provider in the MRI suites. It will
review radiation exposure in the the radiology suite and include
recommendations to minimize them. It will provide anesthetic
techniques for functional brain imaging studies and ambulatory
interventional radiology procedures.
Refresher Course Lecture | 213
Adult Patient With Morbid Obesity and OSA for Ambulatory Surgery:
An Update
10:30-11:30 a.m. | RiverGate
Girish Joshi M.B.B.S., M.D., FFARCSI
This refresher course lecture will provide an update on the
management of morbidly obese patients with obstructive sleep
apnea, a patient population that is increasing signicantly. In
addition, to recent publications, the new ASA recommendations for
selection of patients with OSA will be presented.
Clinical Forum | CF06
Ambulatory Non-Operating Room Anesthesia (NORA): It Ain’t That
Simple
1-2:30 p.m. | Room 206-207
Thomas Cutter M.D.
This forum will discuss the management and concerns for
ambulatory patients having minor procedures outside of the
operating room. Magdalena Anitescu M.D., NORA for the Pain Clinic,
Meghan E. Rodes, M.D., NORA for IR, Loreta Grecu M.D. NORA for
the EP Lab
Refresher Course Lecture | 227
Effective Management of Pain, PONV and Common Adverse Effects
in Ambulatory Surgical Patients
1:45-2:45 p.m. | Room 260-262
Tong Gan M.D.
This refresher course will describe the common postoperative
complications following ambulatory surgery, identify the risk
factors, evaluate the pharmacological and non pharmacological
modalities for management of pain and PONV and recommend
effective management strategies.
Oral Presentations | OR01-2
Ambulatory Anesthesia: Ambulatory Anesthesia Practice and
Outcomes
3-4:30 p.m. | Room 245
Problem-Based Learning Discussions | L090
It’s Just a Quick EGD in the Ofce...but Can I Safely Anesthetize
My Patient Here?
3:30-4:45 p.m. | Room 343-345
Jeena Jacob M.D.
90 Minute Panel | PN60
Crisis Management in Ofce-Based Anesthesia
3:30-5 p.m. | Room 208-210
Michael Walsh M.D.
Leak Patient Fires in Ofce-Based Surgery: Prevention and
Treatment
This panel will focus on three crisis scenarios in ofce based
anesthesia; malignant hyperthermia, local anesthesia toxicity, and
OR res. Risks factors, preventative strategies and emergency
management will be discussed. Andrew Herlich D.M.D., M.D..
F.A.A.P., Malignant Hyperthermia in Ofce Based Anesthesia:
Managing a Crisis, John Dilger M.D. Cosmetic Surgery, Liposuction
and Local Anesthetic Toxicity
90 Minute Panel | PN63
Ambulatory Surgery Airway Challenges
3:30-5 p.m. | Room 225-227
Raafat Hannallah M.D.
This panel will provide a practical approach to the implementation
of the updated difcult airway algorithm in adults and children.
Addressed will be methods of handling unanticipated difcult
airway cases and/or failed intubations in a free-standing surgery
center environment. An overview of the newer airway devices that
may be available for rescue in the ambulatory surgery setting will
be presented. Girish Joshi, M.D., Adults with Unanticipated Difcult
Airways, Jennifer Anderson M.D., Children with Unanticipated
Difcult Airways, Ashutosh Wali M.D. Newer Airway Devices in the
Ambulatory Surgery Setting
Monday, October 13
Problem-Based Learning Discussions | L105
PONV, PDNV and Long QT Syndrome: Balancing Risk and Benet
7:15-8:30 a.m. | Room 343-345
Anuj Malhotra M.D.
Oral Presentations | OR01-1
Ambulatory Anesthesia: Anesthesia Outcomes, Delirium and
Cognitive Dysfunction
8-9:30 a.m. | Room 243
Hands-on Workshop | 820
Ophthalmic Regional Anesthesia
8-11 a.m. | Room 333-334
Marc Feldman M.D., MHS
Orbital Needle Techniques
The workshop includes didactic lectures on ophthalmic regional
anesthesia followed by hands-on sessions with models and
anatomic specimens. Steven Gayer M.D., M.B.A., Sub-Tenon’s
Anesthesia Techniques, Joseph Bayes M.D., Richard Rivers M.D.,
Ph.D.
Problem-Based Learning Discussions | L112
Is Ambulatory Shoulder Surgery Safe in a Patient With Obstructive
Sleep Apnea?
9-10:15 a.m. | Room 343-345
Christopher Canlas M.D.
SCHEDULE BY LEARNING TRACK
52
Poster Presentations | PO01-2
Ambulatory Anesthesia: Sedation, Pharmacokinetics and Recovery
Outcomes
10 a.m.-12 p.m. | Hall B1-Area E
Problem-Based Learning Discussions | L132
A Slip and Fall in the Post Warfarin Era
12:30-1:45 p.m. | Room 343-345
Mercy Udoji M.D.
Refresher Course Lecture | 320
Malignant Hyperthermia in the Ambulatory Setting
1:45-2:45 p.m. | Room E-2
Ronald Litman D.O.
This refresher course will review the basic mechanisms of MH,
and detail the procedures involved with screening possible
MH susceptible patients for ambulatory anesthesia, as well as
describing the protocols when a patient develops MH in the
ambulatory setting.
Refresher Course Lecture | 325
Ultrasound Guided Regional Anesthesia for Ambulatory Surgery
3-4 p.m. | Room E-1
Meg Rosenblatt M.D.
This lecture will discuss the reasons for using us-guided regional
anesthesia in an ambulatory based practice. It will describe the
equipment prerequisites, teach 7+ blocks and their utilities as well
as showing how to begin an ambulatory catheter program.
Problem-Based Learning Discussions | L142
Perioperative Anesthetic Issues for Ambulatory Surgery
3:30-4:45 p.m. | Room 343-345
Dean Jones M.D., FRCPC
90 Minute Panel | PN74
Non-Operating Room Anesthesia: Techniques
3:30-5 p.m. | Room 208-210
Basavana Goudra M.D., FRCA, FCARCSI
Non-Operating Room Anesthesia: Techniques: Introduction
Non-operating room anesthesia is an expanding eld. Due
to unique challenges, the anesthesia skills and techniques
employed in these areas are different from those used in the main
operating room. Three distinguished s with extensive experience
and expertise in interventional bronchoscopy, gastroinestinal
endoscopy and electrophysiological procedures will present their
knowledge in this session. Nelson Thaemert M.D., Non-Operating
Room Anesthesia: Techniques for Electrophysiological Procedures,
Sheila Barnett M.B., B.S., B.Sc., Non-Operating Room Anesthesia:
Techniques for Advanced GI Endoscopic Procedures
Tuesday, October 14
Problem-Based Learning Discussions | L156
It’s Just a Quick EGD in the Ofce...but Can I Safely Anesthetize My
Patient Here?
7:15-8:30 a.m. | Room 343-345
Jeena Jacob M.D.
Refresher Course Lecture | 402
The Geriatric Outpatient: Postoperative Cognitive Dysfunction and
Other Concerns
8-9 a.m. | Room E-1
Kathryn McGoldrick M.D.
Because advanced age amplies the negative prognostic value of
impaired physical status, this lecture will offer recommendations to
avoid potential pitfalls associated with both general and regional
anesthesia in the elderly.
90 Minute Panel | PN81
Pediatric Ambulatory Challenges
8-9:30 a.m. | Room 208-210
Raafat Hannallah M.D.
The Snoring Obese Child for Ambulatory Adeno-Tonsillectomy:
When to Say No
This panel will provide an updated view of three current pediatric
ambulatory challenges. Addressed will be the obese child with
obstructive symptoms (snoring vs. OSAS), the choice of regional
blocks for sub-umbilical surgery (caudal vs. nerve blocks), an
update on the current concerns about the effects of anesthesia on
the young brains and how this may affect the decision to perform
elective diagnostic procedures requiring general anesthesia early
in life. Ronald Litman D.O., Is Caudal Block Still the Preferred
Regional Technique for Sub-Umbilical Surgery in Pediatric
Ambulatory Patients? Lena Sun M.D., Should We Limit the Exposure
of Young Children to “Elective” Diagnostic Procedures Requiring
General Anesthesia or Sedation?
90 Minute Panel | PN82
Management of Patients at Risk of Sleep Apnea in Ambulatory
Anesthesia
8-9:30 a.m. | Room 217-219
Matthias Eikermann M.D., Ph.D.
Postoperative Treatment of Patients with Sleep Apnea: CPAP?
Hospital Admission? Sleep Medicine Consultation? The incidence
of sleep apnea is high and the disease is associated with an
increased incidence of perioperative respiratory complications.
This panel will discuss the optimal allocation of resources in an
ambulatory anesthesia setting in order to optimze the value of
perioperative care in patients with sleep apnea. Satya-Krishna
Ramachandran M.D., Preoperative Screening - Expensive and
Inconclusive? Roman Schuman M.D., Do We Need Preoperative
Treatment to Optimize Sleep Disordered Breathing in Patients
Scheduled for Ambulatory Surgery?
Problem-Based Learning Discussions | L171
A Slip and Fall in the Post Warfarin Era
9-10:15 a.m. | Room 343-345
Mercy Udoji M.D.
120 Minute Panel | PN27
Novel Drugs in Ambulatory Practice. How Would They Change Your
Practice?
1-3 p.m. | Room 220-222
Tong Gan M.D.
Novel Antiemetics. Are They Better Than What We Have?
This panel will address the new and novel pharmacotherapy in
the ambulatory anesthesia setting and how these drugs can
impact on ambulatory anesthesia practice. Sorin Brull M.D.
Perioperative Neuromuscular Management: Novel Challenges and
Solutions in Ambulatory Anesthesia, Eugene Viscusi, M.D., Can
Newer Analgesics Eliminate Opioids in Ambulatory Surgery?
Talmage Egan M.D., New Intravenous Sedative-Hypnotics and
Propofol Formulations: Is There Life Beyond the Milky Way?
EDUCATION

53
90 Minute Panel | PN96
Identifying Triage Decisions in Ambulatory Anesthesia: Right
Patient, Place, Technique and Time
3:30-5 p.m. | Room 228-230
Mary Ann Vann M.D.
Tailoring the Anesthetic for the High Risk Patient and Location
A very important concern in ambulatory anesthesia is the proper
selection of patients and locations for certain procedures. This
panel with address triaging patients to the proper location for their
surgery. Management of high risk patients in the operating room
will be addressed as well as discussion of anesthesia techniques.
Potential postoperative recovery issues for certain patients will
be identied and limitations of recovery rooms will be discussed.
Meena Desai M.D., Triaging the Right Patient to the Right Location,
Stanford Plavin M.D., Adapting Recovery Room Care to Specialized
Patient Needs
Wednesday, October 15
90 Minute Panel | PN97
Challenges in Ambulatory Out-of-OR Anesthesia Practice
8-9:30 a.m. | Room 208-210
Radha Arunkumar M.B., B.S., M.D.
The Patient with Known/Suspected Difcult Airway
Increasingly, more patients are having procedures in an ambulatory
setting. There are potential pitfalls with the locations of care, the
complexity of the procedures and the pre-existing conditions of the
patients. This panel will provide an overview of common and some
rare clinical challenges encountered while anesthetizing in various
locations outside the operating rooms. This will be followed by
presentations on the specic clinical issues associated with
patients with difcult airways, morbid obesity and obstructive
sleep apnea (OSA), cardiac comorbidities including patients with
pacemakers and implantable cardioverter-debrillators (ICD).
Satya-Krishna Ramachandran M.D., FRCA, The Morbidly Obese and
Obstructive Sleep Apnea Patient, Marc Rozner M.D., Ph.D.
The Patient with Cardiac Comorbidities, Including Pacemakers/
Implantable Cardioverter-Debrillators
SCHEDULE BY LEARNING TRACK
54
Cardiac Anesthesia
Saturday, October 11
Refresher Course Lecture | 106
New Developments in Cardiopulmonary Resuscitation
8-9:00 a.m. | La Nouvelle Ballroom AB
Matthias Riess M.D., Ph.D.
This Refresher Course Lecture will provide an overview of the
current epidemiology of cardiac arrest, a review of the current
ACLS guidelines, an introduction to adjunct mechanical devices
such as active compression/decompression and impedance
threshold devices and their physiology, and initiate a discussion
on a more comprehensive role of anesthesiologists in in-hospital
cardiac arrest.
Oral Presentations | OR09-1
Experimental Circulation
8-9:30 a.m. | Room 244
90 Minute Panel | PN37
Modern Day Concepts in Thoracic Endovascular Repair (TEVAR) for
Aortic Aneurysms
8-9:30 a.m. | Room 208-210
David Broussard M.D.
Thoracic Endovascular Repair (TEVAR) is a less invasive
treatment modality for patients with thoracic aortic disease.
This panel will cover modern concepts in Thoracic Endovascular
Repair (TEVAR) for aortic aneurysms. Hernan Bazan M.D. Is
a Vascular Surgeon in New Orleans: Examine how the Various
Types of Hybrid Endovascular Techniques are Applied in Complex
Thoraco-Abdominal Disease Including: Antegrade Stenting,
Fenestrated Grafts, and Debranching Procedures, Crystal Wright
M.D., Understand Etiology of Common Intraoperative and Post-
operative Complications Including Spinal Cord Ischemia, Acute
Kidney Injury, and Gut Malperfusion, Kelly Ural M.D., Examine
the Role of Perioperative Anesthetic Monitoring Choices and
Anesthetic Regimens on Perioperative Morbidity Including Spinal
Cord Perfusion Pressure, Ideal Arterial Pressure, and Ideal
Neuromonitoring
120 Minute Panel | PN02
Practice Guidelines in CV Anesthesia: How Are We Doing as a
Specialty?
8-10 a.m. | Room 252-254
Martin London M.D.
ACCF/AHA Guidelines for Coronary Artery Bypass Grafting
The panel brings together a variety of experts in CV anesthesia
who have actively participated in development of practices
guidelines in areas in which CV anesthesiologists are actively
involved in patient management. Differences in methodology and
potential impacts on clinical practice over time will be discussed
and debated. Nikolaos Skubas M.D. ACCF/AHA Guidelines for
Valvular Heart Disease, Stephen Rupp M.D. ASA Central Venous
Access Guidelines, Scott Reeves M.D., M.B.A., SCA and American
Society of Echocardiography Guidelines, C. David Mazer M.D.
SCA and Society of Thoracic Surgeons Collaborative Guidelines
Refresher Course Lecture | 112
Perioperative Management of Cardiovascular Implantable Electronic
Devices
9:15-10:15 a.m. | La Nouvelle Ballroom AB
Annemarie Thompson M.D.
Patients with CIEDs are presenting for elective surgery in ever
increasing numbers. Anesthesiologists will increasingly be called
upon to assist in the development of institution-specic strategies
based on local resources to efciently manage patients with CIEDs
who present for surgery. A basic understanding of CIEDs combined
with continuing education about the perioperative management of
these devices will assist anesthesiologists in the important task of
caring for patients with CIEDs.
Poster Presentations | PO04-2
Clinical Circulation: Outcomes
10 a.m.-12 p.m. | Hall B1-Area A
Poster Presentations | PO09-3
Experimental Circulation
10 a.m.-12 p.m. | Hall B1-Area B
Problem-Based Learning Discussions | L026
Carotid Endarterectomy: Asleep Versus Awake
12:30-1:45 p.m. | Room 343-345
Jeffrey Dobyns D.O.
Oral Presentations | OR04-1
Clinical Circulation: Outcomes
1-2:30 p.m. | Room 244
120 Minute Panel | PN04
Perioperative Patient Safety in Cardiovascular Surgery: From Data
to Implementation
1-3 p.m. | Room 220-222
Nancy Nussmeier M.D.
The Six C’s in CV Surgery: Communication, Coordination,
Cooperation, Cognition, Coaching, and Conict Resolution
This is a interdisciplinary Patient Safety Panel that will put
into clnical persepctive the last two decades of research in
communication and teamwork in the operating room. Transitions of
care (eg, handoffs) of patients to the intensive care unit will also
be covered. Evidence-based recommendations for implementation
of improvements will be made. Joyce Wahr M.D., Human Factors
and Human Errors in the Cardiac O.R.: What Have We Learned
in 20 Years of Research, Jonathan Mark M.D., Communication
between Teams: Coordination across Transitions of Care, Alan Merry
M.D., The Seventh C: The Just Culture
Hands-on Workshop | 809
Pacemakers and ICDs
1-4 p.m. | Room 278-279
Aman Mahajan M.D., P.h.D.
This lecture and hands-on workshop will describe the design,
functioning, and programming of implantable pacemakers and
AICDs. We will also discuss the perioperative management of
pacemakers during elective and emergency surgeries. We will
identify sources of electromagnetic interference (EMI) causing
pacemaker malfunction. We will describe use of various temporary
pacing devices and generators in perioperative settings. We will
also provide examples of pacemaker related rhythm abnormalities
in the perioperative period. Jason Chua M.D., Jonathan Ho M.D.,
Kimberly Howard-Quijano M.D., Jacques Neelankavil M.D., Eric
Nelson D.O., Peter Schulman M.D., Scott Streckenbach M.D., Dilip
Thakar M.D., Annemarie Thompson M.D.
EDUCATION

55
Refresher Course Lecture | 115
Perioperative Lung Protective Strategies in One-Lung and Two-Lung
Ventilation
1:30-2:30 p.m. | La Nouvelle Ballroom AB
Peter Slinger M.D.
Problem-Based Learning Discussions | L042
I Thought Three Pump Runs Were Bad but This Pulmonary Edema
is Even Worse! What is Going On?
3:30-4:45 p.m. | Room 343-345
Marcellene Franzen, M.D., Lindsey Loveland-Baptist M.D.
Clinical Forum | CF03
Circulatory Assist: The Coming Tidal Wave
3:30-5 p.m. | Room 206-207
Roman Sniecinski M.D.
Indications and outcomes for adult ECMO will be discussed for
different clinical scenarios. Ronald Pearl M.D., Ph.D., ECMO in
Respiratory Failure, Steven Miller M.D., ECMO in Cardiogenic Shock,
Michael Fitzsimons M.D., Troubleshooting ECMO in the ICU
90 Minute Panel | PN44
Thoracic Surgery 2014
3:30-5 p.m. | Room 217-219
Nathaen Weitzel M.D.
Thoracic Surgery 2014 is a 90-minute panel designed to refresh
learners on the management of standard thoracic surgical cases,
but also to delve into complex airway surgery, as well as pain
management strategies for thoracic surgery. Miklos Kertai M.D.
A Typical Thoracic Surgery: Management of Tracheoplasty for
Tracheomalacia, Tracheal Resection, and Sleeve Resections, Julie
Huffmyer M.D., What to Do When the O2 Saturations Fall During
One-Lung Ventilation?, Matthew Fiegel M.D. Pain Management
Strategies for Thoracic Surgery
Sunday, October 12
Problem-Based Learning Discussions | L054
I Thought Three Pump Runs Were Bad but This Pulmonary Edema
is Even Worse! What is Going On?
7:15-8:30 a.m. | Room 343-345
Marcellene Franzen M.D., Lindsey Loveland-Baptist M.D.
Refresher Course Lecture | 204
Rethinking Acute Blood Pressure Management in the Perioperative
Setting
8-9 a.m. | Room E-3
Solomon Aronson M.D., M.B.A., FACC, FCCP, FAHA, FASE
Perioperative Blood Pressure Management
Refresher Course Lecture | 206
Preoperative Cardiac Evaluation for Noncardiac Surgery
8-9 a.m. | La Nouvelle Ballroom AB
Lee Fleisher M.D.
The AHA/ACCF Perioperative Cardiovascular Evaluation Guidelines
were updates in 2013 to reect new evidence. This refresher
course will discuss the new guidelines.
90 Minute Panel | PN51
Heart Failure in Adults Undergoing Non-Cardiac Surgery
8-9:30 a.m. | Room 217-219
Amanda Fox M.D., M.P.H.
Managing Right Heart Failure and Pulmonary Hypertension for Non-
Cardiac Surgery
At the conclusion of the panel the participant will be familiar with
strategies for identifying and managing adult acute and chronic
heart failure patients who are scheduled to undergo non-cardiac
surgery. The participant will understand signicant anesthetic
implications of systolic and diastolic heart failure, right heart
failure, and ventricular assist devices. Leanne Groban M.D.,
Highlights of the Guidelines for Diagnosis and Management of
Adult Chronic Heart Failure, Nancy Nussmeier M.D., Perioperative
Implications of Acute and Chronic Heart Failure in Non-Cardiac
Surgery, Eric Nelson D.O., Managing the VAD Patient for Non-Cardiac
Surgery
Poster Presentations | PO04-1
Clinical Circulation: Echo/Monitoring
8-10 a.m. | Hall B1-Area E
Yuta Kashiwagi M.D.
Hands-on Workshop | 815
Basic TEE Workshop
8 a.m.-4 p.m. | Room 338-339
Sasha Shillcutt M.D.
Two three-hour sessions, with the second session being a
continuation of the rst session. Each session (AM/PM) will
consist of one hour of didactic lectures followed by two hours
hands-on breakout sessions. The breakout sessions, in addition
to live model TTE, will include multiple TEE simulator stations
featuring both normal and pathologic ndings. The participants
will be divided into two identical workshop divisions, each
composed of three stations where participants will rotate. The
participants will spend a total of 40 minutes on each simulation
station (total 2 hours). Julian Bick M.D., TEE Evaluation of the
Mitral Valve, Tara Brakke M.D., Basic TEE Views: Anatomy and
Image Orientation, Susan Martinelli M.D., Rescue TEE in the Non-
Cardiac Room, Candice Montzingo M.D., How Ultrasound Works:
Ultrasound Physics and Principles, Albert Perrino M.D., LV Function
- The Bare Essentials, Christopher Troianos M.D., TEE Evaluation of
the Aorta and Aortic Valve, John Augoustides M.D., Mary Beth Brady
M.D., Amy Duhachek-Stapelman M.D., Alan Finley M.D., Meghann
Fitzgerald M.D., George Guldan III, M.D., Alexander Mittnacht M.D.,
Alina Nicoara M.D., Wanda Popescu M.D., Thomas Schulte M.D.,
Robert Suriani M.D.
Problem-Based Learning Discussions | L068
Patient With a Failing Fontan for Emergency Exploratory
Laparotomy
9-10:15 a.m. | Room 343-345
Galina Leyvi M.D.
Refresher Course Lecture | 209
Congenital Heart Disease in the Adult Presenting for Non-Cardiac
Surgery
9:15-10:15 a.m. | Room E-2
Ilka Theruvath, M.D.
This refresher course will provide an overview of the most common
adult congenital heart lesions, describe the implications of long-
term altered physiology in adult congenital heart disease and
discuss major difculties in anesthetic management of adult
congenital heart patients presenting for non-cardiac surgery.
SCHEDULE BY LEARNING TRACK
56
Clinical Forum | CF05
Adult Congenital Heart Disease (ACHD):Special Considerations for
Patients With CHD Surviving Into Adulthood
10-11:30 a.m. | Room 206-207
James DiNardo M.D.
This session is designed to familiarize the participant with current
expected outcomes for adults with congenital heart heart disease
(ACHD) as well as to educate the participant as to the anesthetic
considerations for ACHD undergoing re-do cardiac procedures,non-
cardiac procedures, and presenting for peripartum management.
Mark Twite M.D., Current Outcomes and Expectations for Patients
With Common Congenital Heart Lesions, Marc Hassid M.D., Adults
With CHD Presenting for Redo-Cardiac Surgical Procedures, Nelson
Thaemert M.D., Adults With CHD Presenting for Non-Cardiac
Surgery, Sugantha Sundar M.D., Adults With CHD Presenting to
Labor and Delivery
Poster Discussions | PD04-2
Clinical Circulation: Blood, Other
10-11:30 a.m. | Room 243
Refresher Course Lecture | 215
Catheter Based Cardiac Surgery: Anesthesia in the Hybrid Suite and
Cath Lab
10:30-11:30 a.m. | Room E-2
Nathaen Weitzel M.D.
This Refresher Course lecture is designed to educate learners
on the intricacies of catheter based cardiac interventions in the
operating room and hybrid suite. Discussion will focus on current
management strategies for TAVR for both trans-femoral and
trans-apical approaches, catheter based mitral valve repair, atrial
appendage exclusion, and lead extractions. The focus will be on
risk identication for patients as well as practical management
techniques in these challenging cases.
Poster Discussions | PD09-1
Experimental Circulation
1-2:30 p.m. | Room 245
Refresher Course Lecture | 233
New Developments in Thoracic Anesthesia
3-4 p.m. | Room 260-262
Edmond Cohen M.D.
The refresher course will discuss the most recent developments
in lung separation, will explain the concept of management of
hypoxemia during one lung ventilation and will address the issue of
protective lung ventilation.
90 Minute Panel | PN61
Cerebral Oximetry Monitoring: Does It Affect Neurologic Outcome?
3:30-5 p.m. | Room 217-219
John Murkin M.D. Cerebral Oxygen Saturation Monitoring: Why and
How to Use It
This session is an interactive panel discussion with featured
presentations outlining the pathophysiology of cerebral blood ow
and concepts of static and dynamic autoregulation and the impact
of cardiopulmonary bypass, reviewing the principles and limitations
of current cerebral oximetry technologies and evidence for their
clinical utility and how to intervene clinically, and exploring new
developments in cerebral oximetry technology and how this can
impact clinical outcomes with an open forum to discuss whether
further technical developments, mechanistic evidence and/or
clinical trials are needed to support widespread utilization. Hilary
Grocott M.D., The Physiology of Cerebral Blood Flow, Charles Hogue
M.D., Cerebral Oximetry: Newer Developments and Their Clinical
Impact
Monday, October 13
Problem-Based Learning Discussions | L098
Carotid Endarterectomy: Asleep Versus Awake
7:15-8:30 a.m. | Room 343-345
Jeffrey Dobyns D.O.
Refresher Course Lecture | 305
Synthetic Colloids in Cardiac Surgery, What Are the Indications?
8-9 a.m. | Room 260-262
Roman Sniecinski M.D.
The role of colloids in cardiac surgery has been debated for
decades. This lecture will review some of the basic theoretical
principles behind the idea of colloids. Additionally, the session will
provide an update of large scale clinical trials and how they may or
may not relate to cardiac surgical patients.
Hands-on Workshop | 822
Intermediate Transesophageal Echocardiography (TEE)
8-11 a.m. | Room 338-339
James Abernathy M.D., M.P.H.
Echo Outside of the Cardiac OR
A case-based, question and answer compilation of sessions
focused on the provider with basic TEE knowledge and designed
to extend that knowledge into more complicated echocardiography
concepts and introduce the participant to three dimensional
echocardiography. Alan Finley M.D., Aortic Valve: When the Area
and Gradient Don’t Agree, Danny Muehlschlegel M.D. The Basics of
3D. What to Do in the OR. (But Doug, the Pictures Are Amazing),
Douglas Shook M.D., Mitral Valve Evaluation: There Is Value in 2D
(Muehlschlegel, None of That 3D Stuff Matters), Nikolas Skubas
M.D., Left Ventricle: Quantitating Function, Can Strain and Strain
Rate Help?, Annemarie Thompson M.D., Diastology. Is There a
Practical Side?
Refresher Course Lecture | 310
Cerebral Protection During Cardiac Surgery
9:15-10:15 a.m. | Room E-3
Charles Hogue M.D.
In this lecture the basic mechanisms of brain injury will be
reviewed as well as approaches to reduce and/or limit the extent
of brain injury during cardiac surgery.
Refresher Course Lecture | 315
Preconditioning the Heart: How It Works and Does It Matter?
12:30-1:30 p.m. | Room E-3
Judy Kersten M.D.
This lecture will review basic mechanisms of pre- and post-
conditioning and remote preconditioning of the heart against
ischemic injury and examine the efcacy of anesthetics for clinical
cardioprotection in cardiac and non-cardiac surgery.
EDUCATION

57
90 Minute Panel | PN67
Understanding the Role of Anemia on Patient Outcomes: An
Innocent Bystander?
1-2:30 p.m. | Room 208-210
Colleen Koch M.D., M.S., M.B.A.
A Hazard of Hospitalization: Prevalence and Outcomes with
Hospital-Acquired Anemia
The panel will provide the attendee with a better understanding of
the role of anemia on perioperative outcomes. It will update the
attendee on current research related to biomarker identication
to better inform when the lower thresholds of tolerable anemia
are reached. The attendee will become aware of the prevalence
of hospital-acquired anemia, their role in mitigating it and its
inuence on patient outcomes. Finally, the attendee will learn how
to treat preoperative anemia and become aware of complications
associated with perioperative treatment strategies. Greg Hare M.D.,
How Low Can You Go? Biomarkers and Hemoglobin Concentrations,
Aryeh Shander M.D., It Takes a Village: Treatment of Anemia in the
Perioperative Setting
Poster Presentations | PO04-3
Clinical Circulation: Physiology/Pharmacology
1-3 p.m. | Hall B1-Area E
Poster Presentations | PO09-1
Experimental Circulation
1-3 p.m. | Hall B1-Area C
Hands-on Workshop | 827
Advanced TEE Workshop
1-4 p.m. | Room 338-339
Sajid Shahul M.D., MPH
This session will focus on the use of advanced echocardiography
to help guide intraoperative diagnosis and decision making.
Albert Cheung M.D., Intraoperative Considerations for Ischemic
MR, Kathryn Glas M.D., Epicardial Echocardiography - Windows
and Intraop Applications, Gregg Hartman M.D., Interesting and
Challenging Cases, Jack Shanewise M.D., Assessment of LV Systolic
Function, Stanton Shernan M.D., Echocardiography to Guide Mitral
Valve Repair
Point-Counterpoint | PC13
Current Controversies in Cardiac Anesthesia
3-4:30 p.m. | Room 211-213
Gregory Janelle M.D., F.A.S.E.
The session will consist of two 45 minute debates on the topics
as described, with a point/counterpoint pertaining to the ongoing
use of pulmonary arterial catheters as one debate followed by a
point/counterpoint on the issue of echocardiography training and
credentialing for anesthesiologists. Manuel Fontes M.D., CON: The
PA Catheter: Does It Still Have a Pulse?, Martin London M.D., PRO:
The PA Catheter: Does It Still Have a Pulse?, Michael Cahalan M.D.,
PRO: Should Basic TEE Be in the Core Curriculum of Anesthesiology
Residency Training?, Colin Royse M.B.,B.S., CON: Should Basic TEE
Be in the Core Curriculum of Anesthesiology Residency Training?
Problem-Based Learning Discussions | L136
Descending Thoracic Aortic Repair - Spinal Cord Protection
Strategies
3:30-4:45 p.m. | Room 343-345
Harendra Arora M.D.
90 Minute Panel | PN75
Guidelines for Blood Management - What Do They Tell Us?
3:30-5 p.m. | Room 217-219
C. David Mazer M.D.
This forum will explore topics relating to cardiac anesthesia and
patient blood management . Topics will include, but not be limited
to, guidelines and regulations for patient blood management,
and perioperative management of platelet inhibitors and use of
factor concentrates. Aryeh Shander M.D., FCCM, Regulating Patient
Blood Management - Who Does it? And Does it Work?, Mark Ereth
M.D., Guidelines for Blood Management - What Do They Tell Us?,
Jerrold Levy M.D., Platelet Inhibitors - When Is It Safe to Operate?
C. David Mazer M.D., Factor Concentrates - What Is Their Place in
Perioperative Bleeding?
Refresher Course Lecture | 334
Heparin Sensitivity and Resistance: Management During
Cardiopulmonary Bypass
4:15-5:15 p.m. | Room 260-262
Alan Finley M.D.
This Refresher Course Lecture will provide an overview of the
pathophysiology and management of heparin resistance during
cardiopulmonary bypass.
Tuesday, October 14
Subspecialty Panels | 609
(SCA) Cardiac Anesthesia
7-8:15 a.m. | Room 231-232
Colleen Koch M.D., M.S., M.B.A.
The SCA Subspecialty panel will review the Top 10 things to know
how to optimally manage patients with mechanical circulatory
support who are undergoing non-cardiac surgical procedures. The
second half of the panel will review current trends in biomarkers
and their role in predicting perioperative outcomes. Adam Evans
M.D., M.B.A., Mechanical Circulatory Support: Top 10 Things to
Know for Optimal Management in the Non-cardiac Surgery Patient,
Amanda Fox M.D., Understanding the Role of Biomarkers: Can They
Predict Perioperative Outcomes?
Refresher Course Lecture | 405
The Pulmonary Artery Catheter in 2014: Past, Present, and Is
There a Future?
8-9 a.m. | Room 260-262
Jonathan Mark M.D.
This lecture will review and recommend methods to improve the
safety of pulmonary artery catheterization; describe the critical
technical details and physical principles that must be considered
to measure PAP accurately; provide examples of normal and
abnormal PAP waveforms; review the current evidence for safety
and efcacy of pulmonary artery catheter monitoring; and consider
challenges for future use of pulmonary artery catheter monitoring.
Point-Counterpoint | PC14
Volatile Anesthetics for Cardioprotection: Is Preconditioning a
Bust?
8-9:30 a.m. | Room 203-205
Stefan De Hert M.D.
Two experts in cardiac anesthesia will debate the evidence that
supports or refutes the use of volatile anesthetics to protect
myocardium against ischemia and reperfusion injury in patients
undergoing cardiac or non-cardiac surgery. Paul Barash M.D., PRO:
Volatile Anesthetics Are Useful for Clinical Cardioprotection, Martin
London M.D., CON: Volatile Anesthetics Are Not Effective for Clinical
Cardioprotection
SCHEDULE BY LEARNING TRACK
58
Poster Presentations | PO09-2
Experimental Circulation
8-10 a.m. | Hall B1-Area C
Hands-on Workshop | 833A, 833B
Thoracic Anesthesia Workshop
8-11 a.m. | Room 356-357
1-4 p.m. | Room 356-357
Edmond Cohen M.D.
The workshop will consist of hands-on demonstration of various
stations equipped with beroptic bronchoscope, video cameras,
mannequins, lung models, double lumen tubes, endobronchial
blockers, and tube exchangers. In addition an adult and a pediatric
simulators will be available for management of crises during
thoracic anesthesia. Finally a torso model would be at used for
the practice of thoracic epidural and paravertebral blocks. Javier
Campos M.D. Levon Capan M.D. Giorgio Della Rocca M.D. Samuel
DeMaria M.D. Cheryl Gooden M.D. Katherine Grichnik M.D., M.S.
Karina Gritsenko M.D. Carin Hagberg M.D. Ingrid Hollinger M.D.
Jonathan Leff M.D. Adam Levine M.D. Steven Neustein M.D. Wanda
Popescu M.D. Alan Sim M.D. Peter Slinger M.D. Joyce Wahr M.D.
Charles Watson M.D. Menachem Weiner M.D.
Refresher Course Lecture | 410
Patient Safety in the Cardiac Operating Room: What Can, Will and
Might Make Patients Safer and You Happier
9:15-10:15 a.m. | Room E-3
James Abernathy, III, M.D., M.P.H.
This refresher course lecture will describe the science of system
analysis, review proven tools and interventions to make care
delivery in operating rooms safer, and discuss future reseach
directions.
Problem-Based Learning Discussions | L161
Descending Thoracic Aortic Repair - Spinal Cord Protection
Strategies
9-10:15 a.m. | Room 343-345
Harendra Arora M.D.
Poster Discussions | PD04-1
Clinical Circulation: Echo
10-11:30 a.m. | Room 243
Refresher Course Lecture | 418
TEE for the Occasional Cardiac Anesthesiologist
11:45-12:45 p.m. | La Nouvelle Ballroom AB
Michael Cahalan M.D.
This Refresher Course will provide a summary of the literature
supporting the crucial role of transesophageal echocardiography
(TEE) in improving the management and outcome of patients
undergoing cardiac surgery as well as a highly efcient basic TEE
examination that is practical to employ by the occasional cardiac
anesthesiologist.
Problem-Based Learning Discussions | L180
Patient With a Failing Fontan for Emergency Exploratory
Laparotomy
12:30-1:45 p.m. | Room 343-345
Galina Leyvi M.D.
Refresher Course Lecture | 422
Massive Post-Cardiopulmonary Hemorrhage: A Rational Approach
to Management
1-2 p.m. | Room E-3
Edwin Avery, IV M.D.
This refresher course lecture aids clinicians in identifying patients
at risk for massive cardiopulmonary bypass hemorrhage and
provides a rational management strategy for those presenting
with this clinical scenario by drawing upon the most up to date
evidence based medicine. This presentation includes discussion/
recommendations of a number of clinical adjuncts to permit
successful treatment of massive bypass related hemorrhage that
include the following: central laboratory and point of care testing
based transfusion guidelines, massive transfusion protocol, use
of blood conservation strategies and integration of pharmacologic
blood conservation/hemostatic agents.
Oral Presentations | OR09-2
Experimental Circulation
1-2:30 p.m. | Room 244
120 Minute Panel | PN28
Percutaneous Approaches to Aortic and Mitral Pathology
1-3 p.m. | Room 225-227
Michael Fitzsimons M.D.
Transcatheter Valve Replacement (TAVR) is an alternative to
surgical treatment of disease of the aortic valve. Percutaneous
management of mitral regurgitation with a clip applied to both
leaets is associated with an improvement in symptoms with
fewer complications such as hemorrhage and stroke while avoiding
bypass. These technologies will soon be a viable alternative
to sternotomy and bypass in lower-risk patients. Program
development requires a multidisciplinary approach. These cases
are performed in a either a hybrid operating room or often out of
the operating room in the cardiac catheterization suite. TEE is
utilized for annular size, prosthesis positioning, and assessment
of complications. Critical decisions are necessary at a time
of signicant hemodynamic instability. We propose a panel to
address key topics to assist anesthesiologists in the development
of a safe, transcatheter valve program. Yianni Augoustides M.D.
Transcatheter versus Surgical Aortic Valve Replacement? A Review
of the Studies Jorg Ender M.D. Percutaneous Approaches to the
Mitral Valve MaryBeth Brady M.D. Anesthetic Management for
Percutaneous Aortic Valve Replacement and Mitral Valve Clipping
Annemarie Thompson M.D. TEE for Percutansour Aortic Valve
Replacement and Mitral Clipping
Poster Presentations | PO04-4
Clinical Circulation: Blood/Coagulation
1-3 p.m. | Hall B1-Area D
EDUCATION

59
Refresher Course Lecture | 429
Update on Strategies for Blood Conservation and Hemostasis in
Cardiac Surgery
2:15-3:15 p.m. | Room 260-262
C. David Mazer M.D.
This Refresher Course Lecture will provide an overview of blood
conservation and blood management programs, review new
anticoagulant and hemostatic drugs, and describe strategies for
optimizing perioperative hemostasis and transfusion.
90 Minute Panel | PN92
Perioperative 3D TEE: Innovative Imaging or Just Pretty Pictures?
3:30-5 p.m. | Room 208-210
Stanton Shernan M.D., F.A.H.A., F.A.S.E.
Is 3D TEE More Accurate Compared to 2D TEE for Evaluating Mitral
Valve Disease?
This Panel Session will focus on the utility of 3D TEE in diagnosing
mitral valve disease and ventricular dysfunction, as well as it
role in facilitating clinical decision-making during cardiac surgery
involving these pathologies and during interventional procedures
in the cardiac catheterization laboratory. Technical and cognitive
limitations and considerations of 3D TEE will also be reviewed.
Nikolaos Skubas M.D., Is 3D TEE Advantageous for Evaluating
Ventricular Function? Madhav Swaminathan M.D. Technical and
Cognitive Limitations of 3D TEE Douglas Shook M.D. Applications of
Interventional 3D TEE in the Cardiac Catheterization Lab
Wednesday, October 15
Refresher Course Lecture | 502
Postoperative Acute Kidney Injury in Cardiac Surgery
8-9 a.m. | Room E-2
Madhav Swaminathan M.D.
Post cardiac-surgery acute kidney injury (AKI) is a serious and
common complication that is strongly associated with short- and
long-term mortality and resource utilization. It’s incidence has been
increasing and preventive efforts have largely proved futile. New
initiatives in this area involve improved risk stratication and early
detection. Early renal recovery may modify adverse outcome and is
considered an important therapeutic target.
90 Minute Panel | PN100
Protecting the Lung During Cardiac Surgery: An Interdisciplinary
Approach
8-9:30 a.m. | Room 208-210
Eric Nelson D.O.
This panel will discuss how to best assess a patient’s preoperative
pulmonary status for cardiac surgery, how to best manage these
patients and protect the lungs during cardiac surgery, and the
safest way to transport these patients to the intensive care unit
and manage their pulmonary status in the postoperative period.
Peter Slinger M.D. Preoperative Risk Stratication William Bradford
M.D. Lung Protection During CPB, How to Best Manage It Anthony
De La Cruz M.D. Transporting and Postoperative Ventilation
Strategies
SCHEDULE BY LEARNING TRACK
60
Critical Care
Saturday, October 11
Problem-Based Learning Discussions | L005
Surviving Septic Shock in the Operating Room and Beyond: What
Do the Guidelines Say?
7:15-8:30 a.m. | Room 343-345
Roman Dudaryk M.D.
Refresher Course Lecture | 101
Sepsis Current Concepts, Guidelines and Perioperative Management
8-9 a.m. | RiverGate
Mark Nunnally M.D., FCCM
This refresher course lecture will review the epidemiology, natural
history and current understanding of the pathophysiology of
sepsis. Perioperative care strategies for patients with severe
sepsis, including newly released guideline recommendations, will
be critically evaluated.
Point-Counterpoint | PC02
We Give Too Much Fluid in the OR
8-9:30 a.m. | Room 211-213
Ozan Akca M.D. PRO
This pro-con debate will focus on the clinical controversy regarding
uid management for high risk perioperative care. Using evidence
and clinical experience, panelists will debate the contention that
current uid management strategies result in too much uid being
given in the perioperative period. Brian Kavanagh M.B. CON
Poster Presentations | PO06-4
Critical Care
8-10 a.m. | Hall B1-Area B
Refresher Course Lecture | 108
Pulmonary Hypertension and Right Ventricular Failure
9:15-10:15 a.m. | Room E-1
Eric Jacobsohn M.B.,Ch.B.
This lecture will review the epidemiology and pathophysiology of
pulmonary hypertension. Anesthetic considerations for patients
with pulmonary hypertension and right ventricular dysfunction will
be reviewed. Principals of monitoring for pulmonary hypertension
will also be reviewed.
Problem-Based Learning Discussions | L027
Elderly Man; Going into Shock; Needs Fluids Now!
12:30-1:45 p.m. | Room 343-345
Elizabeth Frost M.B.,Ch.B.
Oral Presentations | OR06-1
Critical Care | 1-2:30 p.m.
Room 243
Point-Counterpoint | PC03
Tidal Volumes Don’t Really Matter to the Anesthesiologist
1-2:30 p.m. | Room 203-205
James Blum M.D. PRO
This session will review sources of variability regarding ventilator
modes and settings in the OR, debate the quality and adequacy
of clinical evidence regarding specic ventilator settings in
the operating room, discuss optimal blood gas values for
intraoperative mechanical ventilation, and debate the argument
that guidelines for intraoperative mechanical ventilation will
improve perioperative care. Daniel Talmor M.D., M.P.H.CON
90 Minute Panel | PN42
Red Blood Cells: Good, Bad, and Ugly and Some Solutions
1-2:30 p.m. | Room 217-219
Jonathan Jahr M.D.
Solutions (including Blood Substitutes)
This panel will: list the challenges of mobilizing blood for
catastrophies and categorize strategies for availability and
transfusing blood to victims of catastrophies, discuss issues with
aged blood and learn what evidence based medicine provides
as guidance for use of aged versus fresh blood, list methods
to formulate blood substitutes and types currently available
and under testing; evaluate progress of rst, second, and third
generation Hemoglobin-based Oxygen Carriers; discuss clinical
use of blood substitutes in animals and in humans in South
Africa and Russia. It will have three lectures: Mobilizing blood for
catastrophes--natural and man-made--Corey Scher. How bad is
aged blood? Colleen Koch, Solutions (including blood substitutes)-
Jonathan Jahr Colleen Koch M.D., M.S. How Bad Is Aged Blood?
Corey Scher, M.D. “Mobilizing Blood for Catastrophes - Natural and
Man-Made”
Refresher Course Lecture | 226
Heart Failure and Perioperative Care
1:45-2:45 p.m. | Room E-3
Gareth Ackland M.D.
This refresher course will focus on the relevance and impact
of congestive heart failure on perioperative outcomes. Topics
will include preoperative assessment, risk stratication, and
optimization, intraoperative management, and postoperative care.
Refresher Course Lecture | 119
Mechanical Ventilatory Support: What Every Anesthesiologist
Should Know
2:45-3:45 p.m. | Room E-3
Michael Gropper M.D., Ph.D.
This refresher course lecture will describe the rationale for the
modern approach to mechanical ventilation. Topics reviewed will
include causes and mechanisms of ventilator-induced lung injury,
the physiological basis for current and new modes of mechanical
ventilation, strategies for avoiding complications of mechanical
ventilation, and approaches to difcult perioperative ventilation
scenarios.
Point-Counterpoint | PC04
Do We Really Need Risk Adjustment to Measure Outcomes?
3:30-5 p.m. | Room 203-205
Avery Tung M.D.
CON: Risk Adjustment Creates More Problems Than It Solves
This pro-con will examine the use of risk adjustment for outcome
measurement in perioperative care. Using a pro/con format, the
session will describe the theoretical basis for risk adjustment and
current risk adjustment methodologies. Current implementations
of risk adjustment in surgical care, implications for anesthesia
quality, and unintended consequences will also be discussed.
Laurent Glance M.D. PRO: Outcomes Are Meaningless Without Risk
Adjustment
EDUCATION

61
90 Minute Panel | PN45
Optimizing Perioperative Hepatic Function
3:30-5 p.m. | Room 220-222
Randolph Steadman M.D., M.S.
Postoperative Optimization and Rescue
This panel will focus on perioperative management of patients
undergoing hepatic surgery or with hepatic disease by emphasizing
a complete perioperative surgical home approach. Topics will
include preoperative risk assessment, risk stratication, and
medical optimization, intraoperative management including
coagulation and hemodynamic strategies, and postoperative
optimization and rescue. James Findlay M.B.,Ch.B.
Intraoperative Management and Optimization Geraldine Diaz M.D.
Preoperative Risk Stratication and Optimization
Refresher Course Lecture | 124
Transfusion Therapy: Optimal Use of Blood Products
4-5 p.m. | Room E-2
Stephen Surgenor M.B.A., M.D.
This refresher course will review the indications, risks, and
benets of transfusion therapy including red blood cells, plasma,
platelets, and derivatives. In addition, a review of emerging risks of
transfusion therapy and the approach to massive transfusion will
be presented.
Sunday, October 12
Subspecialty Panels | 604
(SOCCA) Trauma and Critical Care Pearls for the Non-Intensivists
7-8:15 a.m. | Room 231-232
Daniel Brown M.D., Ph.D.
An interactive case-based discussion focused on management
of the trauma patient presenting for surgery. Assessment and
management options for securing a denitive airway in the setting
of an existing supraglotic airway will be discussed. As the intra
operative course unfolds, current evidence for management of
trauma-related coagulopathy will be reviewed. Finally, emergent
evaluation of increased airway pressures will be discussed,
including the utility of ultrasound. Daniel Diedrich M.D. Thomas
Grissom M.D.
Refresher Course Lecture | 202
Respiratory Physiology and Perioperative Gas Exchange
8-9 a.m. | Room E-1
Luca Bigatello M.D.
This refresher course lecture will review basic respiratory
physiology including the physiology of normal and abnormal gas
exchange. Topics include diagnostic and therapeutic approaches to
patients with abnormal gas exchange in the perioperative setting,
strategies for managing hypoxia and hypercarbia, management
of acute vs. chronic hypercarbia, and mechanical ventilation
strategies for patients with abnormal gas exchange.
90 Minute Panel | PN52
Simulation Education in Competency-Based Training and
Assessment: Present and Future
8-9:30 a.m. | Room 220-222
Randall Schell M.D., M.Ed.
This panel will discuss the use of simulation training and
assessment in competency-based education in the Milestones
and MOCA era. The rst presenter will review the requirements
for simulation training and testing by the ACGME how simulation
assessment can be used within the Milestones system. The
second presenter will discuss the use of simulation training and
assessment in the ABA initial certication and MOCA system. The
third presenter will discuss the future of simulation training and
assessment in for certication in courses such as anesthesia-
centric ACLS and other related areas. Matthew McEvoy M.D.
Simulation Training and Assessment in the Milestones Era Arna
Banerjee M.B.,B.S. ABA Certication, MOCA, and Simulation Mark
Nunnally M.D., FCCM Future Certications via Simulation Training
and Assessment
Seminar | 813
Perioperative Resuscitation - What’s New?
8-11 a.m. | Room 348-349
Steven Robicsek M.D., Ph.D.
Perioperative resuscitation offers a unique challenge to the
practitioner - in etiology, resources and available personnel. The
term Anesthesia Advanced Circulatory Life Support (A-ACLS) was
introduced in 2008 to describe unique circumstances that may
present. This workshop will consist of an overview lecture followed
by simulation-based adult arrest scenarios that are commonly
encountered in the perioperative setting (block room, OR, PACU,
ICU). A current review of the AHA BLS and ACLS guidelines are
encouraged prior to the workshop and will be discussed during
simulations. The workshop is intended as a supplement to the
AHA BLS and ACLS concepts and algorithms. Gregory Janelle M.D.
Utility of a Focused ECHO Examination Lawrence Caruso M.D.
Elizabeth Mahanna M.D. Steven Venticinque M.D. Melissa Vu M.D.
Lisa Warren M.D.
Problem-Based Learning Discussions | L062
Surviving Septic Shock in the Operating Room and Beyond: What
Do the Guidelines Say?
9-10:15 a.m. | Room 343-345
Roman Dudaryk M.D.
Poster Presentations | PO06-1
Critical Care
10 a.m.-12 p.m. | Hall B1-Area D
Refresher Course Lecture | 218
The Evidence Behind Evidence-Based Medicine
10:30-11:30 a.m. | La Nouvelle Ballroom AB
Brian Kavanagh M.B.
This refresher course lecture will examine the use of literature-
based evidence to guide clinical decisions, present and discuss
evidence supporting and refuting use of evidence-based guidelines
for clinical care, identify pitfalls and challenges in guideline
creation, and suggest strategies for using literature-based
evidence to improve outcomes.
Problem-Based Learning Discussions | L084
Management of Acute Pulmonary Embolism: Anticipating and
Responding to Complexity
12:30-1:45 p.m. | Room 343-345
Ahmed Zaky M.D.
SCHEDULE BY LEARNING TRACK
62
Point-Counterpoint | PC09
A Structured Handoff Protocol Improves the Care of Patients Going
to the ICU After Surgery
1-2:30 p.m. | Room 203-205
Steven Greenberg M.D. PRO
This pro-con will examine challenges in patient safety that occur
during handoff of a critically ill patient to an ICU service, discuss
the concept and implementation of a structured handoff protocol,
and review the evidence for and against the argument that a
structured handoff protocol reduces errors and improves patient
safety. Michael O’Connor M.D., FCCM CON
120 Minute Panel | PN10
Minimizing Postoperative ICU Complications in a Surgical Home
1-3 p.m. | Room 217-219
Trung Vu M.D.
This panel will focus on the postoperative management of high-risk
surgical patients in the intensive care units (ICU). Postoperative
complications in the ICUs are often unrelated to the surgical
procedures. Postoperative cardiac failure, respiratory failure,
and neurological dysfunction particularly delirium are a function
of the patient’s co-morbidity going into surgery. The critical care
anesthesiologists providing care for these high-risk postoperative
patients are in a unique position to lead the perioperative surgical
home. The critical care anesthesiologists can identify the high-
risk patients, perform preoperative risk stratication, and develop
clinical pathways to optimize these patients preoperatively and to
standardize intraoperative strategies to minimize postoperative
complications in the intensive care unit. William Wilson M.D.
Clinical Pathways for High-Risk Patients in Surgical Home Antonio
Hernandez M.D. Preventing Delirium: A Surgical Home Perspective
Philip Lumb M.D. Evidence-based Intraoperative Strategies to
Reduce Postoperative Complications
Problem-Based Learning Discussions | L087
Transfusion Goals and Hemostatic Management of the
Anticoagulated Trauma Patient: Can You Plug a Hole in the Dam?
3:30-4:45 p.m. | Room 343-345
Louanne Carabini M.D.
Problem-Based Learning Discussions | L089
Elderly Man; Going into Shock; Needs Fluids Now!
3:30-4:45 p.m. | Room 343-345
Elizabeth Frost M.B.,Ch.B.
90 Minute Panel | PN62
ACLs for the Anesthesiologist: An Update
3:30-5 p.m. | Room 220-222
Vivek Moitra M.D.
This panel will review important changes in the most recent
revision of ACLS, and their application in the perioperative setting
(AACLS). Aspects of successful ACLS including team training and
crew resource management, and considerations unique to the
obstetric and pediatric patient will be reviewed. Kyle Harrison M.D.
Optimizing AACLS: Simulation and Cognitive Aids Sharon Einav M.D.
Matthew McEvoy M.D.
Refresher Course Lecture | 230
Perioperative Coagulation and Coagulopathy
3-4 p.m. Room E-1
Linda Liu M.D.
This refresher course will review the physiology of normal and
abnormal coagulation in the perioperative period, discuss agents
used to modulate coagulation and their clinical uses, and propose
an algorithm to manage coagulopathic patients.
Refresher Course Lecture | 239
Understanding Clinical Hemodynamics
4:15-5:15 p.m. | Room 260-262
Jeffery Vender M.D., FCCM
The evaluation and management of patients with shock remains a
challenge for perioperative physicians. This lecture will review the
Guyton and Starling models of the circulation and their interaction
in patients with different types of shock. It will also review
current strategies for hemodynamic monitoring, including pulse
pressure variation, central venous oxygenation, and central venous
pressure. It will also review modern concepts of oxygen delivery.
Monday, October 13
Problem-Based Learning Discussions | L109
Management of Acute Pulmonary Embolism: Anticipating and
Responding to Complexity
7:15-8:30 a.m. | Room 343-345
Ahmed Zaky M.D.
Clinical Forum | CF09
Critical Care Forum: Challenges and Controversies in Critical Care
Anesthesiology
8-9:30 a.m. | Room 206-207
Avery Tung M.D., FCCM
This interactive, case-based session will use audience response
technology, literature review, and expert opinion to explore
controversial topics in high risk perioperative care. Topics will
include (but not be limited to) preoperative risk assessment
and decision making, intraoperative management, monitoring
of unstable cardiorespiratory states, atypical physiology, and
postoperative care. Christopher Choukalas M.D., M.S. William
Hurford M.D.
Point-Counterpoint | PC10
Should We Perform CPR When We Know That It Is Futile?
8-9:30 a.m. | Room 211-213
Neal Cohen M.D., M.P.H., M.S.
In general, it is regarded as inappropriate to perform CPR and
other components of ACLS when the expected outcome will not
be improved. Arguments have been made in favor of providing
this intervention nonetheless, on the basis of the peace of mind
benet to families and/or surrogate decision-makers who wish
everything to be done. The point-counterpoint will address the
relative merits of each viewpoint. Nicholas Sadovnikoff M.D.
PRO: Performing CPR in Futile Scenarios Provides a Benet to
Families and Surrogates Who Want to Believe “Everything was
Done” Michael Nurok M.B.,Ch.B., Ph.D. CON: Performing CPR in
Futile Scenarios is Misleading and Dishonest and Should not be
Done no Matter What
120 Minute Panel | PN18
Perioperative Hemodynamic Optimization and Goal Directed
Therapy
8-10 a.m. | Room 217-219
Jeffery Vender M.D., FCCM
This panel will review and discuss the current state of the art in
perioperative goal-directed therapy. Topics will include (but not
be limited to) monitoring strategies and appropriate endpoints to
optimization, uid management, and use of blood, inotropes, and
pressors to achieve predened goals. Application to real world
cases will be discussed. Gary Haynes M.D., Ph.D. Andrew Leibowitz
M.D. Steven Greenberg
EDUCATION

63
Hands-on Workshop | 825
Critical Care Ultrasonography for the Perioperative Physician
8-11 a.m. | Room 356-357
Steven Venticinque M.D.
This hands-on workshop will introduce participants to the use of
surfaceultrasound in perioperative medicine with a focus on acute
hemodynamic and pulmonary assessment. Topics will include
basic transthoracic cardiacevaluation including the estimation
of intravascular volume, ventricularfunction, and an evaluation of
the pleural and pericardial space. The use and utility of surface
ultrasound in the anesthesia-ACLS setting will be discussed.
Participants will develop basic ultrasound skills on live models and
simulators using current imaging systems. Learning will take place
through didactic instruction and mentored, hands-on experience.
The session will include a review of multiple normal and abnormal
ultrasound ndings. Larry Field M.D. Sean Kiley M.D. Michael
Kopec M.D. Robina Matyal M.D. Joseph Meltzer M.D. James Osorio
M.D. Oliver Panzer M.D. Albert Perrino M.D. Ketan Shevde M.D.
Chad Wagner M.D. Troy Wildes M.D.
Hands-on Workshop | 819A, 819B
Perioperative ACLS Simulation Workshop
8-11:30 a.m. | Room 281
1-4:30 p.m. | Room 281
Matthew McEvoy M.D.
This simulation workshop will focus on Perioperative (Anesthesia-
Centric) ACLS which addresses content related to perioperative
urgencies: emergencies of cardiac, pulmonary, neurologic,
metabolic/endocrine, and toxin origin. The workshop will begin
with a 45-minute didactic and Q&A session. The simulation
sessions will follow with each scenario being 15 minutes long with
a 25 to 30-minute debrief afterward that will take into account the
workshop objectives. A 5-minute break will be given between each
station. There will be 4 scenarios-stations per workshop with each
station covering a different perioperative emergency. There will
be a team leader and a rst responder at each station. The other
participants will ll scripted roles to which they will be introduced
(nurse, surgeon, tech, etc) and one participant will play the
observer role in order to give feedback to the team along with the
facilitator. Arna Banerjee M.B.,B.S. Amanda Burden M.D. Larry Field
M.D. Cory Furse M.D. William Hand M.D. Vivek Moitra M.D. Mark
Nunnally M.D., FCCM Catherine Tobin M.D.
Problem-Based Learning Discussions | L117
Management of Severe ARDS in the ICU With ECMO
9-10:15 a.m. | Room 343-345
Jacob Gutsche M.D.
Refresher Course Lecture | 313
(A)ACLS in the Perioperative Period
12:30-1:30 p.m. | Room E-1
Gerald Maccioli M.D.
This refresher course will summarize updates and important
changes to ACLS in 2014. It will review differences between ACLS
in the outpatient and emergency setting and perioperative ACLS
including causes of cardiac arrest and relevant resuscitation
strategies. Adaptations of ACLS algorithms for the perioperative
setting will be presented and discussed.
90 Minute Panel | PN68
Quality Improvement in Critical Care
1-2:30 p.m. | Room 217-219
Gregory Botz M.D.
A Systems Approach
This session will discuss evolving, state of the art strategies for
improving ICU care quality. Topics will include multidisciplinary and
organizational approaches, innovative uses of EMR technology to
drive quality care, and novel strategies for the ICU of the future.
Matthias Merkel M.D., Ph.D. Levering the EMR to Drive Quality
Michael Gropper M.D., Ph.D. New Approaches to Quality in 2014
and Beyond
Poster Presentations | PO06-2
Critical Care
1-3 p.m. | Hall B1-Area D
Refresher Course Lecture | 323
Controversies and Best Practices in Central Line Insertion
1:45-2:45 p.m. | La Nouvelle Ballroom AB
Avery Tung M.D., FCCM
This refresher course will review the changing epidemiology
of central line use in perioperative and critical care, describe
advantages and drawbacks to recent technical advances in line
insertion and changes in clinical practice, review recent ASA
guidelines on central line insertion, and identify known and
emerging high risk complications of central line placement.
Problem-Based Learning Discussions | L141
Management of Co-Intoxications in the ICU Patient
3:30-4:45 p.m. | Room 343-345
Robert Gould M.D.
90 Minute Panel | PN76
Optimizing Perioperative Pulmonary Function
3:30-5 p.m. | Room 220-222
Steven Lisco M.D.
Postoperative Pulmonary Function
This panel will focus on perioperative management of pulmonary
function by emphasizing a complete perioperative surgical home
approach. Topics will include preoperative risk assessment,
risk stratication, and medical optimization, intraoperative
management including mechanical ventilation and uid strategies,
and postoperative optimization and rescue. Todd Sarge M.D.
Intraoperative Pulmonary Optimization Mark Nunnally M.D., FCCM
Preoperative Risk Stratication and Optimization
Refresher Course Lecture | 330
Perioperative Delirium
4:15-5:15 p.m. | RiverGate
Pratik Pandharipande M.D.
This lecture will outline the epidemiology, clinical features, and
major health impact of delirium in critically ill patients. Risk factors
and preventative measures will be outlined and potential therapies
for agitation and delirium will be discussed.
SCHEDULE BY LEARNING TRACK
64
Tuesday, October 14
Problem-Based Learning Discussions | L152
Transfusion Goals and Hemostatic Management of the
Anticoagulated Trauma Patient: Can You Plug a Hole in the Dam?
7:15-8:30 a.m. | Room 343-345
Louanne Carabini M.D.
Problem-Based Learning Discussions | L154
Management of Co-Intoxications in the ICU Patient
7:15-8:30 a.m. | Room 343-345
Robert Gould M.D.
Hands-on Workshop | 830A, 830B
Perioperative ACLS Simulation Workshop
8-11:30 a.m. | Room 281
1-4:30 p.m. | Room 281
Matthew McEvoy M.D.
This simulation workshop will focus on Perioperative (Anesthesia-
Centric) ACLS which addresses content related to perioperative
urgencies: emergencies of cardiac, pulmonary, neurologic,
metabolic/endocrine, and toxin origin. The workshop will begin
with a 45-minute didactic and Q&A session. The simulation
sessions will follow with each scenario being 15 minutes long with
a 25 to 30-minute debrief afterward that will take into account
the workshop objectives. A 5-minute break will be given between
each station. There will be 4 scenarios-stations per workshop
with each station covering a different perioperative emergency.
There will be a team leader and a rst responder at each station.
The other participants will ll scripted roles to which they will be
introduced (nurse, surgeon, tech, etc) and one participant will play
the observer role in order to give feedback to the team along with
the facilitator. Arna Banerjee M.B.,B.S. Amanda Burden M.D. Larry
Field M.D. Cory Furse M.D. William Hand M.D. Vivek Moitra M.D.
Mark Nunnally M.D., FCCM Catherine Tobin M.D.
Oral Presentations | OR06-2
Critical Care
8-9:30 a.m. | Room 244
Problem-Based Learning Discussions | L164
Management of Severe ARDS in the ICU With ECMO
9-10:15 a.m. | Room 343-345
Jacob Gutsche M.D.
Point-Counterpoint | PC16
Can Post-Operative Delirium Really Be Managed?
10-11:30 a.m. | Room 203-205
Pratik Pandharipande M.D. PRO, William Hurford M.D. CON
This pro-con debate will focus on the risk factors for, and
management of, perioperative delirium. Whether postoperative
delirium can be effectively managed will be the focus of this
debate.
90 Minute Panel | PN87
Fluid Administration During the Perioperative Period: Does It Make
a Difference What, and How Much, You Give?
10-11:30 a.m. | Room 208-210
Matthias Jacob M.D., PhD.
This panel will examine uid administration during the Peri-
Operative period. Patient outcomes associated with type of
crystalloid administered will be reviewed. The role of colloid
administration will also be appraised. Recommendations for
resuscitation endpoints in different clinical scenarios will be
discussed. Steven Greenberg M.D. Sheela Pai M.D.
Poster Presentations | PO06-3
Critical Care
10 a.m.-12 p.m. | Hall B1-Area D
90 Minute Panel | PN91
The Evolving Goals of the ICU: Critical Care, Palliative Care, or
Patient-Centered Care
1-2:30 p.m. | Room 217-219
Neal Cohen M.D., M.P.H., M.S.
Palliative care is a new and rapidly growing medical specialty that
emphasizes aggressive symptom management, psychosocial
support of patients and families, and thoughtful clarication
about a patient’s unique hopes, goals and fears regarding his/
her medical care. This session will review the history of the
interaction between palliative care and critical care, dene patient
centered care and discuss current trends in integrating palliative
and critical care, and provide evidence-based approaches for better
provision of palliative care in the ICU. Rebecca Aslakson M.D.,
Ph.D. Palliative Care to Improve Care in the ICU or as an Alternative
to the ICU Allen Gustin M.D. Palliative Care to Improve Care in the
ICU or as an Alternative to the ICU
Point-Counterpoint | PC20
Electronic Health Records Improve Patient Safety – or Do They?
3-4:30 p.m. | Room 203-205
David Feinstein M.D.
This session will explore the impact of electronic health record
use on patient safety and quality of care. s examine how clinical
pathways and decision support derived from electronic health
records impact patient outcomes and measures of safety.
Limitations and potential problems with electronic medical records
will be identied. James Moore M.D. PRO: Electronic Health
Records Improve Patient Safety and Quality of Care Christine Doyle
M.D. CON: Electronic Health Records Increase Errors in Patient Care
and Harm Patients
Poster Discussions | PD06-1
Critical Care
3-4:30 p.m. | Room 243
90 Minute Panel | PN94
Optimizing Perioperative Renal Function
3:30-5 p.m. | Room 220-222
Robert Sladen M.B.,Ch.B., FCCM
Postoperative Managment and Rescue
This panel will focus on perioperative management of patients with
renal disease by emphasizing a complete perioperative surgical
home approach. Topics will include preoperative risk assessment,
risk stratication, and medical optimization, intraoperative
management including uid, inotrope, and hemodynamic
strategies, and postoperative optimization and rescue. Anthony A.
De La Cruz, M.D., Preop Risk Stratication and Optimization Patrick
Neligan M.B., B.Ch. Intraoperative Management: Does Anything
Really Matter?
120 Minute Panel | PN33
Anesthesia for the Patient Too Sick for Anesthesia
3:30-5:30 p.m. | Room 252-254
Daniel Brown M.D., Ph.D.
This session will focus on perioperative management of patients
with advanced end organ disease. A single case-based discussion
format will be used to address diastolic heart failure, advanced
cirrhosis, rhabdomyolysis-induced kidney injury, and nonketotic
hyperosmolar coma. Case stem: A 58-year-old end-stage alcoholic
man is found down at home. He will need emergent fasciotomies.
Zdravka Zarova M.D. Matthew Hallman M.D. Frederic Billings
M.D.
EDUCATION

65
Wednesday, October 15
Refresher Course Lecture | 501
Emergent Airway Management: Tips, Tricks, and Evidence
8-9 a.m. | Room E-1
Aaron Joffe D.O.
This refresher course lecture will review current concepts in
emergent airway management and discuss approaches to
these challenges including alternate intubation technologies,
awake strategies, drug choices, abnormal gas exchange, and
hemodynamic instability. This course will also review challenges in
difcult extubation, including cuff leak marginal respiratory reserve,
and postextubation BiPAP.
90 Minute Panel | PN98
FFP: A Critical Appraisal in 2014
8-9:30 a.m. | Room 217-219
Aryeh Shander M.D.
Physiology and Current Use
This panel will examine the current clinical use of Fresh Frozen
Plasma to treat perioperative coagulopathic states, evaluate and
explore current evidence regarding the effectiveness of FFP for this
purpose, and identify potential evidence-based alternatives to FFP.
Aryeh Shander, M.D. Physiology and Current Use Sibylle Kozek M.D.,
M.B.A. Does It Work?
Refresher Course Lecture | 504
Perioperative Renal Protection
9:15-10:15 a.m. | Room E-1
Michael Hutchens M.D.
This lecture will review the classication and pathophysiology of
acute kidney injury (AKI), the epidemiology and pathophysiology
of perioperative renal dysfunction; and evidence for perioperative
interventions to prevent or ameliorate AKI.
SCHEDULE BY LEARNING TRACK
66
Fundamentals of Anesthesiology
Saturday, October 11
Problem-Based Learning Discussions | L011
It’s Only a MAC Case and Now My Patient is on FIRE!
7:15-8:30 a.m. | Room 343-345
Mark Phillips M.D.
Problem-Based Learning Discussions | L157
The Unanticipated Difcult Airway: A Dynamic and Dangerous
Scenario
7:15-8:30 a.m. | Room 343-345
Lavinia Kolarczyk M.D.
Refresher Course Lecture | 103
Arterial Blood-Gas Analysis: Interpretation and Application
8-9:00 a.m. | Room E-2
Steven Barker Ph.D., M.D.
The interpretation and application of arterial blood-gas (ABG) data
is a task that anesthesiologists must often perform under difcult
circumstances. In this clinical setting, it is helpful to have a simple
algorithm or check-list, both to ensure consistency and obtain a
correct answer within a short time. The purpose of this talk is
to develop such an algorithm and apply it to clinical examples,
wherein we shall interpret both oxygenation and acid-base status,
and then prescribe appropriate treatment.
Oral Presentations | OR13-1
Outcomes and Database Research - Cardiac Outcomes & Risk
8-9:30 a.m. | Room 243
Oral Presentations | OR17-1
Respiration-Ventilation
8-9:30 a.m. | Room 245
Poster Presentations | PO08-3
Equipment, Monitoring and Engineering Technology: Circulation
8-10 a.m. | Hall B1-Area C
Hands-on Workshop | DW01
Basic/Advanced Flexible Fiberoptic Intubation Workshop
8-10:30 a.m. | Room 353-355
Hands-on Workshop | DW02
10:30 a.m.-1 p.m. | Room 353-355
Hands-on Workshop | DW03
2:30-5 p.m. | Room 353-355
Katherine Gil M.D
Basic to Intermediate to Advanced exible beroptic experience:
an introductory discussion of clear indications, contraindications,
techniques, and complications of scope use. Expert instructors
from at least 6 countries (instructing in multiple languages) to
guide you through exible scope hands-on areas to develop your
skill. Mini discussions on local airway anesthetic and hands-
on equipment, with questions and answers in small groups.
Instructors guide you in combined exible scope use in hands-on
areas, to assist the successful completion of most major airway
devices. Learn to make a cheap, 5-minute dexterity model and
practise with multiple levels of difculty. Experience practising
with computerized systems: Virtual Fiberoptic Intubation and
ORSIM simulator program. Challenge yourself in the human
simulation systems with difcult intubation scenarios and in the
trouble-shooting area. Receive handout checklists for all facets
of beroptic practice and intubation. Gail Randel M.D. David
Wong M.D. Valerie Armstead, M.D. Radha Arunkumar M.B., B.S.
Lauren Berkow M.D. Sylvain Boet M.D., M.Ed. Richard Cooper M.D.
Elifce Cosar M.D. Pierre Diemunsch M.D. Stephen Dierdorf M.D. D.
John Doyle M.D. Ludwik Fedorko M.D., Ph.D. David Feinstein M.D.
Lorraine Foley M.D. Giulio Frova M.D. Katherine Hagan M.D. Grant
Lindsay Hounsell M.D. Ling Qun Hu M.D. Orlando Hung M.D Marshal
Kaplan M.D. Robert Krohner D.O. Vicente Martinez-Pons M.D.,
Ph.D. Maria Matuszczak M.D. Alonso Mesa M.D. Leonid Minkovich
M.D. Michael Murphy M.D. Andrew Roth M.D. Bettina Schmitz
M.D., Ph.D., DEAA Massimilano Sorbello M.D. Francis Stellaccio
M.D. Ljuba Stojiljkovic M.D., Ph.D Adriaan Van Rensburg M.D.
Lakshmikumar Venkat Raghavan M.B.,B.S. Leonard Wade, M.S.
Ashutosh Wali M.D., M.B.,B.S. Marcin Wasowicz M.D. David Wong
M.D. Meltem Yilmaz M.D. Andrew Zura M.D.
Hands-on Workshop | 802
Workshop on Emergency Surgical Airway Management Using a Pig
Trachea Model
8-11 a.m. | Room 278-279
William Rosenblatt M.D.
The ability to perform an invasive airway is an essential skill for all
anesthesiologist. This workshop will focus on the performance of
several percutaneous airway techniques in a unique swine trachea
preparation designed for the ASA and the Society for Airway
Management. After a short didactic session, each participant will
perform all of the following techniques: Translaryngeal aspiration
and needle placement, percutaneous large bore catheter
placement (Seldinger delivery), Percutaneous large bore catheter
placement (puncture delivery), bougie aided laryngeal tracheal tube
placement and a unique blind cricothyrotomy technique developed
for the US military, Cric-key. In addition, a high-pressure oxygen/
mannequin station will be available for the practice of tranlaryngeal
jet oxygenation. Ron Abrons M.D., Ph.D. Jennifer Anderson M.D. D.
John Doyle M.D. Jessica Feinleib M.D., Ph.D. Allan Klock M.D.
Andrew Zura M.D.
EDUCATION

67
Seminar | 805
Statistics for Anesthesiologists
8-11 a.m. | Room 335-336
Jeffrey Gross M.D.
This workshop will include a brief review of statistical terminology
and basic principles of descriptive and inferential statistics.
Some common statistical myths will also be busted during the
presentation. The workshop includes a self-evaluation quiz which
will be reviewed at the end of the session. No mathematical
background is required, and the examples lend themselves to
easy computation. Keith Gipson M.D., Ph.D.
Hands-on Workshop | AW01
Workshop on Flexible Endoscopy for Lung Isolation
9-10:15 a.m. | Room 356-357
Hands-on Workshop | AW02
10:30-11:45 a.m. | Room 356-357
Hands-on Workshop | AW03
12-1:15 p.m. | Room 356-357
Hands-on Workshop | AW04
1:30-2:45 p.m. | Room 356-357
Hands-on Workshop | AW01
3-4:15 p.m. | Room 356-357
Scott Schartel D.O.
The workshop is structured to provide participants with instruction
and practical experience in the use of exible endoscopy for
achieving lung isolation/one lung ventilation. Participants will work
with models of the tracheobronchial tree that allow placement
of endobronchial tubes (right and left) and various types of
bronchial blockers. Flexible video endoscopes connected to video
displays will be used. Participants will be given an opportunity
to learn the endoscopic anatomy of the tracheobronchial tree
to facilitate the correct placement of the various devices. The
workshop is structured in a way that will allow participants to
receive individual attention and work at their own level. The
workshop can accommodate novices seeking basic information
and advanced practitioners seeking answers to more complex
questions. The use of multiple instructors during each workshop
will provide opportunities for participants to experience a variety
of approaches to the same tasks and problems. William Simmons
M.D. Dalia Banks M.D. Kyle Harrison M.D. Jerry Clark M.D. Elizabeth
Drum M.D. Andrew Herlich M.D. Douglas Hester M.D.
Swapnil Khoche M.B., B.S. Jerome Klafta M.D. Timothy Maus M.D.
Sheela Pai M.D. Amy Robertson M.D. Daniel Roke M.D. Michael
Woo M.D.
Problem-Based Learning Discussions | L014
Management of Antiplatelet Therapy in Patients With Coronary
Stents for Noncardiac Surgery
9-10:15 a.m. | Room 343-345
Davide Cattano M.D., Ph.D.
Problem-Based Learning Discussions | L017
Perioperative Laboratory and Cardiac Testing: What Is Necessary?
9-10:15 a.m. | Room 343-345
David Hepner M.D.
Problem-Based Learning Discussions | L019
I Swear It Will Only Take 15 Minutes: Anesthesia/Sedation for TEE/
Cardioversion
9-10:15 a.m. | Room 343-345
Julia Metzner M.D.
Problem-Based Learning Discussions | L022
Perioperative Management of the Anemic Patient
9-10:15 a.m. | Room 343-345
Russell Roberson M.D.
Poster Discussions | PD08-1
Equipment, Monitoring and Engineering Technology: Utilizing
Technology - Imaging and Closed Loop Systems
10-11:30 a.m.| Room 244
Poster Presentations | PO13-3
Outcomes and Database Research
10 a.m.-12 p.m. | Hall B1-Area D
Problem-Based Learning Discussions | L028
A Patient With a Temperature of 102.5 F and Rigors 3 Hours After
Surgery
12:30-1:45 p.m. | Room 343-345
Theresa Gelzinis M.D.
Problem-Based Learning Discussions | L034
My Patients Never Have Residual Paralysis in the PACU, or Do They?
12:30-1:45 p.m. | Room 343-345
Stephan Thilen M.D., M.S.
Poster Presentations | PO08-5
Equipment, Monitoring and Engineering Technology:Ventilation and
Supraglotic Airways
1-3 p.m. | Hall B1-Area B
Refresher Course Lecture | 127
Hospital System Failures and Hazard Management in the Operating
Room
1:30-2:30 p.m. | Room E-1
P. Klock M.D.
This refresher course lecture will provide a generic framework
for responding to hospital system failures during anesthetic
care. Topics include: Failure of the following systems: Electrical,
Communication, Fresh Water, Steam, HVAC, Suction. In addition to
these system failures, oods and res in the operating room will
be covered.
Refresher Course Lecture | 118
Anesthesia for Major Orthopedic Surgery
2:45-3:45 p.m. | Room E-2
Andrew Rosenberg M.D.
This lecture will cover areas and issues involved in major
orthopedic anesthesia including regional anesthesia, spine
surgery, beach chair position, rheumatoid arthritis, and
considerations associated with thromboprophylaxis.
SCHEDULE BY LEARNING TRACK
68
Refresher Course Lecture | 120
Operating Room Fire Safety
2:45-3:45 p.m. | Room 260-262
William Culp M.D.
Operating room res represent a constant threat to patients
undergoing surgery, and occur at least as often as wrong-site
surgery. This problem has received intense attention from the lay
press as well as The Joint Commission and the Anesthesia Patient
Safety Foundation, among others. This presentation will serve to
describe the background of the problem, specically discussing the
conditions necessary for re to occur, and how anesthesiologists
can play a key role in reducing this threat. Recently updated safety
guidelines to prevent res by altering anesthetic technique will
be covered. Finally, new research in the eld will be presented to
provide a better scientic appreciation of the scope of this safety
problem.
Problem-Based Learning Discussions | L036
Anesthetic Management of a Patient With Penetrating Chest
Trauma
3:30-4:45 p.m. | Room 343-345
Charles Smith M.D.
Problem-Based Learning Discussions | L045
Blood IS Thicker Than Water: Anesthetic Concerns of
Hypercoagulability
3:30-4:45 p.m. | Room 343-345
Gregory Rose M.D.
Problem-Based Learning Discussions | L046
Prevention and Management of Intraoperative Awareness in High
Risk Patients
3:30-4:45 p.m. | Room 343-345
Kathleen Smith M.D.
Refresher Course Lecture | 122
Mastering Anesthesia for the Elderly Patient
4-5 p.m. | RiverGate
Jeffrey Silverstein M.D.
This session will focus on application of current knowledge and
evolving guidelines and standards to assure that your approach to
the care of the elderly patients is grounded in the current state of
the art. Participants can expect to garner numerous opportunities
to improve their care of the elderly surgical patient.
Sunday, October 12
Problem-Based Learning Discussions | L051
Beyond Swiss Cheese - Cases for the Anesthesia Patient Safety
Ofcer
7:15-8:30 a.m. | Room 343-345
Jonathan Cohen M.D.
Problem-Based Learning Discussions | L052
A Patient With a Temperature of 102.5 F and Rigors 3 hours after
Surgery
7:15-8:30 a.m. | Room 343-345
Theresa Gelzinis M.D.
Subspecialty Panels | 603
(STA) How Can Mobile Technology Help Me Help My Patients?
7-8:15 a.m. | Room 228-230
Maxime Cannesson M.D., Ph.D.
Mobile technology devices (e.g. smartphones and tablet
computers) and apps are nearly ubiquitous tools that are carried
by anesthesia providers in the perioperative setting. As computing
power and software sophistication has grown, so has the
potential to use mobile technology to enhance various aspects
of anesthesia practice. This panel will explore how applications
of mobile technology can improve patient care, perioperative
communication, healthcare resource utilization, and education.
Allan Simpao M.D. Mobile Devices for Critical Event Preparedness
and Management Brian Rothman M.D. Mobile Medical Apps Impact
on Healthcare Consumption Jorge Galvez M.D. Communication,
Cloud Computing, and Collaboration Using Mobile Technology
Clinical Forum | CF04
Evidence-Informed Anesthesia for the Severely Obese; Example
Obstetrics and Gynecology - Does It Exist?
8-9:30 a.m. | Room 206-207
Roman Schumann M.D.
Intraoperative Ventilation Strategies and Extubation Criteria in the
Complex Obese Patient
Two cases describe the complexity that can arise when caring
for an obese parturient or a severely obese woman for routine
minimally invasive hysterectomy and hiatal hernia repair. The
cases will allow us to examine and discuss with the audience
the best available practice evidence for preoxygenation and
airway management, intraoperative ventilation management and
extubation decision making of the severely obese. Physiologic
changes of obesity combined with pregnancy will be addressed,
as well as the dilemma for dosing of anticoagulants and
antibiotics in this population. Vilma Ortiz M.D. Airway Optimization
and Management of the Morbidly Obese Obstetric Patient and
Combined Obesity and Pregnancy Induced Physiological Changes
John Walsh M.D. Antibiotic and Anticoagulant Pharmacology and
Dosing in the Severely Obese
90 Minute Panel | PN50
Airway Management Training: Are We Keeping Up With Technology?
8-9:30 a.m. | Room 208-210
Nicholas Nedeff M.D.
A Multimodal Approach to Airway Training: Does It Make a
Difference?
This panel will provide an overview of different curriculum and
methods, such as simulation, interactive hands-on sessions, and
traditional lectures, being used for airway management training.
Addressed will be the new technologies and devices, such as
video laryngoscopes and supraglottic devices, that have been
recently introduced for airway management and how they affect
both the way we manage airways and the way we train residents
in managing airways. Different assessment tools for evaluating
resident performance will also be addressed. Novel approaches
to airway management training and solutions to limitations in
airway management training will be suggested. Ljuba Stojilj Kovic,
M.D., Ph.D. Simulation and Airway Management: Its Uses, Benets,
and Limitations Carin Hagberg M.D. New Airway Devices and Their
Impact on How We Manage Airways
Poster Presentations | PO02-1
Anesthetic Action and Biochemistry: Efcacy and Safety of Current
and Emerging Anesthetics and Analgesics
8-10 a.m. | Hall B1-Area C
EDUCATION

69
Poster Presentations | PO13-1
Outcomes and Database Research
8-10 a.m. | Hall B1-Area A
Hands-on Workshop | DW04
Basic/Advanced Flexible Fiberoptic Intubation Workshop
8-10:30 a.m. | Room 353-355
Hands-on Workshop | DW05
10:30 a.m.-1 p.m. | Room 353-355
Hands-on Workshop | DW06
2:30-5 p.m. | Room 353-355
Katherine Gil M.D
Basic to Intermediate to Advanced exible beroptic experience:
an introductory discussion of clear indications, contraindications,
techniques, and complications of scope use. Expert instructors
from at least 6 countries (instructing in multiple languages) to
guide you through exible scope hands-on areas to develop your
skill. Mini discussions on local airway anesthetic and hands-
on equipment, with questions and answers in small groups.
Instructors guide you in combined exible scope use in hands-on
areas, to assist the successful completion of most major airway
devices. Learn to make a cheap, 5-minute dexterity model and
practise with multiple levels of difculty. Experience practising
with computerized systems: Virtual Fiberoptic Intubation and
ORSIM simulator program. Challenge yourself in the human
simulation systems with difcult intubation scenarios and in the
trouble-shooting area. Receive handout checklists for all facets
of beroptic practice and intubation. Gail Randel M.D. David
Wong M.D. Valerie Arnistead, M.D. Radha Arunkumar M.B., B.S.
Lauren Berkow M.D. Sylvain Boet M.D., M.Ed. Richard Cooper M.D.
Elifce Cosar M.D. Pierre Diemunsch M.D. Stephen Dierdorf M.D. D.
John Doyle M.D. Ludwik Fedorko M.D., Ph.D. David Feinstein M.D.
Lorraine Foley M.D. Giulio Frova M.D. Katherine Hagan M.D. Grant
Lindsay Hounsell M.D. Ling Qun Hu M.D. Orlando Hung M.D Marshal
Kaplan M.D. Robert Krohner D.O. Vicente Martinez-Pons M.D.,
Ph.D. Maria Matuszczak M.D. Alonso Mesa M.D. Leonid Minkovich
M.D. Michael Murphy M.D. Veronica Payne M.B.,B.S. Andrew Roth
M.D. Bettina Schmitz M.D., Ph.D., DEAA Massimilano Sorbello M.D.
Francis Stellaccio M.D. Ljuba Stojiljkovic M.D., Ph.D Adriaan Van
Rensburg M.D. Lakshmikumar Venkat Raghavan M.B.,B.S. Leonard
Wade, M.S. Ashutosh Wali M.D., M.B.,B.S. Marcin Wasowicz M.D.
David Wong M.D. Meltem Yilmaz M.D. Andrew Zura M.D.
Problem-Based Learning Discussions | L061
Anesthetic Management of a Patient With Penetrating Chest
Trauma
9-10:15 a.m. | Room 343-345
Charles Smith M.D.
Problem-Based Learning Discussions | L069
Prevention and Management of Intraoperative Awareness in High
Risk Patients
9-10:15 a.m. | Room 343-345
Kathleen Smith M.D.
Problem-Based Learning Discussions | L070
Airway Management of a Patient With Penetrating Neck Injury
9-10:15 a.m. | Room 343-345
Albert Varon M.D.
Refresher Course Lecture | 211
Perioperative Management of Patients With Left Ventricular Assist
Devices Undergoing Noncardiac Surgery
9:15-10:15 a.m. | Room 260-262
Michael O’Connor M.D.
This Refresher Course Lecture will use physiologic and
pharmacologic principles to assist the learner in develop a rational
strategy for providing anesthesia for noncardiac surgery in patients
with ventricular assist devices (VADs).
Hands-on Workshop | AW06
Workshop on Flexible Endoscopy for Lung Isolation
9-10:15 a.m. | Room 356-357
Hands-on Workshop | AW07
10:30-11:45 a.m. | Room 356-357
Hands-on Workshop | AW08
12-1:15 p.m. | Room 356-357
Hands-on Workshop | AW09
1:30-2:45 p.m. | Room 356-357
Hands-on Workshop | AW10
3-4:15 p.m. | Room 356-357
Scott Schartel D.O.
The workshop is structured to provide participants with instruction
and practical experience in the use of exible endoscopy for
achieving lung isolation/one lung ventilation. Participants will work
with models of the tracheobronchial tree that allow placement
of endobronchial tubes (right and left) and various types of
bronchial blockers. Flexible video endoscopes connected to video
displays will be used. Participants will be given an opportunity
to learn the endoscopic anatomy of the tracheobronchial tree
to facilitate the correct placement of the various devices. The
workshop is structured in a way that will allow participants to
receive individual attention and work at their own level. The
workshop can accommodate novices seeking basic information
and advanced practitioners seeking answers to more complex
questions. The use of multiple instructors during each workshop
will provide opportunities for participants to experience a variety
of approaches to the same tasks and problems. William Simmons
M.D. Dalia Banks M.D. Kyle Harrison M.D. Jerry Clark M.D. Elizabeth
Drum M.D. Andrew Herlich M.D. Douglas Hester M.D.
Swapnil Khoche M.B., B.S. Jerome Klafta M.D. Timothy Maus M.D.
Sheela Pai M.D. Amy Robertson M.D. Daniel Roke M.D. Michael
Woo M.D.
Oral Presentations | OR13-2
Outcomes and Database Research - Evaluation of Risk
10-11:30 a.m. | Room 244
SCHEDULE BY LEARNING TRACK
70
Point-Counterpoint | PC08
Perioperative Colloid Administration - Should it be Abandoned?
10-11:30 a.m. | Room 211-213
Marc Rozner Ph.D., M.D.
PRO: Colloid Administration is Expensive, Offers No Benet and
Possibly Causes Harm
John Drummond M.D., CON: Colloids are Safe, Effective, and Useful
The 1998 Cochrane albumin meta-analysis red the shot heard
round the world with respect to albumin use. As a result, over
the past 15 years, several large scale studies have attempted
to identify reason(s) for this excess mortality in the albumin
treated groups. Also during this time, hydroxyethyl starch (HES)
solutions were introduced to overcome albumin issues. However,
several HES safety and efcacy studies came under re for
fraudulent research practices with many retractions, and recent
meta-analyses that excluded retracted studies have found excess
kidney injury requiring renal replacement and, possibly, decreased
survival in the HES treated groups. Since both albumin and HES
are more expensive than equipotent crystalloid, offer no additional
benet, and possibly introduce harm, these reports again raise
the questions of safety and efcacy of routine noncrystalloid
administration in the perioperative period.
Poster Presentations | PO08-1
Equipment, Monitoring and Engineering Technology: Securing the
Airway
10 a.m.-12 p.m. | Hall B1-Area C
Problem-Based Learning Discussions | L080
It’s Only a MAC Case and Now My Patient is on FIRE!
12:30-1:45 p.m. | Room 343-345
Mark Phillips M.D.
Poster Discussions | PD08-2
Equipment, Monitoring and Engineering Technology: Enhancing
Patient Safety and Environmentally Sound Practices
1-2:30 p.m. | Room 243
90 Minute Panel | PN102
Perioperative Management of Patients With Endocrine Disease: A
Global Perspective
1-2:30 p.m. | Room 255-257
Karen Domino M.D., M.P.H.
This 90 minute panel will focus on the perioperative management
of patients with important endocrine disorders from a global
perspective. The three s are internationally recognized authorities
in the anesthetic management of patients with endocrine
disorders. Pedro Ibarra M.D., MSc Diabetes and Perioperative
Infection Risk Yuguang Huang M.D Anesthetic Management of
Patients with Multiple Endocrine Neoplasia and Pheochromocytoma
Concezione Tommasino M.D. Perioperative Management of Patients
With Pituitary Disorders
120 Minute Panel | PN11
Intravenous Anesthesia Beyond Propofol
1-3 p.m. | Room 220-222
Keira Mason M.D.
The induction and maintenance of anesthesia is expanding
as new sedatives and anesthetics have been introduced and
are in development. This panel will explore the emerging
options not only for agents, but also for routes and methods
of delivery. The pharmacokinetics, pharmacodynamics and
clinical applications of alternatives will be explored in addition
to novel delivery techniques which include Target Controlled
Infusions and Computerized Assisted Delivery Systems. The
role of pharmacogenomics and its potential application to
anesthesia delivery will be reviewed. Anthony Absalom M.D.
Are Target Controlled Infusions in Our Future? Walter Maurer
M.D. Will Computerized Assisted Delivery Systems Replace
Anesthesiologists?
Poster Presentations | PO13-5
Outcomes and Database Research
1-3 p.m. | Hall B1-Area A
Hands-on Workshop | 817
Awake Fiberoptic Intubation: A Streamlined Approach With Nerve
Blocks
1-4 p.m. | Room 348-349
Scott Miller M.D.
This workshop will begin with a multimedia lecture that provides
an overview of how to successfully achieve skillful awake beroptic
intubations. This lecture will emphasize the participants’
understanding of when awake beroptic intubations should
be performed, patient preparation, sedation schemes, and an
overview of the individual techniques that compose the awake
beroptic intubation. Participants will then rotate through four
distinct stations that each focus on one of these discussed
techniques. While moving through these skills stations,
participants will have hands-on instruction while utilizing live
models and mannequins to simulate airway nerve blocks and
reinforce prociency. Additionally, participants will receive hands-
on training to develop advanced beroptic scope techniques using
mannequins and simulated airway mazes. Melissa Laxton M.D.
John Edward Reynolds M.D. Andrea Strathman M.D. Justin Traunero
M.D.
Refresher Course Lecture | 223
Perioperative Management of Pulmonary Hypertension
1:45-2:45 p.m. | RiverGate
Ronald Pearl M.D., Ph.D.
The number of patients with pulmonary hypertension undergoing
surgery is rapidly increasing, but these patients traditionally
have high morbidity and mortality. These patients can undergo
anesthesia and surgery with good outcomes by following a seven
step approach: recognizing the disorder, diagnosing the etiology,
assessing the severity of the disease, assessing the risks and
benets of anesthesia and surgery, developing an anesthetic plan,
choosing the correct monitoring, and managing the anticipated
complications of systemic hypotension and right heart failure.
EDUCATION

71
Refresher Course Lecture | 224
Obstructive Sleep Apnea - What an Anesthesiologist Should Know
1:45-2:45 p.m. | Room E-1
Frances Chung M.B.B.S., F.R.C.P.C.
The prevalence of patients with obstructive sleep apnea is 11.4%
in male and 4.7% in in female. About 85% to 90% of patients
with obstructive sleep apnea are not diagnosed. There may be
increased risk of perioperative complications. It is essential that
anesthesiologist know how to identify patients with undiagnosed
obstructive sleep apnea and learn the perioperative pathways for
the management of patients with obstructive sleep apnea.
Refresher Course Lecture | 231
Neuromuscular Management and Patient Outcomes
3-4 p.m. | Room E-2
Glenn Murphy M.D.
The aim of this session is to review the effects of residual
neuromuscular blockade on clinical outcomes. Techniques that
may be used to reduce residual paresis and improve patient safety
will be discussed.
Clinical Forum | CF07
A 65-Year-Old Male; Preoperative Evaluation and Management of
CAD for Robotic Prostate Surgery
3-4:30 p.m. | Room 206-207
Paul Kempen M.D., Ph.D.
Cardiac Stents-Management and Operative Thrombosis
This forum will explore controversial developments relating to
the intersection of pre- and perioperative anesthesia and cardiac
management of stented patients, including intraoperative stent
thrombosis management. Topics will include, but not be limited
to, advances in stent designs, preoperative testing, antithrombotic
medications and impact on outdated vs more recent management
guidelines and the controversial role of perioperative beta
blockade. Michael Boisen M.D. Perioperative Stent Thrombosis and
Surgical Risk- Clinical Management Shamsuddin Akhtar M.D.
Perioperative Antiplatelet Management of Stented Patients and
Guidelines Kathirvel Subramaniam M.D. Preoperative Evaluation,
Periperative Statins, and Stenting
Oral Presentations | OR07-2
Drug Disposition, Metabolism and Elimination
3-4:30 p.m. | Room 243
Oral Presentations | OR17-2
Respiration-Respiration-Respiration-Basic Mechanisms, Animal
Models and Clinical Science
3-5 p.m. | Room 244
120 Minute Panel | PN15
Fluid Administration in the Operating Room: An Update Focusing on
Recent Literature
3-5 p.m. | Room 203-205
Andrew Leibowitz M.D.
Monitoring and Optimizing Intravascular Volume
This panel will provide an updated view on intraoperative uid
administration with emphasis on the determination of how much
and what kind is appropriate. It will focus on recent literature that
emphasizes the importance of meticulous uid administration on
patient outcome. John Ellis M.D. Crystalloids Versus Colloids
Michael Wall M.D. Are Synthetic Colloids Safe? Steven Venticinque
M.D. Choosing the Correct Crystalloid
90 Minute Panel | PN65
Optimization of the High-Risk Surgery Patient in the Era of
Enhanced Recovery After Surgery and Perioperative Surgical
Home
3:30-5 p.m. | Room 255-257
Maxime Cannesson M.D., Ph.D.
Hemodynamic Optimization Strategies and Perioperative Goal
Directed Therapy for the High-Risk Surgery Patient
High-Risk surgery represents 10% of the overall volume of
surgeries performed in the US but account for 80% of the overall
postoperative mortality and complications. Hemodynamic and
ventilation optimization strategies have potential to improve the
post-operative outcome of these patients. The Perioperative
Surgical Home concept aims at improving standardization of
care and postoperative outcome by systematic implementation
of best evidence / best practices. This panel will describe the
postoperative outcome of high-risk surgery patients, how the
perioperative surgical home concept can help improving outcome,
and how best evidence hemodynamic and ventilation strategies
can be applied at the bedside to improve outcome. Zeev Kain
M.D., M.B.A. Perioperative Surgical Home for the High-Risk Surgery
Patient: Past, Present, Future Emmanuel Futier M.D., Ph.D.
Ventilation Strategies for the High-Risk Surgery Patient After the
IMPROVE Study
120 Minute Panel | PN17
Preoperative Assessment and Management
3:30-5:30 p.m. | Room 252-254
David Hepner M.D.
Minimizing Pre-Procedural Testing
This panel will emphasize the unique role of anesthesiologists
during the perioperative period leading preoperative clinics and
coordinating perioperative care. This panel will introduce the
participant to the national shift moving away from preoperative
testing to the practice of preoperative medicine. Panel will consist
of national experts in preoperative assessment and management
who will present cutting-edge evidence based concepts and
protocols for implementing evaluation and management of higher
risk patients to facilitate improved outcomes. These topics have
been areas of changing clinical practice and research over the last
couple of years and would prove to be quite helpful for members
practicing in all type of settings. Angela Bader M.D. Surgical
Appropriateness Angela Edwards M.D. The Surgical Home Bobbie
Jean Sweitzer M.D. Moving Away from Preoperative Testing to the
Practice of Preoperative Medicine
Refresher Course Lecture | 238
Weapons of Mass Destruction: Improvised Explosive Devices
4:15-5:15 p.m. | Room E-3
Michael Murray M.D., Ph.D.
Review of IEDs - their mechanism, their injury pattern and how
anesthesiologists should be prepared to manage casualties
from an IED. An important topic that should be of interest to
anesthesiologists following the Boston Marathon Bombing.
SCHEDULE BY LEARNING TRACK
72
Refresher Course Lecture | 240
What’s New in Airway Management
4:15-5:15 p.m. | La Nouvelle Ballroom AB
Lauren Berkow M.D.
This lecture will discuss conventional as well as newer methods
of airway evaluation, and how to use these methods to predict
difcult mask ventilation and intubation. A brief review of the
ASA Difcult Airway Algorithm as well as a review of the currently
available airway devices will be presented. The lecture will also
discuss extubation strategies and the challenges of airway
management outside the operating room setting. Finally, the
role of standardization and the importance of difcult airway
reporting and tracking and how to develop these initiatives will be
discussed.
Monday, October 13
Problem-Based Learning Discussions | L097
Help - My Patient Is on a Multi-Chemotherapeutic Regimen and Is
Coming for a Laparotomy! What Do I Need to Know?
7:15-8:30 a.m. | Room 343-345
Anoushka Afonso M.D.
Problem-Based Learning Discussions | L102
Malignant Hyperthermia in a Child Having a Tethered Cord Release
7:15-8:30 a.m. | Room 343-345
Tae Kim M.D.
Problem-Based Learning Discussions | L108
Airway Management of a Patient With Penetrating Neck Injury
7:15-8:30 a.m. | Room 343-345
Albert Varon M.D.
Refresher Course Lecture | 301
Positioning Problems You Hope to Never Encounter
8-9 a.m. | RiverGate
Mark Warner M.D.
This presentation highlights both common and rare positioning
issues that anesthesiologists encounter and discusses
opportunities to avoid these potentially devastating problems.
Oral Presentations | OR13-3
Outcomes and Database Research
8-9:30 a.m. | Room 245
120 Minute Panel | PN19
ACUTE Care Anesthesiology: Strategies for the Management of
Trauma, Emergencies and Disasters
8-10 a.m. | Room 220-222
Maureen McCunn M.D., MIPP
The ACUTE CARE anesthesiologist is an expert in resuscitation
strategies for trauma, emergencies, and diasasters. Traditional
goals of care may be secondary to immediate life-saving therapies.
Learning to think differently in the approach to these patients
challenges our conventional training. Armagan Dagal M.D., FRCA
Anesthesia for Non-Neurosurgical Procedures in Neurologically
Injured Patients Olga Kaslow M.D., Ph.D. Anesthesia for Patients
with Acute Abdomen: Old Problem and New Challenges Yun-Xia Zuo
M.D. Anesthesiologists Play Critical Roles in Rescue for Earthquake
Wounded
120 Minute Panel | PN21
Neuromuscular Blockade and Reversal
8-10 a.m. | Room 228-230
Sorin Brull M.D.
Safety Issues Regarding Neuromuscular Blockade and Reversal
This panel focuses on the issue of residual paralysis. Data
highlighting the susceptibility of the upper airway and control of
breathing to residual blockade will be presented. An update on
monitoring techniques will be provided, and safety issues related
to neostigmine reversal will be addressed. Cllinical experience with
sugammadex in other countries and future reversal strategies will
be discussed. Lars Eriksson M.D., Ph.D., FRCA What Is the Optimal
Target for Neuromuscular Recovery? Glenn Murphy M.D. Avoiding
the Consequences of Neuromuscular Blockade Matthias Eikermann
M.D. Is There Life after (or without) Sugammadex?
Poster Presentations | PO08-2
Equipment, Monitoring and Engineering Technology: Coagulation,
Hemoglobin, and Glucose
8-10 a.m. | Hall B1-Area C
Seminar | 821
Grant Writing and the NIH Study Section for the Uninitiated
8-11:00 a.m. | Room 348
Michael Andreae M.D.
Career Pathways and Grant Opportunities for Junior Investigators
Participants will be immersed in a mock NIH-study section
as reviewers of NIH grant submissions in anesthesia. Each
participant will receive two authentic NIH grant applications to
read, review and rate prior to the workshop. For the breakout
NIH mock study sessions, participants will divide into small
groups led by the presenters with research interests spanning
animal, human subject and data driven research. Participants
will present their assigned grant applications according to the
actual NIH-study section process. Before and between mock study
sessions, the presenters will delineate typical career pathways for
junior researchers in anesthesiology, point to the corresponding
private and public funding opportunities in their respective eld
of interests and introduce participants to the NIH merit review.
Presenters will share clinical pearls on what reviewers are looking
for, how to integrate research plan and career development
seamlessly on paper and in practice and on statistical aspects,
budget issues and IRB concerns. The presenters have ample
experience with the NIH merit review, are NIH or NSF funded and
actively involved in the mentor-trainee relationships. Participants
experience the NIH merit review in this workshop from the
perspective of a time-pressed reviewer. Participants may submit
their own applications and learn from the ensuing debate.
According to experienced NIH/NSF researchers, reading several
grant applications, pinpointing their strengths and weaknesses
and comparing them to one’s own application is enlightening. An
appreciation of the NIH merit review is crucial for funding success.
Brian Ilfeld M.D., M.S. Your Career Development Plan for a
Mentored Research Training Program: Presentation and Substance
Matthew Johnson Ph.D.How to Rene Your Methods and Statistcs
Section Jeffrey Silverstein M.D. The NIH Merit Review Process: An
Inside Perspective Gary Strichartz Ph.D. Explaining Complex and
Unfamiliar Concepts to Diverse NIH Reviewers Emery Brown M.D.,
Ph.D. Dolores Njoku M.D. Marcos Vidal-Melo M.D., Ph.D.
EDUCATION

73
Hands-on Workshop | 824A
Difcult Airway Workshop With Simulation
8-11 a.m. | Room 353-355
Hands-on Workshop | 824A
1-4 p.m. | Room 353-355
Allan Reed M.D.
This workshop will provide didactic and practicle learning. The
lecture portion will discuss important issues in difcult airway
management. The practicle portion will offer hands-on experience
with various airway devices and difcult airway simulation.
Elizabeth Behringer M.D. Joseph Quinlan M.D. George Arndt M.D.
Shawn T. Beaman, M.D. Lauren Berkow M.D. Ansgar Brambrink
M.D., Ph.D. Edmond Cohen M.D. Richard Cooper M.D. D. John Doyle
M.D., Ph.D. David Ferson M.D. Lorraine Foley M.D. Michael Frass
M.D. Theresa Gelzinis, M.D. Cheryl Gooden M.D. Carin Hagberg M.D.
Antonio Hernandez M.D. Marshal Kaplan M.D. Michael Kristensen
M.D. Pastor Luna M.D. Adrian Matioc M.D. Robert Naruse M.D.
Muhaammed Nasir M.B.,B.S. Vladimir Nekhendzy M.D. Steven
Neustein M.D. Irene Osborn M.D. Ellen O’Sullivan FCAI, FRCA,
FCPSP Anahi Perlas M.D. Ryan Romeo, M.D. William Rosenblatt
M.D. Patricia Roth M.D. John Schaefer III, M.D. Maria Shier M.D.
Francis Stellaccio M.D. Tracey Straker M.D., M.P.H. Maya Suresh
M.D. Wendy Teoh M.B.,B.S., FANZCA Felipe Urdaneta M.D. Sonia
Vaida M.D. Chandy Verghese M.D. Ashutosh Wali M.D., M.B.,B.S.
Andrew Zura M.D.
Problem-Based Learning Discussions | L110
Trauma Induced Coagulopathy
9-10:15 a.m. | Room 343-345
Maged Andrews M.B.,B.Ch.
Problem-Based Learning Discussions | L118
A Patient With End-Stage Liver Disease for Elective Surgery
9-10:15 a.m. | Room 343-345
Christopher Darling D.O., Michael Hannaman M.D.
Problem-Based Learning Discussions | L122
Oh No! Both Arteries in My Neck Are Blocked! Now What?
9-10:15 a.m. | Room 343-345
Stanlies D’Souza M.D.,F.R.C.A
Refresher Course Lecture | 309
A Few New Papers From Outside Anesthesia Which Can Affect Your
Pactice
9:15-10:15 a.m. | Room E-2
James Eisenach M.D.
This course will review take a few papers published within the past
year outside the specialty which have direct impact on patient
medical care in the perioperative, pain, and critical care areas.
Poster Presentations | PO13-2
Outcomes and Database Research
10 a.m.-12 p.m. | Hall B1-Area B
Poster Presentations | PO17-1
Respiration-Clinical and Basic Science
10 a.m.-12 p.m. | Hall B1-Area A
Refresher Course Lecture | 314
Perioperative Glycemic Management: A Practical Guide
12:30-1:30 p.m. | Room E-2
Basem Abdelmalak M.D.
After completing this refresher course attendees will be able to
formulate a comprehensive evidence based yet practical and a
clinically relevant plan for perioperative glycemic management.
Differences between diabetics and hyperglycemic non-diabetics
will be discussed. The whole spectrum of care will be covered;
pre-operative assessment, intraoperative management and
postoperative care. Management of patients utilizing insulin
pumps will be discussed in details.
Problem-Based Learning Discussions | L125
Can the Adult Patient With Morbid Obesity and Obstructive Sleep
Apnea Safely Undergo Outpatient Surgery?
12:30-1:45 p.m. | Room 343-345
Kenneth Hiller M.D.
Problem-Based Learning Discussions | L127
The Unanticipated Difcult Airway: A Dynamic and Dangerous
Scenario
12:30-1:45 p.m. | Room 343-345
Lavinia Kolarczyk M.D.
Problem-Based Learning Discussions | L130
I Swear It Will Only Take 15 Minutes: Anesthesia/Sedation for TEE/
Cardioversion
12:30-1:45 p.m. | Room 343-345
Julia Metzner M.D.
Problem-Based Learning Discussions | L131
Blood IS Thicker Than Water: Anesthetic Concerns of
Hypercoagulability
12:30-1:45 p.m. | Room 343-345
Gregory Rose M.D.
Oral Presentations | OR02-1
Anesthetic Action and Biochemistry: Off Target Effects of
Anesthetics to Improve Patient Safety
1-2:30 p.m. | Room 231-232
Point-Counterpoint | PC11
Computer-Assisted Personalized Sedation (CAPS) - Is the Coming
Technology of CAPS a Friend or Foe?
1-2:30 p.m. | Room 211-213
Walter Maurer M.D.
Brief Review of the Marketplace for CAPS Devices
This point counterpoint session will have active audience
involvement showing how this new technology might t into our
future practice. How can CAPS be safely used on ASA 3 & 4
patients? How can CAPS be used outside of GI cases? When do
you need more than an RN to monitor a patient using CAPS?
Richard Urman M.D., M.B.A., C.P.E. PRO: Technology Being Used to
Assist Skill Sets, Matching Resources with Anesthesia Needs, CAPS
Can Actually Help Us Steven Boggs M.D., M.B.A. CON: So You Want
MAC Without an Anesthetist? Where Have Our Standards Gone!
SCHEDULE BY LEARNING TRACK
74
90 Minute Panel | PN72
Morbid and Ultra Obesity: Growing Challenge in Anesthesiology
1-2:30 p.m. | Room 252-254
Ashish Sinha M.D., Ph.D.
Epidemiology of Obesity
Morbid Obesity is the ubiquitous problem facing all medical
practitioners especially anesthesiologists. Whether one chooses
to practice obstetric anesthesia or pain management, obesity
is the growing challenge in anesthesia. With two-thirds of
the US population overweight or obese, the ‘new normal’ is
heavier (and older and sicker). Management of these patients
requires a thorough understanding of anatomical, physiological
an dpharmacological changes with obesity and a few fail-safe
approaches, particularly to the airway. These lectures will cover
that, along with other information on sleep apnea, metabolic
syndrome and non-narcotic approach to the pain management
of the morbidly obese. Frances Chung, M.B.B.S., F.R.C.P.,
Sleep Apnea Jan Mulier M.D., Ph.D. Opioid Free Anesthesia
Patrick Neligan M.B., B.Ch. Metabolic Syndrome
90 Minute Panel | PN73
How Do We Decide When Not to Operate? Facing Challenges in
Surgical Decision-Making for Older Adults
1-2:30 p.m. | Room 255-257
Mark Neuman M.D., M.Sc.
Incorporating Prognosis into Surgical Decision-making for Older
Adults
Improving surgical decision-making for older adults represents
a key priority for perioperative health policy, with implications for
both the cost and quality of health care in the U.S. This session
will offer a range of perspectives on challenges and opportunities
related to operative decision-making for older adults. Mark D.
Neuman, M.D., M.Sc. (Anesthesiology, Univ. of PA), will address
the use of prognostic models to improve perioperative decision-
making. Zara Cooper, M.D., M.S.C.E. (Surgery & Palliative Care,
Brigham and Women’s Hospital) will discuss recent research
on survival and functional outcomes after major surgery in frail
older adults. Angela M. Bader, MD, MPH (Anesthesiology, Brigham
and Women’s Hospital) will discuss promoters and barriers to
anesthesiologist involvement in surgical decisions for older adults.
Marc J. Kahn, MD, MBA (Medicine, Tulane) will discuss ethical
challenges in surgical decision-making for older adults and the
management of DNR orders in the OR. Elizabeth Rickerson, M.D.,
Integrating Surgery and Palliative Care in Surgical Decision-making
for Older Adults Marc Kahn M.D., M.B.A. Ethical Challenges in
Surgical Decision-making for Older Adults Angela Bader M.D.
Anesthesiologist Involvement in Surgical Decision-making for Older
Adults: Opportunities and Challenges
Poster Presentations | PO07-1
Drug Disposition, Metabolism and Elimination
1-3 p.m. | Hall B1-Area A
Hands-on Workshop | 826
Wire-Guided Airway Management
1-4 p.m. | Room 333-334
Richard Galgon M.D., M.S.
This workshop will consist of a lecture followed by participants
moving through ve hands-on stations to gain knowledge of wire-
guided airway management including using wires to facilitate
intubation in the setting of airway lesions such as tumors, tracheal
deviation or stenosis. Wire-guided double-lumen endotracheal tube
placement and bronchial blocker placement will be demonstrated.
In addition, participants will learn wire-guided exchange of
supraglottic airways, including the laryngeal tube. Ron Abrons M.D.
Laura Hammel M.D. Michael Hannaman M.D. Aaron Joffe D.O. Mark
Leibel M.D. Erich Marks M.D. Kristopher Schroeder M.D. Joshua
Sebranek M.D. John Shepler M.D. Karl Willmann M.D.
Refresher Course Lecture | 318
How to Establish a Perioperative Surgical Home in Your Institution
1:45-2:45 p.m. | RiverGate
Zeev Kain M.D., M.B.A.
This Refresher Course Lecture provides an understanding of
how current and likely future U.S. healthcare reforms will impact
the practice of anesthesiology, how to establish a Perioperative
Surgical Home (PSH), and how the PSH can meet increasing
consumer and payer emphasis on shared decision-making, patient-
centeredness, and patient satisfaction.
Refresher Course Lecture | 321
My Pharmacy Is Out of Fentanyl, What Do I Do Now? Rational
Perioperative Opioid Substitutions
1:45-2:45 p.m. | Room E-3
Dhanesh Gupta M.D.
This Refresher Course Lecture will use pharmacokinetic-
pharmacodynamic principles to assist the learner in developing
rational alternative intraoperative and postoperative dosing
strategies when faced with the unavailability of fentanyl or one of
the other commonly used opioids.
Refresher Course Lecture | 327
Top 10 Respiratory Anesthesia Practices That Drive Me Crazy
3-4 p.m. | Room E-3
David Warner M.D.
As ever more sophisticated ventilators are introduced into the
operating room, there is increasing confusion regarding both the
physiological principles pertinent to respiratory management and
their clinical implications. Many commonly-employed ventilatory
strategies have little or no evidence to justify them, nor are they
supported by a convincing physiological rationale. This lecture
will debunk several timeworn dogmas related to ventilatory
management of the surgical patient, and help anesthesiologists
devise rational plans for providing respiratory support that will in
most cases simplify their practices and improve outcomes. Its
intent is to be both provocative and entertaining.
EDUCATION

75
Refresher Course Lecture | 329
Hazards of the Anesthesia Workstation
3-4 p.m. | La Nouvelle Ballroom AB
James Eisenkraft M.D.
This refresher course lecture will provide an overview of critical
incidents and adverse outcomes that have been reported with
use of anesthesia workstations, review strategies to prevent
adverse outcomes, discuss guidelines for pre use checkout of the
anesthesia machine and the limitations of automated checkouts.
Oral Presentations | OR07-1
Drug Disposition, Metabolism and Elimination
3-4:30 p.m. | Room 245
Problem-Based Learning Discussions | L099
Perioperative Laboratory and Cardiac Testing: What is Necessary?
3:30-4:45 p.m. | Room 343-345
David Hepner M.D.
Problem-Based Learning Discussions | L146
Cardiopulmonary Collapse During Laparoscopic Nissen
Fundoplication
3:30-4:45 p.m. | Room 343-345
Govind Rajan M.D.
Refresher Course Lecture | 331
Obesity and Anesthesia: Crossroads of a Challenge
4:15-5:15 p.m. | Room E-1
Ashish Sinha M.D., Ph.D.
Morbid obesity is the ubiquitous problem facing all medical
practitioners especially anesthesiologists. Whether one chooses
to practice obstetric anesthesia or pain management, obesity
is the growing challenge in anesthesia. With two-thirds of the
US population overweight or obese, the ‘new normal’ is heavier
(and older and sicker). Management of these patients requires a
thorough understanding of changes with obesity and a few fail-safe
approaches, particularly to the airway. This lecture will cover that,
along with other common challenges in anesthetic care of the
obese.
Tuesday, October 14
Problem-Based Learning Discussions | L149
Trauma Induced Coagulopathy
7:15-8:30 a.m. | Room 343-345
Maged Andrews M.B.,B.Ch.
Problem-Based Learning Discussions | L153
Oh No! Both Arteries in My Neck Are Blocked! Now What?
7:15-8:30 a.m. | Room 343-345
Stanlies D’Souza M.D., F.R.C.A
Problem-Based Learning Discussions | L159
My Patients Never Have Residual Paralysis in the PACU, or Do
They?
7:15-8:30 a.m. | Room 343-345
Stephan Thilen M.D., M.S.
Refresher Course Lecture | 406
ATLS Update: What Every Anesthesiologist Needs to Know...BEFORE
Going to the OR!
8-9 a.m. | La Nouvelle Ballroom AB
Maureen McCunn M.D., M.I.P.P.
ATLS is the standard of care for physicians who care for the
injured. Trauma is now the third leading cause of death in all
Americans, and the leading cause of death in those under the age
of 45. Understanding the approach to the severely injured - which
is counter to the traditional approach we learned in medical school
(extensive history, detailed physical exam, differential diagnosis
then conrmatory testing) - will enhance team performance and
optimize patient outcomes.
Oral Presentations | OR02-2
Anesthetic Action and Biochemistry: Emerging Anesthetics and
Analgesics
8-9:30 a.m. | Room 245
90 Minute Panel | PN84
Beyond Smoke and Mirrors: Panel on Surgical Fire Prevention
Including Laser Safety
8-9:30 a.m. | Room 225-227
Charles Cowles M.D., M.B.A.
Laser Safety As It Relates to the Anesthesiologist
This session will bring together experts who will discuss issues
surrounding the prevention of surgical res. Specic discussion
points will include basic surgical re prevention strategies and
the alignment of these strategies with initiatives of the ASA, APSF,
and FDA; Techniques proven to engage surgical team members
in re prevention; and Laser safety issues as it relates to the
anesthesiologist. Kenneth Silverstein M.D., M.B.A. Techniques
Proven to Engage Surgical Teams to Prevent Surgical Fires Jeffrey
Feldman M.D., M.S.E. Basic Surgical Fire Prevention and Efforts of
the ASA/APSF/FDA
Poster Presentations | PO13-6
Outcomes and Database Research
8-10 a.m. | Hall B1-Area A
Hands-on Workshop | 831A
The Use of Ultrasound for Vascular Access in Adults and Pediatrics
8-11 a.m. | Room 338-339
Hands-on Workshop | 831B
1-4 p.m. | Room 338-339
Ehab Farag M.D., F.R.C.A.
The workshop will explain the basics of ultrasound and
sonographic anatomy for central and peripheral blood vessels used
for vascular accesses. The workshop will enable the attendees to
practice the ultrasound scanning on live models. In addition will
give the attendees the oppourtunity to practice ultrasound needle
insertion on mannequins in live simulation like sittings. Wael Ali
Sakr Esa M.D. Maged Argalious M.D., M.B.A. Demetrios Bourdakos
M.D. Hesham Elsharkawy, M.D. Beth Demers Lavelle M.D. Rami
Karroum M.D. Kamal Maheshwari M.D. Loran Mounir M.D. John Seif
M.D. Sivan Wexler M.D. George Youssef M.D.
Problem-Based Learning Discussions | L162
Beyond Swiss Cheese - Cases for the Anesthesia Patient Safety
Ofcer
9-10:15 a.m. | Room 343-345
Jonathan Cohen M.D.
Problem-Based Learning Discussions | L165
Malignant Hyperthermia in a Child Having a Tethered Cord Release
9-10:15 a.m. | Room 343-345
Tae Kim M.D.
SCHEDULE BY LEARNING TRACK
76
Problem-Based Learning Discussions | L169
Cardiopulmonary Collapse During Laparoscopic Nissen
Fundoplication
9-10:15 a.m. | Room 343-345
Govind Rajan M.D.
Refresher Course Lecture | 411
Anesthetics and the Brain – Less Mysterious Than You May Think
9:15-10:15 a.m. | Room 260-262
Misha Perouansky M.D.
This RCL will provide an overview of the historic trajectory of
anesthetic mechanisms research from the mid-19th to the 21st
century. In particular the inuence of novel ideas in biology and
chemistry in directing research into anesthetic pharmacology will
be reviewed and form a background for contemporary efforts.
Neurobiological approaches to understanding anesthesia will be
critically differentiated from alternatives.
Oral Presentations | OR13-4
Outcomes and Database Research - Airway & Sleep Apnea
10-11:30 a.m. | Room 245
90 Minute Panel | PN90
Clinical Pearls: Anesthesia for Adult ENT Surgery
10-11:30 a.m. | Room 228-230
Basem Abdelmalak M.D.
Difcult Airway and the ENT Surgeons
This panel will address a few pertinent topics in the subspecialty
of anesthesia for otolaryngologic surgery: the new difcult airway
algorithm as it relates to the difcult airways encountered in
head and neck cancer patients; the role of the ENT surgeons and
framework for communication between the anesthesiologists
and their ENT surgeons’ colleagues; issues related to the ever
advancing and expanding eld of sinus surgery and how regional
anesthesia can play a role in caring for sinus surgery patients;
special considerations in anesthesia for otologic and neurotologic
surgery; the use of heliox and Laser in managing critical airway
stenosis and related anesthetic considerations. Samuel DeMaria
M.D. Anesthesia for Sinus Surgery D. John Doyle M.D., Ph.D.
Tracheal Stenosis, Heliox, and Laser Vladimir Nekhendzy M.D.
Anesthesia for Ear Surgery
Poster Presentations | PO07-2
Drug Disposition, Metabolism and Elimination
10 a.m.-12 p.m. | Hall B1-Area A
Refresher Course Lecture | 416
Anesthesia for Head and Neck Surgery
11:45-12:45 p.m. | Room E-3
David Healy M.D., MRCP, FRCA
This Refresher Course Lecture will provide an overview of
anesthesia for patients undergoing Head and Neck Surgery. It will
identify key anesthetic techniques and skills of importance to this
patient group. The lecture will emphasize patient safety with a
focus on laser airway surgery and jet ventilation.
Refresher Course Lecture | 417
Preoperative Identication, Evaluation and Optimization of the
Highest Risk Patients
11:45-12:45 p.m. | Room 260-262
Bobbie Jean Sweitzer M.D.
This lecture is specically designed to address the preoperative
assessment and management of the highest risk patients
anticipating anesthesia. The lecture will focus on patients with
conditions such as recent coronary stents, severe heart disease,
anemia, and the frail elderly. This lecture is designed to appeal
to those interested in preoperative evaluation beyond the typical
practice of many anesthesiologists but within the realm of those
positioning themselves to be part of the Surgical Home.
Problem-Based Learning Discussions | L099
Perioperative Laboratory and Cardiac Testing: What is
Necessary?
12:30-1:45 p.m. | Room 343-345
David Hopner M.D.
Problem-Based Learning Discussions | L175
Management of Antiplatelet Therapy in Patients With Coronary
Stents for Noncardiac Surgery
12:30-1:45 p.m. | Room 343-345
Davide Cattano M.D.,Ph.D.
Problem-Based Learning Discussions | L183
Perioperative Management of the Anemic Patient
12:30-1:45 p.m. | Room 343-345
Russell Roberson M.D.
Refresher Course Lecture | 424
Massive Transfusion Protocol in Trauma
1-2 p.m. | La Nouvelle Ballroom AB
Charles Smith M.D.
The use of a massive transfusion protocol facilitates rapid
availability of components in an increased ratio of plasma and
platelets to red blood cells. Understanding the mechanism of
trauma- induced coagulopathy together with surgical control
of hemorrhage and timely application of volume resuscitation
remains the cornerstone of treatment of hemorrhagic shock
in trauma. Point of care viscoelastic assays may allow for goal
directed therapy in trauma- induced coagulopathy.
Clinical Forum | CF14
Dogma and Controversies in Acute and Perioperative Burn Care
1-2:30 p.m. | Room 206-207
Sam Sharar M.D.
This forum will explore both common and controversial issues
encountered in the acute, perioperative, and postoperative care
of patients with signicant burn-related injuries. Using a pediatric
case-based discussion that is also applicable to adult burn-
injured patients, the topics of discussion will not only be relevant
to anesthesiologists who infrequently provide such care, but
also to those participating in acute and perioperative burn care
on a regular basis. Sanjay Bhananker M.D. Airway Management
Following Burn Injury Joe Jansen M.D. Perioperative Burn Care
Lee Woodson M.D., Ph.D. Sedation and Analgesia for Procedural
Burn Care
EDUCATION

77
Point-Counterpoint | PC18
Hypotensive Resuscitation
1-2:30 p.m. | Room 203-205
Joshua Tobin M.D.
This session will critically evaluate the literature for and against
hypotensive resuscitation. Using a Pro-Con format the s will
describe their rationale for enacting or avoiding hypotensive
resuscitation in trauma and acute care anesthesia. Albert Varon
M.D. CON: Hypotensive Resuscitation Has No Proven Benets in
Most Trauma Patients Samuel Galvagno Jr., D.O., Ph.D., M.S.
PRO: Don’t Pop the Clot, Embrace a Lower Blood Pressure
Poster Discussions | PD17-1
Respiration-Upper Airway and Sleep Apnea
1-2:30 p.m. | Room 245
120 Minute Panel | PN30
Computer-Assisted Personalized Sedation (CAPS) - the Future of
Moderate Sedation
1-3 p.m. | Room 252-254
Walter Maurer M.D.
Brief Review of the Marketplace for CAPS Devices
This panel session will show how this new technology might t
into our future practice. Some opinions of the faculty will be in
opposition to the Anesthesiologist. How can CAPS be safely
used on ASA 3 & 4 patients? How can CAPS be used outside
of GI cases? When do you need more than an RN to monitor
a patient using CAPS? Richard Urman M.D., M.B.A., C.P.E.
Technology Being Used to Assist Skill Sets. Matching Resources
with Anesthesia Needs. CAPS Can Actually Help Us Steven Boggs
M.D., M.B.A. So You Want MAC without an Anesthetist? Where Have
Our Standards Gone! John Vargo M.D., M.P.H. CAPS from the GI
Perspective
Poster Presentations | PO02-2
Anesthetic Action and Biochemistry: Molecular Insights into
Anesthetic Mechanism of Action, Safety and Toxicity
1-3 p.m. | Hall B1-Area C
Poster Presentations | PO08-4
Equipment, Monitoring and Engineering Technology: Anesthesia
Depth and Eclectic Assortment of Cool Stuff
1-3 p.m. | Hall B1-Area B
Poster Presentations | PO13-4
Outcomes and Database Research
1-3 p.m. | Hall B1-Area A
Refresher Course Lecture | 428
Strategies for Success in Anesthesia During One-Lung Ventilation
2:15-3:15 p.m. | Room E-3
Gregory Fischer M.D.
This refresher course will review the physiology behind one lung
ventilation, descript the differences and indications for lung
separation versus isolation and demonstrate devices that are
commonly used to achieve these goals.
Refresher Course Lecture | 430
Electrical Safety in the Operating Room
2:15-3:15 p.m. | La Nouvelle Ballroom AB
Jeffrey Gross M.D.
Starting with fundamental principles of electrical theory, this
refresher course will trace the development of electrical power
distribution to homes, hospitals, and operating suites, including
the various safety mechanisms which have been developed to
minimize the risk of macro- and microshock to anesthetized
patients and operating room personnel. The principles of
electrocautery operation will also be discussed. At the conclusion
of the lecture, there will be hands-on demonstrations to reinforce
the concepts.
Poster Discussions | PD08-4
Equipment, Monitoring and Engineering Technology: Advances in
Noninvasive Monitoring
3-4:30 p.m. | Room 245
120 Minute Panel | PN32
Creating the Safe Non-Operating Room Anesthesia (NORA)
Experience
3-5 p.m. | Room 211-213
Brenda Gentz M.D.
Keeping the Medically Challenging Patient Safe
Creating a safe, positive Non-Operating Room (NORA) experience
is the goal of every anesthesia provider, but data suggests
that this environment is not without risk. The changing medical
characteristics of patients, potentially difcult intubations
and modest equipment provided can challenge even the most
seasoned professional. Anticipating critical situations, creating
and dening systems to deal with emergenies, and implementing
known professional guidelines are keys to success. The future
administration of anesthesia drugs in this environment may
change with increased utilization of target controlled infusions
(TCI) and computer assisted personalized sedations (CAPS).
Irene Osborn M.D. Confronting the Difcult Airway in the NORA
Environment Keira Mason M.D. Creating and Supporting a Culture
of Safety in NORA Anthony Absalom M.D. Target Controlled
Infusions and Computer Assisted Personalized Sedation in the
NORA Environment
Refresher Course Lecture | 431
Trauma Anesthesia and Operative Resuscitation
3:30-4:30 p.m. | Room E-1
Joshua Tobin M.D.
The Refresher Course lecture in Trauma Anesthesia and
Operative Resuscitation will evaluate recent advances in
transfusion medicine as well as new critical care interventions
(e.g.; airway management, ventilatory strategies) available
to the anesthesiologist. Emphasis will be placed on the
anesthesiologist’s role in operative resuscitation.
Refresher Course Lecture | 432
Different Strokes for Operative Folks: Prevention of the
Perioperative Cerebrovascular Accident
3:30-4:30 p.m. | Room E-2
George Williams M.D.
An in depth discussion of the pathophyiology and management
of stroke for the anesthesiologist. Strategies to optimize patient
outcomes in this population are discussed in detail, as well as
the clinical approach applied by neurologists and neurosurgeons
in the pre and post operative management of this population in
order to give insight as to the decision to proceed with surgerical
intervention. Methods to address risk factors and promote
maximum post operative functionality are discussed.
SCHEDULE BY LEARNING TRACK
78
Refresher Course Lecture | 433
Current Controversies of Perioperative Fluid Management
3:30-4:30 p.m. | Room E-3
Roman Dudaryk M.D.
This refresher course will provide a much-needed update on
practical implication of perioperative uid therapy. Particular
emphasis will be placed on new evidence regarding colloid effects
on renal function. Applicability of recent studies of colloids
vs crystalloids to various groups of surgical patients will be
discussed. Recommendations for uid choices in the settings of
trauma, sepsis, pre-existent renal failure, ambulatory surgery will
be made.
Problem-Based Learning Discussions | L184
Help - My Patient Is on a Multi-Chemotherapeutic Regimen and Is
Coming for a Laparotomy! What Do I Need to Know?
3:30-4:45 p.m. | Room 343-345
Anoushka Afonso M.D.
Problem-Based Learning Discussions | L188
A Patient With End-Stage Liver Disease for Elective Surgery
3:30-4:45 p.m. | Room 343-345
Christopher Darling D.O. Michael Hannaman M.D.
Problem-Based Learning Discussions | L189
Can the Adult Patient With Morbid Obesity and Obstructive Sleep
Apnea Safely Undergo Outpatient Surgery?
3:30-4:45 p.m. | Room 343-345
Kenneth Hiller M.D.
90 Minute Panel | PN93
Sugammadex: Are We Finally There? Update on Unmet Medical
Need, Clinical Use in Europe and Regulatory Progress
3:30-5 p.m. | Room 217-219
Jonathan Jahr M.D.
Science and Regulatory Stalemate and Solution
This 90-minute panel will review evidence-based medicine
on current reversal of neuromuscular block and understand
unmet medical need, both for emergency cannot intubate and
ventilate crises, and reversal in deep neuromuscular block, list
pharmacology of sugammadex, explain differences in mode
of action of sugammadex, and review phase 2 and 3 data on
sugammadex for safety and efcacy, including newly published
studies about hypersensitivity, renal failure and repeat usage,
update on regulatory stalemate and solution to gain approval,
update on regulatory stalemate and suggest solution to gain
approval, expound on clinical use in Europe of sugammadex,
including postmarketing studies in over 5 million uses, and
understand novel uses of sugammadex, as deep block for
laparoscopic procedures improving safety and outcomes. Glenn
Murphy M.D. Safety and Efcacy of Neostigmine Reversal: Unmet
Medical Need for New Agent Thomas Fuchs-Buder M.D. Current
Use of Sugammadex in Europe and Postmarketing Data on Over 5
Million Uses
Wednesday, October 15
Refresher Course Lecture | 503
Recent Advances in Perioperative Fluid Management and the
Patients’ Outcomes
8-9 a.m. | Room E-3
Ehab Farag M.D., F.R.C.A. Moderator
The discovery of endothelial glycocalyx has changed our
understanding for tissue perfusion to the degree that Starling
principle has been challenged as a valid principle to govern the
tissue perfusion. The aim of this lecture is to present the recently
discovered functions of endothelial glycocalyx and their importance
for patients’ outcomes. The lecture will present the most recent
advances in peri-operative uid management and problems with
using hydroxyethyl starch solutions during the peri-operative period.
Oral Presentations | OR13-5
Outcomes and Database Research - Blood & Transfusions
8-9:30 a.m. | Room 245
Poster Discussions | PD08-3
Equipment, Monitoring and Engineering Technology: Monitoring
Sedation and Cerebral Effects of Anesthesia
8-9:30 a.m. | Room 243
90 Minute Panel | PN99
Big Data, Big Opportunity: Anesthesiology 2.0
8-9:30 a.m. | Room 220-222
Matthew Levin M.D.
Dening Big Data and the Limitations of Traditional Analytic
Approaches
The goal of this panel is to familarize the audience with the
concept of big data and allow them to understand the relevance
of big data to the specialty of Anesthesiology. Panel members will
discuss how people generally dene big data, and what leads to
datasets that are truly too large to be analyzed using traditional
approaches.Questions to be addressed include:What are some of
the practical problems in dealing with large clinical data sets and
how can we get around them? What kind of clinical questions can
big data help us answer, that traditional research techniques (e.g.
randomized controlled trials) cannot?How can we use our current
infrastructure, data warehousing techniques, and visualization
tools to lead to higher quality, more cost effective care? What is
the future of big data in perioperative medicine? For example, can
we combine indoor patient location systems with real time clinical,
stafng, and operational data to enable new models of care?
Jonathan Wanderer, M.D. Metadata, Electronic Medical Records
and Clinicians J. Michael Schmidt Ph.D., M.Sc. Converting Big Data
Analytics into Clinical Practice and the Challenges of Using Big Data
With Traditional Medical Research Techniques Peter Fleischut M.D.
Computational Healthcare
EDUCATION

79
120 Minute Panel | PN34
Aortic Surgery in the 21st Century
8-10 a.m. | Room 228-230
Rae Allain M.D.
Repair of aortic pathology has changed dramatically since
introduction of endovascular techniques, resulting in lower
mortality and changes in anesthetic approach. A shift to EVAR
procedures has reduced the frequency of elective open aortic
procedures, creating an educational challenge: most trainees
have limited opportunities to practice managing aortic clamping
and unclamping before presented with an emergency case.
Simulation may play a valuable educational role in lling this gap.
Surgical prociency in elective EVAR also has begun an evolution
to EVAR as the preferred technique for emergency management
of ruptured AAA. In this situation, there is rationale for an initial
local anesthetic approach. Finally, lumbar CSF drainage has
become a standard in preventing paraplegia in patients undergoing
endovascular or open repair of the thoracic aorta. Daniel Johnson
M.D. Point-of-Care Ultrasound: Tells You What You Need to Know
Preop and Postop Hovig Chitilian M.D. Emergency AAA Repair
under Local Anesthesia?? Marjorie Stiegler M.D. Simulation of
Aortic Cross-Clamp and Unclamp David Collard M.D., M.S.
This Is Spinal Tap with a 14 Gauge Tuohy
SCHEDULE BY LEARNING TRACK
80
Neuroanesthesia
Saturday, October 11
Problem-Based Learning Discussions | L002
Only a Little Sniff of Cocaine; Now an Aneurysm Coiling
Headache!
7:15-8:30 a.m. | Room 343-345
Jess Brallier M.D. Moderator
Refresher Course Lecture | 109
Adult Head Injury: Management Update and Controversies
9:15-10:15 a.m. | Room E-2
Audree Bendo M.D. Co-Moderator
Perioperative Management of the Adult Head Injury Patient
This refresher course lecture will review the perioperative and
critical care management of adult patients with severe traumatic
brain injury. The resuscitation protocol for these patients will be
discussed with specic emphasis on guidelines, implementation
and controversies in management. Martin Smith M.B.,B.S. Co-
Moderator-Critical Care Management and Monitoring of the Adult
Head Injury Patient
Poster Presentations | PO10-2
Experimental Neurosciences: Mechanisms
10 a.m.-12 p.m. | Hall B1-Area C
Problem-Based Learning Discussions | L025
Delayed Emergence After Craniotomy- No Delays Accepted
12:30-1:45 p.m. | Room 343-345
Ra Avitsian M.D.
Problem-Based Learning Discussions | L030
My Ulnar Neuropathy Has Resolved. Now I Have to Go for Spine
Surgery in the Prone Surrender Position
12:30-1:45 p.m. | Room 343-345
Ihab Kamel M.D.
120 Minute Panel | PN06
Babies Are Not Just Large Rat Pups: Controveries on the Impact of
Anesthetics on the Developing Brain
1-3 p.m. | Room 228-230
Sulpicio Soriano M.D.
This panel will examine the controversies on the impact of
anesthetics on the developing brain, with emphasis on molecular
correlates in laboratory models and behavioral assessments
in humans. Andreas Loepke M.D., Ph.D. Cell Age Vulnerability
to Neuronal Demise Laszlo Vutskits M.D. Anesthetics Regulate
Neuroplasticity Randall Flick M.D. Anesthetic Effects on Learning
Behavior in Humans Mary Ellen McCann M.D., M.P.H.
Confounding Factors in Human Studies
Refresher Course Lecture | 114
Blood Pressure and the Brain: How Low Can You Go?
1:30-2:30 p.m. | Room 260-262
John Drummond M.D.
This session will identify aspects of physiologic homeostasis and
clinical management that reduce the vulnerability of the brain and
spinal cord to ischemic injury.
Refresher Course Lecture | 121
Smart Seniors: Avoiding Perioperative Brain Failure
3-5 p.m. | La Nouvelle Ballroom AB
Gregory Crosby M.D. Moderato
Why Seniors Are Vulnerable in the OR and ICU?
This two-hour refresher course lecture panel will focus on the
postoperative evaluation and management of three postoperative
CNS problems in elderly patients. Deborah Culley M.D. Anesthesia
and Analgesia - Friend or Foe? Pratik Pandharipande M.D. Illness,
Surgery and Inammation - Foe for Sure
Problem-Based Learning Discussions | L040
Ah! I Can’t Bear It! This Is the Worst Headache of My Life!
3:30-4:45 p.m. | Room 343-345
Stanlies D’Souza M.D., F.R.C.A. Moderator
90 Minute Panel | PN47
Management of Neurological Events After Anesthesia
3:30-5 p.m. | Room 228-230
Deborah Rusy M.D.
This panel will discuss the management of adverse neurologic
outcomes. Laurel Moore M.D. Stroke This panel will discuss the
management of adverse neurologic outcomes. Sandra Kopp M.D.
Seizures
Sunday, October 12
Problem-Based Learning Discussions | L049
Delayed Emergence After Craniotomy - No Delays Accepted
7:15-8:30 a.m. | Room 343-345
Ra Avitsian M.D. Moderator
Problem-Based Learning Discussions | L055
Deep Brain Stimulation for Parkinson’s Disease: What Is the Role of
the Anesthesiologist?
7:15-8:30 a.m. | Room 343-345
Julia Metzner M.D. Moderator
Poster Presentations | PO10-1
Experimental Neurosciences: Neurotoxicity
8-10 a.m. | Hall B1-Area D
Poster Discussions | PD05-2
Clinical Neurosciences
8-9:30 a.m. | Room 244
90 Minute Panel | PN53
The Yin and Yang of Anesthetic Drugs: Are They Neuroprotective or
Neurotoxic?
8-9:30 a.m. | Room 225-227
Piyush Patel M.D.
Lessons from and Limitations of Each Perspective
This session will review experimental and clinical research on
the neuroprotective and neurotoxic effects of anesthetic drugs.
David Warner M.D. Anesthetics as Neuroprotectants: Hope and
Promise Kristin Engelhard M.D., Ph.D. Anesthetics as Neurotoxins:
Experimental Traumatic Brain Injury
Problem-Based Learning Discussions | L064
Just Another Subarachnoid Hemorrhage? Or Am I Really Up-to-date
on What to Do?
9-10:15 a.m. | Room 343-345
Eduardo Galeano M.D. Moderator
EDUCATION

81
Problem-Based Learning Discussions | L074
Ah! I Can’t Bear It! This Is the Worst Headache of My Life!
12:30-1:45 p.m. | Room 343-345
Stanlies D’Souza M.D.,F.R.C.A. Moderator
Poster Presentations | PO05-1
Clinical Neurosciences
1-3 p.m. | Hall B1-Area E
Refresher Course Lecture | 229
The Impact of Anesthesia on the Young and Old Brain
3-4 p.m. | RiverGate
Audree A. Bendo M.D. Moderator
The assumption that anesthesia has no long-term adverse CNS
consequences may be true for most patients between six months
and 60 years of age. However, for patients younger than six
months or older than 60 years, that status quo assumption is
under challenge from a growing body of evidence. This lecture will
address that evidence and review options for clinical management
based on recent laboratory and clinical trials.
Problem-Based Learning Discussions | L086
Only a Little Sniff of Cocaine; Now an Aneurysm Coiling
Headache!
3:30-4:45 p.m. | Room 343-345
Jess Brallier M.D. Moderator
Monday, October 13
Subspecialty Panels | 606
(SNACC) Anesthesia for Acute Stroke Management: Method, Timing
and Hemodynamics
7-8:15 a.m. | Room 231-232
Ra Avitsian M.D.
With the availability of rapid medical response and education
regarding symptoms of Stroke, much has been discussed
and published about new methods of management including
interventional treatment of acute ischemic stroke. There is
however not enough guidance regarding optimal anesthetic
method and hemodynamic parameters in patients undergoing
this procedure. This panel will consist of a moderator and
three speakers to analyze the current knowldege about the
best anesthetic care for patients with acute ischemic stroke.
Muhammad Hussain M.D. Interventionalist’s View on Optimal
Anesthetic Conditioin for Stroke Pekka Talke M.D. Evidence on
Best Anesthetic Method Alana Flexman M.D. Timing and Best
Hemodynamics in Management of Acute Stroke
Problem-Based Learning Discussions | L101
My Ulnar Neuropathy Has Resolved. Now I Have to Go for Spine
Surgery in the Prone Surrender Position
7:15-8:30 a.m. | Room 343-345
Ihab Kamel M.D. Moderator
Problem-Based Learning Discussions | L133
Awake Craniotomy in a Patient With Obstructive Sleep Apnea
7:15-8:30 a.m. | Room 343-345
Karl Willmann M.D. Moderator
Refresher Course Lecture | 306
Perioperative Management of Patients Undergoing Spine Surgery
8-10 a.m. | La Nouvelle Ballroom AB
Susan Black M.D. Moderator
Overview of the Anesthetic Management of Spine Surgery
This refresher course lecture will review the anesthetic
considerations for patients undergoing spine surgery, including
tracheal intubation, blood conservation techniques, blood loss
and resuscitation, preservation of spinal cord integrity, patient
positioning, and anesthetic and surgical risks during the various
procedures. Michael Todd M.D. Management of Cervical Spine
Lesions/Injury Tod Sloan M.D., Ph.D., M.B.A. Intraoperative Spinal
Cord Monitoring Lorri Lee M.D. Perioperative Visual Loss and Spine
Surgery
Poster Presentations | PO10-3
Experimental Neurosciences: Cerebral Blood Flow and CNS
Ischemia
8-10 a.m. | Hall B1-Area E
Problem-Based Learning Discussions | L111
Crisis in the Neuro-Muscular Junction: Anesthetic Implications
9-10:15 a.m. | Room 343-345
Cristina Barboi M.D. Moderator
Oral Presentations | OR10-2
Experimental Neurosciences
1-2 p.m. | Room 238-239
90 Minute Panel | PN70
Life-Death Transition
1-2:30 p.m. | Room 225-227
George Mashour M.D., Ph.D.
Moderator and Neurobiology of the Dying Brain
This panel will examine the life-death transition from the
perspective of a neurobiologist, intensivist and transplant
anesthesiologist. David McDonagh M.D. Brain Death in the ICU
Paul Picton M.D. Organ Donation after Cardiac Death
Oral Presentations | OR10-1
Experimental Neurosciences: Mechanisms
3-4:30 p.m. | Room 243
Problem-Based Learning Discussions | L137
An Acute Ischemic Stroke Coming to Your Neuroangiography
Suite
3:30-4:45 p.m. | Room 343-345
Ra Avitsian M.D. Moderator
Problem-Based Learning Discussions | L145
Deep Brain Stimulation for Parkinson’s Disease: What Is the Role of
the Anesthesiologist?
3:30-4:45 p.m. | Room 343-345
Julia Metzner M.D. Moderator
Tuesday, October 14
Problem-Based Learning Discussions | L150
An Acute Ischemic Stroke Coming to Your Neuroangiography
Suite
7:15-8:30 a.m. | Room 343-345
Ra Avitsian M.D. Moderator
SCHEDULE BY LEARNING TRACK
82
Problem-Based Learning Discussions | L160
Awake Craniotomy in a Patient With Obstructive Sleep Apnea
7:15-8:30 a.m. | Room 343-345
Karl Willmann M.D. Moderator
Poster Presentations | PO05-2
Clinical Neurosciences
8-10 a.m. | Hall B1-Area E
Poster Discussions | PD10-1
Experimental Neurosciences: Neurotoxicity
10-11:30 a.m. | Room 243
90 Minute Panel | PN88
Sleeping and Waking Is Hard to Do: Mechanisms of Induction and
Emergence From General Anesthesia
10-11:30 a.m. | Room 220-222
Peter Goldstein M.D.
This panel will span translational and clinical science related to
sleep and anesthesiology. Max Kelz M.D., Ph.D. Sleep Neurobiology
and General Anesthesia Ken Solt M.D. Hijacking Arousal Centers
to Reverse Anesthesia George Mashour M.D., Ph.D. Feedback
Connectivity and Unconsciousness in Humans
Poster Presentations | PO10-4
Experimental Neurosciences: Inammation, Cognitive Dysfunction
and Neuroprotection
10 a.m.-12 p.m. | Hall B1-Area E
Problem-Based Learning Discussions | L176
Just Another Subarachnoid Hemorrhage? Or Am I Really Up-to-date
on What to Do?
12:30-1:45 p.m. | Room 343-345
Eduardo Galeano M.D. Moderator
Refresher Course Lecture | 420
Perioperative Management of Cerebrovascular Diseases
1-2 p.m. | Room E-1
Adrian Gelb M.B.,B.Ch., FRCPC Moderator
This refresher course lecture will focus on the perioperative
management of cerebrovascular disease in the operating room,
interventional neuroradiology suite and ICU. Specic procedures
such as angiography, aneurysm clipping/coiling, carotid
endarterectomy/stenting and will be reviewed.
Clinical Forum | CF15
You Want to Test What?: Anesthetic Challenges During Functional
Neurosurgery
3-5 p.m. | Room 206-207
Antoun Koht M.D.
Awake Craniotomy and Regional Blocks
This panel will present several neurosurgical cases: intracranial
aneurysm clipping, posterior fossa tumor resection, and awake
craniotomy for tumor resection and deep brain stimulation. The
discussion will involve optimization of anesthesia, differential
diagnosis of changes and the use of stepwise algorithm to identify
the change. The discussion will clarify the ability and limitation of
each monitor and compatible anesthetic techniques and agents.
The panel will emphasize the input of the audience (audience
response system could be used) and the experience of the panel
members will be used to discuss controversial aspects (such as
controversy about specic monitoring techniques). Tod Sloan M.D.,
Ph.D., M.B.A. Brainstem Tumor Laura Hemmer M.D. Aneurysms
Chanhung Lee M.D. Deep Brain Stimulation
Problem-Based Learning Discussions | L186
Crisis in the Neuro-Muscular Junction: Anesthetic Implications
3:30-4:45 p.m. | Room 343-345
Cristina Barboi M.D. Moderator
Wednesday, October 15
Poster Discussions | PD05-1
Clinical Neurosciences: Intraoperative Monitoring
10-11:30 a.m. | Room 245
EDUCATION

83
SCHEDULE BY LEARNING TRACK
NOTES
84
Obstetric Anesthesia
Saturday, October 11
Subspecialty Panels | 601
(SOAP) Caring for Our Own: Focusing on the Care Provider to
Optimize Safety for Our Patients
7-8:15 a.m. | Room 231-232
Robert Gaiser M.D.
Caring for the Provider Following a Bad Outcome
This panel addresses the communication and lack of
communication in the labor suite. There are several reasons
for poor communication such as bad outcomes and disruptive
physicians. An approach to these barriers will be presented. May
Pian-Smith, M.D. Teaching Effective Communication on Labor and
Delivery, Lawrence Tsen, M.D. The Disruptive Physician
Problem-Based Learning Discussions | L007
Just Another Day on Labor and Delivery: Morbid Obesity and
Preeclampsia
7:15-8:30 a.m. | Room 343-345
Regina Fragneto M.D.
Problem-Based Learning Discussions | L116
Neurologic Complications Following Epidural Placement - How to
Differentiate and Manage?
7:15-8:30 a.m. | Room 343-345
Kelly Elterman M.D. David Hepner M.D.
Refresher Course Lecture | 104
Anesthesia for the Morbidly Obese Parturient
8-9 a.m. | Room E-3
Brenda Bucklin M.D.
The lecture will examine anesthetic and obstetric risk in morbidly
obese parturients as well as provide best practices for anesthetic
management.
Problem-Based Learning Discussions | L020
Placenta Percreta: Preparation and Management
9-10:15 a.m. | Room 343-345
Cathleen Peterson-Layne M.D., Ph.D.
Refresher Course Lecture | 107
Postpartum Hemorrhage
9:15-10:15 a.m. | RiverGate
Jill Mhyre M.D.
A practical approach to clinical management and systems
preparation will be presented for postpartum hemorrhage.
Poster Discussions | PD12-1
Obstetric Anesthesia: Cesarean Delivery
10-11:30 a.m. | Room 243
Problem-Based Learning Discussions | L029
Labor Analgesia and Postpartum Tubal Ligation in a Patient with a
History of Spinal Instrumentation
12:30-1:45 p.m. | Room 343-345
Michael Hofkamp M.D.
Poster Presentations | PO12-2
Obstetric Anesthesia: Labor Analgesia, Patient Safety and
Miscellaneous
1-3 p.m. | Hall B1-Area D
Refresher Course Lecture | 116
Anesthetic Management of the Preeclamptic Patient
2:45-3:45 p.m. | RiverGate
Joy Hawkins M.D.
This RCL will discuss diagnosis and peripartum management of
severe preeclampsia and eclampsia based on co-management
with the obstetric team.
Problem-Based Learning Discussions | L043
Anesthesia for an Hypoplastic Left Heart Syndrome Parturient
3:30-4:45 p.m. | Room 343-345
David Mann M.D.
Problem-Based Learning Discussions | L044
Anesthetic Management of Cesarean Delivery for a Parturient With
Previous Myocardial Infarction and Coronary Artery Stents
3:30-4:45 p.m. | Room 343-345
Daria Moaveni M.D.
Refresher Course Lecture | 123
Dural Puncture and Headache: Let’s Keep It the Patient’s
Headache
4-5 p.m. | Room E-1
Robert Gaiser M.D.
This refresher course will identify various factors that place the
patient at risk for the development of a headache following dural
puncture. If the patient experiences dural puncture, the means for
decreasing the risk of developing a headache will be discussed
followed by the means for the management of the headache.
Barriers to the initiation and implementation of these measures
will be identied as well as means to address these barriers.
Sunday, October 12
Problem-Based Learning Discussions | L048
Cesarean Delivery in a Patient With Hypertrophic Obstructive
Cardiomyopathy
7:15-8:30 a.m. | Room 343-345
Jaime Aaronson M.D. Stephanie Goodman M.D.
EDUCATION

85
Point-Counterpoint | PC07
Combined Spinal-Epidural Labor Analgesia: Forevermore or
Nevermore?
8-9:30 a.m. | Room 211-213
Cynthia Wong M.D.
Epidural analgesia has been the traditional technique of neuraxial
labor analgesia. In the mid 1990’s combined spinal-epidural (CSE)
began growing in popularity. Both techniques have advantages
and disadvantages, particularly for specic patient populations.
Despite many studies, there continues to be controversy in
clinical practice as to the appropriateness of routinely using the
CSE technique for labor analgesia. In this Point-Counterpoint
session, two experienced obstetric anesthesiologists with argue/
discuss the advantages and disadvantages of both techniques,
using evidenced-based data to support their arguments. Barbara
Scavone M.D. PRO: Forevermore Robert Gaiser M.D. CON:
Nevermore
Problem-Based Learning Discussions | L063
Just Another Day on Labor and Delivery: Morbid Obesity and
Preeclampsia
9-10:15 a.m. | Room 343-345
Regina Fragneto M.D.
Problem-Based Learning Discussions | L067
Labor Analgesia and Postpartum Tubal Ligation in a Patient With a
History of Spinal Instrumentation
9-10:15 a.m. | Room 343-345
Michael Hofkamp M.D.
Refresher Course Lecture | 207
Neurologic Complications of Neuraxial Anesthesia in Obstetrics
9:15-10:15 a.m. | RiverGate
David Wlody M.D.
This refresher course lecture will discuss the most common
causes of neurologic injury in obstetric neuraxial anesthesia,
including infectious, chemical, and traumatic etiologies. It will also
discuss the common obstetric nerve palsies and how these can
be distinguished from anesthetic causes of neurologic decits.
Prevention, evaluation, and treatment of neurologic injury will be
discussed.
90 Minute Panel | PN54
Cutting-Edge Technologies and Point-of-Care Devices to Improve
Care of the Obstetric Patient
10-11:30 a.m. | Room 208-210
Brendan Carvalho FRCA
Cutting-Edge Technologies and Point-of-Care Devices to Improve
Care of the Obstetric Patient
This panel will discuss new technologies and point-of-care devices
that can be used to improve the anesthetic management of
obstetric patients. The lectures will cover devices to aid epidural
insertion and maintenance of labor analgesia, technologies to
assess blood loss and hemodynamic parameters during obstetric
hemorrhage, and point-of-care devices to assess hematologic and
coagulation function. Roshan Fernando M.B.,Ch.B. Devices and
Techniques to Aid Epidural Insertion and Optimize Maintenance of
Labor Analgesia Brendan Carvalho F.R.C.A. Cutting-Edge Technology
to Assess Blood Loss and Hemodynamic Parameters during
Obstetric Hemorrhage Alexander Butwick M.B., B.S. Point-of-Care
Devices for Assessing Hematologic and Coagulation Indices
Refresher Course Lecture | 214
Hail Caesar: Anesthesia for Cesarean Delivery
10:30-11:30 a.m. | Room E-1
Lawrence Tsen M.D.
Accounting for a signicant portion of global births annually,
cesarean delivery has a number of anesthetic implications. The
trends, medications, management and controversies associated
with cesarean delivery anesthesia will be discussed.
Problem-Based Learning Discussions | L078
Anesthesia for an Hypoplastic Left Heart Syndrome Parturient
12:30-1:45 p.m. | Room 343-345
David Mann M.D.
Problem-Based Learning Discussions | L079
Anesthetic Management of Cesarean Delivery for a Parturient With
Previous Myocardial Infarction and Coronary Artery Stents
12:30-1:45 p.m. | Room 343-345
Daria Moaveni M.D.
Problem-Based Learning Discussions | L081
Critical Management of a Parturient With Inuenza Progressing to
ARDS
12:30-1:45 p.m. | Room 343-345
Vernon Ross M.D.
120 Minute Panel | PN12
Perioperative Considerations for Ex Utero Intrapartum Treatment
Procedures: Principles, Pitfalls and Progress
1-3 p.m. | Room 225-227
Mark Rollins M.D., Ph.D.
Anesthesia for EXIT Procedures: Perioperative Considerations
The EX utero Intrapartum Treatment (EXIT) procedure allows life
saving interventions to be performed on fetuses with disorders
that would otherwise acutely compromised survival after birth.
During the EXIT procedure, the fetus remains supported by the
placental unit with adequate oxygenation and perfusion, while
surgical repair and resuscitation interventions are performed in a
controlled manner. The EXIT procedure has become more common
outside of academic fetal care centers and requires signicant
multidisciplinary coordination to optimize outcomes. This panel
will provide an overview of the guiding principles, indications,
anesthetic, and perioperative considerations key to the EXIT
procedure. Potential complications during an EXIT procedure
and management strategies will also be discussed. The role
of the anesthesiologist in the multidisciplinary approach to the
fetal patient will be emphasized. Anne Boat M.D. Intraoperative
Fetal Monitoring Debnath Chatterjee M.D. EXIT Complications:
Prevention and Management Olutoyin Olutoye M.D., M.Sc., F.A.A.P.
Evolving Indications for EXIT Procedures
Refresher Course Lecture | 225
State of the Art Labor Analgesia
1:45-2:45 p.m. | Room E-2
Kenneth Nelson M.D.
This refresher course lecture is designed to bring the audience
up to date with the latest advances in labor analgesia including
technology, techniques, agents, and adjuncts.
SCHEDULE BY LEARNING TRACK
86
Refresher Course Lecture | 234
Anesthesia for Nonobstetric Surgery and Procedures
3-4 p.m. | La Nouvelle Ballroom AB
Yaakov Beilin M.D.
This Refresher Course Lecture will provide the information
required to safely anesthetize the pregnant patient presenting
for nonobstetric surgery. The physiologic changes of pregnancy
and how it impacts on the mother, as well as the concepts of
teratogenicity and apotosis as it relates to the developing fetus
will be discussed. An anesthetic plan for safely anesthetizing the
mother will be presented.
Problem-Based Learning Discussions | L094
Anesthetic Considerations for the Jehovah’s Witness Patient
Undergoing Trial of Labor After Cesarean Delivery (TOLAC)
3:30-4:45 p.m. | Room 343-345
Chawla LaToya Mason M.D.
Problem-Based Learning Discussions | L095
Placenta Percreta: Preparation and Management
3:30-4:45 p.m. | Room 343-345
Cathleen Peterson-Layne M.D., Ph.D.
Monday, October 13
Problem-Based Learning Discussions | L104
She Was Advised Not to Get Pregnant and She Did: Pulmonary
Hypertension and Pregnancy
7:15-8:30 a.m. | Room 343-345
Tanya Lucas M.D.
120 Minute Panel | PN20
Maternal Mortality in the Developed World: What Should the
Anesthesiologist Know?
8-10 a.m. | Room 225-227
The panel will be clinically relevant with lectures that include
evidence based recommendations that can be used by the
audience in their practices to provide state of the art patient care.
Robert D’Angelo M.D.
Maternal Mortality Overview
John Sullivan M.D., M.B.A. Amniotic Fluid Embolism Alicia Dennis
MBBS, Ph.D., PGDipEcho, FANZCA Peripartum Cardiomyopathy
Arvind Palanisamy M.D., FRCA Maternal Sepsis
Problem-Based Learning Discussions | L128
A Parturient With Scoliosis and Harrington Rods
12:30-1:45 p.m. | Room 343-345
Allison Lee M.D.
Problem-Based Learning Discussions | L129
Anesthetic Considerations for the Jehovah’s Witness Patient
Undergoing Trial of Labor After Cesarean Delivery (TOLAC)
12:30-1:45 p.m. | Room 343-345
Chawla LaToya Mason M.D.
90 Minute Panel | PN66
Basic Considerations for the Occasional Obstetric Anesthesiologist
8-9:30 a.m. |Room 208-210
This panel will provide practical recommendations for managing
the parturient in labor and cesarean delivery. Protocols for
providing the optimal labor anesthetic as well as way to trouble-
shoot a failed epidural catheter will be discussed. An anesthetic
plan for the routine, urgent and stat cesarean delivery will be
presented.
Yaakov (Jake) Beilin, M.D. Failed Labor Epidural: Where, Oh
Where Did My Pesky Catheter Go? Manuel C. Vallejo, Jr., M.D.
Labor Epidural Analgesia Triple Threat: Keeping Pain Score Low,
Satisfaction Scores High, and Your Reputation Awesome! Chawla La
Toya Mason, M.D. Cesarean Delivery Anesthesia: Should Protocols
for Elective, Urgent and Stat Be the Same?
Problem-Based Learning Discussions | L147
Critical Management of a Parturient With Inuenza Progressing to
ARDS
3:30-4:45 p.m. | Room 343-345
Vernon Ross M.D.
Problem-Based Learning Discussions | L148
A Parturient Presenting in Premature Labor With Single-Ventricle
Physiology Complicated by Breech Presentation and Paroxysmal
Supraventricular Tachycardia: What’s Your Labor Management
Plan?
3:30-4:45 p.m. | Room 343-345
Manuel Vallejo M.D.
90 Minute Panel | PN77
What Are They Doing and Why? Obstetrics for the Anesthesiologist
3:30-5 p.m. | Room 225-227
Barbara Scavone M.D.
This is a 90-minute panel intended to increase the obstetrics
knowledge base for those anesthesiologists who administer
obstetric anesthesia. Fetal assessment will include the most
recent ACOG categories of fetal heart rate interpretation, which
many anesthesiologists are unfamiliar with. Delivery decision-
making will cover topics such as the risks and benets of a trial
of labor after cesarean, vaginal versus cesarean delivery of a
singleton breech presentation, etc. The indications for magnesium
and best practice for the administration of oxytocin will also be
presented. McCallum Hoyt M.D., M.B.A. Fetal Assessment Michaela
Farber M.D., M.S. Delivery Decision-Making Richard Smiley M.D.,
Ph.D. Pharmacology of Common Obstetric Drugs
Tuesday, October 14
Poster Presentations | PO12-1
Obstetric Anesthesia: Cesarean Delivery
10 a.m.-12 p.m. | Hall B1-Area C
Refresher Course Lecture | 414
Improving Patient Safety on the Labor and Delivery Suite through
Changes in Culture, Education, and Communication
11:45-12:45 p.m. | Room E-1
David Birnbach M.D., M.P.H.
This lecture will review suboptimal outcomes in obstetric patients
that were related to poor communication, and will show methods
to improve communication skills, thereby improving patient safety.
Videos of simulated encounters will be shown to demonstrate
principles of good and bad teamwork as well as communication
on the L&D suite. Examples of the importance of situational
awareness will also be addressed.
EDUCATION

87
Problem-Based Learning Discussions | L173
Cesarean Delivery in a Patient With Hypertrophic Obstructive
Cardiomyopathy
12:30-1:45 p.m. | Room 343-345
Jaime Aaronson M.D. Stephanie Goodman M.D.
Problem-Based Learning Discussions | L187
Neurologic Complications Following Epidural Placement - How to
Differentiate and Manage?
12:30-1:45 p.m. | Room 343-345
Kelly Elterman M.D. David Hepner M.D.
Poster Discussions | PD12-2
Obstetric Anesthesia: Labor analgesia, outcomes, hemorrhage and
miscellaneous
3-4:30 p.m. | Room 244
Problem-Based Learning Discussions | L158
A Parturient With Scoliosis and Harrington Rods
7:15-8:30 a.m. | Room 343-345
Allison Lee M.D.
Refresher Course Lecture | 403
Neuraxial Labor Analgesia and Pregnancy Outcome: Fact and
Fiction
8-9 a.m. | Room E-2
Cynthia Wong M.D.
Labor is a complex physiologic process. The mechanisms
responsible for the progress of labor are not well understood. The
effects of analgesia on the progress and outcome of labor are of
concern to anesthesiologists, obstetricians, and parturients. This
lecture will review the available data on the effects of neuraxial
analgesia on the progress of labor and mode of delivery.
Refresher Course Lecture | 408
Strategies to Optimize Cesarean Delivery Analgesia
9:15-10:15 a.m. | Room E-1
Brendan Carvalho F.R.C.A.
Cesarean delivery surgery causes moderate to severe
postoperative pain that is often incompletely relieved by current
pain management protocols. The lecture will discuss the role
of neuraxial opioids, NSAIDS, acetaminophen, gabapentin,
wound inltration, transversus abdominis plane block, and
future analgesic options to optimize post-cesarean analgesia
and improve functional recovery. Analgesic drug exposure in
breastfeeding infants, and techniques to minimize the transfer of
analgesics into breast milk will also be discussed.
Problem-Based Learning Discussions | L167
She Was Advised Not to Get Pregnant and She Did: Pulmonary
Hypertension and Pregnancy
9-10:15 a.m. | Room 343-345
Tanya Lucas M.D.
Problem-Based Learning Discussions | L172
A Parturient Presenting in Premature Labor With Single-Ventricle
Physiology Complicated by Breech Presentation and Paroxysmal
Supraventricular Tachycardia: What’s Your Labor Management
Plan?
9-10:15 a.m. | Room 343-345
Manuel Vallejo M.D.
SCHEDULE BY LEARNING TRACK
88
Pain Medicine
Saturday, October 11
Subspecialty Panels | 602
(ASRA) Advancing Safety and Risk Management Strategies in Pain
Medicine
7-8:15 a.m. | Room 238-239
David Provenzano M.D.
Infection and Interventional Pain Medicine - Prevention,
Identication, and Management
Pain specialists utilize risk analysis and management strategies
when providing and performing non-interventional and
interventional treatment. This subspecialty panel will highlight
three areas in chronic pain management where risk management
strategies are critical to optimizing outcomes: 1) infection control,
2) anticoagulation, and 3) opioid related central and obstructive
sleep apnea. For each of these three areas the associated risks
for both practitioners and patients will be identied and evidence-
based risk management and mitigation strategies will be provided.
Related practice guidelines for each area will also be covered.
Honorio Benzon M.D. Anticoagulation Guidelines for Interventional
Pain Procedures Eugene Viscusi M.D. Opioids Risks with Obstructive
and Central Sleep Apnea
Problem-Based Learning Discussions | L010
Worsening Back Pain: To Inject or Not to Inject That Is the
Question
7:15-8:30 a.m. | Room 343-345
Tariq Malik M.D.
Refresher Course Lecture | 105
Clinical Evaluation and Treatment of Neuropathic Pain
8-9 a.m. | Room 260-262
Timothy Lubenow M.D.
This lecture will address thehistoricak and physical exam
necessary to evaluate complaints of neuropathic pain. The tool
of skin punch biopsy will be highlighted. Treatment algorythm
utilizing recent guidelines regarding treatment alternatives will be
discussed.
90 Minute Panel | PN40
Back Pain and Health Care Redesign: Preparing for Accountable
Care
8-9:30 a.m. | Room 228-230
James Rathmell M.D.
Back Pain and Costs of Care
Amultidisciplinary team from Massachusetts General Hospital has
teamed up to create a coordinated approach to spine care. This
session will present the actual advances epereienced in the rst
year of this coordinated care, aimed at preparing to care effectively
for patients with back pain in this era of health care reform.
Christopher Gilligan M.D., M.B.A. Back Pain and Inpatient
Hospitalization Joseph Schwab M.D., M.S. Back Pain and Algorithms
of Care
Poster Presentations | PO03-2
Chronic and Cancer Pain
8-10 a.m. | Hall B1-Area A
Hands-on Workshop | 804
Acupuncture Workshop
8-11 a.m. | Room 333-334
Yuan-Chi Lin M.D.
Acupuncture is among the oldest healing arts and medical
practices in the world. A part of traditional Chinese medicine,
which is currently widely used in the United States, the practice
restores and maintains health through the stimulation of specic
acupuncture points in the body. Participants will have ample time
to participate in hands-on demonstrations of acupuncture and
related techniques. Joseph Chiang M.D. Brenda Golianu M.D.
Priscilla Harrell M.D. Eric Hsu M.D. Anjana Kundu M.D. Tat Leang
Lee M.B., B.S. Mei-Ying Liang M.D. Yue-Pang Mok M.D. Emily
Ratner M.D. Lynn Rusy M.D. Yung-Fong Sung M.D. Rosalie Tassone
M.D., M.P.H. Cynthia Tung M.D. Shu-Ming Wang M.D.
Hands-on Workshop | 801
Ultrasound Guided Injections-Live Models: Basic Techniques
8 a.m.-12 p.m. | Room 275-277
Hariharan Shankar M.B.
The participants will gain experience with hands-on demonstration
of sonoanatomy, and technique in the performance of stellate
ganglion, cervical and lumbar MBB, facet joint and shoulder
injections. This session will cover ultrasound-guided techniques
for those more experienced in ultrasound guidance under the
tutelage of world renowned expert. Dalia Elmofty, M.D. Intercoastal,
TAP John Hanlon, M.D. Hip and Suprascapular Nerve Injection Anne
Marie McKenzie Brown, M.D. Piriformis, Knee, Ravi Shah, M.D.
Ilioinguinal/Illiohypogastric, Genitofemoral, LFCN
Cadaver Workshops | CA01
Spinal Injections With Fluoroscopy- Cadaver: Basic Techniques
8 a.m.-12 p.m. | Room 271-273
Maunak Rana M.D.
This workshop will consist of a lecture followed by participants
moving throughfour stations to gain knowledge of uoroscopically-
guided interventional pain techniques and the performance
of these interventional techniques at the cadaveric stations.
The learner will be introduced to, review and perform common
uoroscopically guided lumbar/sacral injections for spine related
pain. Injections will include Lumbar Translaminar, Lumbar
Transforaminal, and Caudal Epidural Steroid Injections; Lumbar
Medial Branch/Facet Injections/Radiofrequency Ablation therapies;
Sacroiliac Joint Injections; S1 Transforaminal Injections. Anke
Bellinger M.D. Lumbar MBB/Facet Joint/RFA Paul Hilliard M.D.
Lumbar TFESI/SNRB Khalid Malik M.D. SIJ, S1 TFESI Vikram Patel
M.D. Caudal and Lumbar ESI
Refresher Course Lecture | 111
The Role of Perioperative Physicians in Prevention of Chronic Pain
After Surgery
9:15-10:15 a.m. | Room 260-262
Asokumar Buvanendran M.D.
This refresher course lecture will provide an overview of the risk
factors and the role of the perioperative physician in preventing
chronic pain after surgery.
Poster Discussions | PD03-1
Chronic and Cancer Pain
10-11:30 a.m. | Room 245
EDUCATION

89
Clinical Forum | CF02
Complications in Pain Medicine and Preventive Strategies
1-2:30 p.m. | Room 211-213
Hariharan Shankar M.B.,B.S.
Complications Related to Medications
One of the dreaded factors in pain medicine is treatment related
complications. This may signicantly affect the patient, traumatize
the physician and result in increased health care costs. A better
understanding of the complications may help to initiate preventive
strategies and improve outcome. This discussion will outline
all the potential complications that are likely in pain medicine
practice and suggest preventive strategies. In addition, when
a bad outcome does occur unfortunately, the management
options to decrease the damage will also be outlined. Michael
Erdek M.D. Opioid Related Complications Dalia Elmofty M.D.
Complications in Interventional Pain Practice John Rowlingson
M.D. Management Strategies When Complications Occur
120 Minute Panel | PN07
Evidenced Based Chronic Pain Management in Children and
Adolescents:Is There Evidence or Is It Bias?
1-3 p.m. | Room 252-254
Santhanam Suresh M.D.
This panel will discuss the current evidence for management
of chronic pain in children including cognitive behavioral
management, neuropathic pain, headaches and the use of
complementary therapy by the thought leaders in pediatric pain.
Gary Walco Ph.D. Cognitive Behavioral Management Elliot Krane
M.D. Neuropathic Pain Charles Berde M.D., Ph.D. Headaches Yuan-
Chi Lin M.D. Complementary Therapy
Hands-on Workshop | 808
Ultrasound Guided Injections- Live Models: Advanced Techniques
1-5 p.m. | Room 275-277
Philip Peng M.B.B.S.
Anatomy and relevant techniques for common major joint
injections, muscle injections, and truncal peripheral nerve blocks.
Live model workshop only. Anuj Bhatia, M.D. Lumbar MBB and
Facets Roderick Finlayson, M.D. Cervical MBB and Facets Neilish
Soneji, M.D. Shoulder Daneil Warren, M.D. Stellate Ganglion
Cadaver Workshops | CA02
Spinal Injections With Fluoroscopy-Cadaver: Advanced
Techniques(Cervical/Thoracic)
1-5 p.m. | Room 271-273
Timothy Lubenow M.D.
Advanced Fluorscopically Guided Epidural and Medial Branch
Injections of the Thoracic and Cervical Spine
Workshop featuring advanced uoroscopic injection techniques
of the cervical and thoracic spine. Thoracic/cervical epidural
steroid injection and thoracic/cervical medial branch block or
radiofrequency ablation approaches covered. Kayode Williams
M.B., B.S. Station 1: Cervical Epidural Steroid Injection Salahadin
Abdi M.D. Station 2: Thoracic ESI and TFESI Kenneth Candido M.D.
Station 3: Cervical MBB/RFA David Maine M.D. Station 4: Thoracic
MBB/RFA
Refresher Course Lecture | 113
Complex Regional Pain Syndrome: What’s New?
1:30-2:30 p.m. | Room E-3
Richard Rauck M.D.
This will be a review but also update on diagnosis and treatment
trends in complex regional pain syndrome.
Seminar | 811
Spinal Imaging for the Pain Medicine Physician
2-4 p.m. | Room 338-339
Wyndam Strodtbeck M.D.
Identifying Features in a Spine MRI Relevant for a Pain Physician
At the conclusion of this session, participants will understand
commonly used spine imaging modalities, normal spine images,
systematic reading of spine MRI and interpretation of spine
imaging relevant to a pain practitioner.This session offers a unique
opportunity to learn the commonly used imaging modalities during
the practice of pain medicine, the interpretation of those images
from a Radiologists perspective and their clinical signicance
from an experienced pain practitioner. This session is ideal
for those considering the practice of pain medicine as well as
those experienced pain practitioners attempting to enhance their
knowledge. Hossam Hamda M.D. Reading a CT Myelogram Andrew
Klein M.D. Reading a Spine MRI
90 Minute Panel | PN46
Radiofrequency Ablation for Spinal Pain: Techniques to Optimize
Success
3:30-5 p.m. | Room 225-227
Kevin Vorenkamp M.D.
Cervical Radiofrequency Ablation: Needle Orientation in Relation to
the Medial Branch Anatomy
In this panel Drs. Provenzano, Pino and Vorenkamp will review the
anatomy relevant to RF lesioning of the sacroiliac joint, cervical
spine and lumbar spine. Normal lesion characteristics with various
RF techniques (RFA, pulsed RF, cooled RFA, multi lesion probe) will
be discussed as well as techniques to modify lesion shape and
size. Finally, clinical evidence demonstrating successful integration
of techniques into clinical practice will be discussed. David
Provenzano M.D. Lumbar Medial Branch RFA and Factors Affecting
Lesion Size Carlos Pino M.D. Sacroiliac Joint RFA-Techniques and
Controversies
Sunday, October 12
Oral Presentations | OR03-1
Chronic and Cancer Pain
8-9:30 a.m. | Room 243
Point-Counterpoint | PC06
Long-Term Opioid Treatment for Chronic Non-Malignant Pain
8-9:30 a.m. | Room 203-205
Gary Brenner M.D.. Ph.D.
PRO: The Long-term Use of Opioids is an Acceptable Treatment
Option for Chronic Non-malignant Pain
This session will explore the evidence and distribution of chronic
non-malignant pain and the different treatment options including
the long-term use of opioids. Using a point-counterpoint format,
the will argue for or against the long-term use of opioids for
chronic non-malignant pain, review the current literature as well as
limitations and discuss potential options and future perspectives.
Rene Przkora M.D., Ph.D. CON: Long-term Treatment of Chronic
Non-malignant Pain With Opioids is Not Acceptable
SCHEDULE BY LEARNING TRACK
90
90 Minute Panel | PN101
Neuropathic Pain: From Mechanisms to Outcomes
8-9:30 a.m. | Room 252-254
Jianguo Cheng M.D.
(1) Classication and Mechanisms of Neuropathic Pain; (2)
Interventional Approaches to Neuropathic Pain
Neuropathic pain affects millions of Americans, leading to
individual suffering, short and long term disability, diminished
quality of life, and high cost to society. Healthcare charges
were threefold higher for painful neuropathic disorder patients
compared with matched control subjects. Managing neuropathic
pain is challenging because many neuropathic conditions are
refractory to various treatments. In this educational session we
will bring together experts to review the denition, classication,
mechanisms, assessment and diagnosis, and evidence of
treatment options of neuropathic pain. The focus is on evidence-
based decision making to improve the outcomes of clinical
practice. The listed objectives will be achieved by reviewing
the basic science, evidence-based clinical guidelines, and
management strategies of common neuropathic pain conditions.
The participants will be able to gain competence in applying a
comprehensive approach to neuropathic pain management that
includes nonpharmacological, pharmacological, and interventional
therapies. The key to safe, efcacious, and cost-effective
management of neuropathic pain is to have a multimodal strategy
because neuropathic pain rarely responds well to monotherapy.
Timothy Lubenow M.D. Treatment Approaches to Neuropathic Pain
Philip Peng M.B.B.S. IV Therapy and Ketamine for Neuropathic
Pain
Cadaver Workshops | CA03
Introduction to Ultrasound and Fluoroscopic-Guided Techniques for
Chronic Pain Management: Live Models and Cadavers
8 a.m.-12 p.m. | Room 271-273
David Provenzano M.D.
Ultrasound for Pain Medicine
This session will highlight the procedural skills required for axial
and nonaxial interventional pain procedures performed under both
ultrasound and uoroscopic guidance. Interpretation of various
skeletal and soft tissue structures as seen with uoroscopy and
ultrasound, as well as proper angles and views used to perform
interventional pain management procedures will be taught. In
addition, this session integrates a cadaver station which will
provide direct comparison for specic interventional procedures
performed under both visualization techniques. The ability to view
dynamic images using ultrasound in live models and practicing
needle placement on cadavers offers an added benet. Srinivas
Chiravuri M.D. Ultrasound Guided Interventional Pain Procedures
Robert Goldstein M.D. Fluoroscopic Guided Pain Procedures
Amaresh Vydyanathan M.D. Fluoroscopic Guided Pain Procedures
Maunak Rana M.D.
Cadaver Workshops | CA04
Head and Neck Blocks (Ultrasound and Fluoroscopy)-Cadaver and
Live Models
8 a.m.-12 p.m. | Room 275-277
Miles Day M.D.
Head and Neck Blocks Using Fluoroscopy and Ultrasound
Advanced pain intervention workshop featuring blocks of the
head and neck. Cervical facet injections/medial branch blocks,
stellate ganglion blocks, trigeminal blocks, and greater occipital
nerve blocks are covered. Both uoroscopic and ultrasonographic
approaches are demonstrated where applicable. Antoun Nader
M.D. Station 1. Ultrasound for Stellate and V2/V3 Roderick
Finlayson M.D. Station 2. Ultrasound for Greater Occipital Nerve
(GON) and Cervical Facets Magdalena Anitescu M.D. Station 3.
Fluoro for Cervical MBB/Facets James North M.D. Station 4. Fluoro
for Stellate, Trigeminal Blocks
Refresher Course Lecture | 210
Modern Concepts in Spinal Cord Stimulation
9:15-10:15 a.m. | Room E-3
Timothy Deer M.D.
Neurostimulation is a rapidly advancing and changing therapy for
the treatment of chronic pain. Data is rapidly becoming available
with new treatment modalities and methods of stimulation.
It is important for clinicians to understand the applications,
patient selection and potential risks of such therapies to insure
proper utilization and successful treatment outcomes. Clinical
practice remains highly diverse, based on clinician experience
and perceived patient needs. A review of the data on these new
therapies is vital to insure proper patient selection and therapeutic
utilization. This session will focus on the data and application of
three new advances in Neurostimulation including: Burst, dorsal
root ganglion and High Frequency.Specic recommendations
will be reviewed, accompanied by new survey data from multiple
sources describing current practice, clinician views of the best
practices recommendations, and their willingness and barriers
to change. Discrepancies between current practice and the
consensus recommendations will be identied along with practical
considerations for practice implementation. A highly interactive
session is planned to include the views of the audience in a
mutual exchange designed to mitigate these discrepancies.
Refresher Course Lecture | 216
Head and Neck Pain: A Clinical Approach
10:30-11:30 a.m. | Room E-3
Samer Narouze M.D., Ph.D.
This refresher course lecture entails a review of newest (ICHD-3)
classications of head and neck pain. The diagnostic criteria for
various head and neck pain disorders will be analyzed. This will
help physicians to formulate a practical multimodal treatment plan
for such pain disorders including when to utilize Botox injections
and other various interventional and neuromodulatory techniques.
EDUCATION

91
Refresher Course Lecture | 220
Radiofrequency Ablation for the Treatment of Spine Pain:
Understanding the Basic Principles and Clinical Applications
12:30-1:30 p.m. | Room E-3
David Provenzano M.D.
This refresher course will provide an overview on the utilization
of radiofrequency for the treatment of pain conditions including
cervical and lumbar facet and sacroiliac joint related pain.
Particular areas that will be discussed will include the current
level of efcacy and safety data, patient selection, and the
electrophysiological principles of thermal, pulsed, and cooled
probe radiofrequency. The technical limitations and methods to
modulate lesion size will be described. Equipment advancements
for radiofrequency ablation techniques will also be evaluated.
Problem-Based Learning Discussions | L075
Opioid-Induced Hyperalgesia Tolerance and Chronic Postsurgical
Pain: A Dilemma Complicating Postoperative Pain Management
12:30-1:45 p.m. | Room 343-345
Dalia Elmofty M.D.
Poster Presentations | PO03-1
Chronic and Cancer Pain
1-3 p.m. | Hall B1-Area B
Seminar | 816
Physical Exam Workshop for Pain Physicians
1-4 p.m. | Room 346-347
Brian Starr M.D.
This workshop focuses on training in practical and important
musculoskeletal, neurological physical examination skills for
the comprehensive pain physician. Examination skills focus on
musculoskeletal exam of the cervical and lumbar spine, shoulder,
hip, and sacroiliac joint. Additionally neurological exam of the
head, upper extremities, and lower extremities are covered.
Ming-Chih Kao M.D. Neurological Exam: Lower Extremity Thomas
Kotsonis M.D. Musculoskeletal Exam: l Spine, Hip, SI Joint
Ameet Nagpal M.D. Neurological Exam: Head and Upper
Extremities
Hands-on Workshop | 814
Ultrasound Guided Musculoskeletal Injections- Live Models: Beyond
Corticosteroids
1-5 p.m. | Room 271-273
James Modir M.D.
A 4 hour workshop designed for practitioners interested in
learning the role of non-steroid injectables, relevent gross
anatomy corellated with sonographic imaging, and review common
ultrasound guided musculoskeletal injections on live models.
Peter Cheng D.O. Einar Ottestad M.D. Wyndam Strodtbeck M.D.
Cadaver Workshops | CA05
Radiofrequency Ablation of the Spine, Sacrum, and Lumbar Disc
1-5 p.m. | Room 275-277
Maxim Eckmann M.D.
Radiofrequency Ablation of the Spine, Sacrum, and Lumbar Disc
Advanced interventional pain management workshop featuring
uoroscopically guided radiofrequency (RF) lesions for the
treatment of a variety of spine related pain syndromes, including
cervical facetogenic pain, lumbar facetogenic pain, lumbar
discogenic pain, and sacroiliac pain. Workshop complements
introductory knowledge of injection techniques for prognostic
blockade of these structures where applicable. Conventional
monopolar RF and cooled RF technique demonstrated where
applicable. Esther Benedetti M.D. Station 1: Cervical Facet
Neurotomy Advanced interventional pain management workshop
featuring uoroscopically guided radiofrequency (RF) lesions for the
treatment of a variety of spine related pain syndromes, including
cervical facetogenic pain, lumbar facetogenic pain, lumbar
discogenic pain, and sacroiliac pain. Workshop complements
introductory knowledge of injection techniques for prognostic
blockade of these structures where applicable. Conventional
monopolar RF and cooled RF technique demonstrated where
applicable. Esther Benedetti, M.D. Station 1: Cervical Faret
Neurotomy Ali Mchaourab M.D. Station 2: Lumbar Facet Neurotomy
Michael Erdek M.D. Station 3: Disc Biacuplasty Carlos Pino M.D.
Station 4: Sacroiliac Joint Neurotomy
Problem-Based Learning Discussions | L093
Worsening Back Pain: To Inject or Not to Inject That Is the Question
3:30-4:45 p.m. | Room 343-345
Tariq Malik M.D.
Refresher Course Lecture | 235
Cancer Pain Management in 2014
4:15-5:15 p.m. | RiverGate
Oscar De Leon-Casasola M.D.
The key to the success of cancer pain treatment is determining the
exact source of the pain. Multimodal Pharmacological therapy is
successful in the great majority of patients. For those who cannot
tolerate drug titration or optimal doses do not result in adequate
analgesia, the use of interventional techniques has resulted in
adequate analgesia in the great majority of patients. A description
of the different pharmacological and interventional techniques, and
the caveats in implementing these therapies will be presented.
Monday, October 13
Refresher Course Lecture | 302
Therapeutic Epidural Injections: Safety Considerations and Evidence
Basis
8-9 a.m. | Room E-1
Marc Huntoon M.D.
This session will describe the current uses of various
corticosteroids and other emerging anti-inammatory agents for
the treatment of radiculitis. In addition, recent developments
have reinforced the need for safety strategies to limit potential
complications of both procedurally-related neurological injury and
infections. Participants who do these procedures should consider
attending this session.
SCHEDULE BY LEARNING TRACK
92
120 Minute Panel | PN22
Palliative Care and the Anesthesiologist
8-10 a.m. | Room 252-254
Mihir Kamdar M.D.
Where Anesthesia, Palliative Care, and Modern Healthcare Collide:
Understanding the Importance of Perioperative Palliative Care
Palliative Care is centered on optimizing symptom management,
assisting with medical decision making, and addressing ethical
conict in patients with advanced illness. Tasked with the wellbeing
of patients during the perioperative period, anesthesiologists
are often faced with palliative care issues. They routinely engage
in discussions of perioperative use of advanced directives,
handle ethical dilemmas in the OR, and have expertise in pain
management. Despite this unique position, anesthesiologists
receive little training in palliative care. This panel will discuss the
role of anesthesiologists in perioperative palliative care, educate
attendees on navigating difcult conversations around goals of
care and breaking bad news, discuss ethical dilemmas in the OR,
and highlight the role of anesthesiologists in managing refractory
pain at the end of life. Jacob Strand M.D. What Should I Do When
Things Don’t Go Well?: Breaking Bad News and Honoring Advanced
Directives in the OR Shane Volney M.D. Refractory Pain at the End-
of-Life: The Unique Role of the Anesthesiologist Elizabeth Rickerson
M.D. To Stand Up or Not? Ethical Issues in the Perioperative Setting
and the Surgical ICU
Poster Presentations | PO03-3
Chronic and Cancer Pain
8-10 a.m. | Hall B1-Area B
Problem-Based Learning Discussions | L115
Opioid-Induced Hyperalgesia Tolerance and Chronic Postsurgical
Pain: A Dilemma Complicating Postoperative Pain Management
9-10:15 a.m. | Room 343-345
Dalia Elmofty M.D.
Refresher Course Lecture | 308
The Strain in Pain Lies Mainly in the Brain: Lessons Learned from
the Neuroimaging of Pain
9:15-10:15 a.m. | Room E-1
Sean Mackey M.D., Ph.D.
Chronic pain affects over 100 million Americans costing have
a trillion dollars per year. Recently the CNS has been shown to
play a pivotal role in the generation and maintenance of chronic
pain. Investigators have used central neuroimaging tools to
open windows into the brain to better characterize the neural
correlates of pain. They have discovered that there are brain
regions involved with pain including the somatosensory cortex,
prefrontal cortex, anterior cingulate cortex, and insular cortex. We
will review the current neuroimaging data for pain and describe
their abnormalities in frontal and limbic brain systems associated
with acute and chronic pain. At the end of this talk the participant
will have a better appreciation of the neural plasticity involved with
pain and its therapeutic implications.
Seminar | 818
Practical Pain Medicine Coding, Compliance and Workow
Strategies for 2014
9-11 a.m. | Room 276-277
Kevin Vorenkamp M.D.
Station 2: Billing and Compliance-Avoiding Fraud, Maximizing
Potential
At the conclusion of this session, participants will demonstrate
an appreciation for the factors contributing to a successful and
compliant pain medicine practice. In this interactive workshop,
participants will rotate through all 3 stations for case discussions
on various aspects of pain medicine coding, billing and practice
management. Focus will be on developing a sustainable pain
medicine practice through efcient workow patterns. Additional
emphasis will focus on commonly asked questions regarding ICD-
10 coding, compliance and fraudulent billing examples (and how
to avoid them). Sharon Merrick M.S., CCS-P Station 1: ICD-10 How
Is It Impacting Your Practice? Problems, Solutions Kayode Williams
M.D., M.B.A. Station 3: Clinical Workow: Strategies to Maximize
Efciency AND Patient Satisfaction
Refresher Course Lecture | 317
Improving Safety Through Use of Diagnostic Imaging and Image
Guidance in Pain Medicine
12:30-1:30 p.m. | La Nouvelle Ballroom AB
James Rathmell M.D.
This session is designed to review the use of diagnostic imaging
and image-guided needle placement during the treatment of
patients with chronic and cancer-related pain with an emphasis on
how best to use these technologies to improve safety.
Poster Discussions | PD03-2
Chronic and Cancer Pain
1-2:30 p.m. | Room 244
90 Minute Panel | PN69
Management of Chronic Pain: A Review of Treatment Modalities
1-2:30 p.m. | Room 220-222
Magdalena Anitescu M.D.
Infusion Therapies in Chronic Pain Management
This panel will review the essential treatment modalities in
chronic pain. The 4 s will focus on the following topics: injections
(neuraxial, sympathetic, head and neck, etc), infusions (ketamine,
lidocaine, etc) , surgery (intrathecal pumps, stims, etc) and
destructive/restorative procedures (mild, IDET, coblation,
radiofrequency, etc); this will provide an excellent review for
the practitioner of the current treatment modalities in pain
management. Daniel Warren M.D. Needles, Images and Beyond:
Injections in Interventional Pain Management Salim Hayek M.D.,
Ph.D. Surgical Procedures in Interventional Pain Management
Refresher Course Lecture | 319
Interventional Pain Procedures in Patients on Anticoagulants
1:45-2:45 p.m. | Room E-1
Honorio Benzon M. D.
The RCL will review the reasons for increased bleeding from
medications used in pain management (antidepressants,
anticonvulsants, NSAIDs) and from certain pain procedures
(e.g. spinal cord stimulation); discuss the case reports of spinal
hematoma after pain procedures in patients who were on aspirin
only, on no anticoagulants, or when the coagulation studies were
normal; identify recommended intervals between drug stoppage
and neuraxial procedures as it pertain to the new anticoagulants;
and, explain the upcoming ASRA guidelines on pain procedures in
patients on anticoagulants.
EDUCATION

93
Refresher Course Lecture | 324
Algorithmic Approach to Back Pain
3-4 p.m. | RiverGate
Nagy Mekhail M.D.,Ph.D.
The lecture will describe the anatomy of lumbar spaces and
possible pain generators. The differential diagnosis of Discogenic
pain, Lumbar Radiculopathy, Lumbar Spinal Stenosis, Lumbar
Facets syndrome as well as Sacroiliac Joint dysfunction will be
discussed. Also, the state-of-the-art minimally invasive techniques
to treat such conditions will be demonstrated.
Point-Counterpoint | PC12
Should We Discontinue the Use of Opioids for the Treatment of
Chronic Pain?
3-4:30 p.m. | Room 203-205
Rafael Miguel M.D.
PRO: A Reassessment of Their Risks and Benets
There has been considerable public activity arguing to discontinue
use of long-term opioids for chronic pain management (e.g.,
PROP). There is mounting evidence of increased mortality with
doses above 50-100mg/day morphione equivalents. Furthermore,
chronic pain patienst appear to report similar pain evaluation
scores years after starting their opioid course of therapy as
compared to pre-opioiod treatment. A reassessment of the “there
is no upper limit of opioid therapy” mentality popularized in the
90’s is appropriate. Oscar De Leon-Casasola M.D. CON
Tuesday, October 14
Refresher Course Lecture | 427
Healthcare Reform and Pain Medicine -Impact and Strategies for
Future Success
2:15-3:15 p.m. | Room E-2
Richard Rosenquist M.D.
This lecture will examine the impact of healthcare reform on the
practice of pain medicine and propose strategies to succeed in the
transition to a lower cost model of healthcare delivery.
SCHEDULE BY LEARNING TRACK
94
Pediatric Anesthesia
Saturday, October 11
Problem-Based Learning Discussions | L012
Application of Pediatric Advanced Life Support for Managing a
Patient With a Debrillator Who Develops an Intraoperative Cardiac
Arrest
7:15-8:30 a.m. | Room 343-345
David Young M.D., MBA
90 Minute Panel | PN41
What Anesthesiologists Need to Know About Resuscitating Kids in
the OR
8-9:30 a.m. | Room 255-257
Jayant Deshpande M.D., M.P.H.
This Panel will provide an up-to-date review of the most common
etiologies of perioperative cardiac arrest in children, describe
effective treatment algorithms, and provide practical strategies
for specic pediatric perioperative cardiac arrest scenarios.
Donald Shaffner Jr., M.D. How to Prepare: What Causes Pediatric
Perioperative Cardiac Arrest? Eugenie Heitmiller M.D. Pediatric
Perioperative Cardiac Arrest Algorithms David Murray M.D.
Treatment for Specic Pediatric Perioperative Arrest Scenarios
(Laryngospasm, Prone Positioning, Local Anesthetic Toxicity, etc.)
Poster Presentations | PO15-1
Pediatric Anesthesia
8-10 a.m. | Hall B1-Area E
Hands-on Workshop | 806
Advanced Ultrasound Guided Pediatric Regional Anesthesia
Workshop
8-11 a.m. | Room 338-339
Amod Sawardekar M.D.
This workshop will teach practical skills and performance of
the most common peripheral nerve blocks in pediatric regional
anesthesia that have the most utility with the use of ultrasound.
The participant will better understand the underlying anatomy
of both the target nerves and the surrounding structures. Tarun
Bhalla M.D. Karen Boretsky M.D. Adrian Bosenberg M.B.,Ch.B. Jami
Eidem M.D. Richard Elliott M.D. Arjunan Ganesh M.B.B.S.
Andrea Huang M.D. Giorgio Ivani M.D. Manoj Karmakar M.B.,B.S.
Edward Mariano M.D. Santhanam Suresh M.D. Ravi Shah M.D.
Benjamin Walker M.D.
Problem-Based Learning Discussions | L016
Trials and Tribulations: Interventional Management for Recurrent
Complex Regional Pain Syndrome in Children
9-10:15 a.m. | Room 343-345
Stephen Hays M.D.
Problem-Based Learning Discussions | L024
Tonsillectomy and Adenoidectomy in a Child With Down Syndrome
More to It Than You Think!
9-10:15 a.m. | Room 343-345
Catherine Seipel M.D.
Problem-Based Learning Discussions | L004
When It Rains, It Pours; Large AVM Heart Failure Pulmonary HTN
and Now There Is V-tach!
12:30-1:45 p.m. | Room 343-345
Christina Diaz M.D.
Problem-Based Learning Discussions | L031
Why Does My Patient Scheduled for Endoscopic Sinus Surgery Have
Severe Groin Pain?
12:30-1:45 p.m. | Room 343-345
Kirk Lalwani M.D. Christine Martin M.D.
Poster Discussions | PD15-1
Pediatric Anesthesia: Cardiac
3-4:30 p.m. | Room 244
Problem-Based Learning Discussions | L039
Wake Up Your Surgery Is Not Over
3:30-4:45 p.m. | Room 343-345
Prabhakar Devavaram M.B.,B.S.
Problem-Based Learning Discussions | L041
I Passed Gas in the Operating Room. Are Volatile Agents Really
Silent and Deadly to Patients With Muscular Dystrophy?
3:30-4:45 p.m. | Room 343-345
Matthew Green M.D.
Refresher Course Lecture | 125
Pediatric Ambulatory Anesthesia: Challenges and Controversies
4-5 p.m. | Room E-3
Linda Mason M.D.
This RCL will deal with common ambulatory problems in pediatric
anesthesia including co-morbiditoes like OSA, obesity and
prematurity. In addition, a step by step approach from admission
to discharge of ambulatory surgery will be detailed.
Sunday, October 12
Refresher Course Lecture | 203
Current Controversies in Pediatric Anesthesia
8-9 a.m. | Room E-2
Lena Sun M.D.
This refresher course will deal with controversies that are
commonly encountered in pediatric anesthesia you encounter in
daily practice.
Hands-on Workshop | 812
Pediatric Airway Workshop
8-11 a.m. | Room 346-347
Narasimhan Jagannathan M.D.
This workshop will demonstrate a wide variety of pediatric airway
devices, and will offer the opportunity for participants to become
familiar and comfortable with each device through hands-on
practice. Jennifer Anderson M.D. John Fiadjoe M.D. Agnes Hunyady
M.D. Pete Kovatsis M.D. Mohamed Mahmoud M.B.,B.Ch. Vivian
Manying Yuen M.B.,B.S. Bruno Marciniak M.D. Maria Matuszczak
M.D. John McAllister M.D. Sydney Nykiel D.O. Patrick Olomu M.D.
Paul Reynolds M.D. Jalil Riazi M.D. Lisa Sohn M.D. Paul Stricker
M.D. Peter Szmuk M.D. Samuel Wald M.D. Michelle White M.D.
Problem-Based Learning Discussions | L065
I Passed Gas in the Operating Room. Are Volatile Agents Really
Silent and Deadly to Patients With Muscular Dystrophy?
9-10:15 a.m. | Room 343-345
Matthew Green M.D.
Problem-Based Learning Discussions | L072
Application of Pediatric Advanced Life Support for Managing a
Patient With a Debrillator Who Develops an Intraoperative Cardiac
Arrest
9-10:15 a.m. | Room 343-345
David Young M.D., MBA
EDUCATION

95
Refresher Course Lecture | 212
New Guidelines: Pediatric Advanced Life Support for the
Anesthesiologist
9:15-10:15 a.m. | La Nouvelle Ballroom AB
Eugenie Heitmiller M.D.
This RCL will address the current updated pediatric Advanced
Life support guidelines. In addition, management of a variety of
common arrythmias in neonates and children will be addressed.
90 Minute Panel | PN55
Pediatric Adenotonsillectomy: Enhancing Quality and Efciency;
Ensuring Safety
10-11:30 a.m. | Room 217-219
Lynne Maxwell M.D.
This 90-minute panel will educate attendees how to care for
pediatric adenotonsillectomy patients in order to achieve safe and
efcient care. Deborah Schwengel M.D. Preoperative Assessment
and Decision-Making Ronald Litman D.O. Intraoperative Strategies
to Ensure Postoperative Safety and Efcient PACU Stay Kimmo
Murto M.D. Choosing Safe Postoperative Pain Management, in the
Hospital and at Home
Poster Presentations | PO15-2
Pediatric Anesthesia
10 a.m.-12 p.m. | Hall B1-Area E
Refresher Course Lecture | 217
Anesthesia for the Patient With Congenital Heart Disease for
Emergent Non-Cardiac Surgery: Are You Well Equipped?
10:30-11:30 a.m. | Room 260-262
Dean Andropoulos M.D.
This RCL will deal with children with congenital heart disease
corrected and non-corrected who are scheduled for emergent
surgery. Pharmacodynamics as well as vasoactive management
will be explained in detail for common congenital heart diseases.
Refresher Course Lecture | 219
Anesthetic Induced Neurotoxicity in Pediatric Patients: A Status
Update
12:30-1:30 p.m. | Room E-2
Randall Flick M.D., M.P.H.
This RCL will provide attendees with a case based approach to
common pediatric scenarios that may be encountered in any
practice setting. This RCL will include a description of the case,
review of the relevant literature and discussion of management
options.
Refresher Course Lecture | 221
Neonatal Emergencies: Simple Approach to Success
12:30-1:30 p.m. | Room 260-262
Samuel Wald M.D.
This refresher course will deal with common neonatal emergencies
that are encountered, their preoperative and intraoperative
management including airway and uid management.
120 Minute Panel | PN13
They Walk Among Us: Anesthesia for Adults With Pediatric Disease
1-3 p.m. | Room 228-230
Debra Morrison M.D.
Patients with structural or physiological congenital disease and/
or those born prematurely are now much more likely to live well
into adulthood and require surgery as adults, which may or may
not be related to the underlying disease. As these patients
become mature individuals, stigmata of the disease may become
far less apparent, but the signicance of the original diagnosis
may not diminish. Pediatric anesthesiologists who care for these
patients as children offer the benet of their experience to the
adult anesthesiologists who will inherit them. Edward Nemergut
M.D. Cystic Fibrosis Laura Diaz M.D. Congenital Heart Disease -
Structural Defects and Arrhythmias Claire Brett M.D. Ex-Premies
Richard Dsida M.D. Down Syndrome, Achondroplasia and other
Congenital Diseases Seen in Adult Patients
Hands-on Workshop | 823
Perioperative Pediatric Advanced Life Support Simulation
1-4 p.m. | Room 281
Scott Watkins M.D.
This simulation workshop will focus on Perioperative (Anesthesia-
Centric) PALS with content tailored to events unique to the
pediatric patient including emergencies of cardiac, pulmonary,
neurologic, metabolic, endocrine and toxin origin. The workshop
will begin with a 45-minute didactic and Q&A session. Simulation
sessions will follow with each scenario being 15 minutes in length
with a 25 to 30-minute debrief afterward that will focus on the
workshop objectives. A 5-minute break will be given between each
station. There will be 4 scenario-stations per workshop with each
station covering a different pediatric perioperative emergency.
Workshop attendees will manage each scenario as a team. There
will be a team leader and a rst responder at each station. The
other participants will ll scripted roles to which they will be
introduced (nurse, surgeon, tech, etc.) and one participant will play
the role of observer in order to give feedback to the team (along
with the facilitator). Cory Furse M.D. Elisabeth Hughes M.D. Erin
Pukenas M.D. Amanda Redding M.D. Laura Zeigler M.D.
Problem-Based Learning Discussions | L091
Why Does My Patient Scheduled for Endoscopic Sinus Surgery Have
Severe Groin Pain?
3:30-4:45 p.m. | Room 343-345
Kirk Lalwani M.D. Christine Martin M.D.
Problem-Based Learning Discussions | L096
Tonsillectomy and Adenoidectomy in a Child With Down Syndrome
More to It Than You Think!
3:30-4:45 p.m. | Room 343-345
Catherine Seipel M.D.
Monday, October 13
Poster Presentations | PO15-3
Pediatric Anesthesia
10 a.m.-12 p.m. | Hall B1-Area D
Clinical Forum | CF10
Anesthetic Safety in Newborns Can Be Achieved by Sticking to Little
Details
1-2:30 p.m. | Room 206-207
Susan Verghese M.D
1-day-old 33 week gestation baby admitted with TEF and VACTERL
association for repair. Songyos Valairucha M.D. Senthilkumar
Sadhasivam M.D. Carolyn Bannister M.D.
SCHEDULE BY LEARNING TRACK
96
90 Minute Panel | PN71
TIVA for TOTS
1-2:30 p.m. | Room 228-230
Zulqar Ahmed M.D., F.A.A.P.
Total Intravenous anesthesia TIVA in pediatric population is an
emerging and developing technique that has yet to reach its
full potential. In this panel we plan to cover the whole peri-
operativ scenario from obtaining intravenous access from new
and innovative ways in order to minimize the stress all the way
to a successful TIVA technique. Sam Sharar M.D. Positioning and
Distraction for IV Placement in Kids Gregory Schears M.D.
Topical Anesthesia and Imaging Techniques to Increase IV
Placement Success J. Ansermino M.B., B.Ch.TIVA in Kids - What
Works?
Problem-Based Learning Discussions | L123
Cardiovascular Collapse During Thoracoscopic Tracheoesophageal
Fistula Repair
12:30-1:45 p.m. | Room 343-345
Kimberly Blasius M.D.
Problem-Based Learning Discussions | L135
Using Advanced Trauma Life Support to Manage a Pediatric Trauma
Patient With Traumatic Brain Injury and Disclosure of Difcult News
After a Poor Outcome
12:30-1:45 p.m. | Room 343-345
David Young M.D., MBA
Refresher Course Lecture | 328
Airway Management in Pediatric Emergencies: The Tricks of the
Trade
3-4 p.m. | Room 260-262
Paul Reynolds M.D.
This refresher course will address airway intervention techniques
in infants and children when they encounter emergent situations
using current available techniques.
Problem-Based Learning Discussions | L106
A Child With Mitochondrial Disease and Propofol Allergy Who May
be Susceptible to Malignant Hyperthermia
7:15-8:30 a.m. | Room 343-345
Jayant Pratap M.B.,B.Ch.
Problem-Based Learning Discussions | L140 When It Rains It
Pours; Large AVM Heart Failure Pulmonary HTN and Now There Is
V-tach!
7:15-8:30 a.m. | Room 343-345
Christina Diaz M.D.
Poster Discussions | PD15-2
Pediatric Anesthesia: Miscellaneous
8-9:30 a.m. | Room 244
Problem-Based Learning Discussions | L121
It Is Just a Nosebleed Isn’t It? Anesthetic Considerations for
Unsuspected Pulmonary Hypertension
9-10:15 a.m. | Room 343-345
Shu Ming Wang M.D.
Tuesday, October 14
Subspecialty Panels | 610 (SPA)The Child With Congenital Heart
Disease Presenting for Non-Cardiac Surgery
7-8:15 a.m. | Room 238-239
Shobha Malviya M.D.
The Society for Pediatric Anesthesia panel will provide an
overview of the safe perioperative management for children with
congenital heart disease who present for non-cardiac surgery.
Important ndings on preoperative assessment will be identied
and strategies for optimizing the preoperative condition will be
discussed. A thorough and practical approach to perioperative
management of these patients will be outlined and stafng
challenges will be addressed. Chandra Ramamoorthy M.D.
Preoperative Assessment and Optimization - When Should We
Be Scared Bridget Pearce M.D. Intraoperative and Postoperative
Management - How to Do It with Finesse Dean Andropoulos M.D.,
M.H.C.M. Stafng Issues - When Should We Just Say No
Clinical Forum | CF12
In a Land Far Away From Home ... Remote Anesthetic Care for the
Medically Complex Pediatric Patient
8-9:30 a.m. | Room 206-207
Inger Aliason M.D.
This forum will explore the multitude of challenges associated with
provision of anesthetic care to the medically complex pediatric
patient in remote locations. Topics will inlcude, but not be limited
to, airway management, anesthetic techniques and medications,
radiation exposure and monitoring. Kirk Lalwani M.B., B.S., FRCA
Remote Anesthetic Care for Pediatric PET/CT Keira Mason M.D.
Anesthetic Care of a Child With Duchenne’s Muscular Dystrophy for
MRI Judith Handley M.D. Anesthetic Care for Radiation Therapy of a
Child With Cardiomyopathy
Hands-on Workshop | 832
Point of Care: Novel Use of Ultrasonography in Everyday Pediatric
Anesthesia Practice
8-11 a.m. | Room 353-354
Santhanam Suresh M.D.
The use of point of care ultrasonography for diagnostic and
therapeutic assessments for pediatric patients. This includes use
of the ultrasound for vascular access, airway anatomy, detection
of pneumothorax, and cardiac imaging. Dean Andropoulos M.D.
Wendy Binstock M.D. Vincent Chan M.D. James Di Nardo M.D. Dawit
Haile M.D. Courtney Alan Hardy M.D. Narasimhan Jagannathan
M.D. Bruno Marciniak M.D. Scott Markowitz M.D., FAAP Amod
Sawardekar M.D. Gregory Schears M.D. Luis Zabala M.D.
Problem-Based Learning Discussions | L163
Wake Up Your Surgery Is Not Over
9-10:15 a.m. | Room 343-345
Prabhakar Devavaram M.B.,B.S.
Refresher Course Lecture | 409
Acute Postoperative Pain Management in Infants and Children:
Size Does Matter!
9:15-10:15 a.m. | Room E-2
Patrick Birmingham M.D.
This RCL will deal with common surgical pediatric patients
including neonates and infants undergoing common orthopedic,
urology, pediatric and ENT surgery. Pharmacology of commonly
used medication will be discussed with an evidenced based
approach to care.
EDUCATION

97
Poster Discussions | PD15-3
Pediatric Anesthesia: General
10-11:30 a.m. | Room 244
Problem-Based Learning Discussions | L177
Trials and Tribulations: Interventional Management for Recurrent
Complex Regional Pain Syndrome in Children
12:30-1:45 p.m. | Room 343-345
Stephen Hays M.D.
Problem-Based Learning Discussions | L182
A Child With Mitochondrial Disease and Propofol Allergy Who May
be Susceptible to Malignant Hyperthermia
12:30-1:45 p.m. | Room 343-345
Jayant Pratap M.B.,B.Ch.
120 Minute Panel | PN31
Editor’s Picks in Pediatric Anesthesiology 2014
1-3 p.m. | Room 255-257
Constance Houck M.D.
This session features editors from each of the prominent
Anesthesia journals discussing the publications within their
journal that have particular importance for anesthesiologists
caring for children. Alan Jay Schwartz M.D., M.S. Anesthesiology,
James DiNardo, M.D., Anesthesia and Analgesia, Andrew Davidson,
M.D., Pediatric Anesthesia, Robin Cox, M.D., Canadian Journal of
Anesthesia
Poster Presentations | PO15-4
Pediatric Anesthesia
1-3 p.m. | Hall B1-Area E
Refresher Course Lecture | 426
Anesthetic Management of Common Pediatric Emergencies
2:15-3:15 p.m. | Room E-1
Franklyn Cladis M.D.
This RCL will deal with common pediatric emergencies in infants
and children. The RCL will allow you to navigate your course
through common emergencies that you see in every day practice.
Problem-Based Learning Discussions | L185
Cardiovascular Collapse During Thoracoscopic Tracheoesophageal
Fistula Repair
3:30-4:45 p.m. | Room 343-345
Kimberly Blasius M.D.
Problem-Based Learning Discussions | L193
It Is Just a Nosebleed, Isn’t It? Anesthetic Considerations for
Unsuspected Pulmonary Hypertension
3:30-4:45 p.m. | Room 343-345
Shu Ming Wang M.D.
Problem-Based Learning Discussions | L194
Using Advanced Trauma Life Support to Manage a Pediatric Trauma
Patient With Traumatic Brain Injury and Disclosure of Difcult News
After a Poor Outcome
3:30-4:45 p.m. | Room 343-345
David Young M.D., MBA
SCHEDULE BY LEARNING TRACK
98
Professional Issues
Saturday, October 11
Problem-Based Learning Discussions | L001
A High Risk Patient for Low Risk Outpatient Surgery: Is There Value
in a Surgical Home for a Patient Going Home?
7:15-8:30 a.m. | Room 343-345
Jeanna Blitz M.D.
Problem-Based Learning Discussions | L003
Creating a Culture of Professionalism in Your Department
7:15-8:30 a.m. | Room 343-345
Saundra Curry M.D.
Point-Counterpoint | PC01
Life in the Time of Consolidation: Is Bigger the New Better?
8-9:30 a.m. | Room 203-205
James Grant M.D.
A team of two physicians on either side, facilitated by a 5th
physician serving as moderator, will argue the pros and cons of
the consolidation trend in contemporary anesthesia practice.
Audience participation will be encouraged. Steven Hattamer M.D.
CON Zachary Deutch M.D.CON Michael Simon M.D. PRO Michael
Hicks M.D. PRO
90 Minute Panel | PN103
Quality and Safety Challenges: Raising the Bar on Overseas Surgical
Care Trips
8-9:30 a.m. | Room 206-207
Richard Gillerman M.D., Ph.D.
Quality and Safety Related Policies and Procedures: Unique
Requirements for Providing Safe Perioperative Care During
Overseas Surgical Care Trips
The panel will present diverse topics to help the participant, learn
strategies for ensuring quality and enhancing safety on various
types of overseas surgical care trips; recognize those types of trips
that may best achieve quality and safety goals or put them at risk;
appreciate the value of measuring and reporting trip outcomes
and its relationship to improving patient care; and identify specic
policies and procedures likely to achieve quality and improve
safety on overseas surgical care trips. Mark Singleton M.D.
Quality and Safety Considerations: Differences Between Direct
Patient Care and Teaching Style Overseas Surgical Care Trips
Faye Evans M.D. Quality and Safety Risks and Benets: Pros and
Cons of Practicing Outside the ASA Guidelines During Overseas
Surgical Care Trips Richard Dutton M.D., M.B.A. Quality and Safety
Metrics: What We Need to Learn to Improve Care on Overseas
Surgical Care Trips
90 Minute Panel | PN38
Change Management in Collaborative Quality Improvement Projects
(CQIP)
8-9:30 a.m. | Room 220-222
Mike Schweitzer M.D., M.B.A.
Using Change Management in CQIP
Inuence and drive change through the methodologies of Change
management and Project Management. This panel will provide
an overview of the Statewide Surgical Quality Collaboratives in
place and in development with special emphasis on benets to
patients and physicians. Compare these CQIPs in terms of clinical
effectiveness, outcome improvement, and nancial benets. We
will describe how to collect patient outcome data and turn this
into meaningful information to permit continuous assessment
and improvement of the quality of care, identifying and sharing of
Leading Practices, and prevent complications of care that can all
result in savings. David Mackey M.D. Successful Statewide Surgical
Quality Collaboratives Robert Hsiung M.D. Change Data into
Information for Comparative Effectiveness
90 Minute Panel | PN39
Leaning In: Women in Leadership Roles
8-9:30 a.m. | Room 225-227
Rekha Chandrabose M.D.
Organizing Women at the Local and National Levels
This panel will discuss the role of women in the eld of
anesthesiology. Using the expertise of its panelists, it will address
the current statistics on women in anesthesiology, increasing the
presence of women leaders in the eld of anesthesiology and
discuss methods to successfully address the issues facing women
anesthesiologists. In addition, topics will include mentorship and
access to leadership and business training. Information will be
available regarding instituting a national organization for women in
anesthesiology as well as support for local organizations. Jane C.K.
Fitch M.D. Leading and Advocating: Reections As President of the
American Society of Anesthesiologists and Chair of an Academic
Anesthesiology Department Cynthia Wong M.D. The Status of
Women in Anesthesiology: Identifying Opportunities for Leadership
Elizabeth Rebello M.D. Mentoring Women in Anesthesiology:
Organizing Women at the Local and National Levels
Poster Presentations | PO14-2
Patient Safety and Practice Management
8-10 a.m. | Hall B1-Area D
Seminar | 803
Mastering Perioperative Stress and Burnout: Exploring Methods of
Essential Mind-Fitness, Developing Resilience at Work
8-11 a.m. | Room 281-282
Kenneth Sapire M.D.
Stress and Burnout in the Perioperative Period: Wellness at Work
This will be an opportunity for direct exposure to understanding
and experiencing the Mindtness techniques. Motivation: Stress
and Burnout are more than buzzwords or journal topics. Our lives
caring for patients and being compassionate can be complicated
by multiple factors. Attention will be focused on illuminating
the vital value and inter related nature of diverse contemplative
and mind tness practices and how these can inuence our
worldview,identity,values,ethics, and way of life. Essentially we will
teach the art of wisdom and resilience at work. We will discuss the
relationship of this practice and associated information to brain
neuroplasticity and explore an integrative model that illuminates
the dynamic synergy and interdependence of these different types
of meditative and associated activities. Joel Levey Ph.D Wisdom at
Work, Mindtness and Contemplative Practice for This Day and Age
Michelle Levey M.A Mindtness and Developing Resilience at Work
for This Day and Age
EDUCATION

99
Problem-Based Learning Discussions | L013
Infection Prevention for the Anesthesia Professional: What is the
Least I Should Know and How Do I Apply It to My Practice?
9-10:15 a.m. | Room 343-345
Richard Beers M.D.
Problem-Based Learning Discussions | L018
To Coerce or Not to Coerce: What Are the Questions?
9-10:15 a.m. | Room 343-345
Norma Klein M.D.
Problem-Based Learning Discussions | L033
Burned Out Anesthesiologist: Practice Competence and Colleagues
12:30-1:45 p.m. | Room 343-345
Sergey Pisklakov M.D.
Problem-Based Learning Discussions | L035
Anesthetic Options for Patients Undergoing Dialysis Access
Procedures
12:30-1:45 p.m. | Room 343-345
Derek Woodrum M.D.
Oral Presentations | OR14-1
Patient Safety and Practice Management
1-2:30 p.m. | Room 245
120 Minute Panel | PN03
Setting Up a Perioperative Surgical Home
1-3 p.m. | Room 208-210
Zeev Kain M.D., M.B.A.
Change Management and Dissemination of the PSH Concept
This panel will provide an overview of the operational issues
involved in setting up a perioperative surgical home. Addressed will
be the perspectives of academic practice, private practice, large-
group practice and a health care system. This newly developed
perioperative model will emphasize physician-led, collaborative
care of the surgical patient, with cost-effective involvement of
non-physician practitioners, during all phases of the perioperative
continuum. Arthur Boudreaux M.D. An Academic Perspective
Michael Simon M.D. A Large Group Perspective Mark Schneider
M.D. A Private Practice Perspective Mike Schweitzer M.D., M.B.A.
A Health System Perspectives
120 Minute Panel | PN05
Whose Guidelines and Practice Parameters Apply to
Anesthesiologists?
1-3 p.m. | Room 225-227
John Butterworth IV, M.D.
Some Problems with Guidelines
This panel will feature a description of best practices for
guideline development and will illustrate how poorly constructed,
conicting guidelines can serve to confuse rather than guide good
clinical practice. Jeffrey Apfelbaum M.D. Best Practices: The ASA
Guideline/Practice Parameter Process Terese Horlocker M.D. How
Anesthesia Organizations Other Than ASA Prepare Guidelines
Martin London M.D. How Other Specialties Prepare Guidelines
Beverly Philip M.D. Nonphysician Groups and Their Guidelines and
Their Processes Gene Peterson M.D., Ph.D. Do Guidelines and
Practice Parameters Improve Quality and Safety?
Poster Presentations | PO11-1
History and Education:Challenges: Present and Future
1-3 p.m. | Hall B1-Area C
Oral Presentations | OR11-1
History and Education: Novel Ways to Teach and Learn
3-4:30 p.m. | Room 243
Problem-Based Learning Discussions | L047
Hold My Compass: Tools and Tips So That YOU Don’t Get Lost in the
EP Lab
3:30-4:45 p.m. | Room 343-345
Mark Weiss M.D.
90 Minute Panel | PN49
Governmental Inuences Over Health Care: Lessons Learned From
Working on Capitol Hill
3:30-5 p.m. | Room 255-257
Andrew Gettinger M.D.
The Stimulus Bill of 2010 - Far Reaching Impact on Medical Care
Includng Meaningful Use and HIPAA Privacy Rules
Three anesthesiologists with experience working on Capitol Hill
will provide insights into policies affecting anesthesiologists: cost/
outcomes; meaningful use of HIPAA; pain and opioid legislation.
Michael Oleyar D.O. The War is Over but the Fight Continues:
National and Local Efforts Against Prescription Opioid Abuse
Catherine Scholl M.D. Healthcare Economics: An Anesthesiologists’
Point of View
Sunday, October 12
Problem-Based Learning Discussions | L057
Burned Out Anesthesiologist: Practice Competence and
Colleagues
7:15-8:30 a.m. | Room 343-345
Sergey Pisklakov M.D.
Problem-Based Learning Discussions | L058
The Impaired Anesthesiologist: More Than Just Drugs and Alcohol
7:15-8:30 a.m. | Room 343-345
Gregory Rose M.D.
Problem-Based Learning Discussions | L060
Anesthetic Options for Patients Undergoing Dialysis Access
Procedures
7:15-8:30 a.m. | Room 343-345
Derek Woodrum M.D.
Oral Presentations | OR14-2
Patient Safety and Practice Management
8-9:30 a.m. | Room 245
Problem-Based Learning Discussions | L071
Anesthesiologists and Terminal Live Organ Donation: You Want Me
to Do What?
9-10:15 a.m. | Room 343-345
Richard Wolman M.D.
Problem-Based Learning Discussions | L119
My Patient With a DNR Order Arrested in the OR! Now What?
9-10:15 a.m. | Room 343-345
Juliann Hobbs, M.D., M.P.H.
Problem-Based Learning Discussions | L120
When the Patient Just Says No
9-10:15 a.m. | Room 343-345
Juliann Hobbs, M.D., M.P.H.
SCHEDULE BY LEARNING TRACK
100
Refresher Course Lecture | 208
Decision Making Errors in Anesthesiology
9:15-10:15 a.m. | Room E-1
Marjorie Stiegler M.D.
Medical errors are common despite expertise and skill. This
course will explore the cognitive landscape in which our medical
decisions are made, with an emphasis on patient safety.
Decisions are subject to a variety of subconscious and nonrational
processes, which may lead to mistakes made despite “knowing
better.” Memory reconstruction error, bias, heuristic, loss aversion,
preference, regret, and other hardwired phenomena contribute
to this landscape, but fortunately, strategies for counterbalacing,
prevention, and recovery exist. Up to 80% of medical errors are
related to delayed or incorrect diagnosis. Utlization of checklists
and other decision support may not work well if the algorithm
is inappropriate, due to an incorrect working diagnosis. This
important intersection is explored.
90 Minute Panel | PN56
Beating Back Burnout: Strategies for Career Longevity and
Improved Patient Care
10-11:30 a.m. | Room 220-222
Mary Ann Vann M.D.
This panel will provide a review of burnout and its impact on
patient care and the health of the provider as evidenced in the
literature. Strategies for improving physician well-being in a variety
of practice environments will be highlighted as well as educational
interventions aimed at fostering resiliency and preventing burnout
at all stages. Amy Vinson M.D. Why We Need to Talk about This
Neil Farber M.D., Ph.D. Fostering Well-Being in a Busy Practice
Haleh Saadat M.D. Educational Intervention - DO’s and DON’Ts
90 Minute Panel | PN57
Not All That Glitters is Gold- How Do I Judge Quality from My
Experience as a Surgical Outpatient?
10-11:30 a.m. | Room 225-227
Armin Schubert M.D.
The panel will assemble experts in the emerging interface between
patient experience and clinical quality assessment. As patients
are asked to bear increasing nancial responsibilities, they are
becoming more aware of quality and their proxy perception of
the latter recommendations and questions for assessing patient
experience will be discussed. This theme will be developed for
outpatient sedation, regional anesthesia and the post-procedure
period. The role of big data, such as the SCOR and NACOR
databases will be discussed, especially in light of the emerging
requirements for ambulatory facilities to report CG-CAPS data to
Medcare. Brian Parker M.D. What Is Quality Sedation- From Whose
Perspective? William Sumrall III, M.D. Patient Experience: What
Can Our Patients Tell Us? Gildasio De Oliveira M.D., M.Sc. How
Do Patients Fare After Surgery at the ASC: Recovery and Beyond
Lucinda Everett M.D. Benchmarking Quality and Patient Experience
in Outpatient Anesthesia: Role of National Databases
90 Minute Panel | PN59
Professionalism - An International Perspective
10-11:30 a.m. | Room 255-257
Saundra Curry M.D.
Professionalism- Why Bother?
Internationals will describe how professionalism is applied
in their environments. This can help improve both global
understanding of medical issues and enhance patient outcomes.
Sadek Beloucif M.D. Europe: From Dedication to Professionalism
Mohamed Ben Ammar M.D. Africa - Why Hasn’t My Continent
Embraced This Concept? Eiichi Inada M.D. Wandering Japanese
Anesthesiologists
Poster Presentations | PO14-1
Patient Safety and Practice Management
10 a.m.-12 p.m. | Hall B1-Area B
Problem-Based Learning Discussions | L073
Do You Want to Present a PBLD at the 2015 ASA Meeting? This
PBLD Session Could Help You
12:30-1:45 p.m. | Room 343-345
Sanjay Bhananker M.B., B.S.
Problem-Based Learning Discussions | L077
To Coerce or Not to Coerce: What Are the Questions?
12:30-1:45 p.m. | Room 343-345
Norma Klein M.D.
Problem-Based Learning Discussions | L083
Hold My Compass: Tools and Tips So That YOU Don’t Get Lost in the
EP Lab
12:30-1:45 p.m. | Room 343-345
Mark Weiss M.D.
120 Minute Panel | PN09
Patients Do the Darnedest Things: Tales From the Anesthesia
Incident Reporting System
12:30-2:30 p.m. | Room 211-213
Richard Dutton M.D., M.B.A.
This panel will be led by the Director of the Anesthesia Quality
Institute, and will consist of a series of clinical vignettes
abstracted from the Anesthesia Incident Reporting System. Each
case presentation will be followed by panelist commentary based
on two themes: how the event illustrates patterns and biases
in human cognition; and how to turn such an event into positive
improvements in anesthesia practice. Systems-based thinking
about adverse events (as opposed to individual blame and
shame) will be emphasized. I expect the audience to learn both
from the events themselves (which will be selected to illustrate
current knowledge gaps about emerging threats) as well as from
the discussion about how to think about them. My panelists
are well-published experts in this eld, and skilled and popular
presenters. This panel will also lend itself well to use of an
Audience Response System, if available. Marjorie Stiegler M.D.
Human Cognition during Complex Decision Making Avery Tung M.D.,
F.C.C.M. How to Turn Incidents into Action
Refresher Course Lecture | 128
Human Errors in Medicine: What They Should Mean to Patients,
Providers, and the Public
1:30-2:30 p.m. | E-2
Robert Lagasse M.D.
This Refresher Course Lecture will provide an overview of
human errors by anesthesia providers and their contribution
to perioperative morbidity and mortality. Participants will be
familiarized with a structured review process and the pitfalls of
applying such a process to judging clinical competence in accord
with regulatory requirements. Methods for dealing with victims will
also be discussed, including disclosure to patients, and providing
coping mechanisms for providers as second victims.
Poster Discussions | PD11-1
History and Education:Pioneers of Anesthesia
1-2:30 p.m. | Room 244
Poster Presentations | PO11-2
History and Education:Evaluation: Strategies and Resources
1-3 p.m. | Hall B1-Area D
EDUCATION

101
Refresher Course Lecture | 228
Building a Quality Management System for Meaningful Use
1:45-2:45 p.m. | La Nouvelle Ballroom AB
John Allyn M.D.
The learner will understand the key principles that should guide the
construction and management of an effectice QMS. Specically,
how to keep the department’s QMS separate from provider
privileging will be discussed. Resources presently available
to assist with this work will be discussed. Finally,examples,
management of the interface with AQI, and future directions will be
discussed.
Problem-Based Learning Discussions | L059
When the Patient Just Says No
3:30-4:45 p.m. | Room 343-345
Sarah Smith M.D.
Problem-Based Learning Discussions | L085
A High Risk Patient for Low Risk Outpatient Surgery: Is There Value
in a Surgical Home for a Patient Going Home?
3:30-4:45 p.m. | Room 343-345
Jeanna Blitz M.D.
90 Minute Panel | PN64
Limits of Care: Ethical Issues in the Current Technological
Environment
3:30-5 p.m. | Room 228-230
Paul Barash M.D.
Limits of Care: Ethical Issues in the Current Technological
Environment (Joint Cardiac, Pediatric, and Obstetric Panel)
[Economic issues are implied] Robert Sladen M.B.,Ch.B., FCCM
Limits of Care in Heart Failure and Transplantation Lisa Leffert M.D.
Mother or Baby? A Choice Amy Mesa-Jonassen M.D. Limits of
Care with Congenital Anomalies
Refresher Course Lecture | 237
Mythbusters Episode: Economic Issues of Anesthesia Care
4:15-5:15 p.m. | Room E-2
Amr Abouleish M.D, M.B.A.
This lecture will discuss in detail four common myths about the
economics of anesthesia care: 1.Focusing on turnover time will
improve OR throughput; 2.Because anesthesia revenue includes
time, anesthesia providers prefer longer surgeries; 3.Going from
physician-only stafng to medical direction stafng will reduce
stafng costs; 4.Using per provider (aka FTE) measurements allow
for accurate benchmarking of productivity.
Monday, October 13
Subspecialty Panels | 607
(SEA) Technology Today: Testing, Training and Learning
7-8:15 a.m. | Room 238-239
Ira Todd Cohen M.D., M.Ed.
It’s a Brave New World
Technological advancements and their effect on medical education
and physician evaluation will be discussed by a panel of experts.
Christine Park M.D. Simulation: From Mannequins to MOCA®
Annette Mizuguchi M.D., Ph.D. Web 2.0: The Virtual Learning (and
Exam) Environment Nina Deutsch M.D. Platforms: Launching Pads
for Exploration
Problem-Based Learning Discussions | L100
Giving Feedback: How to Support the Defensive Learner
7:15-8:30 a.m. | Room 343-345
Yulia Ivashkov M.D.
Refresher Course Lecture | 304
Tired of Not Being Taken Seriously? How Professionalism Affects
You
8-9 a.m. | Room E-3
Saundra Curry M.D.
Issues in professionalism occur daily but are often ignored. This
lecture will highlight how professionalism affects everything we do
and how lapses may harm our patients and our own physical and
mental health.
120 Minute Panel | PN23
Embracing Quality Improvement: Key Steps You Can Take Today to
Improve Yourself, Your Department and Your Hospital
8-10 a.m. | Room 255-257
David Zvara M.D.
The approach to Quality Improvement (QI) can either be Individual-
directed or Systems-directed. This session will focus on these
two approaches of QI as they pertain to a healthcare system as
well as to the routine practice of Anesthesiology. Aligning patient
care and quality improvement across a healthcare system will
be addressed. The process of developing a quality improvement
program in a Department of Anesthesiology will be highlighted.
Additionally, the aspects of incorporating QI into residency training
will be discussed. Lastly, Practice Performance Assessment
and Improvement (PPAI) program, which is now a component of
Maintenance of Certication in Anesthesiology (MOCA), will be
addressed. Armin Schubert M.D., M.B.A. Aligning Patient Care and
Quality Improvement in Your Hospital John Allyn M.D. Developing a
Quality Improvement Program in a Department of Anesthesiology
Harendra Arora M.B.,B.S. Quality Improvement As a Key Component
of the Residency Training: How to Train the Next Generation?
Matthew McEvoy M.D. Practice Performance Assessment and
Improvement As a Component of MOCA. What Data Should I
Collect? Where Do I Begin?
Poster Presentations | PO11-3
History and Education: How Far We Have Come
8-10 a.m. | Hall B1-Area D
Poster Presentations | PO14-5
Patient Safety and Practice Management
8-10 a.m. | Hall B1-Area A
Refresher Course Lecture | 307
Ethics in the Real World
9:15-10:15 a.m. | RiverGate
Jeffrey Jacobs, M.D.
Poster Presentations | PO14-3
Patient Safety and Practice Management
10 a.m.-12 p.m. | Hall B1-Area C
Refresher Course Lecture | 312
Chemical Dependency and Anesthesiology
12:30-1:30 p.m. | RiverGate
John Tetzlaff M.D.
This refresher course will discuss the history of addiction to
anesthesia drugs by anesthesia providers, describe the incidence,
chemical and molecular mechanisms, causes, and strategies for
detection and prevention. It will discuss the most current data
about the preferred drugs of abuse for anesthesia providers,
as well as strategies for electronic auditing to detect diversion.
This risks to patients and other providers associated with drug
diversion will be presented. The nal topic discussed will be
prevention, which will include the positives and negatives for
random and “for cause” urine toxicology. The limits of random
testing will be identied.
SCHEDULE BY LEARNING TRACK
102
Problem-Based Learning Discussions | L103
How to Create and Moderate a Great Problem-Based Learning
Discussion (PBLD)
12:30-1:45 p.m. | Room 343-345
Kirk Lalwani M.D.,F.R.C.A
Problem-Based Learning Discussions | L124
Do You Want to Present a PBLD at the 2015 ASA Meeting? This
PBLD Session Could Help You
12:30-1:45 p.m. | Room 343-345
Sanjay Bhananker M.B., B.S.
Problem-Based Learning Discussions | L126
How Not to End Up on the Nightly News: Safe Injection Practices
12:30-1:45 p.m. | Room 343-345
Vilma Joseph M.D.
Problem-Based Learning Discussions | L134
Anesthesiologists and Terminal Live Organ Donation: You Want Me
to Do What?
12:30-1:45 p.m. | Room 343-345
Richard Wolman M.D.
120 Minute Panel | PN24
Milestones: Setting a High Bar or Barely Clearing the Hurdle?
12:30-2:30 p.m. | Room 203-205
Randall Schell M.D., M.Ed.
This panel will give a brief review of the Milestones and the
ACGME NAS as well as the reasons behind the implementation
of this new system. The challenges of using the Milestones for
assessment will be discussed. This will be followed by a detailed
presentation of how to consider the upper and lower bounds of
learner assessment in the Milestones system. Finally, how this
system can or will relate to the goal of training perioperative
physicians will be presented. Glenn Woodworth M.D. Reasons for
the Milestone System and Challenges with Using the Milestones
as Metrics Susan Martinelli M.D. A Tale of Two Limits: Upper
and Lower Bounds of Assessment in the Milestones and NAS
Matthew McEvoy M.D. A Way Forward: Toward the Goal of Excellent
Perioperative Physicians
Oral Presentations | OR11-2
History and Education: How Do Know What We Teach
1-2:30 p.m. | Room 245
Oral Presentations | OR14-3
Patient Safety and Practice Management
1-2:30 p.m. | Room 243
Seminar | 829
Physician Performance Assessment and Improvement: Practice Its
Power for Your Own Practice
1-4 p.m. | Room 356-357
Leslie Jameson M.D.
How to Apply the Physician Performance Assessment and
Improvement Model to Your Practice
Few clinicians have experience in personally developing activities
that assess, educate, and then reassess to achieve improvement
in a patient’s medical care. The major hurdle to change is realizing
what clinical actions and processes to evaluate in preparation
for altering daily practices. Under the tutelage of the PPAI
Editorial Board, workshop participants will select a topic, plan a
chart review, develop an educational program, then select ways
to execute practice changes. Large group instruction provides
the tools for small groups to practice each step. After each
brainstorming segment, groups will share their ideas and plans.
The goal is to provide tools to achieve consistent best practices.
A brief real life example will show application of the PPAI model to
MOC quality projects, and privileging process. Dawn Dillman M.D.
Applying PPAI Mohammed Minhaj M.D. Applying PPAI Francine
Yudkowitz M.D. Using PPAI
Clinical Forum | CF11
What Should You Do When You Don’t Think the Patient Should Have
Surgery at All?
3-4:30 p.m. | Room 206-207
Nancy Glass M.D., M.B.A.
When and How to Engage an Ethics Committee
The purpose of this case-based session is to offer
anesthesiologists a framework for approaching patients in whom
the medical and surgical goals may be unclear. Challenging cases
like these may cause signicant distress to patients, families and
physicians, and may lead to difcult therapeutic relationships and
inter-professional tension if they are poorly handled. Increasingly,
anesthesiologists are called upon to navigate these delicate
situations, taking into account the beliefs and knowledge of all
parties involved. We will use the cases described below to frame
the ethical and medical issues, commonly seen in both adult and
pediatric anesthesia. David Waisel M.D. Hospice Patients in the
Operating Room Stephen Hays M.D. Assessing Whether a Surgery
Is Appropriate for Patient and Family Goals Douglas Coursin
M.D. Very Ill Adult Patients: Deciding Whether to Proceed With
Surgery
Problem-Based Learning Discussions | L138
Infection Prevention for the Anesthesia Professional: What is the
Least I Should Know and How Do I Apply It to My Practice?
3:30-4:45 p.m. | Room 343-345
Richard Beers M.D.
Problem-Based Learning Discussions | L139
Creating a Culture of Professionalism in Your Department
3:30-4:45 p.m. | Room 343-345
Saundra Curry M.D.
Problem-Based Learning Discussions | L144
He’s 15, Needs This Operation and He’s DNR!
3:30-4:45 p.m. | Room 343-345
David Mann M.D.
EDUCATION

103
90 Minute Panel | PN79
Physician Impairment: Incidence, Identication, and Intervention
3:30-5 p.m. | Room 252-254
Keith Berge M.D.
Many conditions including substance abuse, mental illness,
physical disease, and consequences of aging often prevent an
anesthetist from optimally performing their critical duties and
maintaining the ASA core of vigilance and patient protection. Care
providers are often reluctant to seek treatment they need due
to perceived professional and social consequences. Physicians
are reluctant to report even signicantly impaired colleagues.
Physicians should comprehend the various types and presentation
of impairment including the consequences of these conditions
if left untreated. A consistent, planned, and well executed
intervention may encourage a colleague to seek further help, avoid
professional embarrassment, and maintain professional trust.
Ethan Bryson M.D. Impairment, Incompetency, and Distraction
in Anesthesia Providers John Tetzlaff M.D. Identication of the
Impaired Care Provider Michael Fitzsimons M.D. Professional
Intervention: Facing the Facts
Refresher Course Lecture | 332
Advanced Teaching Skills for the Fast-Paced OR: How to
Successfully Educate When Faced With High Clinical Workload,
Lack of Protected Time, and Limited Funding?
4:15-5:15 p.m. | Room E-2
Marek Brzezinski M.D., Ph.D.
This refresher course lecture will provide an overview of the
current and relevant teaching theories, review potential obstacles
and limitations to teaching in the perioperative period, and
provide simple approaches to optimize the rotation curriculum
as well as effective techniques to improve teaching, while not
compromising quality of care.Teaching in the fast-paced, high-
pressure environment of the OR and ICU can be very demanding.
High clinical workload, lack of protected time, and limited funding
represent 3 major and established obstacles to education. The
introduction of competencies and milestones has added yet
another challenging layer of increased pressure on and residency
program leadership to teach, evaluate, assess, and document
American College of Graduate Medical Education (ACGME)
competencies and milestones in the OR and ICU. All these factors
are unlikely to change in the near future; thus, the anesthesiologist
must learn teaching strategies that are time-efcient, simple, and
successful. Such advanced skills to teach and assess learners will
become increasingly important in the ICU as medical education
continues the transition from a time- and process-based system to
a competency-based framework.
Refresher Course Lecture | 335
The Art and Science of Disclosing Unanticipated Outcomes to
Patients: An Anesthesiologist’s Perspective
4:15-5:15 p.m. | La Nouvelle Ballroom AB
Allen Gustin M.D.
This refresher course will outline the denitions associated with
disclosure (medical error, adverse event, unanticipated outcome,
and medical error), will name several disclosure advocacy groups
(to provide resources to physicians), will list some of the leaders
in disclosure as examples of healthcare cultures where disclosure
is encouraged, will discuss the elements of an effective disclosure
conversation, will discuss the barrier/facilitators related to a
physicians willingness to disclose unanticipated outcomes,
discuss ways in which barriers can be overcomes, discuss the
apology and disclosure laws, and will discuss how disclosure/
apologies laws inuence the willingness of a physician to disclose
an unanticipated outcome.
Tuesday, October 14
Problem-Based Learning Discussions | L155
My Patient With a DNR Order Arrested in the OR! Now What?!
7:15-8:30 a.m. | Room 343-345
Juliann Hobbs M.D.,M.P.H.
Refresher Course Lecture | 401
Compensation for Service - When the Revenues Don’t Support the
Expectations
8-9 a.m. | RiverGate
Asa Lockhart M.D., M.B.A.
This lecture provides strategies when the practice revenues do
not support the expected level of services. The goal is to develop
a story that denes the underlying issues, develop a fair market
value budget, and identify quantiable performance metrics to
align incentives.
Point-Counterpoint | PC15
Anesthesia Information Management Systems Should Be the
Standard of Care for All Patients Receiving an Anesthetic
8-9:30 a.m. | Room 211-213
Joseph Szokol M.D., J.D, M.B.A.
The attendee will gain insight into how Anesthesia Information
Management Systems are vital to safe and effective patient care
while at the time being able to critically assess some of the pitfalls
associated with electronic medical records. Wilton Levine M.D.
PRO: Anesthesia Information Management Systems Should Be the
Standard of Care for Every Patient Presenting for Surgery Mark
Deshur M.D., MBA CON: Anesthesia Information Management
Systems Are Not yet Robust or Reliable Enough to Be Considered
Standard of Care
90 Minute Panel | PN85
What Is the Role of the Anesthesiologist Asked to Participate in a
Procedure He/She Believes Will Not Benet the Patient?
8-9:30 a.m. | Room 228-230
Nicholas Sadovnikoff M.D., F.C.C.M.
Ethical Obligations of the Anesthesiologist in High Risk/Low Benet
Procedures
A 97-year-old patient with multiple comorbidities presents with
bilateral femur fractures after a fall. You are asked to provide
anesthesia for bilateral femur repairs. You do not expect the
patient to benet from the surgery - what are your obligations?
Rebecca Aslakson M.D., Ph.D. Ethical Obligations of the
Anesthesiologist in High Risk/Low Benet Procedure Michael Nurok
M.B.,Ch.B., Ph.D. Ethical Obligations of the Anesthesiologist in High
Risk/Low Benet Procedure
90 Minute Panel | PN86
Professionalism - Who Needs It? Why Professionalism Matters No
Matter Where You Work
8-9:30 a.m. | Room 252-254
Saundra Curry M.D.
The Big Picture
The panelists will discuss professionalism and its effects
from three differing perspectives of typical anesthesiologists -
academic, private practitioner and researcher. James West M.D.,
M.A. Professionalism in Academics - The Standard? Richard
Wolman M.D., M.A. Professionalism in Research - Is It Necessary?
Richard Kelly M.D. Is Professionalism in Private Practice an
Oxymoron?
Poster Presentations | PO14-4
Patient Safety and Practice Management
8-10 a.m. | Hall B1-Area B
SCHEDULE BY LEARNING TRACK
104
Problem-Based Learning Discussions | L170
The Impaired Anesthesiologist: More Than Just Drugs and Alcohol
9-10:15 a.m. | Room 343-345
Gregory Rose M.D.
Refresher Course Lecture | 412
Safety and Human Factors in Anesthetic Practice
9:15-10:15 a.m. | La Nouvelle Ballroom AB
Keith Ruskin M.D.
The operating room is a complex and fast-paced environment in
which even seemingly insignicant events can be life-threatening.
This refresher course lecture will discuss the basics of patient
safety and how to reduce the risk of medical errors. Topics to be
discussed include human factors, the accident chain, hazardous
attitudes, situational awareness, and risk management. The
presentation will also include suggested changes to anesthetic
practice that may help to improve patient safety.
Clinical Forum | CF13
Controversial Cases in Organ Donation and End-of-Life Care:
Terminal Live Organ Donation and the Sale of Human Organs
10-11:30 a.m. | Room 206-207
Richard Wolman M.D., M.A.
The Altruistic System of Organ Donation Has Failed; Terminal
Live Organ Donation and the Sale of Human Organs Are Ethical If
Managed Correctly
Two complex cases involving end-of-life wishes and care and organ
donation are presented. The rst involves a request for terminal
live organ donation. The second involves the sale of human
organs. Ethical, legal, and practical issues to be discussed include
autonomy, benecence, nonmalecence, justice, DNR requests,
withdrawal of non-benecial life sustaining medical therapies,
organ donation after brain and cardiac death, and terminal live
organ donation. This session will further describe and debate the
ethical, legal, and practical issues associated with the current
altruistic system of organ donation, non-nancial alternatives, and
market (sale of human organs) alternatives to organ donation. The
ramications of the participation of anesthesiologists in cases
involving these two controversial issues will be discussed. Active
participation of the audience with the discussants is encouraged.
James West M.D., M.A. Patient and Physician Autonomy, DNR, and
Other End-of-Life Issues Michael Souter M.B., Ch.B., FRCA
Ethical Issues in Organ Procurement, the OPO’s Point of View,
Payment for Organs Gail Van Norman M.D. Euthanasia and Organ
Donation; Terminal Live Organ Donation and the Sale of Human
Organs Are Wrong
90 Minute Panel | PN89
Clean Versus Green: Are Optimized Patient Care and Community
Health/Safety Initiatives Mutually Exclusive?
10-11:30 a.m. | Room 225-227
Brian Rothman M.D.
Clean Environment - Green Materials Conservation and Disposal
This panel addresses current trends, techniques, and technologies
to deliver both clean care and operate green facilities. Addressed
are effective patient preparation and contamination minimization,
facility practices that benet both the patient and the environment,
and nally, the conservation of materials to minimize waste and
disposal practices that have the least environmental impact.
Harriet Hopf M.D. Clean Patients - Effective Preparation and
Contamination Minimization Charlotte Bell M.D. Clean Facilities -
Green HVAC and Other Facility Practices Brian Rothman M.D. Clean
Environment - Green Materials Conservation and Disposal
Refresher Course Lecture | 413
Mindfulness in Anesthesia: A Safety and Satisfaction Initiative
11:45 a.m.-12:45 p.m. | RiverGate
Neil Farber M.D., Ph.D.
The perioperative environment is mentally and physically
challenging. Anesthesiologists are continuously faced with
stressors, distractions, multi-tasking, and fatigue. This session
provides an overview of the concept of mindfulness and explores
evidence-based neurobiological and cognitive ndings regarding
its benets for stress reduction, safety, and satisfaction. This
professional competency will be approached from a broad
perspective while providing practical tools for integrating
mindfulness into both the perioperative arena and your personal
life. This session will also incorporate guided activities such that
participants will be able to actually experience various aspects of
mindfulness.
Problem-Based Learning Discussions | L178
How to Create and Moderate a Great Problem-Based Learning
Discussion (PBLD)
12:30-1:45 p.m. | Room 343-345
Kirk Lalwani M.D., F.R.C.A
Problem-Based Learning Discussions | L181
He’s 15, Needs This Operation and He’s DNR!
12:30-1:45 p.m. | Room 343-345
David Mann M.D.
Refresher Course Lecture | 419
Five Years of the AQI: What Do We Know About Ourselves Now?
1-2 p.m. | RiverGate
Richard Dutton M.D., M.B.A.
This refresher course lecture will briey summarize the history
and infrastructure of the AQI, an important ASA investment. A
top-level summary of data from NACOR, AIRS and the Closed
Claim Project will be provided, to illustrate the current state
of anesthesia in the United States; this summary will include
benchmarks for anesthesiologists (age, sex, time in practice)
business performance (practice size, case number, duration, etc.)
and quality outcomes (rates of major and minor complications)
and will include trends over the 5 years of the AQI’s existence.
The last part of the talk will be devoted to current and future
activities of the AQI, including enhanced collection and reporting
of outcome measures; development of standards for assessing
patient experience; linkage to other registries and data sources;
automated collection of clinical outcomes; and the role of the
AQI in meeting federal regulatory standards for performance
measurement in anesthesiology.
Refresher Course Lecture | 423
Do the Right Thing: Resolving Ethical Dilemmas in the OR
1-2 p.m. | Room 260-262
Sarah Smith M.D.
Two cases will be presented during this refresher course
lecture which highlight several topics in bioethics relevant to
the anesthesia practitioner, including medical decision making
capacity, patient autonomy, and the appropriate use of surrogate
decision makers. A practical approach to resolving ethical
dilemmas in the clinical arena based on accepted bioethical
principles will be presented. The history of bioethics within the
eld of anesthesiology will also be reviewed.
EDUCATION

105
Point-Counterpoint | PC19
Simulation in Medical Education: Boon or Boondoggle?
1-2:30 p.m. | Room 211-213
Amanda Burden M.D.
Simulation Is a Boon for Patient Safety and Medical Education
Simulation-based medical education emerged from
anesthesiologists’ efforts to improve patient safety. Interest in this
technology and method of education has expanded as evidenced
by its adoption into many medical disciplines and healthcare
professions and by the ACGME requirements to include more
simulation in residency curricula. It is a popular and interactive
teaching method that allows students to learn from errors without
harming patients. The question remains: What evidence justies
the dramatic increase in simulation in medical education?
Considering the cost of facilities, equipment and personnel
required to run a simulation program, there are those who believe
that simulation-based training should be mandated only when
there is denitive proof that its use leads to improved patient
outcomes or decreased costs for care. This session will be highly
interactive and will include discussion of specic scenarios and
strategies for the use and evidence for simulation. The session
will use an audience response system to stimulate participation.
Ample time for questions and discussion will be provided. Edwin
Bowe M.D. CON: Simulation Is Fun, but Where Is the Beef?
David Gaba M.D. PRO: Simulation Point Counterpoint Moderator
120 Minute Panel | PN26
The Economics of the Perioperative Surgical Home; We Know
Where We Are and Where We Want to Go, But How Do We Get
There?
1-3 p.m. | Room 208-210
Peter Dunbar M.B.,Ch.B., M.B.A
The speakers will present a detailed summary of the economic
drivers that have allowed the PSH to emerge as the ASA’s
preferred future model of anesthesia care. s will present the
views of governement and major employers regarding the current
economic situation and why the status quo is unsustainable.
Discussion will allow participants to ask questions of the panelists
that will be answered from a perspective of people who really
pay the bills. Stanley Stead M.D. MBA Economics of Surgical/
Interventional Care Today and Anesthesiology: Choices for the
Future Jeff Thompson M.D. What the Employers Expect to Buy
with Their Money for Their Employees’ Interventional Care Marc
Leib M.D. How State and Local Government Agencies Think about
Payment for Sugical/Interventional Care
120 Minute Panel | PN29
Everything You Need to Know About Lawsuits, But Didn’t Know
Whom to Ask
1-3 p.m. | Room 228-230
Aparna Ananth M.D.
Risk Management
Panel discussion with who are anesthesiologists with expertise
in Professional Liability and a defense attorney to provide multi-
dimensional viewpoints and information. Colleen O’Leary
Current Climate of Liabilty in Anesthesiology Amy Forbis J.D.
Lawsuits, Defensibility and Your Role as Defendant Amy Forbis
J.D. Conicts Between Your Malpractice Insurance Policy and Your
Personal Interest
Refresher Course Lecture | 425
Improving Patient Safety and Communication During Anesthesia
and Surgery
2:15-4:15 p.m. | RiverGate
Richard Cook M.D.
Why Is It so Hard to Make Progress on Patient Safety?
This two-hour Refresher Course will include 3 talks describing
methods to improve safety and communication in anesthesia and
surgery, as well as safety and communication lessons from the
Closed Claims Project. A question and answer session will follow
the formal presentations.This RC is a patient safety session and
we recommend it for MOCA. Cor Kalkman M.D., Ph.D. Improving
Perioperative Safety Timothy McDonald M.D. Communicate Openly -
Resolve Early
Problem-Based Learning Discussions | L190
Giving Feedback: How to Support the Defensive Learner
3:30-4:45 p.m. | Room 343-345
Yulia Ivashkov M.D.
Problem-Based Learning Discussions | L191
How Not to End Up on the Nightly News: Safe Injection Practices
3:30-4:45 p.m. | Room 343-345
Vilma Joseph M.D.
90 Minute Panel | PN95
Responding to Human Errors: The Good, the Bad, and the Ugly
3:30-5 p.m. | Room 225-227
Robert Lagasse M.D.
Peer Review: Protecting the Victims
This panel will compare and contrast the review processes for
accidents and near misses in the aviation industry with those
of the medical industry. A structured peer review process will be
demonstrated and the limitations of applying causal factor analysis
to performance improvement and competency assessments will
be discussed. The legal implications of human errors contributing
to adverse perioperative events will be presented along with
strategies for minimizing litigation risk. Keith Ruskin M.D.
Lessons Learned from the Federal Aviation Administration Judith
Semo J.D. The Medicolegal Response: Protecting Yourself
Wednesday, October 15
Oral Presentations | OR14-4
Patient Safety and Practice Management
8-9:30 a.m. | Room 244
120 Minute Panel | PN35
Grading the Graders - How Do We Get to Better Performance
Measures?
8-10 a.m. | Room 252-254
Laurent Glance M.D.
Do Quality Measures Really Measure Quality?
This panel will provide an overview of performance measurement,
and will describe the strengths and limitations of process and
outcomes measures. Topics will include the regulatory emphasis
on outcome measurement and value-based purchasing, the
ability of quality measures to truly capture quality, and the use
of physician-specic vs. team-based performance measurement.
Discussion will also include consideration of future directions in
performance measurement. Lee Fleisher M.D. Why Are Process
Measures Fading into the Night? Laurent Glance M.D. Do Quality
Measures Really Measure Quality? Peggy Duke M.D. Attribution of
Outcomes: Whose Outcomes Are They Anyway? It’s All about the
Team! Richard Dutton M.D., M.B.A. What the Future of Performance
Metrics Might Look Like
SCHEDULE BY LEARNING TRACK
106
Regional Anesthesia and Acute Pain
Saturday, October 11
Subspecialty Panel | 608
(ASRA) In-Hospital Falls: What Causes Them and How We Can
Prevent Them
7-8:15 a.m. | Room 243
Sandra Kopp, M.D., M.P.H., Linda Le-Wendling, M.D., F. Kayer
Enneking, M.D.
Problem-Based Learning Discussions | L006
Numb and Number: Should We Use Regional Anesthesia in
Orthopedic Trauma?
7:15-8:30 a.m. | Room 343-345
Nabil Elkassabany M.D.
Problem-Based Learning Discussions | L008
Nerve Injury/Dysfunction and Peripheral Nerve Blockade: Fact or
Fiction
7:15-8:30 a.m. | Room 343-345
Thomas Halaszynski M.D., MBA
120 Minute Panel | PN01
Integrating Regional Anesthesia Into the Perioperative Surgical
Home
8-10 a.m. | Room 217-219
James Hebl M.D.
The Value of Regional Anesthesia in Perioperative Care:
Orthopedics, Colorectal Surgery, Cancer Recurrence, Chronic Pain
and More!
This panel will explore how the practice of regional anesthesia
and actue pain medicine may be integrated into the Perioperative
Surgical Home concept. Specically, the value of regional
anesthesia on perioperative outcomes, the role of clinical
pathways in future models of healthcare, and the impact of the
Patient Protection and Affordable Care Act on the practice of
regional anesthesia and acute pain medicine will be discussed.
Arthur Boudreaux M.D. The Perioperative Surgical Home Concept:
An Overview F. Kayser Enneking M.D. The Role of Clinical Pathways
in Future Models of Healthcare Richard Rosenquist M.D.
Regional Anesthesia and Acute Pain Medicine in the Era of the
Patient Protection and Affordable Care Act
Hands-on Workshop | 807A
Ultrasound-Guided Regional Anesthesia and Clinical Skills
Workshop: Introduction to UGRA for Beginners
8-11 a.m. | Room 346-347
807B | 1-4 p.m. | Room 346-347
Adam Jacob M.D.
The workshop will be formatted to specically cater to
inexperienced ultrasound users. The experience will take place for
participants rotating through 5 interactive stations (approximately
30 minutes per station). Stations will include a combination of
ultrasound-guided upper and lower extremity and truncal blockade
techniques as well as a clinical skills station for needle practice
on simulated neural targets. Kyle Ahn M.D. Adam Amundson M.D.
Gregory Applegate D.O. Ryan Derby M.D., M.P.H. Clint Elliott M.D.
Ryan Endersby M.D. Natasha Funck M.D. Neil Hanson M.D. Rebecca
Johnson M.D. Tae-Wu Kim M.D. Kyle Kirkham M.D., FRCPC Jason
McVicar M.D. Jason Panchamia D.O. Christopher Robards M.D. Jose
Soberon M.D. Hans Sviggum M.D. Patrick Wong M.D.
Problem-Based Learning Discussions | L015
Nerve Injury After Peripheral Nerve Blockade: Best Practices and
Medical-Legal Protection Strategies
9-10:15 a.m. | Room 343-345
H. David Hardman M.D., MBA
Problem-Based Learning Discussions | L023
Analgesic Options for a 68-Year-Old Man With Multiple Rib
Fractures
9-10:15 a.m. | Room 343-345
Kristopher Schroeder M.D., Mark Leibel, M.D.
Refresher Course Lecture | 110
Upper Extremity Regional Anesthesia: Essentials for Your
Practice
9:15-10:15 a.m. | Room E-3
Joseph Neal M.D.
This lecture reviews the evidence base pertaining to upper
extremity regional anesthesia. Key topics include: outcomes,
techniques that optimize success, drug selection, and
complications.
Poster Presentations | PO16-1
Regional Anesthesia and Acute Pain
10 a.m.-12 p.m. | Hall B1-Area E
Poster Presentations | PO16-4
Regional Anesthesia and Acute Pain
1-3 p.m. | Hall B1-Area E
Refresher Course Lecture | 117
Making Regional Anesthesia Work in the Real World
2:45-3:45 p.m. | Room E-1
Francis Salinas M.D.
The lecture will review data that support increawed use of
regional techniques and developemnt of improved techniques
and team strategies to enhance application of regional, with
specic discussions of newer approaches to post-operative pain
management for major in- and outpatient orthopedic procedures.
Poster Discussions | PD16-1
Regional Anesthesia and Acute Pain
3-4:30 p.m. | Room 245
Problem-Based Learning Discussions | L037
Postoperative Ulnar Neuropathy - Could I Have Done Something to
Prevent It?
3:30-4:45 p.m. | Room 343-345
Sanjay Bhananker M.B., B.S.
EDUCATION

107
Point-Counterpoint | PC05
Ultrasound-Guided Regional Anesthesia--Pushing the Limits or Over
the Edge
3:30-5 p.m. | Room 211-213
Meg Rosenblatt M.D.
CON: Over the Edge
One will describe the cutting-edge uses for ultrasound in the
performance of regional anesthesia and advantages for patient
care. The other will challenge these newer options by evaluating
the evidence for their implementation. Anahi Perlas M.D. PRO:
Pushing the Boundaries
90 Minute Panel | PN48
Regional Anesthesia in Children: What Have We Learned From
Large Prospective Databases?
3:30-5 p.m. | Room 252-254
Santhanam Suresh M.D.
This panel will discuss the formation of large registries that help
navigate the world of regional anesthesia in children. Benjamin
Walker M.D. Pediatric Regional Anesthesia Network (PRAN), the
USA Based Network Giorgio Ivani M.D. European Consortium: Have
We Reached a Consensus? Manoj Karmakar M.B.,B.S. Asian
Databases: The Need for Accuracy
Refresher Course Lecture | 126
Regional Anesthesia to Improve Long Term Outcomes After
Surgery
4-5 p.m. | Room 260-262
Michael Andreae M.D., M.S.
To convince our surgical partners of the bents of regional
anesthesia we have to show improved outcomes beyond the
immediate perioperative period. Based on two systematic
reviews and meta-analyses, we will critically evaluate the
evidence suggesting meaningful long term benets of regional
anesthesia. We will discuss randomized controlled trials on
regional anesthesia for the prevention of chronic pain after
surgery and trials on regional anesthesia for improved long term
functional outcomes after major joint surgery. We will outline the
process and limitations of systematic reviews and pinpoint some
typical methodological shortcomings of RCTs such assisting the
participants to better appraise the pertient literature.
Sunday, October 12
Problem-Based Learning Discussions | L050
Perioperative Management of the Patient on Anticoagulant
Therapy: A Fresh Look at an Old Problem
7:15-8:30 a.m. | Room 343-345
Richard Beers M.D.
Problem-Based Learning Discussions | L053
Antibrinolytic Use in Major Orthopedic Procedures: What’s the
Bloody Controversy?
7:15-8:30 a.m. | Room 343-345
Yan Lai M.D., M.P.H.
Problem-Based Learning Discussions | L066
Nerve Injury/Dysfunction and Peripheral Nerve Blockade: Fact or
Fiction
9-10:15 a.m. | Room 343-345
Thomas Halaszynski M.D., MBA
90 Minute Panel | PN58
Nerve Injury Following Regional Anesthesia
10 a.m.-11:30 a.m. | Room 228-230
Vincent Chan M.D.
What Has Ultrasound Taught Us?
This panel will examine the major etiology of nerve injury related
to regional anesthesia (needle placement and local anesthetic
injection) and surgery, appropriate investigations to determine the
diagnosis and prognosis, discuss medico-legal implications and
develop techniques to reduce the frequency, severity, and impact
of these complications. Jeff Gadsden M.D., FANZCA Perineural,
Epineural or Intraneural Injections: Denition and Risk of Nerve
Injury Alain Borgeat M.D. Assessment of Post Block Neurologic
Injury Susan Penney J.D. Medico-Legal Implications of Nerve
Injury
Poster Presentations | PO16-2
Regional Anesthesia and Acute Pain: Ultrasound Guided RA
10 a.m.-12 p.m. | Hall B1-Area A
Refresher Course Lecture | 222
Hemorrhagic and Infectious Complications of Neuraxial Anesthesia
12:30-1:30 p.m. | La Nouvelle Ballroom AB
Terese Horlocker M.D.
This refresher course lecture will present the updated
recommendations of the ASRA practice advisories on Infectious
Complications of Neuraxial Block and Regional Anesthesia in the
Patient Receiving Antithrombotic or Thrombolytic Therapy.
Problem-Based Learning Discussions | L076
Nerve Injury After Peripheral Nerve Blockade: Best Practices and
Medical-Legal Protection Strategies
12:30-1:45 p.m. | Room 343-345
H. David Hardman M.D., MBA
Problem-Based Learning Discussions | L082
Analgesic Options for a 68-Year-Old Man with Multiple Rib
Fractures
12:30-1:45 p.m. | Room 343-345
Mark Leibel M.D. Kristopher Schroeder M.D.
120 Minute Panel | PN14
Controversies and Challenges in Perioperative Pain Management
1-3 p.m. | Room 252-254
Eugene Viscusi M.D.
Perioperative pain management is an arean of many challenges
and controversies. Emerging evidence suggests that the individual
differences of patients may affect their sensitivity to pain.
The future of acute pain may reside with genetic testing and
personalized medicine. Chronic opioid exposure dramatically
alters response to opioid analgesics making new acute pain
extremely difcult to manage. Respiratory events related to opioid
exposure are a critical current concern. Understanding these
challenges prepares the clinician to best target emerging analgesic
approaches. Anita Gupta D.O., Pharm.D. Personalize Medicine: Is
It the Answer to Improving Acute Pain Management? David Clark
M.D. Acute Pain Management in the Opioid Tolerant PatientChad
Brummett M.D. Abnormal Pain Sensitivity and Postoperative Pain
Thomas Witkowski M.D. Respiratory Depression and Acute Pain
Management: Risk Stratication and Reduction
SCHEDULE BY LEARNING TRACK
108
Refresher Course Lecture | 232
The Economics of Regional Anesthesia
3-4 p.m. | Room E-3
Brian Williams M.D., M.B.A.
Peripheral nerve blocks placed before surgery require more
upstream workload, with the aim of patient-centered symptom
reduction downstream. When preoperative nerve blocks are
coupled with intraoperative RA, multiple patient and hospital
benets are achievable. Meanwhile, general anesthesia (GA) use
intraoperatively (instead of RA when the latter may have been more
appropriate but less convenient) can undermine the full potential
for process efciency and patient symptom reduction intended with
preoperative peripheral nerve blocks. Patient symptom reductions
and process efciency improvements can lead to signicant cost
reductions. Codifying economic benets can help to justify building
and sustaining such services when discussing these services with
hospital administrators who may be unaware of these patient-
centered and hospital efciency nuances.
120 Minute Panel | PN16
Transversus Abdominis Plane Block, Paravertebral Block or Thoracic
Epidural: Is There an Ideal Truncal Block?
3-5 p.m. | Room 211-213
Steven Clendenen M.D.
This session will review the past and present use of TAP and
PVB blocks and the current resurgence of these blocks. Thoracic
epidurals are considered the Gold Standard for postoperative
pain management and using a panel format, s will discuss the
advantages, disadvantages, indications and complication of
the individual blocks (epidurals,PVB,TAP) and review the current
literature to support their viewpoint. Manoj Karmakar M.B.,B.S.
Paravertebral Block Michael Barrington M.B.,B.S., Ph.D. Transversus
Abdominis Plane Block Adam Niesen M.D. Thoracic Epidural
Problem-Based Learning Discussions | L088
This Epidural Catheter Is Not Working Well. What Should I Do?
3:30-4:45 p.m. | Room 343-345
Miguel Cruz M.D.
Problem-Based Learning Discussions | L092
Thoracic Epidural Analgesia in the Recently Anticoagulated Patient:
Is This a Good Idea?
3:30-4:45 p.m. | Room 343-345
Anuj Malhotra M.D.
Refresher Course Lecture | 236
Ultrasound Guided Regional Anesthesia in Infants, Children and
Adolescents: Guiding You to Success
4:15-5:15 p.m. | Room E-1
Santhanam Suresh M.D.
This refresher course lecture will deal with US guided regional
techniques for upper, lower extremity, neuraxial and truncal blocks
in infants and children along with dosing guidelines. All blocks
will be highlighted using video demonstration of actual block
performance.
Monday, October 13
Subspecialty Panel|608
(ASRA) In-Hospital Falls: What Causes Them and How We Can
Prevent Them
7-8:15 a.m.|Room 243
Sandra Kopp, M.D., M.P.H., Linda Le-Wendling, M.D., F. Kayser
Enneking, M.D.
Problem-Based Learning Discussions | L107
A 40-Year-Old Woman With Multiple Sclerosis Consulting for
Postoperative Epidural Following Laparoscopic Converted to Open
Colectomy
7:15-8:30 a.m. | Room 343-345
John Shepler M.D. Kristopher Schroeder M.D.
Refresher Course Lecture | 303
Current Concepts and Controversies in Acute Pain Management
8-9 a.m. | Room E-2
Eugene Viscusi M.D.
Recent developments in acute pain management suggest that
treatment strategies can have far reaching implications for both
short-term and long-term outcomes. Recent evidence raises
concerns that short term perioperative exposure may support
tumor growth and reduce survival. Brief opioid exposure may
lead to tolerance, hyperalgesia, abuse, sleep disturbances as
well as the more common opioid nuisance side effects. Chronic
pain following surgery is gaining attention. Causes are likely
multifactorial and a clear preventive strategy remains elusive.
Obstructive and central sleep apnea are a growing concern with
opioid analgesia in the postoperative period yet identication
and monitoring remains extremely challenging. reducing opioids
through a multimodal approach is a common emerging theme.
Clinical Forum | CF08
EXPAREL: A Novel Liposomal Extended-Release Bupivacaine
Formulation
8-9:30 a.m. | Room 203-205
John Rowlingson M.D.
EXPAREL is a novel extended-release formulation of bupivacaine
utilizing the DepoFoam drug delivery platform. This recently
approved drug received an FDA indication for surgical inltration
to provide up to 72 hours of analgesia. Current available data
from the pivitol studies for approval answer many questions about
the safety, efcacy and utility but leave many other questions
unanswered. Clinicians often will venture out and use drugs for
unapproved uses. This panel will summarize the current available
information to guide clinicians on safe use, provide insights to
future applications and present thought provoking applications
in Enhanced Rocovery after Surgery (ERAS) protocols. Admir
Hadzic M.D. Potential Future Uses for EXPAREL: Peripheral Nerve
Blocks and Epidurals Tong Gan M.D. EXPAREL for Inltration, TAP,
Periarticular Inltration: Application in Enhanced Recover After
Surgery (ERAS) Protocols
Problem-Based Learning Discussions | L113
This Epidural Catheter Is Not Working Well. What Should I Do?
9-10:15 a.m. | Room 343-345
Miguel Cruz M.D.
Problem-Based Learning Discussions | L114
Numb and Number: Should We Use Regional Anesthesia in
Orthopedic Trauma?
9-10:15 a.m. | Room 343-345
Nabil Elkassabany M.D.
EDUCATION

109
Refresher Course Lecture | 311
Clinical Pathways for Total Joint Arthroplasty: Essential Components
for Success
9:15-10:15 a.m. | Room 260-262
James Hebl M.D.
This refresher course lecture will provide an overview of the role of
clinical pathways to enhance the quality, improve the safety, and
reduce the cost associated with joint replacement surgery.
Refresher Course Lecture | 316
Lipid Resuscitation for Local Anesthetic and Other Toxic Overdoses
12:30-1:30 p.m. | Room 260-262
Guy Weinberg M.D.
This refresher course will review the development of lipid
resuscitation as an effective treatment for severe toxicity caused
by local anesthetics or other lipophilic drugs. This modality
reverses both CNS and cardiovascular toxicity in animal models
and clinical scenarios. It exemplies translational research and the
ongoing contribution of basic anesthesia scientic investigation
to other medical specialties and improving patient safety at large.
The course will stress both the practical, clinical application
and the underlying proposed mechanisms for the benet of lipid
resuscitation. Limitations of the method and future potential uses
including tissue protection from ischemia-reperfusion injury will
also be discussed.
Poster Presentations | PO16-3
Regional Anesthesia and Acute Pain: Basic sciences
1-3 p.m. | Hall B1-Area B
Hands-on Workshop | 828A
Peripheral Nerve Blocks: Ultrasound, Simulation and Stimulation
1-4 p.m. | Room 352
Hands-on Workshop | 828B
8-11 a.m. | Room 352
Hands-on Workshop | 828C
1-4 p.m. | Room 352
Andrew Rosenberg M.D.
This workshop will consist of a lecture followed by participants
moving through ve stations to gain knowledge of regional
anesthesia techniques including ultrasound guided regional
anesthesia and nerve stimulation technique. In addition there is
a simulation station that has simulators for ultrasound guidance
for the upper extremity, the lower extremity, and the femoral nerve.
There is a station for simulation of nerve stimulation of the upper
extremity. Arthur Atchabahian M.D. Patrick Birmingham M.D.
Patrick Boyle M.D. Levon Capan M.D. Vincent Chan M.D. Jacques
Chelly M.D., Ph.D., M.B.A. Nabil Elkassabany M.D. Richard Elliott
M.D. Jessica George M.D. Trusha Govindji M.D. Thomas Harrison
M.D. Barys Ihnatsenka M.D. Christina Jeng M.D. Jung Kim M.D.
Mitchell Lee M.D. Linda Le-Wendling M.D. Stephen Lucas M.D.
Mitchell Marshall M.D. Jovan Popovic M.D. Santhanam Suresh M.D.
Daniel Wambold M.D. Lisa Warren M.D. Sylvia Wilson M.D. Myron
Yaster M.D.
Cadaver Workshops | CA06
Comprehensive Anatomy-Live Model Ultrasound for Regional
Anesthesia
1-5 p.m. | Room 271-273
Carlo Franco M.D.
Cadaver Workshop and Live Model Ultrasound for Regional
Anesthesia
The workshop will start with a 40 minute lecture on gross anatomy
of nerve blocks and fundamentals of ultrasound imaging. Then the
participants will alternate between a cadaver dissection station
and a live model demonstration to correlate anatomy-ultrasound
at different locations. Xavier Sala-Blanch M.D. Ultrasound
Demonstration
Refresher Course Lecture | 322
Lower Extremity Nerve Blocks: Update
1:45-2:45 p.m. | Room 260-262
Admir Hadzic M.D., Ph.D.
Lower Extremity Nerve Blocks: Updatewill focus on ever changing
techniques, modes of application, pharmacology and perioperative
management of lower extremity nerve blocks.
Refresher Course Lecture | 326
Multimodal Analgesics for Perioperative Pain Control
3-4 p.m. | Room E-2
May Chin M.D.
This refresher course will provide an overview of the
pathophysiology of pain from surgery, review the current evidence
for perioperative use of adjuvant analgesics, and examine the
impact of multimodal analgesia on clinical outcomes.
Oral Presentations | OR16-1
Regional Anesthesia and Acute Pain
3-4:30 p.m. | Room 231-232
Problem-Based Learning Discussions | L143
Tough Choices: Regional or General Anesthesia in a Very Elderly
Patient
3:30-4:45 p.m. | Room 343-345
Jason Lane M.D., M.P.H.
90 Minute Panel | PN78
Regional Anesthesia for Total Shoulder Arthoplasty: Outcomes,
Complications, Techniques, and Use in Ambulatory Surgery
3:30-5 p.m. | Room 228-230
Maxim Eckmann M.D.
Analgesia and Anesthesia of the Shoulder Joint and Surrounding
Tissues, Peripheral Nerve and Brachial Plexus Techniques
This panel is intended to refresh the clinician on methods to
provide perioperative analgesia of the shoulder, review the effects
of regional anesthesia on functional outcomes following total
shoulder arthroplasty, and explore use of continuous perineural
blockade to facilitate outpatient total shoulder arthroplasty.
Hans Sviggum M.D. Benet of Regional Anesthesia in Functional
Outcomes and Patient Satisfaction Following Total Shoulder
Arthroplasty Brian Ilfeld M.D., M.S. Critical Role of Regional
Anesthesia in Ambulatory Total Shoulder Arthroplasty
SCHEDULE BY LEARNING TRACK
110
90 Minute Panel | PN80
Regional Anesthesia Dilemmas Due to Medical Disease
3:30-5 p.m. | Room 255-257
Steven Clendenen M.D.
Patients presenting for a surgical procedure, which could be
performed with a regional anesthetic/analgesic commonly, have
medical problems, which impact the choice or the conduct of that
anesthetic. Perioperative complications related to co-morbidities
may by positively or negatively affect by the choice of a regional
anesthetic/analgesic technique. This panel will include four
presentations on regional anesthesia/analgesia conundrums.
Chester Buckenmaier III, M.D. Acute Pain Management in Patients
with Multiple Trauma Admir Hadzic M.D. Regional Block in the
Patient with Pre-Existing Neuropathy David Auyong M.D.
Regional Anesthesia in the Morbidly Obese Patient Terese Horlocker
M.D. Regional Anesthesia in Patients With Spinal Canal Pathology
Tuesday, October 14
Problem-Based Learning Discussions | L151
Postoperative Ulnar Neuropathy - Could I Have Done Something to
Prevent It?
7:15-8:30 a.m. | Room 343-345
Sanjay Bhananker M.B., B.S.
Refresher Course Lecture | 404
The Age of HCAHPS: The Need for Acute Pain Services Revisited
8-9 a.m. | Room E-3
Michael Bottros M.D.
This refresher course lecture will provide an overview of the
Hospital Consumer Assessment of Healthcare Providers and
Systems (HCAHPS) and its current and future impact on hospital
economics and hospital administration. This information will
provide tools for anesthesiologists to improve their presence and
impact in perioperative medicine, especially in acute pain services,
and help shape hospital policies and protocols.
Poster Discussions | PD16-2
Regional Anesthesia and Acute Pain
8-9:30 a.m. | Room 243
Hands-on Workshop | 828B
Peripheral Nerve Blocks: Ultrasound, Simulation and Stimulation
8-11 a.m. | Room 352
Andrew Rosenberg M.D.
This workshop will consist of a lecture followed by participants
moving through ve stations to gain knowledge of regional
anesthesia techniques including ultrasound guided regional
anesthesia and nerve stimulation technique. In addition there is
a simulation station that has simulators for ultrasound guidance
for the upper extremity, the lower extremity, and the femoral nerve.
There is a station for simulation of nerve stimulation of the upper
extremity. Arthur Atchabahian M.D. Patrick Birmingham M.D.
Patrick Boyle M.D. Levon Capan M.D. Vincent Chan M.D. Jacques
Chelly M.D., Ph.D., M.B.A. Nabil Elkassabany M.D. Richard Elliott
M.D. Jessica George M.D. Trusha Govindji M.D. Thomas Harrison
M.D. Barys Ihnatsenka M.D. Christina Jeng M.D. Jung Kim M.D.
Mitchell Lee M.D. Linda Le-Wendling M.D. Stephen Lucas M.D.
Mitchell Marshall M.D. Jovan Popovic M.D. Santhanam Suresh M.D.
Daniel Wambold M.D. Lisa Warren M.D. Sylvia Wilson M.D.
Myron Yaster M.D.
Problem-Based Learning Discussions | L166
Antibrinolytic Use in Major Orthopedic Procedures: What’s the
Bloody Controversy?
9-10:15 a.m. | Room 343-345
Yan Lai M.D.,M.P.H.
Problem-Based Learning Discussions | L168
Thoracic Epidural Analgesia in the Recently Anticoagulated Patient:
Is This a Good Idea?
9-10:15 a.m. | Room 343-345
Anuj Malhotra M.D.
Refresher Course Lecture | 407
Virtual Cadaver Lab - Anatomy Pearls in Regional Anesthesia to
Improve Clinical Success
9:15-10:15 a.m. | RiverGate
David Auyong M.D.
This lecture covers the anatomical relationships of nerves, blood
vessels, muscle, bone, adipose, and skin that form the foundation
of regional anesthesia. Images will be presented from multiple
dissections in many different fresh tissue cadavers. Unique and
clinically relevant correlations will be made between classic
anatomical textbook images, the cadaver anatomy and ultrasound
images. Anatomical pearls will be reviewed and highlighted
for many nerve block approaches to the upper and lower
extremity including interscalene, supraclavicular, suprascapular,
infraclavicular, axillary, femoral, fascia iliaca, adductor canal, and
the sciatic nerve in the subgluteal and popliteal regions. The
interplay of gross anatomy and ultrasound images will cement
important anatomical relationships, improving clinical success
in regional anesthesia. Many oft repeated teachings in regional
anesthesia will be explored and then conrmed or refuted by
revisiting the gross anatomy of the human body.
Point-Counterpoint | PC17
Should I Be Using More Than One Local Anesthetic Additive During
Peripheral Nerve Blockade?
10-11:30 a.m. | Room 211-213
Anahi Perlas M.D.
This session will review the benets, safety, and clinical efcacy of
multimodal perineural analgesia during peripheral nerve blockade
vs. single-agent dexamethasone alone. Jacques Ya Deau M.D.,
Ph.D. CON: Single-Agent Dexamethasone Should Be Considered
Best Practice Brian Williams M.D., M.B.A. PRO: Multimodal
Perineural Analgesia Should Be Considered Best Practice
90 Minute Panel | PN83
Acute Pain Management in the Patient With Opioid Tolerance,
Dependence or Addiction
10-11:30 a.m. | Room 252-254
David Provenzano M.D.
Perioperative Evaluation and Discharge Planning for the Patient
with Opioid Tolerance
A history of chronic opioid exposure prior to surgery portends
a challenging postoperative pain period. Clinicians often fail
to quantify the degree of opioid use, abuse or addiction prior
to surgery and plan an appropriate anesthetic and analgesic
approach. A carefully planned multimodal approach with regional
anesthesia is likely the best strategy. As part of our role in
perioperative medicine, anesthesiologists can improve satisfaction
and outcome by a careful preoperative assessment of these
challenging patients with a tailored anesthetic and analgesia plan
followed by opioid management in the discharge plan. Asokumar
Buvanendran M.D. Best Perioperative Pain Management Strategies
in the Presence of Profound Opioid Tolerance Oscar De Leon-
Casasola M.D. Pain Management in the Patient with Known or
Suspected Addiction
EDUCATION

111
Poster Presentations|P016-5
Regional Anesthesia and Acute Pain
10 a.m.-12 p.m. | Hall B1 – Area B
120 Minute Panel | PN25
ASRA Practice Advisories: Review and Update
10 a.m.-12 p.m. | Room 217-219
Terese Horlocker M.D.
Regional Anesthesia and Anticoagulation
This panel will review the three most recent Practice Advisories
issued by ASRA: Anticoagulation and Regional Anesthesia,
Infectious Complications, Systemic Toxicity, and Neurological
Complications. Joseph Neal M.D. Approaches to Decrease the Risk
of Neurologic Complications Guy Weinberg M.D. Treatment of Local
Anesthetic Systemic Toxicity James Hebl M.D. Preventing Infectious
Complications through Optimal Asepsis
Poster Presentations | PO16-5
Regional Anesthesia and Acute Pain
10 a.m.-12 p.m. | Hall B1-Area B
Refresher Course Lecture | 415
Continuous Peripheral Nerve Blocks in 2014: Techniques,
Management, Benets, and Avoiding Complications
11:45-12:45 p.m. | Room E-2
Brian Ilfeld M.D., M.S.
This refresher course lecture will cover four main topics relating
to continuous peripheral nerve blocks: (1) techniques to optimize
perineural catheter placement and infusion management; (2)
perineural infusion benets; (3) possible perineural infusion
complications and ways to minimize their frequency; and (4)
ambulatory continuous peripheral nerve blocks. Topics are
included for those unfamiliar with continuous peripheral nerve
blocks as well as cutting-edge techniques and recently-published
data for experienced practitioners.
Problem-Based Learning Discussions | L174
Perioperative Management of the Patient on Anticoagulant
Therapy: A Fresh Look at an Old Problem
12:30-1:45 p.m. | Room 343-345
Richard Beers M.D.
Problem-Based Learning Discussions | L179
Tough Choices: Regional or General Anesthesia in a Very Elderly
Patient
12:30-1:45 p.m. | Room 343-345
Jason Lane M.D., M.P.H.
Refresher Course Lecture | 421
Local Anesthetics: Mechanisms, Toxicities and Controversies From a
Clinical Perspective
1-2 p.m. | Room E-2
John Butterworth M.D.
This refresher course lecture will review the local anesthetic
pharmacology and systemic toxicity, and will indicate those
instances where conventional wisdom is in conict with
contemporary data.
Problem-Based Learning Discussions | L192
A 40-Year -Old Woman With Multiple Sclerosis Consulting for
Postoperative Epidural Following Laparoscopic Converted to Open
Colectomy
3:30-4:45 p.m. | Room 343-345
John Shepler M.D. Kristopher Schroeder M.D.
Wednesday, October 15
120 Minute Panel | PN36
Regional Anesthesia Adjuncts: Helpful or Harmful?
8-10 a.m. | Room 255-257
Brian Williams M.D., M.B.A.
Perineural Dexamethasone and Buprenorphine: Animal Data and
Safety Concerns
This panel will evaluate the safety and efcacy of local anesthetic
additives for both neuraxial and peripheral nerve blockade.
s will present an evidence-based review of popular additives
dexamethasone, buprenorphine, clonidine, and dexmedetomidine.
There will also be a presentation evaluating preliminary clinical
and animal safety data of liposomal bupivacaine use during
regional anesthesia and periarticular administration. Jacques Ya
Deau M.D., Ph.D. Perineural Dexamethasone and Buprenorphine:
Clinical Applications and Efcacy Sandra Kopp M.D. Clonidine
and Dexmedetomidine: The Role of Alpha-2 Agonists in Regional
Anesthesia Brian Ilfeld M.D., M.S. Perineural and Periarticular
Liposomal Bupivacaine
Refresher Course Lecture | 505
Perioperative Analgesia and Effect on Patient Outcomes
9:15-10:15 a.m. | Room E-2
Spencer Liu M.D.
Review of pathophysiology and evidence for effects of regional
analgesia on perioperative outcomes.
Poster Discussions | PD16-3
Regional Anesthesia and Acute Pain
10-11:30 a.m. | Room 244
SCHEDULE BY LEARNING TRACK

112
SUBSPECIALTY PANELS
Date Time Track Fee Code Speaker Speaker Location
Saturday,
Oct. 11
7-8:15 a.m. OB 601 (SOAP) Caring for Our Own: Focusing on
the Care Provider to Optimize Safety for
Our Patients
Robert Gaiser,
M.D.
231-232
PN 602 (ASRA) Advancing Safety and Risk
Management Strategies in Pain Medicine
David Provenzano,
M.D.
238-239
Sunday,
Oct. 12
7-8:15 a.m. FA 603 (STA) How Can Mobile Technology Help Me
Help My Patients?
Maxime
Cannesson, M.D.,
Ph.D.
228-230
CC 604 (SOCCA) Trauma and Critical Care Pearls
for the Non-Intensivists
Daniel Brown
M.D., Ph.D.
231-232
AM 605 (SAMBA) TIVA in 2014 Steven Butz, M.D. 238-239
Monday,
Oct. 13
7-8:15 a.m. NA 606 (SNACC) Anesthesia for Acute Stroke
Management: Method, Timing and
Hemodynamics
Ra Avitsian, M.D. 231-232
PI 607 (SEA) Technology Today: Testing, Training
and Learning
Ira Todd Cohen,
M.D., M.Ed.
238-239
RA 608 (ASRA) In-Hospital Falls: What Causes
Them and How Can We Prevent Them?
Sandra Kopp,
M.D.
243
Tuesday,
Oct. 14
7-8:15 a.m. CA 609 (SCA) Cardiac Anesthesia Colleen Koch,
M.D., M.S.,
M.B.A.
231-232
PD 610 (SPA) The Child With Congenital Heart
Disease Presenting for Non-Cardiac
Surgery
Shobha Malviya,
M.D.
238-239
RCL - REFRESHER COURSE LECTURE
Date Time Track Fee Code Speaker Speaker Location
Saturday,
Oct. 11
8-9 a.m. CC 101 Sepsis Current Concepts, Guidelines and
Perioperative Management
Mark Nunnally
M.D. F.C.C.M.
RiverGate
AM 102 Current Controversies in Adult Outpatient
Anesthesia
Jeffrey Apfelbaum
M.D.
E-1
FA 103 Arterial Blood-Gas Analysis: Interpretation
and Application
Steven Barker
Ph.D. M.D.
E-2
OB 104 Anesthesia for the Morbidly Obese
Parturient
Brenda Bucklin
M.D.
E-3
PN 105 Clinical Evaluation and Treatment of
Neuropathic Pain
Timothy Lubenow
M.D.
260-262
CA 106 New Developments in Cardiopulmonary
Resuscitation
Matthias Riess
M.D. Ph.D.
La Nouvelle
Ballroom AB
9:15-10:15
a.m.
OB 107 Postpartum Hemorrhage Jill Mhyre M.D. RiverGate
CC 108 Pulmonary Hypertension and Right
Ventricular Failure
Eric Jacobsohn
M.B. Ch.B.
E-1
NA 109 Adult Head Injury: Management Update
and Controversies
Audree Bendo
M.D.
Martin Smith
M.B. B.S.
E-2
RA 110 Upper Extremity Regional Anesthesia:
Essentials for Your Practice
Joseph Neal M.D. E-3
CA 111 The Role of the Perioperative Physicians in
Prevention of Chronic Pain After Surgery
Asokumar
Buvanendran,
M.D.
260-262
CA 112 Perioperative Management of
Cardiovascular Implantable Electronic
Devices
Annemarie
Thompson M.D.
La Nouvelle
Ballroom AB
1:30-2:30
p.m.
PN 113 Complex Regional Pain Syndrome: What’s
New?
Richard Rauck
M.D.
E-3
NA 114 Blood Pressure and the Brain: How Low
Can You Go?
John Drummond
M.D.
260-262
CA 115 Perioperative Lung Protective Strategies in
One-Lung and Two-Lung Ventilation
Peter Slinger M.D. La Nouvelle
Ballroom AB
EDUCATION

113
FA 127 Hospital System Failures and Hazard
Management in the Operating
Allan Klock M.D. E-1
PI 128 Human Errors in Medicine: What They
Should Mean to Patients,Providers, and
the Public
Robert S.
Lagasse, M.D.
E-2
2:45-3:45
p.m.
OB 116 Anesthetic Management of the
Preeclamptic Patient
Joy Hawkins M.D. RiverGate
RA 117 Making Regional Anesthesia Work in the
Real World
Francis Salinas
M.D.
E-1
FA 118 Anesthesia for Major Orthopedic Surgery Andrew
Rosenberg M.D.
E-2
CC 119 Mechanical Ventilatory Support: What
Every Anesthesiologist Should Know
Michael Gropper
M.D. Ph.D.
E-3
FA 120 Operating Fire Safety William Culp M.D. 260-262
3-5 p.m. NA 121 Smart Seniors: Avoiding Perioperative
Brain Failure
Gregory Crosby
M.D.
La Nouvelle
Ballroom AB
4-5 p.m. FA 122 Mastering Anesthesia for the Elderly
Patient
Jeffrey Silverstein
M.D.
RiverGate
OB 123 Dural Puncture and Headache: Let’s Keep
It the Patient’s Headache
Robert Gaiser
M.D.
E-1
CC 124 Transfusion Therapy: Optimal Use of Blood
Products
Stephen Surgenor
M.B.A. M.D.
E-2
PD 125 Pediatric Ambulatory Anesthesia:
Challenges and Controversies
Linda Mason
M.D.
E-3
RA 126 Regional Anesthesia to Improve Long Term
Outcomes After Surgery
Michael Andreae
M.D. M.S.
260-262
Sunday, Oct.
12
8-9 a.m. CC 202 Respiratory Physiology and Perioperative
Gas Exchange
Luca Bigatello
M.D.
E-1
PD 203 Current Controversies in Pediatric
Anesthesia
Lena Sun M.D. E-2
CA 204 Rethinking Acute Blood Pressure
Management in the Perioperative Setting
Solomon Aronson
M.D. M.B.A.
F.A.C.C. F.C.C.P.
F.A.H.A. F.A.S.E.
E-3
AM 205 Anesthesia for Outpatient Diagnostic and
Therapeutic Radiology
Thomas Cutter
M.D.
260-262
CA 206 Preoperative Cardiac Evaluation for
Noncardiac Surgery
Lee Fleisher M.D. La Nouvelle
Ballroom AB
9:15-10:15
a.m.
OB
207 Neurologic Complications of Neuraxial
Anesthesia in Obstetrics
David Wlody M.D. RiverGate
PI 208 Decision Making Errors in Anesthesiology Marjorie Stiegler
M.D.
E-1
CA 209 Congenital Heart Disease in the Adult
Presenting for Non-Cardiac Surgery
Ilka Theruvath E-2
PN 210 Modern Concepts in Spinal Cord
Stimulation
Timothy Deer
M.D.
E-3
FA 211 Perioperative Management of Patients
With Left Ventricular Assist Devices
Undergoing Noncardiac Surgery
Michael O’Connor
M.D.
260-262
PD 212 New Guidelines: Pediatric Advanced Life
Support for the Anesthesiologist
Eugenie Heitmiller
M.D.
La Nouvelle
Ballroom AB
10:30-
11:30 a.m.
AM 213 Adult Patient With Morbid Obesity and
OSA for Ambulatory Surgery: An Update
Girish Joshi
M.B.B.S. M.D.
FFARCSI
RiverGate
OB 214 Hail Caesar: Anesthesia for Cesarean
Delivery
Lawrence Tsen
M.D.
E-1
CA 215 Catheter Based Cardiac Surgery:
Anesthesia in the Hybrid Suite and Cath
Lab
Nathaen Weitzel
M.D.
E-2
PN 216 Head and Neck Pain: A Clinical Approach Samer Narouze
M.D. Ph.D.
E-3
SCHEDULE BY SESSION TYPE

114
PD 217 Anesthesia for the Patient With Congenital
Heart Disease for Emergent Non-Cardiac
Surgery: Are You Well Equipped?
Dean
Andropoulos M.D.
260-262
CC 218 The Evidence Behind Evidence-Based
Medicine
Brian Kavanagh
M.B.
La Nouvelle
Ballroom AB
12:30-1:30
p.m.
PD 219 Anesthetic Induced Neurotoxicity in
Pediatric Patients: A Status Update
Randall Flick M.D.
M.P.H.
E-2
PN 220 Radiofrequency Ablation for the Treatment
of Spine Pain: Understanding the Basic
Principles and Clinical Applications
David Provenzano
M.D.
E-3
PD 221 Neonatal Emergencies: Simple Approach
to Success
Samuel Wald
M.D.
260-262
RA 222 Hemorrhagic and Infectious Complications
of Neuraxial Anesthesia
Terese Horlocker
M.D.
La Nouvelle
Ballroom AB
1:45-2:45
p.m.
FA 223 Perioperative Management of Pulmonary
Hypertension
Ronald Pearl M.D.
Ph.D.
RiverGate
FA 224 Obstructive Sleep Apnea - What an
Anesthesiologist Should Know
Frances Chung
M.B.B.S.
F.R.C.P.C.
E-1
OB 225 State of the Art Labor Analgesia Kenneth Nelson
M.D.
E-2
CC 226 Heart Failure and Perioperative Care Gareth Ackland
M.D.
E-3
AM 227 Effective Management of Pain, PONV and
Common Adverse Effects in Ambulatory
Surgical Patients
Tong Gan M.D. 260-262
PI 228 Building a Quality Management System for
Meaningful Use
John Allyn M.D. La Nouvelle
Ballroom AB
3-4 p.m. NA 229 The Impact of Anesthesia on the Young
and Old Brain
Audree A. Bendo
M.D.
RiverGate
CC 230 Perioperative Coagulation and
Coagulopathy
Linda Liu M.D. E-1
FA 231 Neuromuscular Management and Patient
Outcomes
Glenn Murphy
M.D.
E-2
RA 232 The Economics of Regional Anesthesia Brian Williams
M.D. M.B.A.
E-3
CA 233 New Developments in Thoracic Anesthesia Edmond Cohen
M.D.
260-262
OB 234 Anesthesia for Nonobstetric Surgery and
Procedures
Yaakov Beilin
M.D.
La Nouvelle
Ballroom AB
4:15-5:15
p.m.
PN 235 The Role of Perioperative Physicians in
Prevention of Chronic Pain After Surgery
Asokumar
Buvanendran
M.D.
RiverGate
RA 236 Ultrasound Guided Regional Anesthesia in
Infants Children and Adolescents: Guiding
You to Success
Santhanam
Suresh M.D.
E-1
PI 237 Mythbusters Episode: Economic Issues of
Anesthesia Care
Amr Abouleish
M.D. M.B.A.
E-2
FA 238 Weapons of Mass Destruction: Improvised
Explosive Devices
Michael Murray
M.D. Ph.D.
E-3
CC 239 Understanding Clinical Hemodynamics Jeffery Vender
M.D. F.C.C.M.
260-262
FA 240 What’s New in Airway Management Lauren Berkow
M.D.
La Nouvelle
Ballroom AB
Monday, Oct.
13
8-9 a.m. FA 301 Positioning Problems You Hope to Never
Encounter
Mark Warner M.D. RiverGate
PN 302 Therapeutic Epidural Injections: Safety
Considerations and Evidence Basis
Marc Huntoon
M.D.
E-1
RA 303 Current Concepts and Controversies in
Acute Pain Management
Eugene Viscusi
M.D.
E-2
PI 304 Tired of Not Being Taken Seriously? How
Professionalism Affects You
Saundra Curry
M.D.
E-3
EDUCATION

115
CA 305 Synthetic Colloids in Cardiac Surgery
What Are the Indications?
Roman Sniecinski
M.D.
260-262
8-10 a.m. NA 306 Perioperative Management of Patients
Undergoing Spine Surgery
Susan Black M.D. La Nouvelle
Ballroom AB
9:15-10:15
a.m.
PI 307 Ethics in the Real World Jeffrey Jacobs
M.D.
RiverGate
PN 308 The Strain in Pain Lies Mainly in the Brain:
Lessons Learned from the Neuroimaging
of Pain
Sean Mackey
M.D. Ph.D.
E-1
FA 309 A Few New Papers From Outside
Anesthesia Which Can Affect Your Pactice
James Eisenach
M.D.
E-2
CA 310 Cerebral Protection During Cardiac Surgery Charles Hogue
M.D.
E-3
RA 311 Clinical Pathways for Total Joint
Arthroplasty: Essential Components for
Success
James Hebl M.D. 260-262
12:30-1:30
p.m.
PI 312 Chemical Dependency and Anesthesiology John Tetzlaff M.D. RiverGate
CC 313 (A)ACLS in the Perioperative Period Gerald Maccioli
M.D.
E-1
FA 314 Perioperative Glycemic Management: A
Practical Guide
Basem
Abdelmalak M.D.
E-2
CA 315 Preconditioning the Heart: How It Works
and Does It Matter?
Judy Kersten M.D. E-3
RA 316 Lipid Resuscitation for Local Anesthetic
and Other Toxic Overdoses
Guy Weinberg
M.D.
260-262
PN 317 Improving Safety Through Use of
Diagnostic Imaging and Image Guidance in
Pain Medicine
James Rathmell
M.D.
La Nouvelle
Ballroom AB
1:45-2:45
p.m.
FA 318 How to Establish a Perioperative Surgical
Home in Your Institution
Zeev Kain M.D.
M.B.A.
RiverGate
PN 319 Interventional Pain Procedures in Patients
on Anticoagulants
Honorio Benzon
M. D.
E-1
AM 320 Malignant Hyperthermia in the Ambulatory
Setting
Ronald Litman
D.O.
E-2
FA 321 My Pharmacy Is Out of Fentanyl What Do
I Do Now? Rational Perioperative Opioid
Substitutions
Dhanesh Gupta
M.D.
E-3
RA 322 Lower Extremity Nerve Blocks: Update Admir Hadzic
M.D.Ph.D.
260-262
CC 323 Controversies and Best Practices in
Central Line Insertion
Avery Tung M.D.
F.C.C.M.
La Nouvelle
Ballroom AB
3-4 p.m. PN 324 Algorithmic Approach to Back Pain Nagy Mekhail
M.D. Ph.D.
RiverGate
AM 325 Ultrasound Guided Regional Anesthesia
for Ambulatory Surgery
Meg Rosenblatt
M.D.
E-1
RA 326 Multimodal Analgesics for Perioperative
Pain Control
May Chin M.D. E-2
FA 327 Top 10 Respiratory Anesthesia Practices
That Drive Me Crazy
David Warner
M.D.
E-3
PD 328 Airway Management in Pediatric
Emergencies: The Tricks of the Trade
Paul Reynolds
M.D.
260-262
FA 329 Hazards of the Anesthesia Workstation James Eisenkraft
M.D.
La Nouvelle
Ballroom AB
4:15-5:15
p.m.
CC 330 Perioperative Delirium Pratik
Pandharipande
M.D.
RiverGate
FA 331 Obesity and Anesthesia: Crossroads of a
Challenge
Ashish Sinha
M.D. Ph.D.
E-1
SCHEDULE BY SESSION TYPE

116
PI 332 Advanced Teaching Skills for the Fast-
Paced OR: How to Successfully Educate
When Faced With High Clinical Workload
Lack of Protected Time and Limited
Funding?
Marek Brzezinski
M.D. Ph.D.
E-2
CA 334 Heparin Sensitivity and Resistance:
Management During Cardiopulmonary
Bypass
Alan Finley M.D. 260-262
PI 335 The Art and Science of Disclosing
Unanticipated Outcomes to Patients: An
Anesthesiologist’s Perspective
Allen Gustin M.D. La Nouvelle
Ballroom AB
Tuesday, Oct.
14
8-9 a.m. PI 401 Compensation for Service - When the
Revenues Don’t Support the Expectations
Asa Lockhart
M.D. M.B.A.
RiverGate
AM 402 The Geriatric Outpatient: Postoperative
Cognitive Dysfunction and Other Concerns
Kathryn
McGoldrick M.D.
E-1
OB 403 Neuraxial Labor Analgesia and Pregnancy
Outcome: Fact and Fiction
Cynthia Wong
M.D.
E-2
RA 404 The Age of HCAHPS: The Need for Acute
Pain Services Revisited
Michael Bottros
M.D.
E-3
CA 405 The Pulmonary Artery Catheter in 2014:
Past Present and Is There a Future?
Jonathan Mark
M.D.
260-262
FA 406 ATLS Update: What Every Anesthesiologist
Needs to Know...BEFORE Going to the OR!
Maureen McCunn
M.D. M.I.P.P.
La Nouvelle
Ballroom AB
9:15-10:15
a.m.
RA 407 Virtual Cadaver Lab - Anatomy Pearls in
Regional Anesthesia to Improve Clinical
Success
David Auyong
M.D.
RiverGate
OB 408 Strategies to Optimize Cesarean Delivery
Analgesia
Brendan Carvalho
F.R.C.A.
E-1
PD 409 Acute Postoperative Pain Management in
Infants and Children: Size Does Matter!
Patrick
Birmingham M.D.
E-2
CA 410 Patient Safety in the Cardiac Operating :
What Can Will and Might Make Patients
Safer and You Happier
James Abernathy
M.D. M.P.H.
E-3
FA 411 Anesthetics and the Brain Less
Mysterious Than You May Think
Misha Perouansky
M.D.
260-262
PI 412 Safety and Human Factors in Anesthetic
Practice
Keith Ruskin M.D. La Nouvelle
Ballroom AB
11:45 a.m.-
12:45 p.m.
PI 413 Mindfulness in Anesthesia: A Safety and
Satisfaction Initiative
Neil Farber M.D.
Ph.D.
RiverGate
OB 414 Improving Patient Safety on the Labor and
Delivery Suite through Changes in Culture
Education and Communication
David Birnbach
M.D. M.P.H.
E-1
RA 415 Continuous Peripheral Nerve Blocks in
2014: Techniques Management Benets
and Avoiding Complications
Brian Ilfeld M.D.
M.S.
E-2
FA 416 Anesthesia for Head and Neck Surgery David Healy M.D.
M.R.C.P. F.R.C.A.
E-3
FA 417 Preoperative Identication Evaluation and
Optimization of the Highest Risk Patients
BobbieJean
Sweitzer M.D.
260-262
CA 418 TEE for the Occasional Cardiac
Anesthesiologist
Michael Cahalan
M.D.
La Nouvelle
Ballroom AB
1-2 p.m. PI 419 Five Years of the AQI: What Do We Know
About Ourselves Now?
Richard Dutton
M.D. M.B.A.
RiverGate
NA 420 Perioperative Management of
Cerebrovascular Diseases
Adrian Gelb M.B.
B.Ch. FRCPC
E-1
RA 421 Local Anesthetics: Mechanisms Toxicities
and Controversies From a Clinical
Perspective
John Butterworth
M.D.
E-2
CA 422 Massive Post-Cardiopulmonary
Hemorrhage: A Rational Approach to
Management
Edwin Avery IV
M.D.
E-3
PI 423 Do the Right Thing: Resolving Ethical
Dilemmas in the OR
Sarah Smith M.D. 260-262
EDUCATION

117
FA 424 Massive Transfusion Protocol in Trauma Charles Smith
M.D.
La Nouvelle
Ballroom AB
2:15-4:15
p.m.
PI 425 Improving Patient Safety and
Communication During Anesthesia and
Surgery
Richard Cook
M.D.
RiverGate
2:15-3:15
p.m.
PD 426 Anesthetic Management of Common
Pediatric Emergencies
Franklyn Cladis
M.D.
E-1
PN 427 Healthcare Reform and Pain Medicine
-Impact and Strategies for Future Success
Richard
Rosenquist M.D.
E-2
FA 428 Strategies for Success in Anesthesia
During One-Lung Ventilation
Gregory Fischer
M.D.
E-3
CA 429 Update on Strategies for Blood
Conservation and Hemostasis in Cardiac
Surgery
C. Mazer M.D. 260-262
FA 430 Electrical Safety in the Operating Jeffrey Gross
M.D.
La Nouvelle
Ballroom AB
3:30-4:30
p.m.
FA 431 Trauma Anesthesia and Operative
Resuscitation
Joshua Tobin
M.D.
E-1
FA 432 Different Strokes for Operative Folks:
Prevention of the Perioperative
Cerebrovascular Accident
George Williams
M.D.
E-2
FA 433 Current Controversies of Perioperative
Fluid Management
Roman Dudaryk
M.D.
E-3
Wednesday,
Oct. 15
8-9 a.m. CC 501 Emergent Airway Management: Tips Tricks
and Evidence
Aaron Joffe D.O. E-1
CA 502 Postoperative Acute Kidney Injury in
Cardiac Surgery
Madhav
Swaminathan
M.D.
E-2
FA 503 Recent Advances in Perioperative Fluid
Management and the Patients’ Outcomes
Ehab Farag M.D.
F.R.C.A.
E-3
9:15-10:15
a.m.
CC 504 Perioperative Renal Protection Michael Hutchens
M.D.
E-1
RA 505 Perioperative Analgesia and Effect on
Patient Outcomes
Spencer Liu M.D. E-2
90-MINUTE PANEL
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-9:30 a.m. CA PN37 Modern Day Concepts in Thoracic
Endovascular Repair (TEVAR) for Aortic
Aneurysms
David Broussard
M.D.
208-210
PI PN38 Change Management in Collaborative
Quality Improvement Projects (CQIP)
Mike Schweitzer
M.D. M.B.A.
220-222
PI PN39 Leaning In: Women in Leadership Roles Rekha
Chandrabose
M.D.
225-227
PN PN40 Back Pain and Health Care Redesign:
Preparing for Accountable Care
James Rathmell
M.D.
228-230
PD PN41 What Anesthesiologists Need to Know
About Resuscitating Kids in the OR
Jayant
Deshpande M.D.
M.P.H.
255-257
PI PN103 Quality and Safety Challenges: Raising the
Bar on Oversees Surgical Care
Richard
Gillerman, M.D.,
Ph.D.
206-207
1-2:30 p.m. CC PN42 Red Blood Cells: Good Bad and Ugly and
Some Solutions
Jonathan Jahr
M.D.
217-219
3:30-5 p.m. AM PN43 Advanced Diagnostic Bronchoscopy:
Coming Soon to an ASC near You
Basem
Abdelmalak M.D.
208-210
CA PN44 Thoracic Surgery 2014 Nathaen Weitzel
M.D.
217-219
CC PN45 Optimizing Perioperative Hepatic Function Randolph
Steadman M.D.
M.S.
220-222
PN PN46 Radiofrequency Ablation for Spinal Pain:
Techniques to Optimize Success
Kevin Vorenkamp
M.D.
225-227
SCHEDULE BY SESSION TYPE

118
NA PN47 Management of Neurological Events After
Anesthesia
Deborah Rusy
M.D.
228-230
RA PN48 Regional Anesthesia in Children: What
Have We Learned From Large Prospective
Databases?
Santhanam
Suresh M.D.
252-254
PI PN49 Governmental Inuences Over Health
Care: Lessons Learned From Working on
Capitol Hill
Andrew Gettinger
M.D.
255-257
Sunday,
Oct. 12
8-9:30 a.m. FA PN50 Airway Management Training: Are We
Keeping Up With Technology?
Nicholas Nedeff
M.D.
208-210
CA PN51 Heart Failure in Adults Undergoing Non-
Cardiac Surgery
Amanda Fox M.D.
M.P.H.
217-219
CC PN52 Simulation Education in Competency-
Based Training and Assessment: Present
and Future
Randall Schell
M.D. M.Ed.
220-222
NA PN53 The Yin and Yang of Anesthetic Drugs: Are
They Neuroprotective or Neurotoxic?
Piyush Patel M.D. 225-227
PN PN101 Neuropathic Pain: From Mechanisms to
Outcomes
Jianguo Cheng
M.D.
252-254
10-11:30
a.m.
OB PN54 Cutting-Edge Technologies and Point-
of-Care Devices to Improve Care of the
Obstetric Patient
Brendan Carvalho
F.R.C.A.
208-210
PD PN55 Pediatric Adenotonsillectomy: Enhancing
Quality and Efciency; Ensuring Safety
Lynne Maxwell
M.D.
217-219
PI PN56 Beating Back Burnout: Strategies for
Career Longevity and Improved Patient
Care
Mary Ann Vann
M.D.
220-222
PI PN57 Not All That Glitters is Gold- How Do I
Judge Quality from My Experience as a
Surgical Outpatient?
Armin Schubert
M.D.
225-227
RA PN58 Nerve Injury Following Regional
Anesthesia
Vincent Chan
M.D.
228-230
PI PN59 Professionalism - An International
Perspective
Saundra Curry
M.D.
255-257
1-2:30 p.m. FA PN102 Perioperative Management of Patients
With Endocrine Disease: A Global
Perspective
Karen Domino
M.D. M.P.H.
255-257
3:30-5 p.m. AM PN60 Crisis Management in Ofce-Based
Anesthesia
Michael Walsh
M.D.
208-210
CA PN61 Cerebral Oximetry Monitoring: Does It
Affect Neurologic Outcome?
John Murkin M.D. 217-219
CC PN62
ACLs for the Anesthesiologist: An Update Vivek Moitra M.D. 220-222
AM PN63 Ambulatory Surgery Airway Challenges Raafat Hannallah
M.D.
225-227
PI PN64 Limits of Care: Ethical Issues in the
Current Technological Environment
Paul Barash M.D. 228-230
FA PN65 Optimization of the High-Risk Surgery
Patient in the Era of Enhanced Recovery
After Surgery and Perioperative Surgical
Home
Maxime
Cannesson M.D.
Ph.D.
255-257
Monday, Oct.
13
8-9:30 a.m. OB PN66 Basic Considerations for the Occasional
Obstetric Anesthesiologist
Yaakov (Jake)
Beilin M.D.
208-210
1-2:30 p.m. CA PN67 Understanding the Role of Anemia
on Patient Outcomes: An Innocent
Bystander?
Colleen Koch
M.D. M.S.
M.B.A.
208-210
CC PN68 Quality Improvement in Critical Care Gregory Botz M.D. 217-219
PN PN69 Management of Chronic Pain: A Review of
Treatment Modalities
Magdalena
Anitescu M.D.
220-222
NA PN70 Life-Death Transition George Mashour
M.D. Ph.D.
225-227
PD PN71 TIVA for TOTS Zulqar Ahmed
M.D. F.A.A.P.
228-230
EDUCATION

119
FA PN72 Morbid and Ultra Obesity: Growing
Challenge in Anesthesiology
Ashish Sinha
M.D. Ph.D.
252-254
FA PN73 How Do We Decide When Not to Operate?
Facing Challenges in Surgical Decision-
Making for Older Adults
Mark Neuman
M.D. M.Sc.
255-257
3:30-5 p.m. AM PN74 Non-Operating Anesthesia: Techniques Basavana Goudra
M.D. F.R.C.A.
FCARCSI
208-210
CA PN75 Guidelines for Blood Management - What
Do They Tell Us?
C. Mazer M.D. 217-219
CC PN76 Optimizing Perioperative Pulmonary
Function
Steven Lisco M.D. 220-222
OB PN77 What Are They Doing and Why? Obstetrics
for the Anesthesiologist
Barbara Scavone
M.D.
225-227
RA PN78 Regional Anesthesia for Total Shoulder
Arthoplasty: Outcomes Complications
Techniques and Use in Ambulatory
Surgery
Maxim Eckmann
M.D.
228-230
PI PN79 Physician Impairment: Incidence
Identication and Intervention
Keith Berge M.D. 252-254
RA PN80 Regional Anesthesia Dilemmas Due to
Medical Disease
Steven Clendenen
M.D.
255-257
Tuesday, Oct.
14
8-9:30 a.m. AM PN81 Pediatric Ambulatory Challenges Raafat Hannallah
M.D.
208-210
AM PN82 Management of Patients at Risk of Sleep
Apnea in Ambulatory Anesthesia
Matthias
Eikermann M.D.
Ph.D.
217-219
FA PN84 Beyond Smoke and Mirrors: Panel on
Surgical Fire Prevention Including Laser
Safety
Charles Cowles
M.D. M.B.A.
225-227
PI PN85 What Is the Role of the Anesthesiologist
Asked to Participate in a Procedure He/
She Believes Will Not Benet the Patient?
Nicholas
Sadovnikoff M.D.
F.C.C.M.
228-230
PI PN86 Professionalism - Who Needs It? Why
Professionalism Matters No Matter Where
You Work
Saundra Curry
M.D.
252-254
10-11:30
a.m.
RA PN83 Acute Pain Management in the Patient
With Opioid Tolerance Dependence or
Addiction
David Provenzano
M.D.
252-254
CC PN87 Fluid Administration During the
Perioperative Period: Does It Make a
Difference What and How Much You
Give?
Matthias Jacob
M.D. Ph.D.
208-210
NA PN88 Sleeping and Waking Is Hard to Do:
Mechanisms of Induction and Emergence
From General Anesthesia
Peter Goldstein
M.D.
220-222
PI
PN89 Clean Versus Green: Are Optimized Patient
Care and Community Health/Safety
Initiatives Mutually Exclusive?
Brian Rothman
M.D.
225-227
FA PN90 Clinical Pearls: Anesthesia for Adult ENT
Surgery
Basem
Abdelmalak M.D.
228-230
1-2:30 p.m. CC PN91 The Evolving Goals of the ICU: Critical
Care Palliative Care or Patient-Centered
Care
Neal Cohen M.D.
M.P.H. M.S.
217-219
3:30-5 p.m. CA PN92 Perioperative 3D TEE: Innovative Imaging
or Just Pretty Pictures?
Stanton Shernan
M.D. F.A.H.A.
F.A.S.E.
208-210
FA PN93 Sugammadex: Are We Finally There?
Update on Unmet Medical Need Clinical
Use in Europe and Regulatory Progress
Jonathan Jahr
M.D.
217-219
CC PN94 Optimizing Perioperative Renal Function Robert Sladen
M.B. Ch.B.
F.C.C.M.
220-222
PI PN95 Responding to Human Errors: The Good
the Bad and the Ugly
Robert Lagasse
M.D.
225-227
SCHEDULE BY SESSION TYPE

120
AM PN96 Identifying Triage Decisions in Ambulatory
Anesthesia: Right Patient Place
Technique and Time
Mary Ann Vann
M.D.
228-230
Wednesday,
Oct. 15
8-9:30 a.m. AM PN97 Challenges in Ambulatory Out-of-OR
Anesthesia Practice
Radha Arunkumar
M.B. B.S. M.D.
208-210
CC PN98 FFP: A Critical Appraisal in 2014 Aryeh Shander
M.D.
217-219
FA PN99 Big Data, Big Opportunity: Anesthesiology
2.0
Mark A. Levin
M.D.
220-222
CA PN100 Protecting the Lung During Cardiac
Surgery: An Interdisciplinary Approach
Eric Nelson D.O. 208-210
120-MINUTE PANEL
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-10 a.m. RA PN01 Integrating Regional Anesthesia Into the
Perioperative Surgical Home
James Hebl M.D. 217-219
CA PN02 Practice Guidelines in CV Anesthesia: How
Are We Doing as a Specialty?
Martin London
M.D.
252-254
1-3 p.m. PI PN03 Setting Up a Perioperative Surgical Home Zeev Kain M.D.
M.B.A.
208-210
CA PN04 Perioperative Patient Safety in
Cardiovascular Surgery: From Data to
Implementation
Nancy Nussmeier
M.D.
220-222
PI PN05 Whose Guidelines and Practice
Parameters Apply to Anesthesiologists?
John Butterworth
IV M.D.
225-227
NA PN06 Babies Are Not Just Large Rat Pups:
Controveries on the Impact of Anesthetics
on the Developing Brain
Sulpicio Soriano
M.D.
228-230
PN PN07 Evidenced Based Chronic Pain
Management in Children and
Adolescents:Is There Evidence or Is It
Bias?
Santhanam
Suresh M.D.
252-254
AM PN08 Anesthesia and Sedation for MRI:
Adapting to Technological Advances and
Demands
Keira Mason M.D. 255-257
Sunday,
Oct. 12
12:30-2:30
p.m.
PI PN09 Patients Do the Darndest Things: Tales
From the Anesthesia Incident Reporting
System
Richard Dutton
M.D. M.B.A.
211-213
1-3 p.m. CC PN10 Minimizing Postoperative ICU
Complications in a Surgical Home
Trung Vu M.D. 217-219
FA PN11 Intravenous Anesthesia Beyond Propofol Keira Mason M.D. 220-222
OB PN12
Perioperative Considerations for Ex
Utero Intrapartum Treatment Procedures:
Principles Pitfalls and Progress
Mark Rollins M.D.
Ph.D.
225-227
PD PN13 They Walk Among Us: Anesthesia for
Adults With Pediatric Disease
Debra Morrison
M.D.
228-230
RA PN14 Controversies and Challenges in
Perioperative Pain Management
Eugene Viscusi
M.D.
252-254
3-5 p.m. FA PN15 Fluid Administration in the Operating : An
Update Focusing on Recent Literature
Andrew Leibowitz
M.D.
203-205
RA PN16 Transversus Abdominis Plane Block
Paravertebral Block or Thoracic Epidural:
Is There an Ideal Truncal Block?
Steven Clendenen
M.D.
211-213
3:30-5:30
p.m.
FA PN17 Preoperative Assessment and
Management
David Hepner
M.D.
252-254
Monday, Oct.
13
8-10 a.m. CC PN18 Perioperative Hemodynamic Optimization
and Goal Directed Therapy
Jeffery Vender
M.D. F.C.C.M.
217-219
FA PN19 ACUTE Care Anesthesiology: Strategies for
the Management of Trauma Emergencies
and Disasters
Maureen McCunn
M.D. M.I.P.P.
220-222
OB PN20 Maternal Mortality in the Developed
World: What Should the Anesthesiologist
Know?
Robert D’Angelo
M.D.
225-227
EDUCATION

121
FA PN21 Neuromuscular Blockade and Reversal Francois Donati
M.D. Ph.D.
228-230
PN PN22 Palliative Care and the Anesthesiologist Mihir Kamdar
M.D.
252-254
PI PN23 Embracing Quality Improvement: Key
Steps You Can Take Today to Improve
Yourself Your Department and Your
Hospital
David Zvara M.D. 255-257
12:30-2:30
p.m.
PI PN24 Milestones: Setting a High Bar or Barely
Clearing the Hurdle?
Randall Schell
M.D. M.Ed.
203-205
Tuesday, Oct.
14
10 a.m.-12
p.m.
RA PN25 ASRA Practice Advisories: Review and
Update
Terese Horlocker
M.D.
217-219
1-3 p.m. PI PN26 The Economics of the Perioperative
Surgical Home; We Know Where We Are
and Where We Want to Go But How Do
We Get There?
Peter Dunbar
M.B. Ch.B. M.B.A
208-210
AM PN27 Novel Drugs in Ambulatory Practice. How
Would They Change Your Practice?
Tong Gan M.D. 220-222
CA PN28 Percutaneous Approaches to Aortic and
Mitral Pathology
Michael
Fitzsimons M.D.
225-227
PI PN29 Everything You Need to Know About
Lawsuits But Didn’t Know Whom to Ask
Aparna Ananth
M.D.
228-230
FA PN30 Computer-Assisted Personalized Sedation
(CAPS) - the Future of Moderate Sedation
Walter Maurer
M.D.
252-254
PD PN31 Editor’s Picks in Pediatric Anesthesiology
2014
Constance Houck
M.D.
255-257
3-5 p.m. FA PN32 Creating the Safe Non-Operating
Anesthesia (NORA) Experience
Brenda Gentz
M.D.
211-213
3:30-5:30
p.m.
CC PN33 Anesthesia for the Patient Too Sick for
Anesthesia
Daniel Brown
M.D. Ph.D.
252-254
Wednesday,
Oct. 15
8-10 a.m. FA PN34 Aortic Surgery in the 21st Century Rae Allain M.D. 228-230
PI PN35 Grading the Graders - How Do We Get to
Better Performance Measures?
Laurent Glance
M.D.
252-254
RA PN36 Regional Anesthesia Adjuncts: Helpful or
Harmful?
Brian Williams
M.D. M.B.A.
255-257
CLINICAL FORUM
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
1-2:30 p.m.
AM CF01 Pediatric Ambulatory Anesthesia: Clinical
Forum
Lucinda Everett
M.D.
206-207
PN CF02 Complications in Pain Medicine and
Preventive Strategies
Hariharan
Shankar M.B.
B.S.
211-213
3:30-5 p.m. CA CF03 Circulatory Assist: The Coming Tidal Wave Roman Sniecinski
M.D.
206-207
Sunday, Oct.
12
8-9:30 a.m. FA CF04 Evidence-Informed Anesthesia for the
Severely Obese; Example Obstetrics and
Gynecology - Does It Exist ?
Roman
Schumann M.D.
206-207
10-11:30
a.m.
CA CF05 Adult Congenital Heart Disease
(ACHD):Special Considerations for
Patients With CHD Surviving Into
Adulthood
James DiNardo
M.D.
206-207
1-2:30 p.m. AM CF06 Ambulatory Non-Operating Anesthesia
(NORA): It Ain’t That Simple
Thomas Cutter
M.D.
206-207
3-4:30 p.m. FA CF07 A 65-Year-Old Male; Preoperative
Evaluation and Management of CAD for
Robotic Prostate Surgery
Paul Kempen
M.D. Ph.D.
206-207
Monday, Oct.
13
8-9:30 a.m. RA CF08 EXPAREL: A Novel Liposomal Extended-
Release Bupivacaine Formulation
John Rowlingson
M.D.
203-205
CC CF09 Critical Care Forum: Challenges
and Controversies in Critical Care
Anesthesiology
Avery Tung M.D.
F.C.C.M.
206-207
SCHEDULE BY SESSION TYPE

122
1-2:30 p.m. PD CF10 Anesthetic Safety in Newborns Can Be
Achieved by Sticking to Little Details
Susan Verghese
M.D
206-207
3-4:30 p.m. PI CF11 What Should You Do When You Don’t
Think the Patient Should Have Surgery at
All?
Nancy Glass M.D.
M.B.A.
206-207
Tuesday, Oct.
14
8-9:30 a.m. PD CF12 In a Land Far Away From Home ... Remote
Anesthetic Care for the Medically Complex
Pediatric Patient
Inger Aliason
M.D.
206-207
10-11:30
a.m.
PI CF13 Controversial Cases in Organ Donation
and End-of-Life Care: Terminal Live Organ
Donation and the Sale of Human Organs
Richard Wolman
M.D. M.A.
206-207
1-2:30 p.m. FA CF14 Dogma and Controversies in Acute and
Perioperative Burn Care
Sam Sharar M.D. 206-207
3-5 p.m. NA CF15 You Want to Test What?: Anesthetic
Challenges During Functional
Neurosurgery
Antoun Koht M.D. 206-207
POINT-COUNTERPOINT
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-9:30 a.m. PI PC01 Life in the Time of Consolidation: Is Bigger
the New Better?
James Grant M.D. 203-205
CC PC02 We Give Too Much Fluid in the OR Ozan Akca M.D.,
Brian Kavanegh,
M.B.
211-213
1-2:30 p.m. CC PC03 Tidal Volumes Don’t Really Matter to
the Anesthesiologist
James Blum M.D.
Daniel Talmor
M.D. Ph.D.
203-205
3:30-5 p.m. CC PC04 Do We Really Need Risk Adjustment to
Measure Outcomes?
Avery Tung M.D.
Laurent Glance
M.D.
203-205
RA PC05 Ultrasound-Guided Regional Anesthesia--
Pushing the Limits or Over the Edge
Meg Rosenblatt
M.D.
Anahi Perlas M.D.
211-213
Sunday, Oct.
12
8-9:30 a.m. PN PC06 Long-Term Opioid Treatment for Chronic
Non-Malignant Pain
Gary Brenner
M.D. Ph.D.
Rene Przkora
M.D. Ph.D.
203-205
OB PC07 Combined Spinal-Epidural Labor
Analgesia: Forevermore or Nevermore?
Cynthia Wong
M.D.
211-213
10-11:30
a.m.
FA PC08 Perioperative Colloid Administration -
Should it be Abandoned?
Marc Rozner
Ph.D. M.D.
John Drummond
M.D.
211-213
1-2:30 p.m. CC PC09 A Structured Handoff Protocol Improves
the Care of Patients Going to the ICU After
Surgery
Steven Greenberg
M.D. Michael
O’Connor, M.D.,
FCCM
203-205
Monday, Oct.
13
8-9:30 a.m. CC PC10 Should We Perform CPR When We Know
That It Is Futile?
Neal Cohen M.D.
M.P.H. M.S.
211-213
1-2:30 p.m. FA PC11 Computer-Assisted Personalized Sedation
(CAPS) - Is the Coming Technology of
CAPS a Friend or Foe?
Walter Maurer
M.D.
211-213
3-4:30 p.m. PN PC12 Should We Discontinue the Use of Opioids
for the Treatment of Chronic Pain?
Rafael Miguel
M.D.
Oscar DeLeon-
Casaola M.D.
203-205
CA PC13 Current Controversies in Cardiac
Anesthesia
Gregory Janelle
M.D. F.A.S.E.
211-213
Tuesday, Oct.
14
8-9:30 a.m. CA PC14 Volatile Anesthetics for Cardioprotection:
Is Preconditioning a Bust?
Stefan De Hert
M.D.
203-205
PI PC15 Anesthesia Information Management
Systems Should Be the Standard of Care
for All Patients Receiving an Anesthetic
Joseph Szokol
M.D. J.D M.B.A.
211-213
EDUCATION

123
10-11:30
a.m.
CC PC16 Can Post-Operative Delirium Really Be
Managed?
Pratik
Pandharipande
M.D., William
Hurford, M.D.
203-205
RA PC17 Should I Be Using More Than One Local
Anesthetic Additive During Peripheral
Nerve Blockade?
Anahi Perlas M.D. 211-213
1-2:30 p.m. FA PC18 Hypotensive Resuscitation Joshua Tobin
M.D.
203-205
PI PC19 Simulation in Medical Education: Boon or
Boondoggle?
Amanda Burden
M.D.
211-213
3-4:30 p.m. CC PC20 Electronic Health Records Improve Patient
Safety? or Do They?
David Feinstein
M.D.
203-205
PBLD
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
7:15-8:30
a.m.
PI L001 A High Risk Patient for Low Risk
Outpatient Surgery: Is There Value in a
Surgical Home for a Patient Going Home?
Jeanna Blitz M.D. 343-345
NA L002 Only a Little Sniff of Cocaine; Now an
Aneurysm Coiling Headache!
Jess Brallier M.D. 343-345
PI L003 Creating a Culture of Professionalism in
Your Department
Saundra Curry
M.D.
343-345
CC L005 Surviving Septic Shock in the Operating
and Beyond: What Do the Guidelines Say?
Roman Dudaryk
M.D.
343-345
RA L006 Numb and Number: Should We Use
Regional Anesthesia in Orthopedic
Trauma?
Nabil Elkassabany
M.D.
343-345
OB L007 Just Another Day on Labor and Delivery:
Morbid Obesity and Preeclampsia
Regina Fragneto
M.D.
343-345
RA L008 Nerve Injury/Dysfunction and Peripheral
Nerve Blockade: Fact or Fiction
Thomas
Halaszynski M.D.
M.B.A.
343-345
AM L009 Perioperative Anesthetic Issues for
Ambulatory Surgery
Dean Jones M.D.
FRCPC
343-345
PN L010 Worsening Back Pain: To Inject or Not to
Inject That Is the Question
Tariq Malik M.D. 343-345
FA L011 It’s Only a MAC Case and Now My Patient
is on FIRE!
Mark Phillips
M.D.
343-345
PD L012 Application of Pediatric Advanced
Life Support for Managing a Patient
With a Debrillator Who Develops an
Intraoperative Cardiac Arrest
David Young M.D.
M.B.A.
343-345
OB L116 Neurologic Complications Following
Epidural Placement - How to Differentiate
and Manage?
Kelly Elterman
M.D.
David Hepner
M.D.
343-345
FA L157 The Unanticipated Difcult Airway: A
Dynamic and Dangerous Scenario
Lavinia Kolarczyk
M.D.
343-345
9-10:15
a.m.
PI L013 Infection Prevention for the Anesthesia
Professional: What is the Least I Should
Know and How Do I Apply It to My
Practice?
Richard Beers
M.D.
343-345
FA L014 Management of Antiplatelet Therapy
in Patients With Coronary Stents for
Noncardiac Surgery
Davide Cattano
M.D. Ph.D.
343-345
RA L015 Nerve Injury After Peripheral Nerve
Blockade: Best Practices and Medical-
Legal Protection Strategies
H. David Hardman
M.D. M.B.A.
343-345
PD L016 Trials and Tribulations: Interventional
Management for Recurrent Complex
Regional Pain Syndrome in Children
Stephen Hays
M.D.
343-345
FA L017 Perioperative Laboratory and Cardiac
Testing: What Is Necessary?
David Hepner
M.D.
343-345
SCHEDULE BY SESSION TYPE

124
PI L018 To Coerce or Not to Coerce: What Are the
Questions?
Norma Klein M.D. 343-345
FA L019 I Swear It Will Only Take 15 Minutes:
Anesthesia/Sedation for TEE/
Cardioversion
Julia Metzner
M.D.
343-345
OB L020 Placenta Percreta: Preparation and
Management
Cathleen
Peterson-Layne
M.D. Ph.D.
343-345
AM L021 It’s Just a Cataract: How a Simple Thing
Can Go Bad
Michael Pilla M.D. 343-345
FA L022 Perioperative Management of the Anemic
Patient
Russell Roberson
M.D.
343-345
RA L023 Analgesic Options for a 68-Year-Old Man
With Multiple Rib Fractures
Mark Leibel
M.D. Kristopher
Schroeder M.D.
343-345
PD L024 Tonsillectomy and Adenoidectomy in a
Child With Down Syndrome More to It
Than You Think!
Catherine Seipel
M.D.
343-345
12:30-1:45
p.m.
PD L004 When It Rains It Pours; Large AVM Heart
Failure Pulmonary HTN and Now There
Is V-tach!
Christina Diaz
M.D.
343-345
NA L025 Delayed Emergence After Craniotomy- No
Delays Accepted
Ra Avitsian M.D. 343-345
CA L026 Carotid Endarterectomy: Asleep Versus
Awake
Jeffrey Dobyns
D.O.
343-345
CC L027 Elderly Man; Going into Shock; Needs
Fluids Now!
Elizabeth Frost
M.B. Ch.B.
343-345
FA L028 A Patient With a Temperature of 102.5 F
and Rigors 3 Hours After Surgery
Theresa Gelzinis
M.D.
343-345
OB L029 Labor Analgesia and Postpartum Tubal
Ligation in a Patient with a History of
Spinal Instrumentation
Michael Hofkamp
M.D.
343-345
NA L030 My Ulnar Neuropathy Has Resolved. Now I
Have to Go for Spine Surgery in the Prone
Surrender Position
Ihab Kamel M.D. 343-345
PD L031 Why Does My Patient Scheduled for
Endoscopic Sinus Surgery Have Severe
Groin Pain?
Kirk Lalwani M.D.
Christine Martin
M.D.
343-345
AM L032 PONV PDNV and Long QT Syndrome:
Balancing Risk and Benet
Anuj Malhotra
M.D.
343-345
PI L033 Burned Out Anesthesiologist: Practice
Competence and Colleagues
Sergey Pisklakov
M.D.
343-345
FA L034 My Patients Never Have Residual Paralysis
in the PACU, or Do They?
Stephan Thilen
M.D. M.S.
343-345
PI L035 Anesthetic Options for Patients
Undergoing Dialysis Access Procedures
Derek Woodrum
M.D.
343-345
3:30-4:45
p.m.
FA L036 Anesthetic Management of a Patient With
Penetrating Chest Trauma
Charles Smith
M.D.
343-345
RA L037 Postoperative Ulnar Neuropathy - Could I
Have Done Something to Prevent It?
Sanjay Bhananker
M.B. B.S.
343-345
AM L038 Is Ambulatory Shoulder Surgery Safe in a
Patient With Obstructive Sleep Apnea?
Christopher
Canlas M.D.
343-345
PD L039 Wake Up Your Surgery Is Not Over Prabhakar
Devavaram M.B.
B.S.
343-345
NA L040 Ah! I Can’t Bear It! This Is the Worst
Headache of My Life!
Stanlies D’Souza
M.D. F.R.C.A
343-345
PD L041 I Passed Gas in the Operating . Are
Volatile Agents Really Silent and Deadly to
Patients With Muscular Dystrophy?
Matthew Green
M.D.
343-345
CA L042 I Thought Three Pump Runs Were Bad but
This Pulmonary Edema is Even Worse!
What is Going On?
Marcellene
Franzen M.D.
Lindsey Loveland-
Baptist M.D.
343-345
EDUCATION

125
OB L043 Anesthesia for an Hypoplastic Left Heart
Syndrome Parturient
David Mann M.D. 343-345
OB L044 Anesthetic Management of Cesarean
Delivery for a Parturient With Previous
Myocardial Infarction and Coronary Artery
Stents
Daria Moaveni
M.D.
343-345
FA L045 Blood IS Thicker Than Water: Anesthetic
Concerns of Hypercoagulability
Gregory Rose
M.D.
343-345
FA L046 Prevention and Management of
Intraoperative Awareness in High Risk
Patients
Kathleen Smith
M.D.
343-345
PI L047 Hold My Compass: Tools and Tips So That
YOU Don’t Get Lost in the EP Lab
Mark Weiss M.D. 343-345
Sunday, Oct.
12
7:15-8:30
a.m.
OB L048 Cesarean Delivery in a Patient With
Hypertrophic Obstructive Cardiomyopathy
Jaime Aaronson
M.D.
Stephanie
Goodman M.D.
343-345
NA L049 Delayed Emergence After Craniotomy- No
Delays Accepted
Ra Avitsian M.D. 343-345
RA L050 Perioperative Management of the Patient
on Anticoagulant Therapy: A Fresh Look at
an Old Problem
Richard Beers
M.D.
343-345
FA L051 Beyond Swiss Cheese - Cases for the
Anesthesia Patient Safety Ofcer
Jonathan Cohen
M.D.
343-345
FA L052 A Patient With a Temperature of 102.5 F
and Rigors 3 hours after Surgery
Theresa Gelzinis
M.D.
343-345
RA L053 Antibrinolytic Use in Major Orthopedic
Procedures: What’s the Bloody
Controversy?
Yan Lai M.D.
M.P.H.
343-345
CA L054 I Thought Three Pump Runs Were Bad but
This Pulmonary Edema is Even Worse!
What is Going On?
Lindsey Loveland-
Baptist M.D.
Marcellene
Franzen M.D.
343-345
NA L055 Deep Brain Stimulation for Parkinson’s
Disease: What Is the Role of the
Anesthesiologist?
Julia Metzner
M.D.
343-345
AM L056 It’s Just a Cataract: How a Simple Thing
Can Go Bad
Michael Pilla M.D. 343-345
PI L057 Burned Out Anesthesiologist: Practice
Competence and Colleagues
Sergey Pisklakov
M.D.
343-345
PI L058 The Impaired Anesthesiologist: More Than
Just Drugs and Alcohol
Gregory Rose
M.D.
343-345
PI L060 Anesthetic Options for Patients
Undergoing Dialysis Access Procedures
Derek Woodrum
M.D.
343-345
9-10:15
a.m.
FA L061 Anesthetic Management of a Patient With
Penetrating Chest Trauma
Charles Smith
M.D.
343-345
CC L062 Surviving Septic Shock in the Operating
and Beyond: What Do the Guidelines Say?
Roman Dudaryk
M.D.
343-345
OB L063 Just Another Day on Labor and Delivery:
Morbid Obesity and Preeclampsia
Regina Fragneto
M.D.
343-345
NA L064 Just Another Subarachnoid Hemorrhage?
Or Am I Really Up-to-date on What to Do?
Eduardo Galeano
M.D.
343-345
PD L065 I Passed Gas in the Operating . Are
Volatile Agents Really Silent and Deadly to
Patients With Muscular Dystrophy?
Matthew Green
M.D.
343-345
RA L066 Nerve Injury/Dysfunction and Peripheral
Nerve Blockade: Fact or Fiction
Thomas
Halaszynski M.D.
M.B.A.
343-345
OB L067 Labor Analgesia and Postpartum Tubal
Ligation in a Patient With a History of
Spinal Instrumentation
Michael Hofkamp
M.D.
343-345
CA L068 Patient With a Failing Fontan for
Emergency Exploratory Laparotomy
Galina Leyvi M.D. 343-345
SCHEDULE BY SESSION TYPE

126
FA L069 Prevention and Management of
Intraoperative Awareness in High Risk
Patients
Kathleen Smith
M.D.
343-345
FA L070 Airway Management of a Patient With
Penetrating Neck Injury
Albert Varon M.D. 343-345
PI L071 Anesthesiologists and Terminal Live Organ
Donation: You Want Me to Do What?
Richard Wolman
M.D.
343-345
PD L072 Application of Pediatric Advanced
Life Support for Managing a Patient
With a Debrillator Who Develops an
Intraoperative Cardiac Arrest
David Young M.D.
M.B.A.
343-345
12:30-1:45
p.m.
PI L073 Do You Want to Present a PBLD at the
2015 ASA Meeting? This PBLD Session
Could Help You
Sanjay Bhananker
M.B.B.S.
343-345
NA L074 Ah! I Can’t Bear It! This Is the Worst
Headache of My Life!
Stanlies D’Souza
M.D. F.R.C.A
343-345
PN L075 Opioid-Induced Hyperalgesia Tolerance
and Chronic Postsurgical Pain: a
Dilemma Complicating Postoperative Pain
Management
Dalia Elmofty
M.D.
343-345
RA L076 Nerve Injury After Peripheral Nerve
Blockade: Best Practices and Medical-
Legal Protection Strategies
H. David Hardman
M.D. M.B.A.
343-345
PI L077 To Coerce or Not to Coerce: What Are the
Questions?
Norma Klein M.D. 343-345
OB L078 Anesthesia for an Hypoplastic Left Heart
Syndrome Parturient
David Mann M.D. 343-345
OB L079 Anesthetic Management of Cesarean
Delivery for a Parturient With Previous
Myocardial Infarction and Coronary Artery
Stents
Daria Moaveni
M.D.
343-345
FA L080 It’s Only a MAC Case and Now My Patient
is on FIRE!
Mark Phillips
M.D.
343-345
OB L081 Critical Management of a Parturient With
Inuenza Progressing to ARDS
Vernon Ross M.D. 343-345
RA L082 Analgesic Options for a 68-Year-Old Man
with Multiple Rib Fractures
Mark Leibel M.D.
Kristopher
Schroeder M.D.
343-345
PI L083 Hold My Compass: Tools and Tips So That
YOU Don’t Get Lost in the EP Lab
Mark Weiss M.D. 343-345
CC L084 Management of Acute Pulmonary
Embolism:Anticipating and Responding to
Complexity
Ahmed Zaky M.D. 343-345
3:30-4:45
p.m.
PI L059 When the Patient Just Says No Sarah Smith M.D. 343-345
PI L085 A High Risk Patient for Low Risk
Outpatient Surgery: Is There Value in a
Surgical Home for a Patient Going Home?
Jeanna Blitz M.D. 343-345
NA L086 Only a Little Sniff of Cocaine; Now an
Aneurysm Coiling Headache!
Jess Brallier M.D. 343-345
CC L087 Transfusion Goals and Hemostatic
Management of the Anticoagulated
Trauma Patient: Can You Plug a Hole in
the Dam?
Louanne Carabini
M.D.
343-345
RA L088 This Epidural Catheter Is Not Working
Well. What Should I Do?
Miguel Cruz M.D. 343-345
CC L089 Elderly Man; Going into Shock; Needs
Fluids Now!.
Elizabeth Frost
M.B. Ch.B.
343-345
AM L090 It’s Just a Quick EGD in the Ofce...but
Can I Safely Anesthetize My Patient Here?
Jeena Jacob M.D. 343-345
PD L091 Why Does My Patient Scheduled for
Endoscopic Sinus Surgery Have Severe
Groin Pain?
Kirk Lalwani M.D.
Christine Martin
M.D.
343-345
EDUCATION

127
RA L092 Thoracic Epidural Analgesia in the
Recently Anticoagulated Patient: Is This a
Good Idea?
Anuj Malhotra
M.D.
343-345
PN L093 Worsening Back Pain: To Inject or Not to
Inject That Is the Question
Tariq Malik M.D. 343-345
OB L094 Anesthetic Considerations for the
Jehovah’s Witness Patient Undergoing Trial
of Labor After Cesarean Delivery (TOLAC)
Chawla LaToya
Mason M.D.
343-345
OB L095 Placenta Percreta: Preparation and
Management
Cathleen
Peterson-Layne
M.D. Ph.D.
343-345
PD L096 Tonsillectomy and Adenoidectomy in a
Child With Down Syndrome More to It
Than You Think!
Catherine Seipel
M.D.
343-345
Monday, Oct.
13
7:15-8:30
a.m.
FA L097 Help - My Patient Is on a Multi-
Chemotherapeutic Regimen and Is
Coming for a Laparotomy! What Do I Need
to Know?
Anoushka Afonso
M.D.
343-345
CA L098 Carotid Endarterectomy: Asleep Versus
Awake
Jeffrey Dobyns
D.O.
343-345
PI L100 Giving Feedback: How to Support the
Defensive Learner
Yulia Ivashkov
M.D.
343-345
NA L101 My Ulnar Neuropathy Has Resolved. Now I
Have to Go for Spine Surgery in the Prone
Surrender Position
Ihab Kamel M.D. 343-345
FA L102 Malignant Hyperthermia in a Child Having
a Tethered Cord Release
Tae Kim M.D. 343-345
OB L104 She was Advised Not to Get Pregnant and
She Did: Pulmonary Hypertension and
Pregnancy
Tanya Lucas M.D. 343-345
AM L105 PONV PDNV and Long QT Syndrome:
Balancing Risk and Benet
Anuj Malhotra
M.D.
343-345
PD L106 A Child With Mitochondrial Disease and
Propofol Allergy Who May be Susceptible
to Malignant Hyperthermia
Jayant Pratap
M.B. B.Ch.
343-345
RA L107 A 40-Year-Old Woman With Multiple
Sclerosis Consulting for Postoperative
Epidural Following Laparoscopic Converted
to Open Colectomy
John Shepler
M.D.
Kristopher
Schroeder M.D.
343-345
FA L108 Airway Management of a Patient With
Penetrating Neck Injury
Albert Varon M.D. 343-345
CC L109 Management of Acute Pulmonary
Embolism:Anticipating and Responding to
Complexity
Ahmed Zaky M.D. 343-345
NA L133 Awake Craniotomy in a Patient With
Obstructive Sleep Apnea
Karl Willmann
M.D.
343-345
PD L140
When It Rains It Pours; Large AVM Heart
Failure Pulmonary HTN and Now There
Is V-tach!
Christina Diaz
M.D.
343-345
9-10:15
a.m.
FA L110 Trauma Induced Coagulopathy Maged Andrews
M.B. B.Ch.
343-345
NA L111 Crisis in the Neuro-Muscular Junction:
Anesthetic Implications
Cristina Barboi
M.D.
343-345
AM L112 Is Ambulatory Shoulder Surgery Safe in a
Patient With Obstructive Sleep Apnea?
Christopher
Canlas M.D.
343-345
RA L113 This Epidural Catheter Is Not Working
Well. What Should I Do?
Miguel Cruz M.D. 343-345
RA L114 Numb and Number: Should We Use
Regional Anesthesia in Orthopedic
Trauma?
Nabil Elkassabany
M.D.
343-345
PN L115 Opioid-Induced Hyperalgesia Tolerance
and Chronic Postsurgical Pain: A
Dilemma Complicating Postoperative Pain
Management
Dalia Elmofty
M.D.
343-345
SCHEDULE BY SESSION TYPE

128
CC L117 Management of Severe ARDS in the ICU
With ECMO
Jacob Gutsche
M.D.
343-345
FA L118 A Patient With End-Stage Liver Disease for
Elective Surgery
Christopher
Darling D.O.
Michael
Hannaman M.D.
343-345
PI L119 My Patient With a DNR Order Arrested in
the OR! Now What?!
Juliann Hobbs
M.D. M.P.H.
343-345
PI L120 When the Patient Just Says No Sarah Smith M.D. 343-345
PD L121 It Is Just a Nosebleed Isn’t It? Anesthetic
Considerations for Unsuspected
Pulmonary Hypertension
Shu Ming Wang
M.D.
343-345
FA L122 Oh No! Both Arteries in My Neck Are
Blocked! Now What?
Stanlies D’Souza
M.D. F.R.C.A
343-345
12:30-1:45
p.m.
PI L103 How to Create and Moderate a Great
Problem - Based Learning Discussion
(PBLD)
Kirk Lalwani M.D.
F.R.C.A
343-345
PD L123 Cardiovascular Collapse During
Thoracoscopic Tracheoesophageal Fistula
Repair
Kimberly Blasius
M.D.
343-345
PI L124 Do You Want to Present a PBLD at the
2015 ASA Meeting? This PBLD Session
Could Help You
Sanjay Bhananker
M.D. F.R.C.A
343-345
FA L125 Can the Adult Patient With Morbid Obesity
and Obstructive Sleep Apnea Safely
Undergo Outpatient Surgery?
Kenneth Hiller
M.D.
343-345
PI L126 How Not to End Up on the Nightly News:
Safe Injection Practices
Vilma Joseph
M.D.
343-345
FA L127 The Unanticipated Difcult Airway: A
Dynamic and Dangerous Scenario
Lavinia Kolarczyk
M.D.
343-345
OB L128 A Parturient With Scoliosis and Harrington
Rods
Allison Lee M.D. 343-345
OB L129 Anesthetic Considerations for the
Jehovah’s Witness Patient Undergoing Trial
of Labor After Cesarean Delivery (TOLAC)
Chawla LaToya
Mason M.D.
343-345
FA L130 I Swear It Will Only Take 15 Minutes:
Anesthesia/Sedation for TEE/
Cardioversion
Julia Metzner
M.D.
343-345
FA L131 Blood IS Thicker Than Water: Anesthetic
Concerns of Hypercoagulability
Gregory Rose
M.D.
343-345
AM L132 A Slip and Fall in the Post Warfarin Era Mercy Udoji M.D. 343-345
PI L134 Anesthesiologists and Terminal Live Organ
Donation: You Want Me to Do What?
Richard Wolman
M.D.
343-345
PD
L135 Using Advanced Trauma Life Support to
Manage a Pediatric Trauma Patient With
Traumatic Brain Injury and Disclosure of
Difcult News After a Poor Outcome
David Young M.D.
M.B.A.
343-345
3:30-4:45
p.m.
CA L136 Descending Thoracic Aortic Repair - Spinal
Cord Protection Strategies
Harendra Arora
M.D.
343-345
NA L137 An Acute Ischemic Stroke Coming to Your
Neuroangiography Suite
Ra Avitsian M.D. 343-345
PI L138 Infection Prevention for the Anesthesia
Professional: What is the Least I Should
Know and How Do I Apply It to My
Practice?
Richard Beers
M.D.
343-345
PI L139 Creating a Culture of Professionalism in
Your Department
Saundra Curry
M.D.
343-345
CC L141 Management of Co-Intoxications in the
ICU Patient
Robert Gould
M.D.
343-345
AM L142 Perioperative Anesthetic Issues for
Ambulatory Surgery
Dean Jones M.D.
FRCPC
343-345
RA L143 Tough Choices: Regional or General
Anesthesia in a Very Elderly Patient
Jason Lane M.D.
M.P.H.
343-345
EDUCATION

129
PI L144 He’s 15 Needs This Operation and He’s
DNR!
David Mann M.D. 343-345
NA L145 Deep Brain Stimulation for Parkinson’s
Disease: What Is the Role of the
Anesthesiologist?
Julia Metzner
M.D.
343-345
FA L146 Cardiopulmonary Collapse During
Laparoscopic Nissen Fundoplication
Govind Rajan
M.D.
343-345
OB L147 Critical Management of a Parturient With
Inuenza Progressing to ARDS
Vernon Ross M.D. 343-345
OB L148 A Parturient Presenting in Premature
Labor With Single-Ventricle Physiology
Complicated by Breech Presentation and
Paroxysmal Supraventricular Tachycardia:
What’s Your Labor Management Plan?
Manuel Vallejo
M.D.
343-345
OB L187 Neurologic Complications Following
Epidural Placement - How to Differentiate
and Manage?
Kelly Elterman
M.D.
David Hepner
M.D.
343-345
Tuesday, Oct.
14
7:15-8:30
a.m.
FA L149 Trauma Induced Coagulopathy Maged Andrews
M.B. B.Ch.
343-345
NA L150 An Acute Ischemic Stroke Coming to Your
Neuroangiography Suite
Ra Avitsian M.D. 343-345
RA L151 Postoperative Ulnar Neuropathy - Could I
Have Done Something to Prevent It?
Sanjay Bhananker
M.D. F.R.C.A
343-345
CC L152 Transfusion Goals and Hemostatic
Management of the Anticoagulated
Trauma Patient: Can You Plug a Hole in
the Dam?
Louanne Carabini
M.D.
343-345
FA L153 Oh No! Both Arteries in My Neck Are
Blocked! Now What?
Stanlies D’Souza
M.D. F.R.C.A
343-345
CC L154 Management of Co-Intoxications in the
ICU Patient
Robert Gould
M.D.
343-345
PI L155 My Patient With a DNR Order Arrested in
the OR! Now What?!
Juliann Hobbs
M.D. M.P.H.
343-345
AM L156 It’s Just a Quick EGD in the Ofce...but
Can I Safely Anesthetize My Patient Here?
Jeena Jacob M.D. 343-345
OB L158 A Parturient With Scoliosis and Harrington
Rods
Allison Lee M.D. 343-345
FA L159 My Patients Never Have Residual Paralysis
in the PACU, or Do They?
Stephan Thilen
M.D. M.S.
343-345
NA L160 Awake Craniotomy in a Patient With
Obstructive Sleep Apnea
Karl Willmann
M.D.
343-345
9-10:15
a.m.
CA L161 Descending Thoracic Aortic Repair - Spinal
Cord Protection Strategies
Harendra Arora
M.D.
343-345
FA L162 Beyond Swiss Cheese - Cases for the
Anesthesia Patient Safety Ofcer
Jonathan Cohen
M.D.
343-345
PD L163 Wake Up Your Surgery Is Not Over Prabhakar
Devavaram M.B.
B.S.
343-345
CC L164 Management of Severe ARDS in the ICU
With ECMO
Jacob Gutsche
M.D.
343-345
FA L165 Malignant Hyperthermia in a Child Having
a Tethered Cord Release
Tae Kim M.D. 343-345
RA L166 Antibrinolytic Use in Major Orthopedic
Procedures: What’s the Bloody
Controversy?
Yan Lai M.D.
M.P.H.
343-345
OB L167 She was Advised Not to Get Pregnant and
She Did: Pulmonary Hypertension and
Pregnancy
Tanya Lucas M.D. 343-345
RA L168 Thoracic Epidural Analgesia in the
Recently Anticoagulated Patient: Is This a
Good Idea?
Anuj Malhotra
M.D.
343-345
FA L169 Cardiopulmonary Collapse During
Laparoscopic Nissen Fundoplication
Govind Rajan
M.D.
343-345
SCHEDULE BY SESSION TYPE

130
PI L170 The Impaired Anesthesiologist: More Than
Just Drugs and Alcohol
Gregory Rose
M.D.
343-345
AM L171 A Slip and Fall in the Post Warfarin Era Mercy Udoji M.D. 343-345
OB L172 A Parturient Presenting in Premature
Labor With Single-Ventricle Physiology
Complicated by Breech Presentation and
Paroxysmal Supraventricular Tachycardia:
What’s Your Labor Management Plan?
Manuel Vallejo
M.D.
343-345
12:30-1:45
p.m.
OB L173 Cesarean Delivery in a Patient With
Hypertrophic Obstructive Cardiomyopathy
Jaime Aaronson
M.D.
Stephanie
Goodman M.D.
343-345
FA L099 Perioperative Laboratory and Cardiac
Testing: What is Necessary?
David Hepner
M.D.
343-345
RA L174 Perioperative Management of the Patient
on Anticoagulant Therapy: A Fresh Look at
an Old Problem
Richard Beers
M.D.
343-345
FA L175 Management of Antiplatelet Therapy
in Patients With Coronary Stents for
Noncardiac Surgery
Davide Cattano
M.D. Ph.D.
343-345
NA L176 Just Another Subarachnoid Hemorrhage?
Or Am I Really Up-to-date on What to Do?
Eduardo Galeano
M.D.
343-345
PD L177 Trials and Tribulations: Interventional
Management for Recurrent Complex
Regional Pain Syndrome in Children
Stephen Hays
M.D.
343-345
PI L178 How to Create and Moderate a Great
Problem - Based Learning Discussion
(PBLD)
Kirk Lalwani M.D.
F.R.C.A
343-345
RA L179 Tough Choices: Regional or General
Anesthesia in a Very Elderly Patient
Jason Lane M.D.
M.P.H.
343-345
CA L180 Patient With a Failing Fontan for
Emergency Exploratory Laparotomy
Galina Leyvi M.D. 343-345
PI L181 He’s 15 Needs This Operation and He’s
DNR!
David Mann M.D. 343-345
PD L182 A Child With Mitochondrial Disease and
Propofol Allergy Who May be Susceptible
to Malignant Hyperthermia
Jayant Pratap
M.B. B.Ch.
343-345
FA L183 Perioperative Management of the Anemic
Patient
Russell Roberson
M.D.
343-345
3:30-4:45
p.m.
FA L184 Help - My Patient Is on a Multi-
Chemotherapeutic Regimen and Is
Coming for a Laparotomy! What Do I Need
to Know?
Anoushka Afonso
M.D.
343-345
PD L185 Cardiovascular Collapse During
Thoracoscopic Tracheoesophageal Fistula
Repair
Kimberly Blasius
M.D.
343-345
NA
L186 Crisis in the Neuro-Muscular Junction:
Anesthetic Implications
Cristina Barboi
M.D.
343-345
FA L188 A Patient With End-Stage Liver Disease for
Elective Surgery
Christopher
Darling D.O.
Michael
Hannaman M.D.
343-345
FA L189 Can the Adult Patient With Morbid Obesity
and Obstructive Sleep Apnea Safely
Undergo Outpatient Surgery?
Kenneth Hiller
M.D.
343-345
PI L190 Giving Feedback: How to Support the
Defensive Learner
Yulia Ivashkov
M.D.
343-345
PI L191 How Not to End Up on the Nightly News:
Safe Injection Practices
Vilma Joseph
M.D.
343-345
RA L192 A 40-Year -Old Woman With Multiple
Sclerosis Consulting for Postoperative
Epidural Following Laparoscopic Converted
to Open Colectomy
John Shepler
M.D.
Kristopher
Schroeder M.D.
343-345
EDUCATION

131
PD L193 It Is Just a Nosebleed Isn’t It? Anesthetic
Considerations for Unsuspected
Pulmonary Hypertension
Shu Ming Wang
M.D.
343-345
PD L194 Using Advanced Trauma Life Support to
Manage a Pediatric Trauma Patient With
Traumatic Brain Injury and Disclosure of
Difcult News After a Poor Outcome
David Young M.D.
M.B.A.
343-345
CADAVER WORKSHOPS
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8 a.m.-12
p.m.
PN CA01 Spinal Injections With Fluoroscopy-
Cadaver: Basic Techniques
Maunak Rana
M.D.
271-273
1-5 p.m. PN CA02 Spinal Injections With Fluoroscopy-
Cadaver: Advanced Techniques(Cervical/
Thoracic)
Timothy Lubenow
M.D.
271-273
Sunday, Oct.
12
8 a.m.-12
p.m.
PN CA03 Introduction to Ultrasound and
Fluoroscopic-Guided Techniques for
Chronic Pain Management: Live Models
and Cadavers
David Provenzano
M.D.
271-273
PN CA04 Head and Neck Blocks (Ultrasound and
Fluoroscopy)-Cadaver and Live Models
Miles Day M.D. 275-277
1-5 p.m. PN CA05 Radiofrequency Ablation of the Spine,
Sacrum, and LuM.B.A.r Disc
Maxim Eckmann
M.D.
275-277
Monday, Oct.
13
1-5 p.m. RA CA06 Comprehensive Anatomy-Live Model
Ultrasound for Regional Anesthesia
Carlo Franco
M.D. Xavier Sala-
Blanch M.D.
271-273
HANDS-ON WORKSHOP
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-10:30
a.m.
FA DW01 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil
M.D.
353-355
8-11 a.m. FA 802 Workshop on Emergency Surgical Airway
Management Using a Pig Trachea Model
William
Rosenblatt M.D.
278-279
PN 804 Acupuncture Workshop Yuan-Chi Lin M.D. 333-334
PD 806 Advanced Ultrasound Guided Pediatric
Regional Anesthesia Workshop
Amod Sawardekar
M.D.
338-339
RA 807A Ultrasound-Guided Regional Anesthesia
and Clinical Skills Workshop: Introduction
to UGRA for Beginners
Adam Jacob M.D. 346-347
8:00 a.m.-
12 p.m.
PN 801 Ultrasound Guided Injections-Live Models:
BasicTechniques
Hariharan
Shankar M.B.
275-277
9-10:15
a.m.
FA AW01 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
10:30 a.m.-
1 p.m.
FA DW02 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil M.D 353-355
10:30-
11:45 a.m.
FA AW02 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
12-1:15
p.m.
FA AW03 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
1-4 p.m. CA 809 Pacemakers and ICDs Aman Mahajan
M.D. Ph.D.
278-279
AM 810 Must Know Blocks for Ambulatory
Anesthesia
David Auyong
M.D.
265-268
RA 807B Ultrasound-Guided Regional Anesthesia
and Clinical Skills Workshop: Introduction
to UGRA for Beginners
Adam Jacob M.D. 346-347
1-5 p.m. PN 808 Ultrasound Guided Injections- Live Models:
Advanced Techniques
Philip Peng
M.B.B.S.
275-277
SCHEDULE BY SESSION TYPE
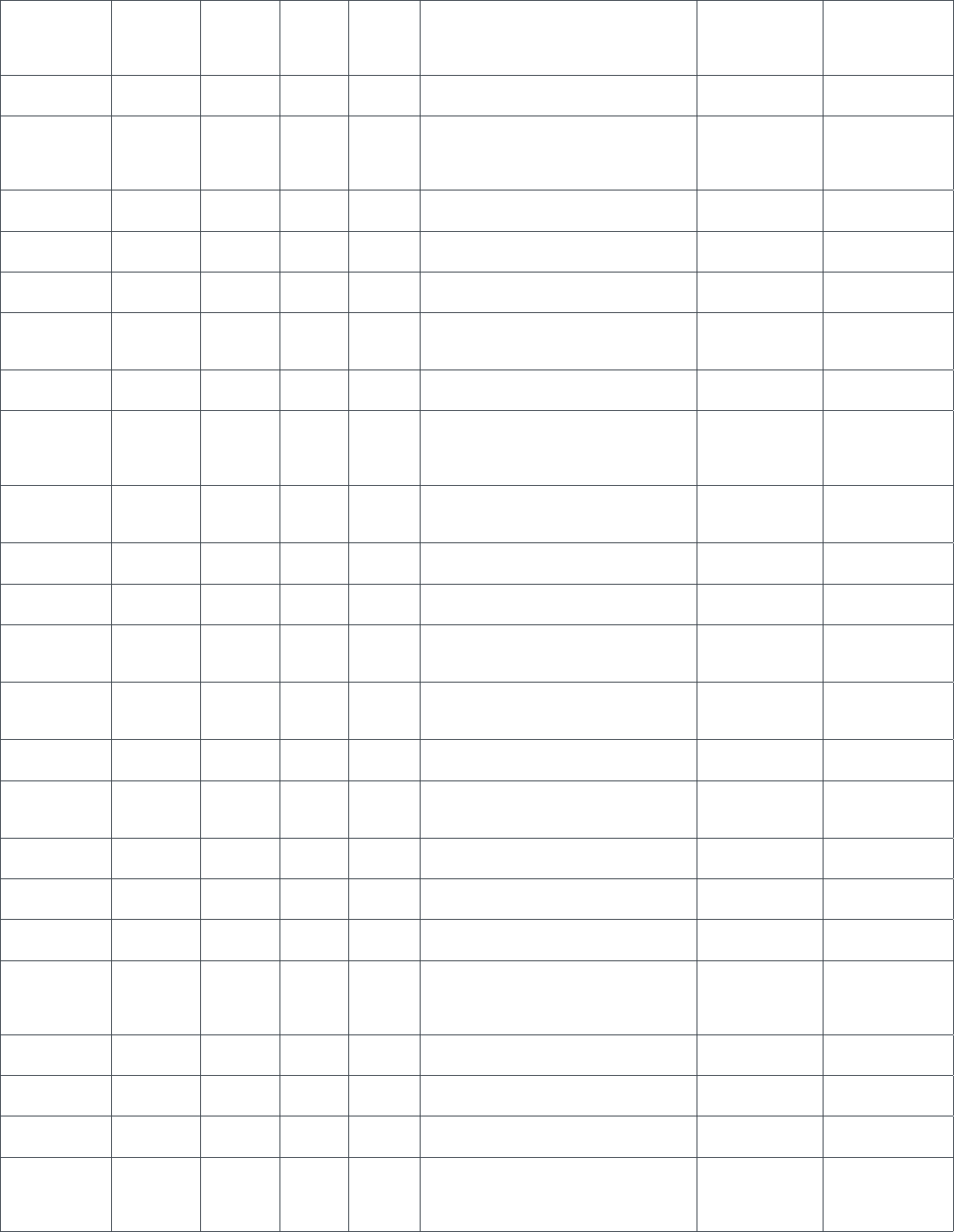
132
1:30-2:45
p.m.
FA AW04 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
2:30-5 p.m. FA DW03 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil M.D 353-355
3-4:15 p.m. FA AW05 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
Sunday,
Oct. 12
8-10:30
a.m.
FA DW04 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil M.D 353-355
8-11 a.m. PD 812 Pediatric Airway Workshop Narasimhan
Jagannathan M.D.
346-347
8 a.m.-4
p.m.
CA 815 Basic TEE Workshop Sasha Shillcutt
M.D.
338-339
9-10:15
a.m.
FA AW06 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O., William
Simmons, M.D.
356-357
10:30 a.m.-
1 p.m.
FA DW05 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil M.D 353-355
10:30-
11:45 a.m.
FA AW07 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O.
William Simmons
M.D.
356-357
12-1:15
p.m.
FA AW08 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O., William
Simmons, M.D.
356-357
1-4 p.m. FA 817 Awake Fiberoptic Intubation: A
Streamlined Approach With Nerve Blocks
Scott Miller M.D. 348-349
PD 823 Perioperative Pediatric Advanced Life
Support Simulation
Scott Watkins
M.D.
281
1-5 p.m. PN 814 Ultrasound Guided Musculoskeletal
Injections- Live Models: Beyond
Corticosteroids
James Modir M.D. 271-273
1:30-2:45
p.m.
FA AW09 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O., William
Simmons, M.D.
356-357
2:30-5 p.m. FA DW06 Basic/Advanced Flexible Fiberoptic
Intubation Workshop
Katherine Gil M.D
353-355
3-4:15 p.m. FA AW10 Workshop on Flexible Endoscopy for Lung
Isolation
Scott Schartel
D.O., William
Simmons, M.D.
356-357
Monday, Oct.
13
8-11 a.m. AM 820 Ophthalmic Regional Anesthesia Marc Feldman
M.D. MHS
333-334
CA 822 Intermediate Transesophageal
Echocardiography (TEE)
James Abernathy
M.D. M.P.H.
338-339
CC 825 Critical Care Ultrasonography for the
Perioperative Physician
Steven
Venticinque M.D.
356-357
FA 824A Difcult Airway Workshop With Simulation Elizabeth
Behringer M.D.
Joseph Quinlan
M.D.
353-355
8-11:30
a.m.
CC 819A Perioperative ACLS Simulation Workshop Matthew McEvoy
M.D.
281
1-4 p.m. FA 826 Wire-Guided Airway Management Richard Galgon
M.D. M.S.
333-334
CA 827 Advanced TEE Workshop Sajid Shahul M.D.
MPH
338-339
FA 824B Difcult Airway Workshop With Simulation Elizabeth
Behringer M.D.
Joseph Quinlan
M.D.
353-355
EDUCATION

133
RA 828A Peripheral Nerve Blocks: Ultrasound
Simulation and Stimulation
Andrew
Rosenberg M.D.
352
1-4:30 p.m. CC 819B Perioperative ACLS Simulation Workshop Matthew McEvoy
M.D.
278
Tuesday, Oct.
14
8-11 a.m. PD 832 Point of Care: Novel Use of
Ultrasonography in Everyday Pediatric
Anesthesia Practice
Santhanam
Suresh M.D.
353-354
RA 828B Peripheral Nerve Blocks: Ultrasound
Simulation and Stimulation
Andrew
Rosenberg M.D.
352
FA 831A The Use of Ultrasound for Vascular Access
in Adults and Pediatrics
Ehab Farag M.D.
F.R.C.A.
338-339
CA 833A Thoracic Anesthesia Workshop Edmond Cohen
M.D.
356-357
CC 830A Perioperative ACLS Simulation Workshop Matthew McEvoy
M.D.
281
1-4 p.m. RA 828C Peripheral Nerve Blocks: Ultrasound
Simulation and Stimulation
Andrew
Rosenberg M.D.
352
FA 831B The Use of Ultrasound for Vascular Access
in Adults and Pediatrics
Ehab Farag M.D.
F.R.C.A.
338-339
CA 833B Thoracic Anesthesia Workshop Edmond Cohen
M.D.
356-357
1-4:30 p.m. CC 830B Perioperative ACLS Simulation Workshop Matthew McEvoy
M.D.
281
SEMINAR
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-11 a.m. PI 803 Mastering Perioperative Stress and
Burnout: Exploring Methods of Essential
Mind-Fitness Developing Resilience at
Work
Kenneth Sapire
M.D.
281-282
FA 805 Statistics for Anesthesiologists Jeffrey Gross
M.D. Keith Gibson
M.D. Ph.D.
335-336
2-4 p.m. PN 811 Spinal Imaging for the Pain Medicine
Physician
Wyndam
Strodtbeck M.D.
338-339
Sunday,
Oct. 12
8-11 a.m. CC 813 Perioperative Resuscitation - What’s New? Steven Robicsek
M.D. Ph.D.
348-349
1-4 p.m. PN 816 Physical Exam Workshop for Pain
Physicians
Brian Starr M.D. 346-347
Monday, Oct.
13
8-11 a.m.
FA 821 Grant Writing and the NIH Study Section
for the Uninitiated
Michael Andreae
M.D.
348
9-11 a.m. PN 818 Practical Pain Medicine Coding
Compliance and Workow Strategies for
2014
Kevin Vorenkamp
M.D.
276-277
1-4 p.m. PI 829 Physician Performance Assessment and
Improvement: Practice Its Power for Your
Own Practice
Leslie Jameson
M.D.
356-357
RESIDENTS & MEDICAL STUDENTS
Date Time Track Fee Code Speaker Speaker Location
Friday, October
10
7:30-9 p.m. RM01 Residents and Medical Students
Grassroots Seminar
Jeffrey Plagenhoef
M.D.
Hilton Riverside
9-11 p.m. RM02 Resident and Medical Student Welcome
Reception
Mark Bicket M.D. Hilton Riverside
Saturday, Oct.
11
8-9:30 a.m. RM03 Models of Practice Panel Roy Soto M.D. R02-03
8-11 a.m. RM04a Medical Student Workshop-Ochsner
Health System
Mack Thomas
M.D.
Offsite
SCHEDULE BY SESSION TYPE

134
RM04b Medical Student Workshop-Louisiana
State University
Judy Johnson
M.D.
Offsite
RM04c Medical Student Workshop-Tulane
University
Lihua Zhang M.D. Offsite
9:30-11
a.m.
RM05 Resident Written Board Prep Sajid Shahul M.D R02-03
RM06 Subspecialty Panel Walter Maurer
M.D.
R04-05
1-2 p.m. RM07 Practice Management I Erica Stein M.D. R02-03
2-3 p.m. RM08 Practice Management II Judith Jurin Semo
J.D. Esq.
R02-03
3:30-5:30
p.m.
RM09 Residency Meet and Greet Chad Greene La Nouvelle
Ballroom C
Sunday,
Oct. 12
10:00 a.m.-
12 p.m.
RM10 Resident Component House of Delegates Mark Bicket M.D. R02-03
10 a.m.-1
p.m.
RM11 Medical Student Component House of
Delegates
Chad Greene R04-05
2-5 p.m. FA RM12 FAER Medical Student Anesthesia
Research Fellowship Symposium
Paloma Toledo
M.D. M.P.H.
R08-09
2:30-5 p.m. FA RM13 Resident Regional Anesthesia Workshop Julia Pollock M.D.
Raymond Joseph
M.D.
R06-07
GOVERNANCE EVENTS
Date Time Track Fee Code Speaker Speaker Location
Sunday,
Oct. 12
8 a.m.-
12 p.m.
SPE07 House of Delegates: Session I Jane C.K. Fitch
M.D.
Grand Ballroom,
Hilton Riverside
Wednesday,
Oct. 15
8 a.m.-12
p.m.
SPE26 House of Delegates: Session II Jane C.K. Fitch
M.D.
Grand Ballroom,
Hilton Riverside
SPECIAL MEETINGS & EVENTS
Date Time Track Fee Code Speaker Speaker Location
Saturday, Oct.
11
8-10 a.m. FA SPE01 Challenges in Anesthesiology: A European
Perspective
Daniela Filipescu
M.D.
265-268
10:30-
11:45 a.m.
SPE02 ANESTHESIOLOGY™ 2014 Opening
Session
Jane C.K. Fitch
M.D.
Great Hall AD
1-2 p.m. FA SPE03 Ellison C. Pierce Jr., M.D., Patient Safety
Memorial Lecture: Competence and
Teamwork Are Not Enough: The Value of
Cognitive Aids
David Gaba M.D. Great Hall B
2-4 p.m. CA SPE04 Perioperative Cardiology: Results from
VISION, POISE-2, SIRS and ENIGMA-2
Daniel I. Sessler
M.D.
Great Hall A
FA SPE05 Anesthesia Patient Safety Foundation
Workshop: Competence and Teamwork
Are Not Enough: Implementing Emergency
Manuals and Checklists
Jeffrey B. Cooper
Ph.D.
Great Hall B
Sunday,
Oct. 12
8-10 a.m. PI SPE06 WFSA Panel: Government Funded
Healthcare and Anesthesia - An
International Perspective on Successes
and Failures
Adrian W. Gelb
M.B., B.Ch.
Great Hall B
10-11 a.m. SPE27 PQRS Reporting via the QCDR Reporting
Channel
Richard P. Dutton
M.D. M.B.A.
252-254
12:30-1:30
p.m.
FA SPE08 Society for Airway Management
Ovassapian Lecture: The Airway Approach
Algorithm: What Would Andy Say?
William H.
Rosenblatt M.D.
Great Hall B
4-4:30 p.m. SPE09 ABA Informational Session: Assessment
Programs for Primary Certication in
Anesthesiology
Deborah Culley
M.D.
335-336
4:30-5 p.m. SPE10 ABA Informational Session: Maintenance
of Certication in Anesthesiology Program
(MOCA)
Deborah Culley
M.D.
335-336
EDUCATION

135
Monday,
Oct. 13
8-10 a.m. SPE11 Best of Abstracts: Basic Science James Rathmell
M.D.
265-268
FA SPE12 FAER Academy of Research Mentors:
Mentored Research Training Grants
(MRTG): Success Elements for Trainees
and Mentors
Evan D. Kharasch
M.D. Ph.D.
342
FA SPE13 International Forum on Patient Safety and
Quality Outcomes
Richard P. Dutton
M.D. M.B.A.
Great Hall B
10:20-
11:35 a.m.
SPE14 Emery A. Rovenstine Lecture: Health Care
at the Crossroads: The Imperative for
Change
Karen B. Domino
M.D. M.P.H.
Great Hall AD
11:45 a.m.-
1:15 p.m.
SPE15 Celebration of Research James C.
Eisenach M.D.
Great Hall B
2-3 p.m. FA SPE16 FAER - Helrich Research Lecture: The
Clinical Neuroscience of Anesthesia:
Research, Education and Patient Care
Emery N. Brown
M.D. Ph.D.
Great Hall B
2-4 p.m. FA SPE17 Patrick Sim Forum: An Afternoon With
the WLM Laureates of the History of
Anesthesia
David B. Waisel
M.D.
265-268
3-5 p.m. FA SPE18 FAER Panel: Future of Anesthesiology
Research
Zeljko Bosnjak
Ph.D.
Great Hall B
5-6 p.m. PI SPE19 How Can FAER’s New Education
Mentorship Academy Help Anesthesiology
Educators
Catherine Kuhn
M.D.
Great Hall B
Tuesday, Oct.
14
8-10 a.m. PN SPE20 Reduce Compliance Risks With Opioid
Prescribing
John F.
Dombrowski M.D.
Great Hall B
8-11 a.m. SPE21 Journal Symposium: How to Mechanically
Ventilate Patients in the Operating in
2014
Jeanine P. Wiener-
Kronish M.D.
275-277
10 a.m.-12
p.m.
SPE28 AQI Listening Session Richard P. Dutton
M.D. M.B.A.
223
10:30-
11:30 a.m.
PN SPE22 John W. Severinghaus Lecture on
Translational Science: Basic Science to
Clinical Practice: The Tale of Long-Acting
Opioids
Evan Kharasch
M.D. Ph.D.
Great Hall AD
12:40-1:50
p.m.
SPE23 Lewis H. Wright Memorial Lecture James P. Bagian
M.D.
265-268
1-3 p.m. SPE24 Best of Abstracts: Clinical Science James Rathmell
M.D.
275-277
2-4 p.m. PI SPE25 History Panel - Show Me the Money:
A Brief History of Remuneration in
Anesthesiology
Douglas R. Bacon
M.D. M.A.
265-268
SCHEDULE BY SESSION TYPE
136
Corporate Non-CME Educational Updates
Edwards Lifesciences, ASA Industry Supporter, Presents:
Perioperative Goal-Directed Therapy: A key element of the
Perioperative Surgical Home
Saturday, October 11 | 7-10 p.m. | Downtown Marriott at the
Convention Center – Blaine Kern Ballroom
William Hand, M.D.
Medical University of South Carolina
Charleston, SC
Mervyn Maze, M.B., Ch.B.
University of California San Francisco
San Francisco, CA
Tim Miller, M.B., Ch.B.
Duke University
Durham, NC
Monty Mythen, M.B., B.S.
University College London Hospitals
London, UK
Variability exists with care pathways and in particular amounts of
volume administered within same categories of surgical cases.
The Perioperative Surgical Home model is in part designed to
help decrease some of the variability across the continuum of
care of the surgical patient. Use of Perioperative Goal-Directed
Therapy to optimize uid management has been shown to reduce
post-surgical complications, length of stay and associated costs.
Precise uid management is a key element of the intraoperative
care model. This session addresses the data, type of surgical
cases, and rationale for implementation of a Perioperative Goal-
Directed Therapy approach for managing patients in the optimal
volume range. For more information and to register, please see an
Edwards representative at Booth #1307.
ACELRX PHARMACEUTICALS, ASA Annual Meeting Supporter,
Presents: The Future of PCA
Sunday, October 12 | 7-8 a.m. | Hilton Riverside, Jefferson
Ballroom
Gene Viscusi, M.D., Professor of Anesthesiology and Director,
Acute Pain Management
Harold Minkowitz, M.D., Anesthesiologist
The traditional and widely used IV patient-controlled analgesia
has been shown to cause harm to patients following surgery in a
number of ways including the adverse side effects of commonly
used opioids, the invasive IV route of delivery and the inherent
potential for programming and delivery errors associated with the
complexity of the infusion pumps. This educational session will
discuss the pros and cons of the traditional infusion pump and
explore innovative alternatives to post-operative pain medication
and delivery. For more information and to register, please see an
AcelRx representative at Booth #2129.
Masimo, ASA Industry Supporter, Presents:
Noninvasive Monitoring Advancements to Improve Perioperative
Geriatric Patient Safety
Sunday, October 12
Registration starting at 6:30 p.m.
Program and Dinner at 7-8:30 p.m.
New Orleans Marriott, Canal Street | Grand Ballroom
Emery N. Brown, M.D., Ph.D.
Massachusetts General Hospital
Boston, MA
Michael Ramsay, M.D., FRCA
Baylor University Medical Center
Dallas, TX
Aryeh Shander, M.D., FCCM, FCCP
Mount Sinai Hospital
New York, NY
A comprehensive update and case-based learning approach
to applying the latest advancements in noninvasive monitoring
in perioperative care with a focus on the geriatric patient. This
will encompass new advances in understanding the anesthesia
mechanism in the brain and identifying individual agent signatures
along with their utilization for anesthetic management, opioid
management and post-operative respiratory remote monitoring,
and transfusion management. For more information and to register,
please see a Masimo representative at Booth # 829.
Cheetah Medical, ASA Annual Meeting Supporter, Presents:
Clinical and Economic Considerations of Non-Invasive
Hemodynamic Monitoring in Perioperative Fluid Management
Sunday, October 12 | 7-10 p.m. | JW Marriott Hotel, New Orleans
Monty Mythen, M.B., B.S.
University College London Hospitals
London, UK
Paul Heerdt, M.D.
Weill Medical College of Cornell University
New York, NY
Tom Hopkins, M.D.
Duke University Hospital
Durham, NC
Fluid management strategies based on perioperative hemodynamic
monitoring have been shown to reduce surgical complications,
enable faster ambulation and shorten length of hospital stay. This
session will address how to mitigate post-operative complications
and enhance recovery by optimizing intraoperative uid therapy.
It will cover the use of hemodynamic parameters to guide uid
management, as well as the available options for perioperative
hemodynamic monitoring with focus on the 100% noninvasive
CHEETAH NICOM technology. Finally, it will discuss an innovative
method for hospitals evaluating the cost effectiveness for
noninvasive hemodynamic monitoring. For more information and to
register, please see a Cheetah Medical representative at Booth #
1915.
CORPORATE NON-CME EDUCATION EVENTS

137
CORPORATE NON-CME EDUCATION EVENTS
NOTES

138
Foundation for Anesthesia Education and Research (FAER)
FOUNDING SUPPORTER
American Society of Anesthesiologists
The Foundation for Anesthesia Education and Research
thanks its founding supporter, the American Society of
Anesthesiologists, for its $2 million in funding in 2013.
COMPONENT SOCIETY CONTRIBUTORS
$5,000 or more
Arizona Society of Anesthesiologists
Connecticut State Society of Anesthesiologists
Minnesota Society of Anesthesiologists
Tennessee Society of Anesthesiologists
Texas Society of Anesthesiologists
$2,000-$4,999
California Society of Anesthesiologists
Kansas State Society of Anesthesiologists
Maine Society of Anesthesiologists
Massachusetts Society of Anesthesiologists
Michigan Society of Anesthesiologists
New York State Society of Anesthesiologists
Oklahoma Society of Anesthesiologists
Virginia Society of Anesthesiologists
Washington State Society of Anesthesiologists
$1,000-$1,999
Alabama State Society of Anesthesiologists
DC Society of Anesthesiologists
Florida Society of Anesthesiologists
Georgia Society of Anesthesiologists
Illinois Society of Anesthesiologists
Indiana Society of Anesthesiologists
Iowa Society of Anesthesiologists
Kentucky Society of Anesthesiologists
Maryland Society of Anesthesiologists
Ohio Society of Anesthesiologists
Oregon Society of Anesthesiologists
Pennsylvania Society of Anesthesiologists
South Dakota Society of Anesthesiologists
Wisconsin Society of Anesthesiologists
Up to $999
Arkansas Society of Anesthesiologists
Colorado Society of Anesthesiologists
Kansas City Society of Anesthesiologists
Mississippi Society of Anesthesiologists
New Jersey State Society of Anesthesiologists
New Mexico Society of Anesthesiologists
Rhode Island Society of Anesthesiologists
South Carolina Society of Anesthesiologists
Utah Society of Anesthesiologists
Vermont Society of Anesthesiologists
West Virginia Society of Anesthesiologists
Wyoming Society of Anesthesiologists
SUBSPECIALTY SOCIETY CONTRIBUTORS
$30,000
$15,000
Up to $5,000
Society of Academic Anesthesiology Associations (SAAA)
Society for the Advancement of Geriatric Anesthesia (SAGA)
Society of Cardiovascular Anesthesiologists (SCA)
Society of Critical Care Anesthesiologists (SOCCA)
Society for Education in Anesthesia (SEA)
Society for Neuroscience in Anesthesiology and Critical Care
(SNACC)
Society for Obstetric Anesthesia & Perinatology (SOAP)
CORPORATE DONORS
$25,000-$49,999
$10,000-$24,999
$5,000-$9,999
AxelRX Pharmaceuticals, Inc.
Baxter Healthcare Corporation
Draeger Medical Inc.
Frank Moya Continuing Education Programs
Piramal Critical Care Inc.
Preferred Physicians Medical
$1,000-$4,999
B. Braun Medical Inc.
Galleon Pharmaceutics
Karl Storz Endoscopy
Mainline Medical
Sheridan Healthcare
TEAMHealth
FAER DONOR LIST

139
SOCIETY FOR ANESTHESIA EDUCATION AND RESEARCH –
ANESTHESIOLOGY DEPARTMENT DONORS
University of Alabama at Birmingham
Albany Medical Center
Albert Einstein College of Medicine/Monteore Medical Center
Anesthesiology Institute, Cleveland Clinic
Brigham and Women’s Hospital
University of California Davis
University of California Irvine
University of California San Diego
University of California San Francisco
University of Cincinnati Medical Center
University of Colorado
Columbia University College of Physicians and Surgeons
Dartmouth-Hitchcock Medical Center
David Geffen School of Medicine at UCLA
Duke University
Emory University School of Medicine
Fletcher Allen Health Care
University of Florida College of Medicine
George Washington University
Georgetown University Hospital
Georgia Health Sciences University
Henry Ford Hospital
Icahn School of Medicine at Mount Sinai
University of Illinois at Chicago
University of Iowa
John H. Stroger Hospital of Cook County
Johns Hopkins University
Loma Linda University
University of Louisville
Loyola University Medical Center
University of Maryland School of Medicine
Massachusetts General Hospital
University of Massachusetts Medical School
Mayo Clinic Rochester
Medical College of Wisconsin
University of Minnesota
University of Missouri-Kansas City
University of Nebraska Medical Center
University of New Mexico School of Medicine
New York University Medical Center
University of North Carolina Hospitals
Northwestern University Feinberg School of Medicine
Ohio State University
University of Oklahoma Health Sciences Center
Park Slope Anesthesia Associates of New York Methodist Hospital
University of Pennsylvania School of Medicine
Penn State Milton S. Hershey Medical Center
University of Pittsburgh Medical Center
University of Rochester Medical Center
Springeld Anesthesia Services of Baystate Medical Center
Stanford University Medical Center
State University of New York, Brooklyn (Downstate)
State University of New York, Buffalo
State University of New York, Stony Brook
State University of New York, Upstate Medical University
St. Luke’s-Roosevelt Hospital Center
University of Tennessee Medical Center at Knoxville
University of Texas Medical Branch-Galveston
University of Texas Southwestern Medical Center
Tufts Medical Center
Vanderbilt University School of Medicine
University of Virginia
University of Washington
Washington University School of Medicine in St. Louis
Wayne State University School of Medicine
Weill Cornell Medical College
University of Wisconsin, Madison
Yale University
PRACTICE GROUP & ANESTHESIOLOGY DEPARTMENT
CONTRIBUTORS
Anesthesia Consultants Medical Group
Harvard Medical Faculty Physicians
Northwestern University Feinberg School of Medicine
Palm Beach Spine & Diagnostic Institute
Ohio State University
Olympic Anesthesia Services
Parish Management Consultants
Park Slope Anesthesia
Pratt Anesthesiology Associates
Santa Fe Anesthesia Specialists, PC
Southern Tier Anesthesiologists, PC
Spectrum Medical Group
Springeld Anesthesia Services
Westside Anesthesiology PC
UF Health Science Center Jacksonville
University Anesthesiologists, S.C.
University of Wisconsin, Madison
INDIVIDUAL SUPPORTERS
FAER would like to thank the many individuals in the
anesthesiology community who support FAER through charitable
contributions each year. For a complete list of individual
contributors, pick up a copy of the 2013/2014 annual report at
the FAER booth in the ASA Resource Center or visit FAER.org and
review the annual report online.
SUPPORT RESEARCH AND EDUCATION IN ANESTHESIOLOGY
You can help fund discovery and innovation in anesthesiology that
will change the future of medical practice and patient care. To
make a contribution, visit the FAER booth or go to FAER.org/donate.
FAER DONOR LIST
140
Anesthesia Patient Safety Foundation Donor List (APSF)
Corporate Donors
Founding Patron
American Society of Anesthesiologists
Sustaining Professional Association
($125,000 and higher)
American Association of Nurse Anesthetists
Grand Patron ($100,000 and higher)
Covidien
Sponsoring Patron ($30,000-$49,999)
Preferred Physicians Medical Risk Retention Group
Benefactor Patron ($20,000-$29,999)
AbbVie
Baxter Anesthesia and Critical Care
CareFusion
GE Healthcare
Masimo Foundation
PharMEDium Services
The Doctors Company Foundation
Patron ($10,000-$19,999)
Cook Medical
Draeger Medical
Edwards Lifesciences
Merck and Company
Philips Healthcare
Spacelabs Medical
Teleex Medical
Sustaining Donor ($5,000 to $9,999)
Becton Dickinson
Codonics
Mindray North America
Nihon Kohden America, Inc
Pall Corporation
Respiratory Motion
Sheridan Healthcorp, Inc
Smiths Medical
Sponsoring Donor ($1,000 to $4,999)
AMBU, Inc
Anesthesia Business Consultants
Belmont Instrument Corporation
B. Braun Medical, Inc
Hospira, Inc
iMDsoft
Intersurgical, Inc
Micropore Inc
SenTec AG
TRIFID Medical Group LLC
W.R. Grace
Corporate Level Donor ($500 to $999)
NeuroWave Systems
Paragon Service
ProMed Strategies
Wolters Kluwer
Subscribing Societies
American Society of Anesthesia Technologists and Technicians
American Society of Dentist Anesthesiologists
Community Donors
(includes individuals, anesthesia groups, specialty organizations,
state societies)
Grand Sponsor ($15,000 and higher)
US Anesthesia Partners (GHA-Houston, JLR-Orlando,
Pinnacle-Dallas)
Benefactor Sponsor ($5,000 to $14,999)
Alabama State Society of Anesthesiologists
American Academy of Anesthesiologist Assistants
Anaesthesia Associates of Massachusetts
Anesthesia Medical Group (Nashville, TN)
Anonymous
Connecticut State Society of Anesthesiologists
Indiana Society of Anesthesiologists
Minnesota Society of Anesthesiologists
Frank B. Moya, MD, Continuing Education Programs
North American Partners in Anesthesia
Robert K. Stoelting, MD
Tennessee Society of Anesthesiologists
Valley Anesthesiology Foundation
Thomas F. Walker, MD
Sustaining Sponsor ($2,000 to $4,999)
Anesthesia Consultants Medical Group
Anesthesia Resources Management
Arizona Society of Anesthesiologists
Madison Anesthesiology Consultants
Massachusetts Society of Anesthesiologists
Michiana Anesthesia Care
Michigan Society of Anesthesiologists
Michael D. Miller, MD
North Carolina Society of Anesthesiologists
Old Pueblo Anesthesia Group
Pennsylvania Society of Anesthesiologists
Raizman Frischman Maatzus & Rizza
Society of Academic Anesthesiology Associations
Society of Cardiovascular Anesthesiologists
Springeld Anesthesia Service at Baystate Medical Center
Contributing Sponsor ($750 to $1,999)
Afliated Anesthesiologists of Oklahoma City, OK
Alaska Association of Nurse Anesthetists
Alaska Society of Anesthesiologists
AllCare Clinical Associates (Asheville, NC)
American Association of Oral and Maxillofacial Surgeons
American Society of PeriAnesthesia Nurses
Anesthesia Services of Birmingham
Associated Anesthesiologists of St. Paul, MN
Balboa Anesthesia Group
Casey D. Blitt, MD
Dr. and Mrs. Robert A. Caplan
Frederick W. Cheney, MD
California Society of Anesthesiologists
Jeffrey B. Cooper, PhD
Dr. and Mrs. Robert Cordes
David S. Currier, MD
District of Columbia Society of Anesthesiologists
John H. Eichhorn, MD
Gerald Feldman
Foundation for Anesthesia Education and Research
Georgia Society of Anesthesiologists
Mark P. Fritz, MD
Goldilocks Anesthesia Foundation
Illinois Society of Anesthesiologists
Iowa Society of Anesthesiologists
APSF DONOR LIST

141
Kansas City Society of Anesthesiologists
Kentucky Society of Anesthesiologists
Lorri A. Lee, MD
Anne Marie Lynn, MD
Maryland Society of Anesthesiologists
Joseph L. Meltzer, MD
Patricia A. Meyer, PharmD
Missouri Society of Anesthesiologists
Nevada State Society of Anesthesiologists
Northwest Anesthesia Physicians
Nurse Anesthesia of Maine
Ohio Academy of Anesthesiologist Assistants
Ohio Society of Anesthesiologists
Oklahoma Society of Anesthesiologists
Oregon Society of Anesthesiologists
Frank J. Overdyk, MSEE, MD
Pamela P. Palmer, MD
Srikanth S. Patankar, MD
A. William Paulsen, PhD, AA-C
James M. Pepple, MD
Physician Anesthesia Service
Rhode Island Society of Anesthesiologists
Laura M. Roland, MD
Carol E. Rose, MD
Drs. Ximena and Daniel Sessler
Society for Airway Management
Society for Ambulatory Anesthesia
Society for Obstetric Anesthesia and Perinatology
Society for Pediatric Anesthesia Patient Safety and Education Fund
South Dakota Society of Anesthesiologists
South Denver Anesthesiologists
Spectrum Medical Group
Stockham-Hill Foundation
Tejas Anesthesia
Texas Association of Nurse Anesthetists
Texas Society of Anesthesiologists
The Saint Paul Foundation
Mary Ellen and Mark A. Warner
Washington State Society of Anesthesiologists
Wisconsin Association of Nurse Anesthetists
Wisconsin Society of Anesthesiologists
Sponsor ($200 to $749)
Anesthesia Associates of Columbus, GA
Anesthesia Associates of Kansas City
Anesthesia Associates of Northwest Dayton, Inc.
Donald E. Arnold, MD
Robert L. Barth, MD
William C. Berger, MD
Vincent C. Bogan, CRNA
Amanda Burden, MD
Lillian K. Chen, MD
Joan M. Christie, MD
Marlene V. Chua, MD
Daniel J. Cole, MD
Melvin A. Cohen, MD
Colorado Society of Anesthesiologists
Glenn E. DeBoer, MD
Andrew E. Dick, MD
Rajiv Doshi, MD
Richard P. Dutton, MD, MBA
Stephen B. Edelstein, MD
Jan Ehrenwerth, MD
Michael R. England, MD
Cynthia A. Ferris, MD
Georgia Association of Nurse Anesthetists
Ian J. Gilmour, MD
Richard Gnaedinger, MD
James D. Grant, MD
Joel G. Greenspan, MD
Allen N. Gustin, MD
Robert J. Hahn, MD
John A. Hamel, MD
Timothy N. Harwood, MD
Gary R. Haynes, MD
Daniel E. Headrick, MD
John F. Heath, MD
Simon C. Hillier, MD
Glen E. Holley, MD
Paul M. Jaklitsch, MD
Robert E. Johnstone, MD
Kansas Society of Anesthesiologists
Marshal B. Kaplan, MD
Heidi M. Koenig, MD
Michael G. Kral, MD
James Lamberg, DO
Hans Larsen, CRNA (in honor of Dr. Timothy Dowd)
Rodney C. Lester, PhD, CRNA
Kevin P. Lodge, MD
Michael J. Loushin, MD
Maine Society of Anesthesiologists
Edwin Mathews, MD
Gregory B. McComas, MD
E. Kay McDivitt, MD
Mississippi Society of Anesthesiologists
Roger A. Moore, MD
Robert C. Morell, MD
Soe Myint, MD
Joseph J. Naples, MD
John B. Neeld, MD
New Jersey State Society of Anesthesiologists
New Mexico Society of Anesthesiologists
Mark C. Norris, MD
Ducu Onisei, MD
Michael A. Olympio, MD
Mukesh K. Patel, MD
Pennsylvania Association of Nurse Anesthetists
Lee S. Perrin, MD
Drs. Beverly and James Philip
Tian Hoe Poh, MD
Matthew W. Ragland, MD
Neela Ramaswamy, MD (in honor of Dr. Bhattacahyra)
Maunak E Rana, MD
Yashesh R. Savani, MD
Howard Schapiro and Jan Carroll
Sanford H. Schaps, MD
David Solosko and Sandra Kneiss
South Carolina Society of Anesthesiologists
Shepard B. Stone, PA
Kenneth R. Stone, MD
Mark L. Stram, MD
Dr. and Mrs. Stephen J. Thomas
Bijo J. Thomas, MD
University of Maryland Anesthesiology Associates
Susan A Vassallo, MD (in honor of Neelakantan Sunder, MD)
J. Clark Venable, MD
Vermont Society of Anesthesiologists
Virginia Society of Anesthesiologists
Denham S. Ward, MD, PhD
Thomas L. Warren, MD
Mark and Heidi Weber
Matthew B. Weinger, MD
Andrew Weisinger, MD
West Florida Anesthesia Consultants
APSF DONOR LIST
142
West Virginia State Society of Anesthesiologists
Wichita Anesthesiology, Chartered
Mark D. Zajkowski, MD, DDS
In Memoriam
In memory of Margie Frola, CRNA (Sharon Rose Johnson, MD)
In memory of Hank Davis, MD (Sharon Rose Johnson, MD)
In memory of Andrew Glickman, MD (Sharon Rose Johnson, MD)
In memory of Ellison C. Pierce, Jr., MD
(Alexander A. Hannenberg, MD)
In memory of E. S. Siker, MD (Donal Lucas Pelligrini, MD)
In memory of E. S. Siker, MD (Christopher Troianos, MD)
In memory of Howard Zauder, MD (James P. McMichael, MD)
In memory of E. S. Siker, MD (Drs. Susan E. and Jerry A. Dorsch)
In memory of Stanley E. Borum, MD
(Texas Society of Anesthesiologists)
In memory of Enoch C. McReynolds, MD
(Texas Society of Anesthesiologists)
In memory of Russell Morrison, CRNA, MS
(Jeanne M. Kachnij, CRNA, MS)
In memory of Mark G. Ewell, MD
(Texas Society of Anesthesiologists)
Note: Donations are always welcome.
Donate online at apsf.org/donate_form.php or mail to APSF, 1061
American Lane, Schaumburg, IL 60173-4973
(Donor list current through July 08, 2014)
APSF DONOR LIST

143
APSF DONOR LIST
NOTES
144
Hope For The Warriors® - Run For The Warriors®
Sunday, October 12 | 6 a.m.
Following last year’s successful event in San Francisco, ASA is
sponsoring, for a fth consecutive year, Hope For The Warriors®
- Run For The Warriors®. Run along the mighty Mississippi by
participating in the ASA Run For The Warriors® 5k Run/Walk
sponsored in collaboration with Hope For The Warriors®.
This event will bring together meeting attendees, exhibitors, local
residents and military personnel in an effort to support wounded
warriors and their families.
Check in at the Run For The Warriors booth for details on the race.
Share this experience by asking your friends and colleagues to
join you. If you have not yet registered for the run, please visit
the Hope For The Warriors® booth located in Lobby B1 of the
Convention Center.
ASA Welcome Reception
Saturday, October 11 | 5-6:30 p.m.
In its fth year, the ANESTHESIOLOGY™ 2014 annual meeting
attendee and exhibitor Welcome Reception will take place on
Saturday, October 11, 5-6:30 p.m. at the Convention Center
in the exhibit area.
All registrants will be encouraged to stop by the reception to
mingle and network with their fellow physicians and visit with
ASA’s corporate supporters and exhibitors.
Connection Center
One of the numerous benets to attending the
ANESTHESIOLOGY™ 2014 annual meeting is the opportunity to
meet your peers from around the world. We’ve built the program
with that in mind and created the Connection Center just for you!
The Connection Center is your chance to meet other attendees,
share your experiences and explore the latest technology, science
and medicine in one convenient space. At the Connection Center
you’ll nd:
ASA Resource Center
Convention Center, Hall B-1
Friday, October 10 | 3-7 p.m.
Saturday, October 11 | 7 a.m.-6:30 p.m.
Sunday, October 12-Tuesday, October 14 | 7 a.m.-5 p.m.
Be sure to stop by the ASA Resource Center to explore ASA
offerings and meet our staff. You can update your membership,
make a PAC donation, learn about the new WLM library and more.
Exhibits
Complete details about exhibits may be found in the separate
Exhibit Guide online.
Convention Center, Halls B2-D
Saturday, October 11 | 11 a.m.-6:30 p.m.
Sunday, October 12 | 9 a.m.-4 p.m.
Monday, October 13 | 9 a.m.-3 p.m.
ASA Connection Lounges 1 & 2
Convention Center, Halls B-2 & D
Make this space your go-to-place to recharge yourself and your
mobile device. The ASA Connection Lounges are a great place to
share stories and discuss challenges while relaxing and
catching-up on e-mail in the exhibit hall.
Scientic and Educational Exhibits
Convention Center, Hall D
Visit the Scientic and Educational Exhibits area to learn about
new technologies, practices, equipment and other important topics
in the eld of anesthesiology. Please note, the Scientic and
Educational Exhibits are not designated for CME credit.
Afliated Subspecialty Society Pavilion, Booth #111
ASRA: American Society of Regional Anesthesia and Pain Medicine
SAMBA: Society for Ambulatory Anesthesia
SCA: Society of Cardiovascular Anesthesiologists
SEA: Society for Education in Anesthesia
SOCCA: Society of Critical Care of Anesthesiologists
SOAP: Society for Obstetric Anesthesia and Perinatology
NETWORK

145
Enjoy lunch at the ASA Bistro
Convention Center, Hall E, behind aisle 2300
Saturday, October 11-Monday October 13
11 a.m.- 2:30 p.m.
Food and beverage services are available within the Morial
Convention Center at the ASA Bistro, inside Hall E. There are also
many restaurants located in the surrounding area outside of Morial
Convention Center. You will also nd a list of restaurants in the
New Orleans area on the new ANESTHESIOLOGY™ 2014 online
community and our ASA website.
The ASA Bistro provides a comfortable setting for attendees to
eat, meet and network during the meeting. Located right on the
exhibit oor, you will no longer have to leave the convention center
to get a great meal at a good price. For only $26, including tax, you
will get a delicious variety of menu items, including beverages and
dessert.
Daily lunch menus includes salads, soup, entrée choices,
vegetables, pasta and more.
There will be ample seating for everyone, and the food and
beverage locations inside the exhibit hall will be easily accessible
to all the education areas. Sit down, relax and enjoy some great
food all at a convenient location to accommodate your busy
schedule.
Need ASA Bistro tickets?
Visit the Bistro kiosk located in the Convention Center, Lobby 1.
International Connection Lounge
Convention Center
Friday, October 10 | 3-7 p.m.
Saturday, October 11-Tuesday, October 14 | 7 a.m.-5 p.m.
International attendees can connect with their colleagues from
across the globe at our International Connection Lounge. The
connection lounge will have language facilitators on hand who
speak Chinese, Japanese, Portuguese and Spanish. International
attendees are also encouraged to utilize the connection lounge
to schedule a meeting with colleagues in one of our small
meeting rooms, as space permits. Relax in the lounge area or
talk with, ESA Voyages, our international travel partner, about
plans for next year’s meeting in San Diego. To recognize our
international attendees, ASA will provide a ribbon distinguishing
our international attendees, which can be picked up while in the
connection center. Certicates of attendance will be available at
the connection center.
The International Attendee Connection Lounge will not be open on
Wednesday, October 15.
Online Community: Stay Connected
ASA is once again offering an online community to enhance
attendees’ meeting experience. The ANESTHESIOLOGY™ 2014
annual meeting online community will allow you to:
• View the proles and interests of other attendees
• Discover which contacts from Facebook, Twitter and
LinkedIn are also attending
• Build a personalized schedule of sessions to attend
• Download handouts and other materials
• Schedule 1:1 meetings with other attendees
• Converse with users during and after the meeting
• Receive recommendations on who to meet at the meeting
based on your prole
• Search for people at the meeting who share your interests
• Get speaker prole lists and attendee lists on session pages
• Access a full mobile experience on iPhone, iPad, Android and
Blackberry
• See the educational sessions and events your colleagues
are attending
• Engage in conversations with presenters
• Schedule 1:1 meetings with exhibitor personnel
• Search and view exhibiting companies, products and
descriptions
• Search educational sessions
• Receive notications and real-time alerts on can’t-miss events
and important information
• Calendar-to-calendar overlay so you can schedule appointments
with attendees and exhibitors without conicting with their
current schedule
• Find designated meeting areas that will be made available at
the Ernest N. Morial Convention Center so you can message the
location to meet with an exhibitor or attendee through the online
community
• Access and view the ePosters website through the online
community when it becomes available during the rst day of
registration on site in New Orleans.
• Access the mobile-friendly registration site from the online
community
• Easily create a prole, which is 90 percent completed and
captured from your registration
• Create private chat rooms by invitation only to other attendees.
Accessing the New Online Community
Upon registering for the ANESTHESIOLOGY™ 2014 annual
meeting, attendees will receive a personalized email from Pathable
inviting them to join the annual meeting online community. The
e-mail used for registration is the same e-mail account to which
the invitation will be sent. If you have any questions about
accessing your personal online community account, please let
an ASA staff member know at any of the information counters
in Lobby A and D of the Convention Center, or stop by the booth
dedicated to the online community in Lobby B-1. Don’t miss out
on this chance to connect with your colleagues, maximize your
networking opportunities and organize your time in New Orleans.
CONNECTION CENTER
146
Governance
House of Delegates
Governance Meetings will be held at the Hilton New Orleans
Riverside (ASA’s Headquarters hotel).
House of Delegates, Session I
Sunday, October 12
8 a.m. | Hilton Riverside, Grand Ballroom
This session will include award presentations and remarks by the
President and President Elect. Nominations of 2015 Ofcers will
be made from the oor of the House.
Reference Committee Hearings
Sunday, October 12
1:15 p.m. | Hilton Riverside, Grand Ballroom
Open hearings will be conducted by each of the appointed
Reference Committees. Each committee will consider the reports
attributed to it in the Delegate’s handbook. These sessions are
required to remain open until at least 3 p.m., but must conclude
no later than 5 p.m.
Reference Committees
Sunday, October 12
Administrative Affairs
1:15-5 p.m. | Hilton Riverside, Grand Salon A, Sec. 1-6
Professional Affairs
1:15-5 p.m. | Hilton Riverside, Grand Salon B, Sec. 7-8, 10-11
Scientic Affairs
1:15-5 p.m. | Hilton Riverside, Grand Salon C, Sec. 17-18, 20-21
Finance
1:15-5 p.m. | Hilton Riverside, Grand Salon C, Sec. 16, 19, 22
House of Delegates, Session II
Wednesday, October 15
8 a.m. | Hilton Riverside, Grand Ballroom
This session renders decisions on actions of the Board of
Directors and new business brought before the governing body
prior to announced deadlines. Ofcers are elected and installed.
October Interim Board Meeting
Wednesday, October 15
The October Interim Board of Directors meeting immediately
follows the House of Delegates Session II. This session elects the
committees of the Board and conducts other business that will set
the tone for the 2015 governance year.
Orientation Sessions
Committee, Section and Division Chair Orientation
Friday, October 10
2-5 p.m. | Hilton Riverside, Melrose
New Delegates Orientation Meeting
Saturday, October 11
8-9 a.m. | Hilton Riverside, Grand Salon A, Sec. 3 & 6
Caucuses
Candidates’ Visits to Caucuses
Candidates in contested elections will address the ve regional
caucuses at their regularly scheduled sessions. Each candidate
will be assigned times and locations so that no two candidates
are in the same venue simultaneously. The amount of time that
each candidate may address the caucus and engage in a Q&A
session will be determined by the number of candidates who have
announced their intent to seek elected ofce prior to the July
deadline.
Caucus Schedule
All regional and state caucus meetings will be held at the Hilton
New Orleans Riverside. Times, days and locations are subject to
change.
Regional Caucus Meetings
Regional Caucus Chairs Meeting
Tuesday, October 14
10-11 a.m. | Hilton Riverside, Melrose
Academic Caucus
Saturday, October 11
3-5 p.m. | Hilton Riverside, Oak Alley
Frontier Caucus
Saturday, October 11
12-2 p.m. | Hilton Riverside, Oak Alley
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Oak Alley
Mid-Atlantic Caucus
Saturday, October 11
2:30-5 p.m. | Hilton Riverside, Grand Salon C, Sec. 13-18
Tuesday, October 14
3:30-6 p.m. | Hilton Riverside, Grand Salon C, Sec. 13-18
Midwest Caucus
Saturday, October 11
2:30-4:30 p.m. | Hilton Riverside, Grand Salon B, Sec. 7-12
Tuesday, October 14
3-6 p.m. | Hilton Riverside, Grand Salon B, Sec. 7-12
New England Caucus
Saturday, October 11
1-4:30 p.m. | Hilton Riverside, Melrose
Tuesday, October 14
3:30-6:00 p.m. | Hilton Riverside, Melrose
Southern Caucus
Saturday, October 11
2:30-5 p.m. | Hilton Riverside, Grand Salon A
Tuesday, October 14
3-5:30 p.m. | Hilton Riverside, Grand Salon A
Western Caucus
Saturday, October 11
2:15-4:15 p.m. | Hilton Riverside, Grand Salon D
Tuesday, October 14
3:15-6 p.m. | Hilton Riverside, Grand Salon D
NETWORK

147
State Caucus Meetings
California
Saturday, October 11
12-2 p.m. | Hilton Riverside, Grand Salon D
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Grand Salon D
Florida
Saturday, October 11
12:30-2:30 p.m. | Hilton Riverside, Hilton Expo Center A
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Grand Salon A
Georgia
Saturday, October 11
1-2 p.m. | Hilton Riverside, Warwick
Tuesday, October 14
2-3 p.m. | Hilton Riverside, Warwick
Illinois
Saturday, October 11
12:30-2:30 p.m. | Hilton Riverside, Elmwood
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Elmwood
Maryland
Tuesday, October 14
2:30-3:30 p.m. | Hilton Riverside, Norwich
Missouri
Saturday, October 11
7-9 a.m. | Hilton Riverside, Rosedown
Tuesday, October 14
1:30-3:30 p.m. | Hilton Riverside, Rosedown
Nevada
Tuesday, October 14
10:30-11:30 a.m. | Hilton Riverside, Trafalgar
New Jersey
Tuesday, October 14
6-7 p.m. | Hilton Riverside, Durham
New York
Saturday, October 11
10 a.m.-12 p.m. | Hilton Riverside, Rosedown
Tuesday, October 14
10 a.m.-12 p.m. | Hilton Riverside, Rosedown
Ohio
Saturday, October 11
1:30-3:30 p.m. | Hilton Riverside, Durham
Tuesday, October 14
1:30-3:30 p.m. | Hilton Riverside, Durham
Pennsylvania
Saturday, October 11
12-1:15 p.m. | Hilton Riverside, Melrose
1:30-2:30 p.m. | Hilton Riverside, Jasperwood
Tuesday, October 14
2:30-3:30 p.m. | Hilton Riverside, Jasperwood
Pennsylvania Resident
Saturday, October 11
10:30 a.m.-12 p.m. | Hilton Riverside, Durham
Tennessee
Saturday, October 11
12-2 p.m. | Hilton Riverside, Fountain
Tuesday, October 14
1-2:30 p.m. | Hilton Riverside, Melrose
Texas
Saturday, October 11
12:30-2:30 p.m. | Hilton Riverside, Jefferson Ballroom
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Jefferson Ballroom
Virginia
Saturday, October 11
12-2 p.m. | Hilton Riverside, Hilton Expo Center #2
Wisconsin
Saturday, October 11
12-1 p.m. | Hilton Riverside, Magnolia
Committee Meetings
All committee meetings will be held at the Hilton New Orleans
Riverside. Times, days and locations are subject to change.
Committee on Academic Anesthesiology
Monday, October 13
7-9 a.m. | Hilton Riverside, Rosedown
Committee on Ambulatory Surgical Care
Monday, October 13
1-2:30 p.m. | Hilton Riverside, Jasperwood
Committee on Anesthesia Care Team
Tuesday, October 14
8-11 a.m. | Hilton Riverside, Grand Salon B, Sec. 7 & 10
Committee on Anesthesiologist Assistant Education and Practice
Monday, October 13
1-3:30 p.m. | Hilton Riverside, Grand Salon C, Sec. 13 & 16
Committee on Annual Meeting Oversight
Tuesday, October 14
8-10 a.m. | Hilton Riverside, Grand Salon A, Sec. 3 & 6
Committee on Blood Management
Monday, October 13
2-3:30 p.m. | Hilton Riverside, Elmwood
Committee on Bylaws
Tuesday, October 14
10:30 a.m.-12 p.m. | Hilton Riverside, Norwich
Committee on Cardiovascular and Thoracic Anesthesia
Sunday, October 12
1-2:30 p.m. | Hilton Riverside, Oak Alley
Committee on Communications
Tuesday, October 14
9-10:30 a.m. | Hilton Riverside, Elmwood
Committee on Critical Care Medicine
Monday, October 13
8-9:30 a.m. | Hilton Riverside, Grand Ballroom A, Sec. 4
Committee on Economics
Tuesday, October 14
7-10 a.m. | Hilton Riverside, Jasperwood
147
ASA GOVERNANCE PROGRAM
148
Committee on Economics – Contractor Advisory Committee (CAC)
Tuesday, October 14
10-11 a.m. | Hilton Riverside, Jasperwood
Committee on Electronic Media and Information Technology
Monday, October 13
2-5 p.m. | Hilton Riverside, Magnolia
Committee on Equipment and Facilities
Saturday, October 11
7-9 a.m. | Hilton Riverside, Oak Alley
Committee on Equipment and Facilities Task Force on
Environmental Sustainability
Tuesday, October 14
8-9:30 a.m. | Hilton Riverside, Norwich
Committee on Ethics
Saturday, October 11
7-10 a.m. | Hilton Riverside, Magnolia
Committee on Expert Witness Testimony Review
Tuesday, October 14
1-3 p.m. | Hilton Riverside, Trafalgar
Committee on Future Models of Anesthesia Practice
Monday, October 13
7:30-10 a.m. | Hilton Riverside, Grand Salon A, Sec. 3-6
Committee on Geriatric Anesthesia
Monday, October 13
11 a.m.-12:30 p.m. | Hilton Riverside, Melrose
Committee on Global Humanitarian Outreach
Tuesday, October 14
8-10 a.m. | Hilton Riverside, Grand Salon C, Sec. 13 & 16
Committee on Governance Effectiveness and Efciencies
Monday, October 13
8-10 a.m. | Hilton Riverside, Hilton Expo Center A
Committee on Governmental Affairs
Monday, October 13
8-10 a.m. | Hilton Riverside, Oak Alley
Committee on Health Policy Research
Friday, October 10
5-7 p.m. | Hilton Riverside, Norwich
Committee on Large Group Practice
Tuesday, October 14
8-10 a.m. | Hilton Riverside, Jefferson Ballroom
Committee on Membership
Monday, October 13
8-9 a.m. | Hilton Riverside, Jasperwood
Committee on Neuroanesthesia
Saturday, October 11
2-3 p.m. | Hilton Riverside, Trafalgar
Committee on Newsletter
Tuesday, October 14
10:30 a.m.-12 p.m. | Hilton Riverside, Elmwood
Committee on Obstetric Anesthesia
Saturday, October 11
9-10 a.m. | Hilton Riverside, Durham
Committee on Occupational Health
Tuesday, October 14
8-10 a.m. | Hilton Riverside, Magnolia
Committee on Occupational Health Special Session
Monday, October 13
1-2 p.m. | Hilton Riverside, Durham
Committee on Pain Medicine
Sunday, October 12
1:30-3 p.m. | Hilton Riverside, Rosedown
Committee on Pain Medicine – Subcommittee on Palliative
Medicine
Sunday, October 12
3-4 p.m. | Hilton Riverside, Norwich
Committee on Patient Safety and Education
Monday, October 13
9-10:30 a.m. | Hilton Riverside, Grand Salon D, Sec. 19 & 22
Committee on Pediatric Anesthesia
Saturday, October 11
9:30-11 a.m. | Hilton Riverside, Oak Alley
Committee on Performance and Outcomes Measurement
Monday, October 13
6:30-8 a.m. | Hilton Riverside, Trafalgar
Committee on Practice Management
Monday, October 13
7-10 a.m. | Hilton Riverside, Melrose
Committee on Problem-Based Learning Discussions
Monday, October 13
7-8 a.m. | Hilton Riverside, Durham
Committee on Professional Diversity
Sunday, October 12
11:15 a.m.-1 p.m. | Hilton Riverside, Magnolia
Committee on Professional Liability
Saturday, October 11
7-8:30 a.m. | Hilton Riverside, Durham
Committee on Quality Management and Departmental
Administration
Tuesday, October 14
7-10 a.m. | Hilton Riverside, Oak Alley
Committee on Regional Anesthesia
Monday, October 13
1-2:30 p.m. | Hilton Riverside, Trafalgar
Committee on Residents and Medical Students
Saturday, October 11
11 a.m.-12 p.m. | Hilton Riverside, Jasperwood
Committee on Respiratory Care
Saturday, October 11
8-9:30 a.m. | Hilton Riverside, Trafalgar
NETWORK

149
Committee on Rural Access to Anesthesia Care
Sunday, October 12
7-8 a.m. | Hilton Riverside, Magnolia
Committee on Scientic Advisory
Monday, October 13
3-4 p.m. | Hilton Riverside, Jasperwood
Committee on Specialty Societies
Tuesday, October 14
12:15-1:15 p.m. | Hilton Riverside, Jasperwood
Committee on Standards and Practice Parameters
Monday, October 13
8:30-9:30 a.m. | Hilton Riverside, Elmwood
Committee on Surgical and Procedural Anesthesia
Saturday, October 11
8:30-10 a.m. | Hilton Riverside, Elmwood
Committee on Transplant Anesthesia
Monday, October 13
7-8 a.m. | Hilton Riverside, Norwich
Committee on Trauma and Emergency Preparedness
Monday, October 13
4-6 p.m. | Hilton Riverside, Trafalgar
Committee on Uniformed Services and Veterans’ Affairs
Saturday, October 11
2-4 p.m. | Hilton Riverside, Norwich
Committee on Young Physicians
Monday, October 13
9-10 a.m. | Hilton Riverside, Durham
Abstract Review and Educational Track Subcommittee Meetings
All abstract review and educational track subcommittee meetings
will be held at the Hilton New Orleans Riverside. Times, days and
locations are subject to change.
Abstract Review Subcommittee on Ambulatory and Geriatric
Anesthesia
Sunday, October 12
10-11 a.m. | Hilton Riverside, Rosedown
Abstract Review Subcommittee on Chronic and Cancer Pain
Sunday, October 12
3-4 p.m. | Hilton Riverside, Durham
Abstract Review Subcommittee on Critical Care
Saturday, October 11
4-5 p.m. | Hilton Riverside, Elmwood
Abstract Review Subcommittee on Equipment, Monitoring and
Engineering Technology
Saturday, October 11
3-4 p.m. | Hilton Riverside, Warwick
Abstract Review Subcommittee on Experimental Circulation
Sunday, October 12
9-10 a.m. | Hilton Riverside, Magnolia
Abstract Review Subcommittee on Outcomes and Database
Research
Tuesday, October 14
7-8 a.m. | Hilton Riverside, Durham
Abstract Review Subcommittee on Patient Safety
and Practice Management
Tuesday, October 14
8-9 a.m. | Hilton Riverside, Rosedown
Abstract Review Subcommittee on Pediatric Anesthesia
Monday, October 13
7-8 a.m. | Hilton Riverside, Elmwood
Abstract Review Subcommittee on Regional Anesthesia
and Acute Pain
Monday, October 13
8-9 a.m. | Hilton Riverside, Grand Salon C, Sec. 13 & 16
Abstract Review Subcommittee on Respiration
Sunday, October 12
8-9 a.m. | Hilton Riverside, Oak Alley
Educational Track Subcommittee on Ambulatory Anesthesia
Tuesday, October 14
1-2 p.m. | Hilton Riverside, Magnolia
Educational Track Subcommittee on Cardiac Anesthesia
Sunday, October 12
7-8 a.m. | Hilton Riverside, Norwich
Educational Track Subcommittee on Critical Care
Saturday, October 11
2-3 p.m. | Hilton Riverside, Rosedown
Educational Track Subcommittee on Fundamentals of
Anesthesiology
Monday, October 13
7-10 a.m. | Hilton Riverside, Magnolia
Educational Track Subcommittee on Neuroanesthesia
Saturday, October 11
8-9 a.m. | Hilton Riverside, Warwick
Educational Track Subcommittee on Obstetric Anesthesia
Tuesday, October 14
3-5 p.m. | Hilton Riverside, Magnolia
Educational Track Subcommittee on Pain Medicine
Sunday, October 12
12:30-1:30 p.m. | Hilton Riverside, Rosedown
Educational Track Subcommittee on Pediatric Anesthesia
Monday, October 13
7-8 a.m. | Hilton Riverside, Warwick
Educational Track Subcommittee on Professional Issues
Monday, October 13
1-2 p.m. | Hilton Riverside, Warwick
Educational Track Subcommittee on Regional Anesthesia
and Acute Pain
Monday, October 13
9-10 a.m. | Hilton Riverside, Warwick
Editorial Board Meetings
All editorial board meetings will be held at the Hilton New Orleans
Riverside. Times, days and locations are subject to change.
ASA GOVERNANCE PROGRAM
150
Anesthesiology Executive Editors Meeting
Sunday, October 12
8 a.m.-12 p.m. | Hilton Riverside, Trafalgar
Editorial Board for Anesthesia Patient Safety Program (APS)
Sunday, October 12
2-4 p.m. | Hilton Riverside, Warwick
Editorial Board for ANESTHESIOLOGY
Monday, October 13
3-6:30 p.m. | Hilton Riverside, Grand Salon A, Sec. 1-6
Editorial Board for the Self-Education and Evaluation Program (SEE)
Saturday, October 11
2-4 p.m. | Hilton Riverside, Magnolia
Editorial Board for Practice Performance Assessment and
Improvement Meeting
Saturday, October 11
4:30-6 p.m.
Hilton Riverside Hotel, Durham Room
Editorial Board for Simulation-Based Training (SEB)
Monday, October 13
5-7 p.m. | Hilton Riverside, Oak Alley
NETWORK

151
ASA GOVERNANCE PROGRAM
NOTES
152
NETWORK
Resident Activities
Friday, October 10
RM01 Residents and Medical Students Grassroots Seminar
7:30-9 p.m. | Hilton Riverside, Grand Salon A
Mark Bicket M.D.
Members will discuss the basics of the policy making process,
ways to inuence this process, and the value of civic engagement.
Jeffrey Plagenhoef M.D.
RM02 Resident and Medical Student Welcome Reception
9-11 p.m. | Hilton Riverside, Grand Salon B
Mark Bicket
Network and interact with fellow peers. Event is hosted by the ASA
Resident Governing Council.
Saturday, October 11
RM03 Models of Practice Panel
8-9:30 a.m. | Room R02-03
Roy Soto M.D.
The anesthesia employment landscape is changing rapidly.
Anesthesiologists can either be employed by a private group, a
larger local or national multispecialty organization, a hospital,
or even an investment rm. Understanding this landscape is an
important step in determining desired lifestyle, workload, and
income following graduation. During this panel discussion, we will
discuss these employment models with a focus on the positives
and negatives of each, as well as a discussion of national
employment trends and likely future models. Eric Mason M.D.,
Mark Norling M.D., Narendra Trivedi M.D.
RM04a Medical Student Workshop-Ochsner Health System
8-11 a.m. | Offsite
Mack Thomas M.D.
This workshop is offered to a limited number of students and
participation will be offsite. Details of the workshop are designed
and implemented by the host institution but will include an
introduction to the eld of anesthesiology, a variety of hands-on
workshops for students (airway management and intubation,
regional anesthesia, IV and arterial line placement, etc.),
and didactics. The goal is to provide increased exposure to
fundamental principles and some hands-on practice for medical
students interested in the eld of anesthesiology. Details will
follow after registration, please register for only one location.
RM04b Medical Student Workshop-Louisiana State University
8-11:00 a.m. | Offsite
Judy Johnson M.D.
This workshop is offered to a limited number of students and
participation will be offsite. Details of the workshop are designed
and implemented by the host institution but will include an
introduction to the eld of anesthesiology, a variety of hands-on
workshops for students (airway management and intubation,
regional anesthesia, IV and arterial line placement, etc.),
and didactics. The goal is to provide increased exposure to
fundamental principles and some hands-on practice for medical
students interested in the eld of anesthesiology. Details will
follow after registration, please register for only one location.
RM04c Medical Student Workshop-Tulane University
8-11 a.m. | Offsite
Lihua Zhang, M.D.
This workshop is offered to a limited number of students and
participation will be offsite. Details of the workshop are designed
and implemented by the host institution but will include an
introduction to the eld of anesthesiology, a variety of hands-on
workshops for students (airway management and intubation,
regional anesthesia, IV and arterial line placement, etc.),
and didactics. The goal is to provide increased exposure to
fundamental principles and some hands-on practice for medical
students interested in the eld of anesthesiology. Details will
follow after registration, please register for only one location.
RM05 Resident Written Board Prep
9:30-11 a.m. | Room R02-03
Sajid Shahul M.D
In this 90 minute seminar, the facilitators will briey review the
format of the written board certication examination and discuss
some of the concepts deemed to be challenging and difcult by
many residents. Frequently missed items (Keywords) from the
2014 in-training examination, divided into basic and advanced
topics by the ABA, will be used to anchor the discussions. The
facilitators will also share insight on study strategies, discuss
study resources available, and tips on test taking skills.
RM06 Subspecialty Panel
9:30-11 a.m. | Room R04-05
Walter Maurer M.D.
Ambulatory Anesthesia - What is New and Exciting for the Future?
• NORA (Non-Operating Room Anesthesia) – Show me the
money
• Monitored Anesthesia Care (MAC) as different from moderate/
deep sedation.
• How do anesthesiologists t into the burgeoning area of
sedation by non-anesthesiologists?
• Details of SEDAYS (rst commercial CAPS device) Ethicon
Endo-Surgery a division of Johnson & Johnson.
This session will also focus on the history of the subspecialty,
current and future state of the fellowship program, & clinical pearls
in Labor & Delivery suites.
Arthur Calimaran M.D.
Obstetric Anesthesia: Past, Present and Future
RM07 Practice Management I
1-2 p.m. | Room R02-03
Erica Stein M.D.
Transitioning from Residency to Practice
Presenting yourself in the best possible light on paper and in
person is sometimes easier said than done. Discussion will focus
not only on some of the common pitfalls, but also on some of the
details which will make you look like a star.
Lars Helgeson M.D.
Do’s and Don’ts on Your CV and During the Interview
RM08 Practice Management II
2-3 p.m. | Room R02-03
Judith Jurin Semo J.D., Esq.
Employment Contracts
This session will briey discuss a number of the terms,
organizations and concepts which will have a signicant impact on
how you practice and function on a day to day basis.
Arpana Ananth M.D.
Practice Management Keywords

153
RM09 Residency Program Meet and Greet
3:30-5:30 p.m. | La Nouvelle Ballroom C
Chad Greene
This event is the highlight of the Medical Student Component, and
has been benecial for all medical students (especially fourth year
medical students) applying to anesthesiology residency programs.
Program directors and residents showcase their respective
programs just before interview season.
Sunday, October 12
RM10 Resident Component House of Delegates
10 a.m.-12 p.m. | Room R02-03
Mark Bicket M.D.
Delegates must register between 9:30-10 a.m. before the HOD
meeting. In order to vote in Governing Council elections, you
must be credentialed rst. This session is open to all residents,
whether you are a delegate or not. During this meeting, we will
have the opportunity to hear from nationally known guests, and
we will present new and exciting ways for residents to get involved
politically on both local and national levels. We will also hold
elections for the 2014-15 ASA Resident Component Governing
Council, with results announced during this meeting. Awards
will also be given to residency programs who have reached
100-percent ASAPAC contributions.
RM11 Medical Student House of Delegates
10 a.m.-1 p.m. | Room R04-05
Chad Greene
Delegates must register between 9:30-10 a.m. before the HOD
meeting. In order to vote in Governing Council elections, you must
be credentialed rst. This session will include Delegate voting
on Medical Student Component Governing Council elections and
other relevant business. Educational topics include presentations
from current leaders in anesthesiology, advice for matching into
residency, research opportunities, and a Q & A session with
current residents. All medical students are invited to attend.
RM12 FAER Medical Student Anesthesia Research Fellowship
Symposium
2-5 p.m. | Room R08-09
Paloma Toledo M.D., M.P.H. Moderator
Annual Symposium showcasing the FAER-funded research projects
conducted by medical students in anesthesiology laboratories
across the nation. The Medical Student Anesthesia Research
Fellowship (MSARF) is a program FAER implemented to increase
the number of outstanding medical students, who want to pursue
academic careers in anesthesiology research. For a complete list
of program participants and meeting presenters, please visit the
FAER booth in the ASA Resource Center.
RM13 Resident Regional Anesthesia Workshop
2:30-5 p.m. | Room R06-07
Julia Pollock M.D.
This course will focus on the anatomy and sonoanatomy of upper
and lower extremity as well as truncal blocks commonly used in
the perioperative period.
• Ultrasound Guidance
• Brachial Plexus Blocks
• Lower-Extremity Blocks
• Paravertebral/TAPBlocks
• Lung Ultrasound
RESIDENTS & MEDICAL STUDENT COMPONENT
154
Registration
Full-service registration is located in Lobby A and D of the
Convention Center. Advance and on-site registration hours
at the center are as follows:
Registration hours
Friday, October 10 | 3-7 p.m.
Saturday, October 11-Tuesday, October 14 | 7 a.m.-5 p.m.
Wednesday, October 15 | 7 a.m.-12 p.m.
In addition, to the Convention Center, there are print-only badge
kiosks at two hotels on Friday, October 10, from 3-7 p.m. These
are located at the Hilton New Orleans Riverside, rst oor
registration counters across from the hotel gift shop and at the
New Orleans Marriott (Canal Street), second oor registration desk
outside La Galleries.
Speakers/presenters should pick up their badges in the
Presenter Ready Room, near the Julia Street Entrance off of
Lobby A of the Convention Center.
Registration Materials
All registration materials and name badges are provided at the
time of badge pick up. Registration materials will only be provided
at the convention center and not at the hotel registration areas.
ASA Tote Bags will be available for pick in the Resource Center
located in Exhibit Hall B1. Each attendee will be provided with a
ticket in their registration material to redeem one (1) tote bag.
Bag Pick-Up Areas: ASA Resource Center, Hall B-1,
October 10, 3 p.m. and October 11, 11 a.m.
Admission Requirements
(BADGES ARE REQUIRED)
Admission to non-ticketed activities (all available on a rst-come,
rst-served basis), including the Opening Session, Welcome
Reception, Panels, Special Lectures, Medically Challenging
Cases (MCCs) and Refresher Course Lectures (RCLs), Scientic
Abstracts and exhibits will be granted by the ANESTHESIOLOGY™
2014 annual meeting attendee badge only. Admission to ticketed
functions, including Problem-Based Learning Discussions (PBLDs),
Workshops, activities and special events will require both the
ANESTHESIOLOGY™ 2014 annual meeting attendee badge and a
ticket.
Tickets and Name Badges
All registrants for the ANESTHESIOLOGY™ 2014 annual meeting
will receive a name badge. Materials have not been mailed in
advance. Badges and tickets can be obtained at self-print kiosks
(pre-registrants only) or at the registration counters (all registrants)
during registration hours.
If you have pre-registered for the meeting, please visit the advance
registration desk or use the self-print registration kiosks to receive
your registration materials. Once registration materials have been
picked up, please visit an on-site registration desk to make any
changes or to register for additional courses.
Ticket Refunds/Exchanges
No refunds or exchanges are allowed after Monday, September 22.
If you purchase tickets at the meeting, please check them carefully
before you leave the ticket sales counter.
Ribbons
Members and individuals serving ASA and/or contributing to
the ANESTHESIOLOGY™ 2014 annual meeting program receive
ribbons recognizing their contribution and support. If you are one
of these individuals, thank you. You can pick up your ribbons at the
following locations.
Governance (HOD, Committee)
Ribbon counter at registration area
Convention Center, Lobby D
Presenters (all types)
Presenter Ready Room
Great Hall Lounge, South
Scientic and Educational Exhibitors
Exhibitor Registration Area
Convention Center, Lobby E
All Others
Ribbon counter in the registration area
Convention Center, Lobby D
ATTEND

155
General Information
ASA Information Services
Located in Lobby A and Lobby D, the ASA Information Services
areas should be able to assist with attendee needs or direct
attendees to the appropriate areas and services for assistance.
If you are away from the convention center and need to contact
ASA during registration hours, please call 504-670-6600. Within
the Convention Center, ASA maintains a helpline to meet any
attendee requests. This number will be posted in different area
throughout the Convention Center.
Business Services
Monday-Friday | 9 a.m.-5:30 p.m.
The UPS store is located in Lobby F in the Convention Center.
Phone: 504-670-8941 Fax: 504-670-8887.
Cell Phones and Pagers
Please turn off your pager or cellular telephone, or congure it
to silent operation. Cameras or cellular telephones with photo
capabilities may not be used.
Children at the Meeting
Children under 16 years of age will not be allowed into educational
sessions. If it is necessary for your children to accompany you
into the exhibit hall, please carefully supervise them for safety
reasons. This is the parents’ responsibility. Equipment and
accessories on display are valuable and can be hazardous to
children.
Daily News
Level 2, Room 240
Friday, October 10 | 12-5 p.m.
Saturday, October 11-Monday, October 13 | 8 a.m.-5 p.m.
Tuesday, October 14 | 8 a.m.-3 p.m.
Disclaimer
Materials and information presented during the
ANESTHESIOLOGY™ 2014 annual meeting represent the personal
viewpoint of the individual presenter and do not represent the
opinions, positions or viewpoints of ASA. By registering to attend
the ANESTHESIOLOGY™ 2014 annual meeting, attendees
acknowledge they are voluntarily participating in the ASA-
sponsored medical educational program and waive any right to
make any claim, including any claim for injury or damages, against
ASA for reliance on materials or information presented during the
ANESTHESIOLOGY™ 2014 annual meeting. ASA does not assume
any responsibility for any expenses incurred by registrants without
prior written authorization from ASA.
E-mail Stations
E-mail stations will be located in the International Connection
Lounge, Lobby A of the Convention Center Saturday, October
11-Wednesday, October 15.
Exhibitor Information Retrieval Program
Registrants for the ANESTHESIOLOGY™ 2014 annual meeting
except exhibitors and spouses/guests will be provided with an
encoded name badge. Exhibitors will use the encoded information
to record names, mailing addresses and email addresses (when
provided voluntarily) of registrants who wish to receive further
information.
Future ASA Meetings
October 24-28, 2015 | San Diego, CA
October 22-26, 2016 | Chicago, IL
October 21-25, 2017 | Boston, MA
October 13-17, 2018 | San Francisco, CA
October 19-23, 2019 | Orlando, FL
October 3-7, 2020 | Washington, D.C.
In Case of Emergency
It is important to stay calm when reporting an incident. MCCNO
has RED EMERGENCY PHONES conveniently located through the
facility. In order to expedite a response, a MCCNO Public Safety
Dispatcher is available 24 hours a day. The emergency number
504-582-3040 is the primary emergency number for the facility.
Please dial just 3040 from a MCCNO phone. The Dispatcher will
dispatch EMS, Ofcers, Event Managers, etc. PLEASE REFRAIN
FROM CALLING 911. The convention center is very large;
Facility and Public Safety personnel coordinate the movement of
emergency services to the scene. In addition to RED EMERGENCY
PHONES, and calling dispatch at 504-582-3040, Public Safety
Ofcers are available should you need assistance.
Lost and Found
Lost and found will be handled by the main registration area in
the Convention Center. Inquiries for lost or found items should be
directed to Registration Desk A in Lobby D.
Luggage/Bag Storage and Coat Check
Lobby B-2 of the Convention Center
Saturday, October 11 | 7 a.m.-5 p.m.
Sunday, October 12 | 8:30 a.m.-6:30 p.m.
Monday, October 13-Tuesday, October 14 | 8 a.m.-5 p.m.
Wednesday, October 15 | 8 a.m.-12 p.m.
Medical Services and First-Aid Ofces
Two locations will be made available in the Convention Center.
Lobby B-2 Medical Services and First-Aid Ofce.
Hours/Days of Operations:
Tuesday, October 7–Thursday, October 9 | 8 a.m.-5 p.m.
Friday, October 10 | 9 a.m.-7:30 p.m.
Saturday, October 11 | 6:30 a.m.-7 p.m.
Sunday, October 12–Tuesday, October 14 | 6:30 a.m.-5:30 p.m.
Wednesday, October 15 | 6:30 a.m.-1 p.m.
Lobby E – Medical Services and First Aid Ofce
Hours/Days of Operations:
Saturday, October 11 | 6:30 a.m.-7 p.m.
Sunday, October 12–Tuesday, October 14 | 6:30 a.m.-5:30 p.m.
No Smoking
Smoking is not permitted in the Convention Center or any room
or area in which ASA-sponsored or organized activities are held.
This prohibition includes the registration area, the exhibit hall and
meeting rooms.
GENERAL INFORMATION
156
Photography/Videotaping Policies
No photography, videotaping or audio taping is permitted in the
scientic sessions, instructional courses, exhibit hall or committee
meetings.
Presenter Ready Room
Friday, October 10 | 3-7 p.m.
Saturday, October 11-Tuesday, October 14 | 7 a.m.-5 p.m.
Wednesday, October 15 | 7 a.m.-12 p.m.
The Presenter Ready Room is designated as the location for
ASA presenters to preview and upload or get help modifying
their presentations. Presenters are required to check in at the
Presenter Ready Room. Technical support personnel skilled with
Apple computers, PCs, and Keynote software will be available
to offer assistance and answer questions. Any presenter using
their own Apple computer or using Keynote software should
notify an ASA staff person or technical support personnel as
early as possible so that we are prepared to accommodate your
presentation. To reach the Presenter Ready Room by phone, dial
(504) 670-6601 in the Morial Convention Center.
Press Room
Level 2, Room 224
Friday, October 10 | 12-5 p.m.
Saturday, October 11-Monday, October 13 | 8 a.m.-5 p.m.
Tuesday, October 14 | 8 a.m.-3 p.m.
Should you need to call the Press Room, please dial
504-670-6602 within the Convention Center.
San Diego Booth
The ANESTHESIOLOGY™ 2015 annual meeting will take place on
October 24-28, 2015 at the San Diego Convention Center in San
Diego. Representatives from the San Diego Convention Bureau
will be available on site in New Orleans in Lobby B1 to answer any
questions you may have about the city, attractions, hotels or the
convention center.
Session and Product Locators
Stations will be located in Lobby D near registration at the
Convention Center. Attendees will be able to search sessions, nd
room locations of all ASA events as well as search for particular
exhibitor products and which companies are providing products on
the exhibit hall oor.
SmartTots
The International Anesthesia Research Society (IARS) presents
SmartTots, a collaborative research initiative designed
to investigate, fund and ensure the safety of anesthetics
administered to neonates and young children. Visit our booth
located in Lobby B-1 for more information about anesthetic-
induced neurotoxicity, ongoing research projects and how you can
contribute to the effort.
Special Needs Statement
ASA is committed to making its activities accessible to all
individuals. If you are in need of an accommodation, please do
not hesitate to call and/or submit a description of your needs in
writing in order to receive service.
WiFi
Complimentary WiFi will be provided and is available throughout
all common areas, meeting rooms and specic areas within the
Connection Center/Exhibit Hall in the Convention Center.
Worship
There are many places of worship located near the Convention
Center and the nearby hotel community. Check with your hotel
concierge for complete listing locations and times of service.
Transportation
Concierge Airport Transportation
One World Transport is the ofcial concierge transportation
service for the ANESTHESIOLOGY™ 2014 annual meeting. The
transport service will provide comfortable town car or limousine
transportation options from Louis Armstrong International Airport,
allowing you to relax before you arrive at your hotel destination.
To reserve your car transport, contact One World Transport at
reservations@oneworldtransport.com to place your reservation.
Hotel Shuttle Bus
With the exception of the ASA headquarter hotel (Hilton New
Orleans Riverside) and any other hotels within immediate walking
distance of the convention center, ASA will operate a shuttle bus
transportation program (Friday–Wednesday) from designated New
Orleans hotels within the 2014 ASA hotel/housing program.
View the shuttle bus schedule below.
New Orleans Public Transportation Options
The airport is located approximately 13 miles from the Ernest N.
Morial Convention Center
Ground Transportation from the Airport to the Convention Center by
Taxi
A taxi costs approximately $33 from the airport to the Central
Business District (CBD) for one or two persons and $14 (extra per
passenger) for three or more passengers.
Taxi ranks are located on the lower level, outside the baggage
claim area. Taxis accept credit cards
Ground Transportation from the Airport to the Convention Center by
Airport Shuttle
Shuttle service is available from the airport to the hotels in the
CBD for $20 (per person, one-way) or $38 (per person, round-trip).
Three bags per person. Call 1-(866) 596-2699 or (504) 522-3500
to make a reservation. Advance reservations are required 48
hours prior to travel for all ADA accessible transfers. Please call
in advance of your travel date for the specially-equipped shuttle
to be reserved. Ticket booths are located on the lower level in the
baggage claim area. Please visit www.airportshuttleneworleans.
com for more details or to make a reservation.
Ground Transportation from the Airport to New Orleans Central
Business District by Bus
The E2 - Airport Route provides service from the Louis Armstrong
New Orleans International Airport in Kenner, down Airline Drive into
New Orleans. During weekdays only, it provides service to the New
Orleans CBD. The airport bus stop is on the second level of the
airport, near the Delta counter, in the median (look for the sign and
bench).
The fare from the Louis Armstrong New Orleans International
Airport to New Orleans Central Business district is $2. There will
be a short walk to the convention center area
Please visit jeffersontransit.org/e2airport.php or call
(504) 818-1077 for more details
ATTEND

157
Airport Limousines
Airport Limousine is the ofcial limousine service for Louis
Armstrong New Orleans International Airport. Convenient kiosks
are located in the baggage claim area and no-hassle curbside
pickups are available. Rates begin at $58 for one or two
passengers. Please visit www.airportlimousineneworleans.com
or call (504) 305-2405 for more details
Rates
Sedans
1-2 Passengers - $58
3 Passengers - $68
*A $3 fuel charge will be added to the cost.
SUV
4 Passengers - $78
5 Passengers - $88
*A $3 fuel charge will be added to the cost.
Limo
6 Passengers - $98
7 Passengers - $108
8 Passengers - $118
*For each passenger over 8, is an additional
$10 per person
Special Needs Transportation
A dedicated toll free number has been provided and will be active
during event for all SPECIAL NEEDS TRANSPORTATION requests.
Handicapped accessible equipment will be provided during
scheduled and posted shuttle operation hours. Attendees can
book reservations for this service by simply calling the toll free
number (877) 899-0986 at least 20 minutes prior to requested
pick up time during posted Hotel Shuttle hours of operation.
Shuttle Program Routes
*Subject to change
SHUTTLE BUS PICK-UP/DROP-OFF - Morial Convention Center,
located on Convention Center Blvd.
ROUTE 1 (RED)
Hilton New Orleans Riverside
Westin New Orleans Canal Place
ROUTE 2 (GREEN)
DoubleTree by Hilton Hotel New Orleans
Loews New Orleans Hotel
Renaissance New Orleans Arts Hotel
Residence Inn New Orleans Downtown
W New Orleans
Windsor Court
ROUTE 3 (ORANGE)
Courtyard New Orleans Downtown near the French Quarter
Hampton Inn & Suites Downtown/French Quarter
InterContinental New Orleans
JW Marriott New Orleans
New Orleans Marriott
Omni Royal Crescent Hotel
Sheraton New Orleans
ROUTE 4 (PURPLE)
Chateau LeMoyne French Quarter
Crowne Plaza New Orleans French Quarter
Hilton Garden Inn New Orleans French Quarter/CBD
Hotel Monteleone
Hyatt French Quarter
Renaissance New Orleans Pere Marquette Hotel
Ritz-Carlton New Orleans
Roosevelt New Orleans Hotel
Wyndham New Orleans French Quarter
ROUTE 5 (TAN)
Omni Royal Orleans
InterContinental San Francisco
Palace Hotel, A Luxury Collection Hotel
San Francisco Marriott Marquis
Westin San Francisco Market Street
WALKING HOTELS
Courtyard New Orleans Downtown Convention Center
Embassy Suites New Orleans Convention Center
Hampton Inn & Suites New Orleans Convention Center
Hilton Garden Inn New Orleans Convention Center
Hyatt Place New Orleans
New Orleans Downtown Marriott at the Convention Center
SpringHill Suites New Orleans Downtown
Wyndham Riverfront New Orleans
Shuttle Bus Operation Service Hours
Inbound Service FROM: Designated Hotels TO:
Convention Center every 15-20 mins
Friday, Oct. 10 --
Saturday, Oct. 11 6:30-10 a.m.
Sunday, Oct. 12* 6:30-10 a.m.
Monday, Oct. 13 6:30-10 a.m.
Tuesday, Oct. 14 6:30-10 a.m.
Wednesday, Oct. 15 7:00-10 a.m.
Midday Service FROM: Convention Center TO:
Designated Hotels every 30 mins
Friday, Oct. 10 2:30-7:30 p.m.
Saturday, Oct. 11 10 a.m.-3 p.m.
Sunday, Oct. 12* 10 a.m.-3 p.m.
Monday, Oct. 13 10 a.m.-3 p.m.
Tuesday, Oct. 14 10 a.m.-3 p.m.
Wednesday, Oct. 15 10 a.m.-1 p.m.
Outbound Service FROM: Convention Center TO:
Designated Hotels every 15-20 mins
Friday, Oct. 10 --
Saturday, Oct. 11 3-7 p.m.
Sunday, Oct. 12* 3-6 p.m.
Monday, Oct. 13 3-6 p.m.
Tuesday, Oct. 14 3-6 p.m.
GENERAL INFORMATION
158
Tour and Activity Assistance
Assistance with signing up on site or conrming tour/activities
previously arranged can be found at the tour desk in Lobby A of
the Convention Center, from Friday, October 10–Tuesday,
October 14. Tour buses/transportation will depart from the
Center’s Lobby A entrance.
Thursday, October 9
10:30 a.m.-2:30 p.m.
New Orleans Cooking Experience | $315
Friday, October 10
9 a.m.-5 p.m.
Bonjour from Louisiana | $154 Adult/$133 Child
11 a.m.-2 p.m.
Crescent City Cocktails/Lunch | $126
7 a.m. - 11 p.m.
Jazz Tour/Dinner | $230
Saturday, October 11
10:30 a.m.-2:30 p.m.
New Orleans Cooking Experience | $315
9 a.m.-1 p.m.
Creole Promenade/Snack | $35
10:30 a.m.-2 p.m.
Steamboat Natchez/Buffet | $112 Adult/$93 Child
9 a.m.-1:30 p.m.
Airboat Adventures/Lunch | $140 Adult/$132 Child
Sunday, October 12
10 a.m.-2 p.m.
Audubon Zoo | $ 89 Adult/$83 Child
9:30 a.m.-1:30 p.m.
Cajun & Creole Hands on Cooking | $183
8:15 a.m. - 3:30 p.m.
Plantation Lifestyles/Lunch | $148
5:15 p.m. - 10:30 p.m.
Broadway in the Big Easy/Dinner | $358
Monday, October 13
10 a.m.-1:30 p.m.
Cemetery Tour/Lunch | $125 Adult/$105 Child
9:30 a.m.-1 p.m.
Cajun & Creole Cuisine Demo | $75
9:30 a.m.-3:30 p.m.
Shopping on Magazine Street/Lunch | $173
6:30-11:30 p.m.
Sunset in the Swamplands/Dinner | $325
Tuesday, October 14
8:15 a.m.-3:30 p.m.
Plantation Lifestyles/Lunch | $148
9 a.m.-12 p.m.
Forever New Orleans | $58
9 a.m.-12:30 p.m.
Mysteries of Louisiana Swamplands | $68
9 a.m.-2 p.m.
National WWII Museum/Lunch | $185
10 a.m.-3 p.m.
Grand Dames/Garden District/Lunch | $205
1-3 p.m.
Mardi Gras Behind the Mask/Snack | $90
Wednesday, October 15
9:30 a.m.-3:30 p.m.
Shopping on Magazine Street/Lunch | $173
10:30 a.m.-2 p.m.
Steamboat Natchez/Buffet | $112 Adult/$93 Child
1:30-4:30 p.m.
Cajun & Creole Cuisine Demo | $75
Thursday, October 16
9 a.m.-5 p.m.
Au Revoir from Louisiana/Buffet | $154 Adult/$133 Child
12-5 p.m.
Cajun Exploration/Lunch | $317
Tours that do not meet minimum attendance requirements
may be canceled. If this happens, you will be contacted to
select a new tour or get a refund.
ATTEND

159
GENERAL INFORMATION
NOTES

160
Covidien
#1128
Surgical
Information
Systems
#529
Mindray
#1117
BD
703
Connection Lounges
Masimo
#829
Product Theater
ASA Resource Center
e-Posters
Medically Challenging Cases
Hospira
#621
CONNECTION CENTER/EXHIBIT HALL

161
Scientic & Educational
Exhibits
Connection Lounges
Teleex
#1619
Edwards
Lifesciences
#1307
Baxter
#1701
PharMEDium
#1801
Product & Tech-
nology
EXPERIENCE
New
Product-
Showcase
ASA Bistro
AcelRx
#2129
Optum
#1821
TEAM
Health
#2015
Cheetah
#1915
Merck
#2310
Industry Supporters
Annual Meeting
Supporters
CONNECTION CENTER/EXHIBIT HALL

162
CONVENTION CENTER/EXHIBIT HALL
Great Hall A-D: Opening Session,
Rovenstine Lecture, Severinghaus
Lecture, ASA/APSF Pierce lecture,
APSF Workshop, International Panels,
Celebration of Research, FAER
Sessions
Hall B1: ASA Resource Center,
e-Posters, Medically Challenging
Cases, e-Poster on Demand
Connection Center: Exhibits, Scientic
& Educational Exhibits, ASA Bistro,
ASA Subspecialty Pavilion, Product &
Technology EXPERIENCE, Connection
Lounges, Product Theater

163
CONVENTION CENTER/EXHIBIT HALL
International Connection Lounge,
Presenter Ready Room, Refresher
Course Lecture Download Station
Refresher Course Lectures
Registration, e-Poster on Demand
Station, ASA Info Counter, Refresher
Course Lecture Download Stations
Shuttle Bus Drop Off
Rivergate Room: Refresher
Course Lecture

164
Rooms: R02-R09
Resident & Medical Student Programs
& La Nouvelle Ballroom
Panels
Subspecialty Panels
Clinical Forum
Point Counter Point Oral Presentations,
Poster Discussions
Refresher Course Lectures
CONVENTION CENTER/LEVEL 2

165
CONVENTION CENTER/LEVEL 2
Refresher Course Lectures
WLM Events Cadaver Workshops, Workshops

166
PBLDs
Workshops
CONVENTION CENTER/LEVEL 3

167
HOTEL MAP
1. Crowne Plaza New Orleans French Quarter
2. Chateau LeMoyne French Quarter
3. Courtyard New Orleans Downtown Near
4. Courtyard New Orleans Downtown
5. DoubleTree by Hilton Hotel New Orleans
6. Embassy Suites New Orleans Convention
7. Hampton Inn & Suites Downtown/French
8. Hampton Inn & Suites New Orleans
9. Hilton Garden Inn New Orleans Conven
10. Hilton Garden Inn New Orleans French
11. Hilton New Orleans Riverside (HQ)
12. Hotel Monteleone
13. Hyatt French Quarter
14. Hyatt Place New Orleans
15. InterContinental New Orleans
16. JW Marriott New Orleans
17. Loews New Orleans Hotel
18. New Orleans Downtown Marriott at the
Convention Center
19. New Orleans Marriott
20. Omni Royal Crescent Hotel
21. Omni Royal Orleans
22. Renaissance New Orleans Arts Hotel
23. Renaissance New Orleans Pere Marquette Hotel
24. Residence Inn New Orleans Downtown
25. The Roosevelt New Orleans Hotel
26. Sheraton New Orleans
27. SpringHill Suites New Orleans Downtown
28. Ritz-Carlton, New Orleans
29. W New Orleans
30. Windsor Court Hotel
31. Westin New Orleans Canal Place
32. Wyndham New Orleans French Quarter
33. Wyndham Riverfront New Orleans
170
From
EXIT 236A
Esplanade
From
EXIT 235B
Canal St
St. Peter St
Marais St
Treme St
Treme St
Crozat St
N. Villere St
N. Villere St
N. Robertson St
Cleveland St
La Salle St
La Salle St
La Salle St
Claiborne Av
Freret St
S. Rober tson St
Clara St
S. Liberty St
S. Saratoga St
Gravier St
Sugar Bowl Dr
N. Claiborne Av
S. Claiborne Av
Girod St
Julia St
Clio St
Clio St
Calliope St
Erato St
Erato St
Thalia St
Melpomene St
N. Claiborne Av
Iberville St
Conti St
N. Roman St
N. Robertson St
N. Villere St
Marais St
Treme St
St. Claude St
Governor Nicholls St
Dumaine St
Chartres St
Royal St
Exchange Alley
Dorsiere St
Bourbon St
Dauphine St
Burgundy St
French Market Pl
Barracks St
Kerlerec St
Laharpe St
Columbus St
St. Bernard Av
Ursulines Av
St. Philip St
Dumaine St
St. Ann St
Orleans Av
Wilkinson
Toulouse St
St. Louis St
Bienville St
St. Ann St
St. Peter St
St. Philip St
Ursulines Av
S. Roman St
S. Rampart St
S. Rampart St
O’Keefe St
O’Keefe St
University Pl
Baronne St
Baronne St
Penn St
Carroll St
St. Joseph St
St. Joseph St
Poeyfarre St
To C r escent City Con ne ct io n B r i d g e ( Toll Bridge)
Andrew Higgins Dr
Julia St
Girod St
Lafayette St
Perdido St
Union St
Gravier St
Gravier St
Lafayette St
Girod St
N. Maestri
S. Maestri
Capdeville
Julia St
Notre Dame St
Carondelet St
Carondelet St
Church St
Constance St
Carondelet St
Prytania St
N. Diamond St
Gaiennie St
Calliope St
Baronne St
B
a
c
o
n
P
l
S. Peters St
S. Peters St
N. Peters St
N. Clay St
N. Front St
Fulton St
Commerce St
Poe St
Triangle St
Constance St
Front St
Camp St
Camp St
Natchez St
Barracks St
Kerlerec St
Dauphine St
Royal St
Char tres St
Decatur St
N. Peters St
Frenchmen St
Marigny St
Mandeville St
Spain St
Franklin Av
Port St
Press St
Clovet St
Montegut St
St. Ferdinand St
St. Roch Av
Elysian Fields Av
Burgundy St
N. Rampart St
St. Claude St
McShane Pl
Marais St
Urquhart St
N. Villere St
N. Rober tson St
Annette St
St. Anthony St
Pauger St
Touro St
L
a
tt
e
Av
Patterson St
Delaronde St
Pelican Av
Pelican Av
Alix St
Eliza St
Eliza St
Evel
ina St
Nunez St
Opelousas Av
Slidell St
Homer St
Brookly
n St
Powder St
Seguin St
Bermuda St
La Vergne St
Oliver St
Valette St
Bellville St
Elmira St
Pirate’s
P. Antoines
Annunciation St
Thalia St.
Martin Luther King Jr.
Terpsichore St.
Euterpe St.
Polymnia St.
Felicity St.
Constance St
Terpsicchore St
Euterpe St
Race St
Orange St
Richard St
St. Mary’s St.
St. Andrews St.
St. Andrews St.
Josephine St.
Felicity St.
N. Claiborne Av
N. Claibor ne Av
N. Claiborne Av
N. Claiborne Av
St. Thomas St
S. Rampart St
S. Saratoga St
Liberty St
S. Robertson St
Magnolia St
Clara St
Willow St
LaSalle St
Freret St
Coliseum St
G
ove
rn
o
r
N
i
c
h
o
l
l
s
S
t
Camp St
S. Diamond St
Clinton St
Madison
St
John Churchill Chase
Palmyra St
Iberville St
Conti St
Bienville St
St. Louis St
Latte Av
Dumaine St
St. Philip St
Ursulines Av
Gov. Nicholls St
B
a
y
o
u
R
d
N. Derbigny St
S. Derbigny St
Orleans Av
Henderson St
Newton St
Pacic Ave
Atlantic Ave
Evelina St
Dianan St
Decatur St
Common St
Magazine St
Tchoupitoulas St
Tchoupitoulas St
Convention Center Bl
St. Charles Av
N. Peters St
Morgan St
Bouny St
Patterson St
Verret St
Magazine St
Jackson Ave.
St. Charles Av
Dryades St
Simon Bolivar Ave.
Howard Av
Canal St
Poydras St
Loyola Av
Poydras St
Esplanade Av
N. Ra
mpart St
Elk Pl
Basin St
Canal St
Tulane Av
O
r
l
e
a
n
s
A
v
Esplanade Av
P
o
n
t
c
h
a
r
t
r
a
i
n
E
x
p
w
y
P
o
n
t
c
h
a
r
t
r
a
i
n
E
x
p
w
y
Crescent City Connection
Greater New Orleans Br.
10 10
90
BUS
90
BUS
90
BUS
90
90
MOON WALK
JA
CKSO
N
SQUA
RE
FRENCH
QUARTER
POLICE STATION
VISITOR
INFORMATION
CENTER
ST. LO
UIS
CA
THEDRAL
RIVERWALK
ST. LOUIS
CEMETERY
NO. 1
LOUIS
ARMSTRONG
PARK
WASHINGTON
SQUARE
ST. LOUIS
CEMETERY NO. 2
CANAL
PLACE
LAFAYETTE
SQUARE
JACKSON
BREWERY
GALLIER
HALL
CITY HALL
UNION
STATION
U.S. POST OFFICE
NEW ORLEANS ERNEST N. MORIAL
CONVENTION CENTER
SPANISH PLAZA
WOLDENBERG
RIVERFRONT PARK
RIVERBOAT
DOCKS
RIVERBOAT
DOCKS
AQUARIUM
OF THE AMERICAS
CANAL ST. FERRY
Free Pedestrians: Toll for Vehicles
LEE CIRCLE
CONTEMPORARY
ARTS CENTER
NATIONAL
WORLD WAR II
MUSEUM
Vieux Carré
French
Market
CRUISE SHIP
TERMINAL
HARRAH'S
NEW ORLEANS
CASINO
WORLD
TRADE
CENTER
IMAX THEATRE
NEW ORLEANS
ARENA
MERCEDES-BENZ
SUPERDOME
OGDEN MUSEUM
OF SOUTHERN
ART
LOUISIANA
CHILDREN’S
MUSEUM
LOUISIANA
STATE MUSEUM
U.S.
Mint
POLICE
STATION
BASIN ST. STATION
TOURIST INFO CENTER
STATE
COURTHOUSE
MARDI GRAS
WORLD
FRENCH QUARTER
TREME
FAUBOURG
MARIGNY
ALGIERS
CBD
CENTRAL BUSINESS DISTRICT
WAREHOUSE/ARTS
DISTRICT
GARDEN DISTRICT
(STARTS AT JACKSON AVE.)
M
ississippi River
200
1000
1200
1300
1400
1500
1600
200
300
400
600
800
300
400
500
600
700
800
900
1000
1100
1200
1300
800
700
600
500
900
100
700
500
1400
1100
33
29
30
31
28
27
26
25
23
24
22
21
20
19
18
17
16
15
14
13
32
11
10
9
12
8
7
2
6
5
3
4
1
1. Astor Crowne Plaza French Quarter
2. Chateau LeMoyne French Quarter
3. Courtyrd Downtown Near the French Quarter
4. Courtyard Downtown/Convention Center
5. DoubleTree by Hilton
6. Embassy Suites Convention Center
7. Hampton Inn & Suites Downtown/French Quarter
8. Hampton Inn & Suites Convention Center
9. Hilton Garden Inn Convention Center
10. Hilton Garden Inn French Quarter/CBD
11. Hilton Riverside - HQ Hotel
12. Hotel Monteleone
13. Hyatt French Quarter
14. Hyatt Place Convention Center
15. InterContinental Hotel
16. JW Marriott
17. Loews Hotel
18. New Orleans Downtown Marriott at the
Convention Center
19. New Orleans Marriott
20. Omni Royal Crescent
21. Omni Royal Orleans
22. Renaissance Arts Hotel
23. Renaissance Pere Marquette
24. Residence Inn Downtown
25. Roosevelt Hotel
26. Sheraton Hotel
27. SpringHill Suites Downtown
28. The Ritz-Carlton
29. W New Hotel
30. Windsor Court
31. Westin Canal Place
32. Wyndham French Quarter
33. Wyndham Riverfront Hotel
11
Convention
Center

168
House of Delegates, Grand Ballroom
Reference Committee Meetings
Regional Caucus Meetings
HILTON NEW ORLEANS RIVERSIDE/LEVEL 1

169
HILTON NEW ORLEANS RIVERSIDE/LEVEL 2
Governance Staff Support Ofce
Speaker of the House Ofce

170
State Caucus Meetings
Committee Meetings
HILTON NEW ORLEANS RIVERSIDE/LEVEL 3
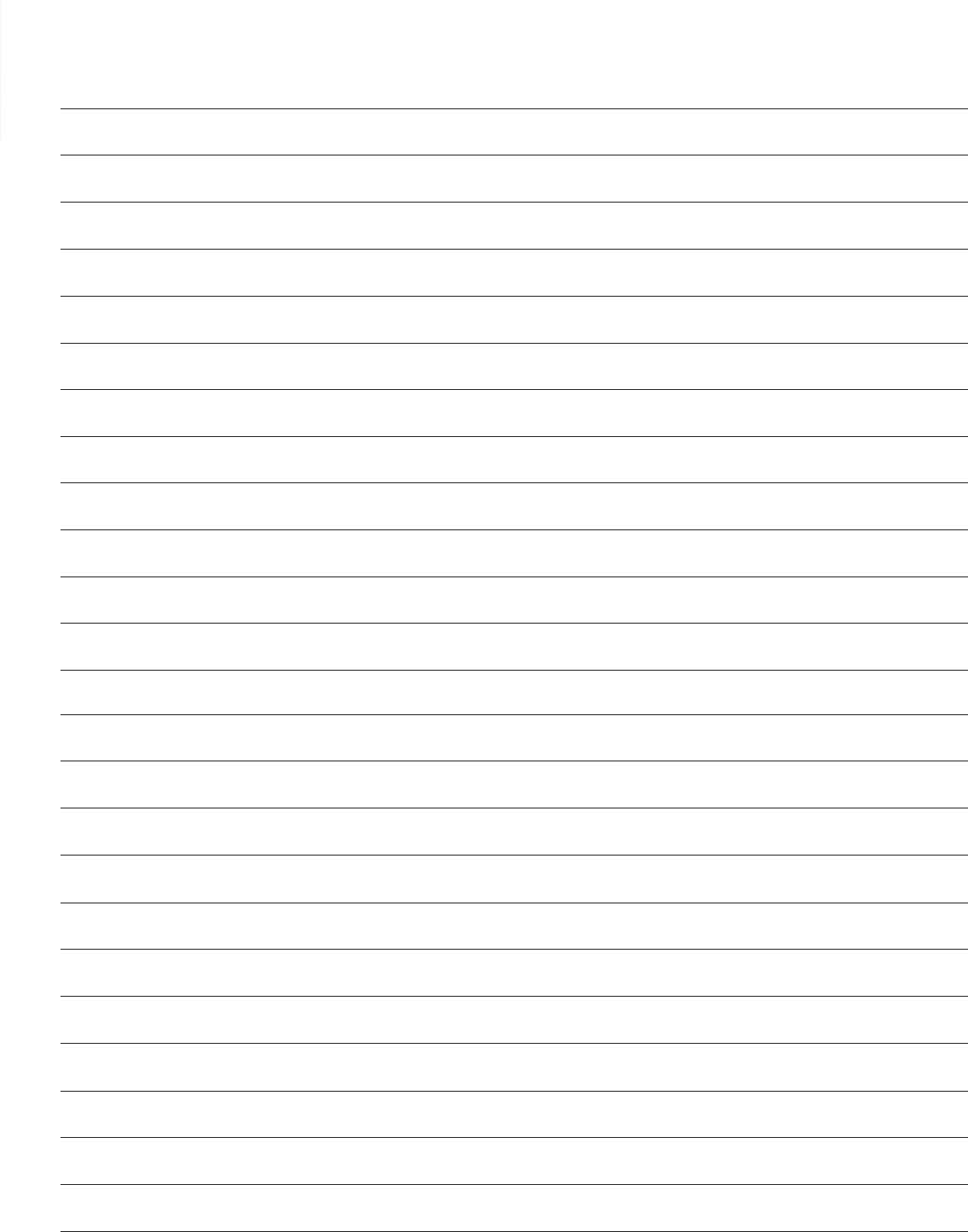
171
NOTES

172
The following planners have disclosed that they have financial relationships with commercial interests:
Asokumar Buvanendran
Funded Research - Pzifer, Cumberland; Consulting Fees - Medtronics, Kimberly Clark
James Eisenach
Consulting Fees - Adynxx
Girish Joshi
Honoraria - Pfizer, Baxter, Pacira, Cadence, Mylan
Dean Connors
Michael O’Connor
Karen Domino
Brenda Gentz
Audree Bendo
Saundra Curry
Randall Flick
Joy Hawkins
David Hepner
Terese Horlocker
Avery Tung
Lawrence Tsen
Sulpicio Soriano
Meg Rosenblatt
Scott Reeves
Mary Dale Peterson
Beverly Philip
James Abernathy
Funded Research -
Pharmedium
Anthony Absalom
Funded Research -
Unrestricted research grant
from Carefusion Inc.
John Allyn
Ownership - Spectrum
Medical Group (markets a QA
product, FIDES
Aparna Ananth
Honoraria - Physicians
Insurance - Board of
Directors
Dean Andropoulos
Royalties - Textbook Editor;
Funded Research - Hospira,
NIH
J. Ansermino
Equity Position - LGT Medical;
Funded Research - Draeger
Medical, Covidien; Consulting
Fees - GE Medical
Gregory Applegate
Honoraria - University of
Buffalo
George Arndt
Ownership - WMI; Royalties
- WMI; Consulting Fees -
Cook Inc.; Honoraria - Cook,
Inc. , NWAS
Solomon Aronson
Consulting Fees - The
Medicines Company
David Auyong
Honoraria - Kimberly Clark
Corporation, SonoSite
Rafi Avitsian
Funded Research - Hospira
Inc.; Consulting Fees - Parker
Hannifin Inc.
James Benonis
Honoraria - I Flow / Kimberly
Clark
Charles Berde
Consulting Fees - CVS -
consulting around safe opioid
prescribing, Cubist -
consulting around opioid
antagonists in children
Lauren Berkow
Consulting Fees - Masimo,
Teleflex, Medtronic, Ambu;
Honoraria - Masimo
Corporation, Teleflex Medical,
Medtronic Xomed
Patrick Birmingham
Funded Research - Cadence
Pharmaceuticals
James Blum
Funded Research - Retia
Medical, NIH; Consulting
Fees - Retia Medical
Ansgar Brambrink
Funded Research - as a
co-investigator; investigator
initiated multicenter trial;
Karl Storz America
Emery Brown
Funded Research - Masimo
Sorin Brull; Consulting Fees -
Merck
Marek Brzezinski
Honoraria - Grifols Inc.
Alexander Butwick
Funded Research - Masimo;
Other Material Support -
Haemonetics Corp.
Maxime Cannesson
Funded Research - Masimo
Corp, Edwards Lifesciences;
Consulting Fees - Gauss
Surgical, Masimo Corp,
Edwards Lifesciences
Brendan Carvalho
Funded Research - Pacira;
Consulting Fees - Smith
Medical
Davide Cattano
Other Material Support
- Haemonetic Inc provided
research supply for TEG-PM
Vincent Chan
Other Material Support - BK
Medical, Philips, SonoSite,
Ultrasonix
Jianguo Cheng
Salary - Cleveland Clinic;
Funded Research -
Department of Defense
Research Grant
Srinivas Chiravuri
Consulting Fees - St. Jude
Medical
Franklyn Cladis
Royalties - Textbook Editor
Steven Clendenen
Honoraria - Cadence, Pacira
Edmond Cohen
Honoraria - Speaking
Honoraria from Cook Critical
Care; Other Material Support
- Cook Critical Care
Deborah Culley
Honoraria - American Board
of Anesthesiology
William Culp
Ownership - Patent rights on
fire safety device
Andrew Davidson
Consulting Fees - $500
consulting for Matsui
Pharmaceuticals Oct 2013
The following planners have disclosed that they have no financial relationships with commercial interests:
The following contributors for ANESTHESIOLOGY™ 2014 have reported financial relationships with commercial interests:

173
Miles Day
Royalties - Epimed International
Stefan De Hert
Honoraria - Abbvie and Baxter
Philip Deveraeaux
Funded Research - Abbott Diagnostics,
Astra Zeneca, Bayer, Boehringer
Ingelheim, Bristol-Myers Squibb,
Covidien, Philips Healthcare, Stryker,
Roche Diagnostics
Peter Dunbar
Salary - Talaria, Inc.; Ownership - Talaria,
Inc.; Equity Position - Talaria, Inc.
Maxim Eckmann
Other Material Support - Medtronic
and Boston Scientific Pain Fellowship
Educational Grants, none of their
products featured in this workshop
John Ellis
Ownership - destinationCME LLC;
Honoraria - Baxter
Kristin Engelhard
Honoraria -Abbvie (Invited Talks),
Fresenius Kabi (Invited Talks)
Mark Ereth
Other Material Support - Cheetah
Developments
Lars Eriksson
Consulting Fees - Medical advisor to
Alteco Medical AB; Honoraria - Lecture
honoraria from Merck Inc and Abbvie AB
Ehab Farag
Funded Research - Hospira Company;
Honoraria - Hospira Company
Jeffrey Feldman
Consulting Fees - Covidien, Draeger
Medical Inc.
Alana Flexman
Funded Research - Hospira Inc.;
Honoraria - Hospira Inc.
Amy Forbis
Salary - Attorney and Director at BBL Law
Carlo Franco
Consulting Fees - B Braun
David Gaba
Royalties - Elsevier
Richard Galgon
Consulting Fees - CardioMed Device
Consultants LLC, Quintiles Consulting
Jorge Galvez
Funded Research - Microsoft
Tong Gan
Funded Research - Acacia, Cubist,
Fresenius, Pacira, Purdue, AcelRx,
Cheetah, Covidien, Deltex, Merck,
Premier; Consulting Fees - Baxter,
Edwards Life Science, Hospira, QRx;
Honoraria - Merck, Edwards, Fresenius,
Cadence, AcelRx
Adrian Gelb
Consulting Fees - Masimo Inc., Mylan
Inc.
Kathryn Glas
Royalties - LWW
Steven Greenberg
Honoraria - CASMED
Leanne Groban
Royalties - Elsevier-Editor
Michael Gropper
Funded Research - NIH, Gordon and
Betty Moore Foundation
Anita Gupta
Funded Research - PHRI Foundation
research Grant, Cumberland, Millennium;
Consulting Fees - Depomed, Cadence
Admir Hadzic
Equity Position - Macosta Medical
USA; Funded Research - Glaxo Smith
Kline Industries, Pacira, Baxter;
Consulting Fees - Skypharma, GE,
SonoSite, Codman & Shrutleff Inc.,
Johnson and Johnson, Cadence, Pacira,
Bbraun Medical, Baxter
Katherine Hagan
No financial relationship with commercial
interest.
Carin Hagberg
Consulting Fees -Unpaid consultant
for Ambu A/S; Other Material Support
- Research: Ambu A/S, Cadence
Pharmaceuticals, Karl Storz Endoscopy,
King Systems
Raafat Hannallah
Honoraria - Baxter Healthcare
H. David Hardman
Funded Research - Pacira
Pharmaceuticals; Consulting Fees -
Resolute Medical, LLC. Medical advisory
board member
Salim Hayek
Stock Options - Neuros; Funded
Research - Boston Scientific, Medtronic;
Consulting Fees - Boston Scientific;
Honoraria - Boston Scientific
David Healy
Funded Research
Charles Hogue
Stock Options - Ornim Medical; Funded
Research - Covidien, Inc.; Consulting
Fees - Ornim Medical, Merck, CSL
Behring
Marc Huntoon
Funded Research -CNS Therapeutics
/Malinkrodt, St. Jude Medical, Medtronics
Jason Hwang
Ownership - PolkaDoc; Royalties - The
Innovator’s Prescription: A Disruptive
Solution for Health Care
Brian Ilfeld
Funded Research - FAER Grant and
NIH Career Development Grant,
Summit Medical, Teleflex Medical,
Baxter Healthcare, Pacira
Pharmaceuticals
Giorgio Ivani
Consulting Fees - GE
Matthias Jacob
Funded Research -unrestricted research
grant by GRIFOLS (basic experimental
research), unrestricted research grant by
Fresenius Kabi (clinical registry);
Consulting Fees - member of GRIFOLS
Albumin Advisory Board; Honoraria - B.
Braun, Fresenius Kabi, GRIFOLS,
Serumwerk Bernburg
Jonathan Jahr
Funded Research - PI on Phase 3a and
3b studies on sugammadex; Honoraria -
Speaker’s Bureau
Leslie Jameson
Honoraria - GE Medical advisory board,
Masimo Clinical Advisory Board
Zeev Kain
Funded Research - NIH; Honoraria -
Merck; Consulting Fees - Merck
Allan Klock
Other Material Support - unpaid scientific
advisory board member for Ambu
Corry Kucik
Salary - US Navy
Jonathan Leff
Consulting Fees - CasMed, HeartWeb;
Other Material Support - CasMed,
HeartWeb
Andrew Leibowitz
Salary - (Spouse) Merck and Novartis;
Equity Position - (Spouse) Merck and
Novartis; Stock Options - (Spouse) Merck
and Novartis; Consulting Fees - Elcam
Medical, Misc. Legal Firms
Adam Levine
Consulting Fees - Mylan Specialties;
Honoraria - Mylan Specialties
Wilton Levine
Royalties - Codonics, Inc, Western
Enterprises
Asa Lockhart
Ownership - Golden Caduceus
Consultants
Shobha Malviya
Funded Research - Cadence
Pharmaceuticals
Jonathan Mark
Royalties - I serve as Section Editor,
Cardiac Anesthesia for UpToDate (online
medical information). I have never been
paid yet, but I understand that in time, I
will receive royalties for my work.
Chawla LaToya Mason
Royalties - I have received royalty
payments from Lippincott Williams
Wilkins as a result of my serving as
Associate Editor for a textbook project
(Shnider & Levinson’s Anesthesia for
Obstetrics, 5th Edition).
Keira Mason
Funded Research - Hospira
Lynne Maxwell
Funded Research - Cadence
Pharmaceuticals; Consulting Fees -
Cubist Pharmaceuticals; Other Material
Support - Luitpold Pharmaceuticals
DISCLOSURES
174
C. Mazer
Funded Research - Boehringer-Ingelheim,
CSL Behring, Cubist, Medicines
Company, Fresenius-Kabi, Allocure;
Honoraria - Astra-Zeneca, Cubist,
Medicines Company, Fresenius - Kabi
David McDonagh
Consulting Fees - Cephalogics Corp. LLC
Joseph McIsaac
Salary - Integrated Anesthesia
Associates, Inc.; Ownership - Integrated
Anesthesia Associates, Inc., (Spouse)
Mountain Laural Biomedical, LLC;
Royalties - Elsevier Publishers
William McIvor
Funded Research - (10% salary) support
grant from the AHRQ as part of Matt
Weinger’s multi-center sim study
Nagy Mekhail
Funded Research - Kimberly Clark,
Bioness, & CNS Therapeutics; Consulting
Fees - Flowonix, Medtronic Spinal, &
Spinal Modulation
Alan Merry
Equity Position - Safer Sleep LLC
Rafael Miguel
Honoraria - Teva Pharmaceuticals,
Johnson and Johnson
Alexander Mittnacht
Honoraria - Abiomed, Casmed
Annette Mizuguchi
Ownership - (Spouse)
www.ptemasters.com
James Modir
Honoraria - Faculty for AAPMU
James Moore
Consulting Fees - Assisted colleagues
at Cedars Sinai with their implementation
of the anesthesia component of the
Epic electronic health record system.
Paid through the Encore HR human
resource organization.
Jan Mulier
Funded Research - MSD; Consulting Fees
- MedecBenelux, Abbvie, Orion
John Murkin
Stock Options - Ornim Medical
Glenn Murphy
Consulting Fees - Merck; Honoraria -
Merck
David Murray
Funded Research - Agency for Health
Quality and Research (AHRQ) 3/1/2010
2/28/2014, RO1 1R18HS022265-01,
Principal Investigator: Murray, David John
Michael Murray
Salary - Mayo Clinic
Kimmo Murto
Funded Research - Janssen
Pharmaceuticals
Antoun Nader
Funded Research - Pfizer
John Neeld
Consulting Fees - Mag Mutual Ins. Co
Dolores Njoku
Royalties - McGraw Hill Education
Nancy Nussmeier
Salary - Wolters Kluwer Health
Michael Oleyar
Ownership - Founder and CEO of Chartos,
Inc., a personal health records company
Vilma Ortiz
Royalties - Informa HealthCare
Einar Ottestad
Honoraria - Faculty for AAPMU
Pratik Pandharipande
Funded Research - Hospira Inc.;
Honoraria - Hospira Inc.
Philip Peng
Other Material Support - Equipment
support from SonoSite, Canada
Stanford Plavin
Honoraria - Speaker’s Bureau for Pacira,
Speaker’s Bureau for Eisai
David Provenzano
Consulting Fees - Kimberly-Clark, St.
Jude Medical, Medtronic Inc., Janssen
Pharmaceuticals; Honoraria - Cadence
Pharmaceuticals
Satya-Krishna Ramachandran
Consulting Fees - MERCK, Galleon
Pharmaceuticals
Chandra Ramamoorthy
Funded Research - Masimo Corporation
Maunak Rana
Stock Options - Medtronic; Funded
Research - St. Jude, Boston Scientific;
Honoraria - Neurotherm
James Rathmell
Consulting Fee- American Board of
Anesthesiology
Richard Rauck
Funded Research - Medtronic, Boston
Scientific, Jazz, Mallinkrodt, Spinal
Modulation; Consulting Fees - Jazz,
Boston Scientific, Mallinkrodt; Honoraria
- Boston Scientific, Jazz
Russell Roberson
Funded Research -The manufacturer of
IV iron, AMAG, has provided IV iron at
no cost and paid for iron labs (~$40375
of value) for a pilot study for which I’m a
co-investigator
William Rosenblatt
Consulting Fees - AMBU Corporation
Richard Rosenquist
Royalties - UpToDate Educational
Materials, (Spouse) UpToDate Section
Editor; Consulting Fees - EMMI Education
Material Development
Colin Royse
Ownership - Director of HeartWeb
Keith Ruskin
Consulting Fees - Masimo Corporation
Todd Sarge
Funded Research - NIH RO1 Grant
#1UM1HL108724-01A1; Honoraria -
Society of Critical Care Medicine -
speaker honoraria
John Schaefer
Ownership - Sim Tunes; Royalties -
Laerdal Medical
Daniel Sessler
Royalties - Sedasys, Ethicon Endo
Surgery; Funded Research - NIH,
Canadian Institues of Health Research,
Population Health Research Institute,
Drown Foundation, MERCK, 3M,
Covidien, Abbvie, Mölnlycke, 37
Company; Consulting Fees - 3M (donated
to charity), Carefusion (donated to
charity), Mölnlycke (dontaed to charity),
37 Company (donated to charity), Abbvie,
Merck
Aryeh Shander
Funded Research - CSL Behring,
Masimo, OPK Biotech, US Department
of Defense, ZymoGenetics Inc.;
Consulting Fees - American Regent,
AMAG Pharmaceuticals, Baxter, CSL
Behring, DARPA, Deerfield Institute,
Gauss Surgical, Masimo Corp., New
Jersey State District Attorey, Octapharma,
OPK Biotech, Zymogenetics
Hariharan Shankar
Honoraria - Dannemiller Foundation,
AAPMU.org; Other Material Support -
Philips, Sonosite, BK Medical
Stanton Shernan
Other Material Support -
e-echocardiography.com, Philips
Healthcare, Inc.
Douglas Shook
Honoraria - Edwards Lifesciences, Sorin
Group; Other Material Support - Philips
Healthcare, Inc., Sorin Group, Edwards
Lifesciences
Allan Simpao
Funded Research - Microsoft
Richard Smiley
Consulting Fees - InSite Medical
Technologies, Inc.
Roman Sniecinski
Funded Research - Covidien, LLP
Jose Soberon
Funded Research - Pacira Corporation
Michael Souter
Salary - Medical advisor with salary
support to University of Washington from
LIfeCenter Northwest, an OPO, and a
former National Medical Advisor to AOPO.
Stanley Stead
Salary - Stead Health Group
Francis Stellaccio
Honoraria - Airway World
Lena Sun
Funded Research - Smart Tots Research
Fund
Joshua Tobin
Honoraria - May Clinic Grand Rounds
Honorarium; Other Material Support
-Silicone Occlusive Dressing For
Penetrating Thoracic Trauma,
Cricothyrotomy Forceps
John Vargo
Consulting Fees - Cook Medical, Inc.
Boston Scientific, Inc., Olympus America,
Inc., Ethicon EndoSurgery

175
Albert Varon
Royalties - Cambridge University Press
Jeffery Vender
Consulting Fees - Pharmedium; Other
Material Support - Board of
Directors - Adeptus, Board of Directors-
Wirtz Corporation
Chandy Verghese
Honoraria - The LMA Company; Other
Material Support - The LMA Company
Marcos Vidal-Melo
Funded Research - investigator initiated
grants from NIH and Merck
Eugene Viscusi
Funded Research - AcelRx, Cumberland,
Pacira; Consulting Fees - AcelRx,
Cadence, Cubist, Salix, Pacira; Honoraria
- Cadence, Pacira, Cubist
Gary Walco
Consulting Fees - Purdue Pharma,
Janssen Pharmaceuticals
Benjamin Walker
Consulting Fees - (Spouse) ABC Medical
Education (Radiology CME)
Guy Weinberg
Ownership - Lipid Resuscitation, ResQ
Pharma, LLC
Jeanine Wiener-Kronish
Royalties - Critical Care Secrets (Editor),
UCSF/Medical College of Wisconsin;
Funded Research - NIH; Honoraria -
Duke, Columbia, University of Toronto,
UCSF, University of Wisconsin, Society of
Critical Care Medicine
George Williams
Funded Research- Teleflex, funded
research project analyzing waste
anesthetic gas levels in the post
anesthesia care unit
Kayode Williams
Funded Research - Named co
investigator in Medtronic sponsored SCS
study on mechanisms SCS in chronic
pain study-site Johns Hopkins School of
Medicine
Myron Yaster
Consulting Fees -Endo pharmaceuticals;
Purdue Pharmaceuticals; Astra Zeneca..I
have participated in funded research or
been on a DSMB
The following contributors for ANESTHESIOLOGY™ 2014 have reported no financial relationships with commercial interests:
Full Name
Jaime Aaronson
Kenneth Abbey
Basem Abdelmalak
Salahadin Abdi
Amr Abouleish
Ron Abrons
Gareth Ackland
Anoushka Afonso
Zulqar Ahmed
Kyle Ahn
Ozan Akca
Shamsuddin Akhtar
Wael Ali Sakr Esa
Inger Aliason
Rae Allain
Ellen Allinger
Ahmad Alomari
Aditee Ambardekar
Adam Amundson
Jennifer Anderson
T. Anderson
Maged Andrews
Moris Aner
Shane Angus
Magdalena Anitescu
Jeffrey Apfelbaum
Melinda Aquino
James Arens
Maged Argalious
Donald Arnold
Harendra Arora
Brett Arron
Radha Arunkumar
Rebecca Aslakson
Arthur Atchabahian
Joshua Atkins
Yianni Augoustides
Edwin Avery, IV
Michael Avram
Catherine Bachman
Douglas Bacon
Angela Bader
James Bagian
Michael Bailin
Keith Baker
Gabriele Baldini
Christine Ball
Arna Banerjee
Dalia Banks
Mathew Banks
Shawn Banks
DISCLOSURES
176
Carolyn Bannister
Paul Barash
Cristina Barboi
Julian Barker
Sheila Barnett
Michael Barrington
Karsten Bartels
Joseph Bayes
Hernan Bazan
Shawn Beaman
Scott Beattie
Richard Beers
Elizabeth Behringer
Yaakov (Jake) Beilin
Charlotte Bell
Anke Bellinger
Sadek Beloucif
Mohamed Ben Ammar
Esther Benedetti
Honorio Benzon
Keith Berge
Jeffrey Berger
William Berry
Tarun Bhalla
Sanjay Bhananker
Anuj Bhatia
Julian Bick
Mark Bicket
David Biel
Luca Bigatello
Daniel Biggs
Frederic Billings
Wendy BInstock
David Birnbach
Edward Bittner
Susan Black
Jocelyn Blake
Pamela Bland
Kimberly Blasius
Jeanna Blitz
Anne Boat
Sylvain Boet
Steven Boggs
Karen Boretsky
Alain Borgeat
Adrian Bosenberg
Zeljko Bosnjak
Michael Bottros
Gregory Botz
Arthur Boudreaux
M. Bould
Demetrios Bourdakos
Edwin Bowe
Patrick Boyle
William Bradford
MaryBeth Brady
Tara Brakke
Jess Brallier
Gary Brenner
Claire Brett
Jane Brock
David Broussard
Daniel Brown
Karen Brown
Ethan Bryson
Chester Buckenmaier
Brenda Bucklin
Amanda Burden
John Butterworth
Steven Butz
Michael Cahalan
Arthur Calimaran
Brian Cammarata
Kenneth Candido
Keith Candiotti
Christopher Canlas
Levon Capan
Louanne Carabini
Franco Carli
Ian Carroll
George Carter
Lawrence Caruso
Daniel Castillo
Maria Castillo
Matthew Chan
Rekha Chandrabose
Wei Chao
Debnath Chatterjee
Jacques Chelly
Peter Cheng
Meir Chernofsky
Albert Cheung
Joseph Chiang
May Chin
Hovig Chitilian
Christopher Choukalas
Jason Chua
Frances Chung
Robert Cima
David Clark
Jerry Clark
Randall Clark
Rebecca Claure
Ira Cohen
Jonathan Cohen
Neal Cohen
David Collard
Jeremy Collins
Nancy Collop
Cristopher Connor
Richard Cook
Jeffrey Cooper
Richard Cooper
Zara Cooper
Darin Correll
Elifce Cosar
Charles Cote
James Cottrell
Douglas Coursin
Charles Cowles
Robin Cox
Gregory Crosby
Miguel Cruz
Krista Curell
Thomas Cutter
Marcelo Cypel
Armagan Dagal
Robert D’Angelo
Christopher Darling
Anthony De La Cruz
Oscar De Leon-Casasola
Gildasio De Oliveira
Andre De Wolf
Matthew DeCamp
Timothy Deer
Giorgio Della Rocca
Christina DeLucca
Samuel DeMaria
Alicia Dennis
Ryan Derby
Mark Dershwitz
Meena Desai
Jayant Deshpande
Mark Deshur
Zachary Deutch
Nina Deutsch
Prabhakar Devavaram
James Di Nardo
Carol Ann Diachun
Christina Diaz
Geraldine Diaz
Laura Diaz
David Dickerson
Daniel Diedrich
Pierre Diemunsch
Stephen Dierdorf
John Dilger
Dawn Dillman
James DiNardo
Michelle Diu
Katherine Dobie
Jeffrey Dobyns
Thomas Dodds
John Dombrowski
Karen Domino
Melanie Donnelly
D. John Doyle
Larry Driver
Richard Driver
Elizabeth Drum
John Drummond
Richard Dsida
Stanlies D’Souza
Gerald Dubowitz
Roman Dudaryk
Amy Duhachek-Stapelman
Peggy Duke
Richard Dutton
Jane Easdown
Angela Edwards
David Edwards
Talmage Egan
Jesse Ehrenfeld
Jami Eidem
Sharon Einav
Andrew Eisenhauer
James Eisenkraft
Nabil Elkassabany
Herodotos Ellinas
Clint Elliott
Richard Elliott
Dalia Elmofty
Hesham Elsharkawy
Kelly Elterman
Charles Emala
Logan Emory
Jorg Ender
Ryan Endersby
Calvin Eng
Mitchell Engle
Scott Engwall
F. Kayser Enneking
Michael Erdek
Monique Espinosa
Adam Evans
Faye Evans
Lucinda Everett
Brenda Fahy
Ashraf Farag
Michaela Farber
Neil Farber
William Feaster
Ludwik Fedorko
Jessica Feinleib
David Feinstein
Marc Feldman
Ana Fernandez-Bustamante
Roshan Fernando
Massimo Ferrigno
David Ferson
John Fiadjoe
Matthew Fiegel
Larry Field
Patrick Filip
Daniela Filipescu
James Findlay
Perry Fine
Roderick Finlayson
Alan Finley
Paul Firth
Gregory Fischer
Quentin Fisher
Jane Fitch
Meghann Fitzgerald
Michael Fitzsimons
Peter Fleischut
Lee Fleisher
Lorraine Foley
Manuel Fontes
Amanda Fox
Regina Fragneto
Marcellene Franzen
Michael Frass
Gyorgy Frendl
Wallace Friedman
Elizabeth Frost
Giulio Frova
Thomas Fuchs-Buder
Natasha Funck
William Furman
Cory Furse
Emmanuel Futier
Andrea Gabrielli
Jeff Gadsden
Robert Gaiser
Jonathan Gal
Maria Galati
Eduardo Galeano
Samuel Galvagno
Marcelo Gama de Abreu
Charlene Gamaldo
Kishor Gandhi
Arjunan Ganesh
Michael Ganter
Leslie Garson
Steven Gayer
Sarah Gebauer
Simon Gelman

177
Theresa Gelzinis
Jessica George
Ronald George
Andrew Gettinger
Katherine Gil
Thomas Gildea
Richard Gillerman
Christopher Gilligan
Keith Gipson
Laurent Glance
Nancy Glass
Barbara Gold
Sara Goldhaber-Fiebert
Julian Goldman
Peter Goldstein
Robert Goldstein
Brenda Golianu
Jeffrey Gonzales
Cheryl Gooden
Stephanie Goodman
Ori Gottlieb
Vijaya Gottumukkala
Basavana Goudra
Robert Gould
Trusha Govindji
Stuart Grant
Roxana Grasu
Loreta Grecu
Matthew Green
Chad Greene
Katherine Grichnik
Thomas Grissom
Jonathan Griswold
Karina Gritsenko
Hilary Grocott
Jeffrey Gross
Wendy Gross
Carrie Guheen
George Guldan
Padma Gulur
Dhanesh Gupta
Allen Gustin
Jacob Gutsche
Dawit Haile
Thomas Halaszynski
Matthew Hallman
Hossam Hamda
Laura Hammel
William Hammonds
William Hand
Judith Handley
John Hanlon
Michael Hannaman
Alexander Hannenberg
Jason Hansen
Neil Hanson
Courtney Alan Hardy
Greg Hare
Priscilla Harrell
Anna Harris
Kyle Harrison
Thomas Harrison
Gregg Hartman
Stephen Harvey
Stephen Haskins
Afton Hassett
Marc Hassid
Gary Haynes
Stephen Hays
James Hebl
Paul Heerdt
Eugenie Heitmiller
Lars Helgeson
Laura Hemmer
Amy Henry
Andrew Herlich
Antonio Hernandez
Shannon Hersey
Douglas Hester
Eric Heyer
James Hicks
Michael Hicks
Laureen Hill
Kenneth Hiller
Paul Hilliard
Jonathan Ho
Juliann Hobbs
George Hoffman
Michael Hofkamp
Ingrid Hollinger
W. Michael Hooten
Harriet Hopf
Leila Hosseinian
Constance Houck
Grant Lindsay Hounsell
Steven Howard
Kimberly Howard-Quijano
David Hoyt
McCallum Hoyt
Robert Hsiung
Eric Hsu
Ling Qun Hu
Andrea Huang
Yuguang Huang
Anthony Hudetz
Julie Huffmyer
Elisabeth Hughes
Tessa Huncke
Orlando Hung
Agnes Hunyady
William Hurford
Muhammad Hussain
Michael Hutchens
Jaime Hyman
Pedro Ibarra
Fumito Ichinose
Barys Ihnatsenka
Eiichi Inada
Robert Isaak
Stacey Ishman
Yulia Ivashkov
Adam Jacob
Jeena Jacob
Jeffrey Jacobs
Eric Jacobsohn
Narasimhan Jagannathan
Uday Jain
Gregory Janelle
Joe Jansen
Christina Jeng
Aaron Joffe
Roger Johns
Daniel Johnson
Judy Johnson
Matthew Johnson
Rebecca Johnson
Dean Jones
Keith Jones
Raymond Joseph
Vilma Joseph
Marc Kahn
Cor Kalkman
Mihir Kamdar
Ihab Kamel
Ming-Chih Kao
Marshal Kaplan
Manoj Karmakar
Rami Karroum
Olga Kaslow
Tripti Kataria
Jonathan Katz
Brian Kavanagh
Donald Keeler
Henrik Kehlet
Richard Kelly
Max Kelz
Paul Kempen
Judy Kersten
Miklos Kertai
Sabry Khalil
Evan Kharasch
Yury Khelemsky
Sachin Kheterpal
Swapnil Khoche
Sean Kiley
Peter Killoran
Jinu Kim
Jung Kim
Soo Yeon Kim
Tae Kim
Tae-Wu Kim
Kyle Kirkham
Jerome Klafta
Andrew Klein
Norma Klein
Colleen Koch
Antoun Koht
Lavinia Kolarczyk
Michael Kopec
Sandra Kopp
Eugene Koshkin
Sabine Kost-Byerly
Thomas Kotsonis
Pete Kovatsis
Sibylle Kozek
Elliot Krane
Michael Kristensen
Robert Krohner
Cindy Ku
Catherine Kuhn
Priya Kumar
Anjana Kundu
Robert Lagasse
Yan Lai
Kirk Lalwani
Mary Landrigan-Ossar
Jason Lane
Beth Demers Lavelle
Gary Lawson-Boucher
Melissa Laxton
Allison Lee
Chanhung Lee
Lorri Lee
Mitchell Lee
Richard Lee
Se Won Lee
Tat Leang Lee
Lisa Leffert
Marc Leib
Mark Leibel
Daniel Leizman
Louis Lejarza
Imanuel Lerman
Joel Levey
Michelle Levey
Matthew Levin
Linda Le-Wendling
Michael Lewis
Galina Leyvi
Mei-Ying Liang
J. Lance Lichtor
Yuan-Chi Lin
Ian Lipski
Steven Lisco
Ronald Litman
Linda Liu
Spencer Liu
Andreas Loepke
Martin London
Lindsey Loveland-Baptist
Stephen Lucas
Tanya Lucas
Danielle Ludwin
Philip Lumb
Pastor Luna
Maria Lupa
Holly Lynch
Gerald Maccioli
David Mackey
Sean Mackey
David MacLeod
Aman Mahajan
Elizabeth Mahanna
Kamal Maheshwari
Mohamed Mahmoud
David Maine
Mazen Maktabi
Anuj Malhotra
Vinod Malhotra
Khalid Malik
Tariq Malik
David Mann
Bruno Marciniak
Alan Marco
Michael Margarson
Lynette Mark
Scott Markowitz
Erich Marks
Mitchell Marshall
Christine Martin
David Martin
Gavin Martin
Susan Martinelli
Vicente Martinez-Pons
Ricardo Martinez-Ruiz
George Mashour
Eric Mason
Linda Mason
DISCLOSURES
178
Adrian Matioc
Maria Matuszczak
Robina Matyal
Walter Maurer
Timothy Maus
Aubrey Maze
John McAllister
Mary Ellen McCann
Patrick McCarty
Craig McClain
Maureen McCunn
Timothy McDonald
Matthew McEvoy
Kathryn McGoldrick
Ali Mchaourab
Anne Marie McKenzie Brown
Kathryn McQueen
Kelly McQueen
Jason McVicar
Jannicke Mellin-Olsen
Estela Melman
Joseph Meltzer
Sharon Merrick
Alonso Mesa
Amy Mesa-Jonassen
David Metro
Julia Metzner
Jill Mhyre
Edward Michna
Brett Miles
Scott Miller
Steven Miller
Thomas Miller
Mohammed Minhaj
Leonid Minkovich
John Mitchell
Daria Moaveni
Vivek Moitra
Yue-Pang Mok
William Montgomery
Candice Montzingo
Richard Moon
Laurel Moore
Debra Morrison
Wayne Morriss
Thomas Mort
Loran Mounir Soliman
Danny Muehlschlegel
Michael Murphy
Ross Musumeci
Paul Myles
Ameet Nagpal
Ryan Nagy
Samer Narouze
Robert Naruse
Muhaammed Nasir
Joseph Neal
Nicholas Nedeff
Jacques Neelankavil
Vladimir Nekhendzy
Patrick Neligan
Eric Nelson
Kenneth Nelson
Edward Nemergut
Mark Neuman
Steven Neustein
Alina Nicoara
James North
Mark Nunnally
Michael Nurok
Sydney Nykiel
Charles Nyman
Colleen O’Leary
Howard Odom
Mooyeon Oh-Park
Colleen O’Leary
Susan O’Leary
Patrick Olomu
Olutoyin Olutoye
Irene Osborn
James Osorio
Kristie Osteen
Ellen O’Sullivan
Medge Owen
William Paganelli
Sheela Pai
Arvind Palanisamy
Jason Panchamia
Oliver Panzer
Christine Park
Brian Parker
Anil Patel
Piyush Patel
Vikram Patel
Minda Patt
Kenneth Pauker
Veronica Payne
Bridget Pearce
Ronald Pearl
Paolo Pelosi
Susan Penney
Anahi Perlas
Misha Perouansky
Albert Perrino
Tjorvi Perry
Gene Peterson
Cathleen Peterson-Layne
James Philip
Mark Phillips
May Pian-Smith
Paul Picton
Carlos Pino
Sergey Pisklakov
Jean-Francois Pittet
Mihai Podgoreanu
David Polaner
Julia Pollock
Wanda Popescu
Jovan Popovic
Helen Powers
Y.s. Prakash
Ravindra Prasad
Jayant Pratap
Johnathan Pregler
Paul Preston
Ernesto Pretto
Rene Przkora
Erin Pukenas
Patrick Purdon
Joseph Quinlan
Dan Raemer
Govind Rajan
Niraja Rajan
Sally Rampersad
Gail Randel
Jacob Raphael
Emily Ratner
Aeyal Raz
Elizabeth Rebello
Amanda Redding
Sundara Reddy
Allan Reed
Mohamed Rehman
John Edward Reynolds
Paul Reynolds
Rosamund Rhodes
Jalil Riazi
Mark Rice
Elizabeth Rickerson
Matthias Riess
Sean Rivard
Richard Rivers
Christopher Robards
Amy Robertson
Steven Robicsek
David Robinowitz
Albert Robinson
Stephen Robinson
Meghan Rodes
Leopoldo Rodriguez
Daniel Roke
Mark Rollins
Philip Roman
Ryan Romeo
Gregory Rose
Andrew Rosenberg
Vernon Ross
Andrew Roth
Patricia Roth
David Rothenberg
Brian Rothman
John Rowlingson
Marc Rozner
Stephen Rupp
Deborah Rusy
Lynn Rusy
Haleh Saadat
Senthilkumar Sadhasivam
Nicholas Sadovnikoff
Amgad Saied
Xavier Sala-Blanch
Francis Salinas
Samuel Samuel
Kenneth Sapire
Mona Sarkiss
Amod Sawardekar
Barbara Scavone
Scott Schartel
Gregory Schears
Randall Schell
Corey Scher
Andrew Schlay
Michelle Schlunt
Bettina Schmitz
Gerhard Schneider
Mark Schneider
Kai Schoenhage
Catherine Scholl
Kristopher Schroeder
Armin Schubert
Thomas Schulte
Caleb Schultz
Roman Schumann
Joseph Schwab
Alan Jay Schwartz
Andrew Schwartz
Mike Schweitzer
Deborah Schwengel
Karen Schwenzer
Joshua Sebranek
John Seif
Catherine Seipel
Audrey Shafer
David Shaff
Donald Shaffner
Ravi Shah
Sajid Shahul
Jack Shanewise
Fred Shapiro
Sam Sharar
Deepak Sharma
James Shear
Torin Shear
John Shepler
George Sheplock
Ketan Shevde
Maria Shier
Sasha Shillcutt
George Silvay
David Silver
Jeffrey Silverstein
Kenneth Silverstein
Alan Sim
William Simmons
Michael Simon
Nina Singh-Radcliff
Mark Singleton
Ashish Sinha
Nikolas Skubas
Robert Sladen
Peter Slinger
Tod Sloan
Charles Smith
Kathleen Smith
Martin Smith
Sarah Smith
Timothy Smith
Lisa Sohn
Daneshvari Solanki
Ken Solt
Neilesh Soneji
Massimilano Sorbello
Roy Soto
Karen Souter
Dmitri Souzdalnitski
Donat Spahn
William Spearman
Stephen Spring
Sven Staender
Brian Starr
Creed Stary
Susan Staudt, MD
Randolph Steadman
Erica Stein
John Stephenson
Marjorie Stiegler
Tracey Stierer
Ljuba Stojiljkovic

179
Tracey Straker
Jacob Strand
Andrea Strathman
Scott Streckenbach
Gary Strichartz
Paul Stricker
Wyndam Strodtbeck
Kathirvel Subramaniam
Erin Sullivan
John Sum-Ping
William Sumrall
Sugantha Sundar
Yung-Fong Sung
Maya Suresh
Santhanam Suresh
Stephen Surgenor
Robert Suriani
Hans Sviggum
Madhav Swaminathan
BobbieJean Sweitzer
Alexandra Szabova Min
Peter Szmuk
Joseph Szokol
Pekka Talke
Daniel Talmor
Rosalie Tassone
Richard Taus
Wendy Teoh
Gregory Terman
John Tetzlaff
Julie Thacker
Nelson Thaemert
Dilip Thakar
Ilka Theruvath
Oliver Theusinger
Stephan Thilen
Leslie Thomas
Mack Thomas
Annemarie Thompson
Jeff Thompson
Arlyne Thung
Mitchell Tobias
Catherine Tobin
Kate Tobin
Michael Todd
Reda Tolba
Paloma Toledo
Concezione Tommasino
Justin Traunero
Kevin Tremper
Narendra Trivedi
Christopher Troianos
Angela Truong
Stephen Ttendo
Cynthia Tung
Mark Twite
Mercy Udoji
Joshua Uffman
Kelly Ural
Felipe Urdaneta
Richard Urman
Sonia Vaida
Shermeen Vakharia
Songyos Valairucha
Manuel Vallejo
Christa Van Dort
Gail Van Norman
Adriaan Van Rensburg
Mary Ann Vann
Megan Varellas
Lakshmikumar Venkat Ragha-
van
Steven Venticinque
Susan Verghese
Amy Vinson
Ashwin Viswanathan
Shane Volney
Kevin Vorenkamp
Melissa Vu
Trung Vu
Laszlo Vutskits
Amaresh Vydyanathan
Chad Wagner
Joyce Wahr
David Waisel
Samuel Wald
Ashutosh Wali
Michael Wall
John Walsh
Michael Walsh
Daniel Wambold
Jonathan Wanderer
Shu-Ming Wang
Denham Ward
David Warner
Mark Warner
Daniel Warren
Lisa Warren
Marcin Wasowicz
Jonathan Waters
Scott Watkins
Charles Watson
Deborah Watson
Matthew Wecksell
Menachem Weiner
Matthew Weinger
Mark Weiss
Nathaen Weitzel
Lynda Wells
Eric Werner
James West
Sivan Wexler
Michelle White
Richard Whitlock
Duminda Wijeysundera
Troy Wildes
David Wilkinson
Brian Williams
Brian Williams
Libby Williams
Julie Williamson
Tamara Willis
Karl Willmann
Sylvia Wilson
William Wilson
Thomas Witkowski
David Wlody
Ruth Wohlfeld
Richard Wolman
Cynthia Wong
David Wong
Patrick Wong
Michael Woo
Derek Woodrum
Lee Woodson
Christopher Wray
Crystal Wright
Hannah Wunsch
Yan Xu
Jacques Yadeau
Samuel Yanofsky
Meltem Yilmaz
David Young
George Youssef
Francine Yudkowitz
Vivian Manying Yuen
Luis Zabala
Zdravka Zarova
Ahmed Zaky
Warren Zapol
Laura Zeigler
John Zerwas
Yun-Xia Zuo
Andrew Zura
David Zvara
DISCLOSURES
180
Jaime Aaronson M.D.
Basem Abdelmalak M.D.
Salahadin Abdi M.D.
James Abernathy M.D., M.P.H.
Amr Abouleish M.D, M.B.A.
Ron Abrons M.D., Ph.D.
Anthony Absalom M.D.
Gareth Ackland M.D.
Anoushka Afonso M.D.
Zulqar Ahmed M.D., F.A.A.P.
Kyle Ahn M.D.
Ozan Akca M.D.
Shamsuddin Akhtar M.D.
Wael Ali Sakr Esa M.D.
Inger Aliason M.D.
Rae Allain M.D.
John Allyn M.D.
Adam Amundson M.D.
Aparna Ananth M.D.
Arpana Ananth M.D.
Zirka Anastasian M.D.
Jennifer Anderson M.D.
T. Anderson M.D., Ph.D.
Michael Andreae M.D., M.S.
Maged Andrews M.B.,B.Ch.
Dean Andropoulos M.D.
Magdalena Anitescu M.D.
J. Ansermino M.B., B.Ch.
Jeffrey Apfelbaum M.D.
Gregory Applegate D.O.
Maged Argalious M.D., M.B.A.
Valerie Armstead M.D.
George Arndt M.D.
Solomon Aronson M.D., M.B.A., FACC, FCCP,
FAHA, FASE
Harendra Arora M.B.,B.S.
Radha Arunkumar M.B., B.S., M.D.
Rebecca Aslakson M.D., Ph.D.
Arthur Atchabahian M.D.
John Augoustides M.D.
Yianni Augoustides M.D.
David Auyong M.D.
Edwin Avery, IV M.D.
Ra Avitsian M.D.
Michael Avram Ph.D.
Douglas Bacon M.D., M.A.
Angela Bader M.D.
James Bagian M.D., PE
Keith Baker M.D., Ph.D.
Christine Ball M.B.,B.S., FANZCA
Arna Banerjee M.B.,B.S.
Dalia Banks M.D.
Carolyn Bannister M.D.
Paul Barash M.D.
Cristina Barboi M.D.
Steven Barker Ph.D., M.D.
Sheila Barnett M.B., B.S., B.Sc.
Michael Barrington M.B.,B.S., Ph.D.
Joseph Bayes M.D.
Hernan Bazan M.D.
Shawn Beaman M.D.
Richard Beers M.D.
Elizabeth Behringer M.D.
Yaakov Beilin M.D.
Yaakov (Jake) Beilin M.D.
Charlotte Bell M.D.
Anke Bellinger M.D.
Sadek Beloucif M.D.
Mohamed Ben Ammar M.D.
S. Patrick Bender M.D.
Audree Bendo M.D.
Esther Benedetti M.D.
James Benonis M.D.
Honorio Benzon M. D.
Charles Berde M.D., Ph.D.
Keith Berge M.D.
Lauren Berkow M.D.
William Berry M.D.
Tarun Bhalla M.D.
Sanjay Bhananker M.D.
Anuj Bhatia M.D.
Julian Bick M.D.
Mark Bicket M.D.
Luca Bigatello M.D.
Frederic Billings M.D.
Wendy Binstock M.D.
Patrick Birmingham M.D.
David Birnbach M.D., M.P.H.
Susan Black M.D.
Kimberly Blasius M.D.
Jeanna Blitz M.D.
James Blum M.D.
Anne Boat M.D.
Sylvain Boet M.D., M.Ed.
Steven Boggs M.D., M.B.A.
Michael Boisen M.D.
Karen Boretsky M.D.
Alain Borgeat M.D.
Adrian Bosenberg M.B.,Ch.B.
Zeljko Bosnjak Ph.D.
Michael Bottros M.D.
Gregory Botz M.D.
Arthur Boudreaux M.D.
Demetrios Bourdakos M.D.
Edwin Bowe M.D.
Patrick Boyle M.D.
William Bradford M.D.
Mary Beth Brady M.D.
Tara Brakke M.D.
Jess Brallier M.D.
Ansgar Brambrink M.D., Ph.D.
Gary Brenner M.D.. Ph.D.
Claire Brett M.D.
David Broussard M.D.
Charles Brown M.D., M.H.S.
Daniel Brown M.D., Ph.D.
Emery Brown M.D., Ph.D.
Sorin Brull M.D.
Chad Brummett M.D.
Ethan Bryson M.D.
Marek Brzezinski M.D., Ph.D.
Chester Buckenmaier III, M.D.
Brenda Bucklin M.D.
Amanda Burden M.D.
John Butterworth IV, M.D.
Alexander Butwick M.B., B.S.
Steven Butz M.D.
Asokumar Buvanendran M.D.
Michael Cahalan M.D.
Arthur Calimaran M.D.
Javier Campos M.D.
Kenneth Candido M.D.
Christopher Canlas M.D.
Maxime Cannesson M.D., Ph.D.
Levon Capan M.D.
Louanne Carabini M.D.
Lawrence Caruso M.D.
Brendan Carvalho FRCA
Maria Castillo M.D.
Davide Cattano M.D.,Ph.D.
Matthew Chan M.D.
Vincent Chan M.D.
Rekha Chandrabose M.D.
Debnath Chatterjee M.D.
Jacques Chelly M.D., Ph.D., M.B.A.
Jianguo Cheng M.D.
Albert Cheung M.D.
Joseph Chiang M.D.
May Chin M.D.
Srinivas Chiravuri M.D.
Hovig Chitilian M.D.
Christopher Choukalas M.D., M.S.
Jason Chua M.D.
Frances Chung M.B.B.S., F.R.C.P.C.
Franklyn Cladis M.D.
David Clark M.D.
Jerry Clark M.D.
Steven Clendenen M.D.
Edmond Cohen M.D.
Ira Todd Cohen M.D., M.Ed.
Jonathan Cohen M.D.
Neal Cohen M.D., M.P.H., M.S.
C. David Collard M.D., M.S.
Douglas Colquhoun M.B., Ch.B., M.Sc.,
M.P.H.
Daniel Cook B.S.
Richard Cook M.D.
Jeffrey Cooper Ph.D.
Richard Cooper M.D.
Elifce Cosar M.D.
Douglas Coursin M.D.
Charles Cowles M.D., M.B.A.
Robin Cox M.D.
Gregory Crosby M.D.
Miguel Cruz M.D.
Deborah Culley M.D.
William Culp M.D.
Saundra Curry M.D.
Thomas Cutter M.D.
Armagan Dagal M.D., FRCA
Robert D’Angelo M.D.
Christopher Darling D.O.
Andrew Davidson M.D.
Miles Day M.D.
Stefan De Hert M.D.
Anthony De La Cruz M.D.
Oscar De Leon-Casasola M.D.
Timothy Deer M.D.
Giorgio Della Rocca M.D.
Christina DeLucca M.D.
Samuel DeMaria M.D.
Alicia Dennis MBBS, Ph.D., PGDipEcho,
FANZCA
Ryan Derby M.D., M.P.H.
Meena Desai M.D.
Jayant Deshpande M.D., M.P.H.
Mark Deshur M.D., MBA
Zachary Deutch M.D.
Nina Deutsch M.D.
Prabhakar Devavaram M.B.,B.S.
Philip Devereaux M.D.

181
James Di Nardo M.D.
Christina Diaz M.D.
Geraldine Diaz M.D.
Laura Diaz M.D.
Daniel Diaz-Gil Medical Student
David Dickerson M.D.
Daniel Diedrich M.D.
Pierre Diemunsch M.D.
Stephen Dierdorf M.D.
John Dilger M.D.
Dawn Dillman M.D.
James DiNardo M.D.
Jeffrey Dobyns D.O.
Lena Dohlman M.D., M.P.H.
John Dombrowski M.D.
Karen Domino M.D., M.P.H.
Carolina Donado M.D.
Christine Doyle M.D.
D. John Doyle M.D., Ph.D.
Elizabeth Drum M.D.
John Drummond M.D.
Richard Dsida M.D.
Stanlies D’Souza M.D.,F.R.C.A
Roman Dudaryk M.D.
Amy Duhachek-Stapelman M.D.
Peggy Duke M.D.
Peter Dunbar M.B.,Ch.B., M.B.A
Richard Dutton M.D., M.B.A.
Maxim Eckmann M.D.
Angela Edwards M.D.
Talmage Egan M.D.
Junji Egawa M.D.
Jami Eidem M.D.
Matthias Eikermann M.D.
Sharon Einav M.D.
James Eisenach M.D.
James Eisenkraft M.D.
Foad Elahi MD
Nabil Elkassabany M.D.
Clint Elliott M.D.
Richard Elliott M.D.
John Ellis M.D.
Dalia Elmofty M.D.
Hesham Elsharkawy M.D.
Kelly Elterman M.D.
Charles Emala M.D.
Jorg Ender M.D.
Ryan Endersby M.D.
Calvin Eng M.D.
Kristin Engelhard M.D., Ph.D.
F. Kayser Enneking M.D.
Michael Erdek M.D.
Mark Ereth M.D.
Lars Eriksson M.D., Ph.D., FRCA
Adam Evans M.D., M.B.A.
Faye Evans M.D.
Lucinda Everett M.D.
Brenda Fahy M.D., FCCM
Ehab Farag M.D., F.R.C.A.
Michaela Farber M.D., M.S.
Neil Farber M.D., Ph.D.
Ludwik Fedorko M.D., Ph.D.
Jessica Feinleib M.D., Ph.D.
David Feinstein M.D.
Jeffrey Feldman M.D., M.S.E.
Marc Feldman M.D., MHS
Xiaomei Feng M.D., Ph.D.
Ana Fernandez-Bustamante M.D., Ph.D.
Roshan Fernando M.B.,Ch.B.
David Ferson M.D.
John Fiadjoe M.D.
Matthew Fiegel M.D.
Larry Field M.D.
Patrick Filip M.D.
Daniela Filipescu M.D.
James Findlay M.B.,Ch.B.
Roderick Finlayson M.D.
Alan Finley M.D.
Gregory Fischer M.D.
Jane Fitch M.D.
Meghann Fitzgerald M.D.
Michael Fitzsimons M.D.
Peter Fleischut M.D.
Lee Fleisher M.D.
Alana Flexman M.D.
Randall Flick M.D.
Lorraine Foley M.D.
Manuel Fontes M.D.
Amy Forbis J.D.
Amanda Fox M.D., M.P.H.
Regina Fragneto M.D.
Carlo Franco M.D.
Marcellene Franzen M.D.
Michael Frass M.D.
Elizabeth Frost M.B.,Ch.B.
Giulio Frova M.D.
Thomas Fuchs-Buder M.D.
Natasha Funck M.D.
Cory Furse M.D.
Emmanuel Futier M.D., Ph.D.
David Gaba M.D.
Jeff Gadsden M.D., FANZCA
Robert Gaiser M.D.
Eduardo Galeano M.D.
Richard Galgon M.D., M.S.
Samuel Galvagno Jr., D.O., Ph.D., M.S.
Jorge Galvez M.D.
Tong Gan M.D.
Kishor Gandhi M.D., M.P.H.
Arjunan Ganesh M.B.B.S.
Steven Gayer M.D., M.B.A.
Adrian Gelb M.B.,B.Ch., FRCPC
Theresa Gelzinis M.D.
Brenda Gentz M.D.
Jessica George M.D.
Andrew Gettinger M.D.
Katherine Gil M.D
Thomas Gildea M.D.
Richard Gillerman M.D., Ph.D.
Christopher Gilligan M.D., M.B.A.
Keith Gipson M.D., Ph.D.
Laurent Glance M.D.
Kathryn Glas M.D.
Nancy Glass M.D., M.B.A.
Neil Goldenberg M.D., Ph.D.
Sara Goldhaber-Fiebert M.D.
Peter Goldstein M.D.
Robert Goldstein M.D.
Brenda Golianu M.D.
Jeffrey Gonzales M.D.
Cheryl Gooden M.D.
Stephanie Goodman M.D.
Basavana Goudra M.D., FRCA, FCARCSI
Robert Gould M.D.
Trusha Govindji M.D.
James Grant M.D.
Stuart Grant M.D.
Loreta Grecu M.D.
Matthew Green M.D.
Steven Greenberg
Chad Greene
Katherine Grichnik M.D., M.S.
Thomas Grissom M.D.
Karina Gritsenko MD
Leanne Groban M.D.
Hilary Grocott M.D.
Michael Gropper M.D., Ph.D.
Jeffrey Gross M.D.
Carrie Guheen M.D.
George Guldan III, M.D.
Anita Gupta D.O., Pharm.D.
Dhanesh Gupta M.D.
Allen Gustin M.D.
Jacob Gutsche M.D.
Admir Hadzic M.D.
Katherine Hagan M.D.
Carin Hagberg M.D.
Dawit Haile M.D.
Thomas Halaszynski M.D., MBA
Matthew Hallman M.D.
Hossam Hamda M.D.
Laura Hammel M.D.
William Hammonds M.D.
William Hand M.D.
Judith Handley M.D.
John Hanlon M.D.
Raafat Hannallah M.D.
Michael Hannaman M.D.
Neil Hanson M.D.
David Hardman M.D.
H. David Hardman M.D., MBA
Courtney Alan Hardy M.D.
Greg Hare M.D.
Priscilla Harrell M.D.
Kyle Harrison M.D.
Thomas Harrison M.D.
Gregg Hartman M.D.
Stephen Haskins M.D.
Marc Hassid M.D.
Steven Hattamer M.D.
Joy Hawkins M.D.
Salim Hayek M.D., Ph.D.
Gary Haynes M.D., Ph.D.
Stephen Hays M.D.
David Healy M.D., MRCP, FRCA
James Hebl M.D.
Eugenie Heitmiller M.D.
Lars Helgeson M.D.
Laura Hemmer M.D.
David Hepner M.D.
Andrew Herlich D.M.D., M.D.. F.A.A.P.
Antonio Hernandez M.D.
Douglas Hester M.D.
Michael Hicks M.D.
Kenneth Hiller M.D.
Paul Hilliard M.D.
Jonathan Ho M.D.
Juliann Hobbs M.D.,M.P.H.
Michael Hofkamp M.D.
Charles Hogue M.D.
Ingrid Hollinger M.D.
SPEAKER INDEX
182
Harriet Hopf M.D.
Terese Horlocker M.D.
Constance Houck M.D.
Grant Lindsay Hounsell M.D.
Kimberly Howard-Quijano M.D.
McCallum Hoyt M.D., M.B.A.
Robert Hsiung M.D.
Eric Hsu M.D.
Ling Qun Hu M.D.
Andrea Huang M.D.
Yuguang Huang M.D
Jeffrey Hubbard M.D., M.S.
Anthony Hudetz D.B.M., Ph.D.
Julie Huffmyer M.D.
Elisabeth Hughes M.D.
Orlando Hung M.D
Marc Huntoon M.D.
Agnes Hunyady M.D.
William Hurford M.D.
Muhammad Hussain M.D.
Michael Hutchens M.D.
Jason Hwang M.D.
Pedro Ibarra M.D., MSc
Barys Ihnatsenka M.D.
Mizuko Ikeda M.D., Ph.D.
Brian Ilfeld M.D., M.S.
Eiichi Inada M.D.
Yumiko Ishizawa MD, MPH, PhD
Giorgio Ivani M.D.
Yulia Ivashkov M.D.
Khalil Jabbour M.D.
Adam Jacob M.D.
Jeena Jacob M.D.
Matthias Jacob M.D., PhD.
Jeffrey Jacobs M.D.
Eric Jacobsohn M.B.,Ch.B.
Narasimhan Jagannathan M.D.
Jonathan Jahr M.D.
Leslie Jameson M.D.
Gregory Janelle M.D., F.A.S.E.
Joe Jansen M.D.
Christina Jeng M.D.
Vesna Jevtovic-Todorovic M.D.
Aaron Joffe D.O.
Roger Johns M.D.
Daniel Johnson M.D.
Judy Johnson M.D.
Matthew Johnson Ph.D.
Rebecca Johnson M.D.
Dean Jones M.D., FRCPC
Raymond Joseph M.D.
Vilma Joseph M.D.
Girish Joshi M.D.
Marc Kahn M.D., M.B.A.
Zeev Kain M.D., M.B.A.
Cor Kalkman M.D., Ph.D.
Mihir Kamdar M.D.
Ihab Kamel M.D.
Ming-Chih Kao M.D.
Marshal Kaplan M.D.
Manoj Karmakar M.B.,B.S.
Rami Karroum M.D.
Olga Kaslow M.D., Ph.D.
Brian Kavanagh M.B.
Donald Keeler M.D.
Henrik Kehlet M.D., Ph.D.
Richard Kelly M.D.
Max Kelz M.D., Ph.D.
Paul Kempen M.D., Ph.D.
Judy Kersten M.D.
Miklos Kertai M.D.
Evan Kharasch M.D., Ph.D.
Swapnil Khoche M.B., B.S.
Sean Kiley M.D.
Jung Kim M.D.
Tae Kim M.D.
Tae-Wu Kim M.D.
Kyle Kirkham M.D., FRCPC
Jerome Klafta M.D.
Andrew Klein M.D.
Norma Klein M.D.
Allan Klock M.D.
P. Klock M.D.
Colleen Koch M.D., M.S.
Antoun Koht M.D.
Lavinia Kolarczyk M.D.
Michael Kopec M.D.
Sandra Kopp M.D.
Eugene Koshkin M.D.
Thomas Kotsonis M.D.
Pete Kovatsis M.D.
Sibylle Kozek M.D., M.B.A.
Elliot Krane M.D.
Michael Kristensen M.D.
Robert Krohner D.O.
Catherine Kuhn M.D.
Anjana Kundu M.D.
Andrea Kurz M.D.
Karim Ladha M.D.
Robert Lagasse M.D.
Yan Lai M.D.,M.P.H.
Kirk Lalwani M.B., B.S., FRCA
Jason Lane M.D., M.P.H.
Beth Demers Lavelle M.D.
Melissa Laxton M.D.
Allison Lee M.D.
Bonny Lee M.D.
Chanhung Lee M.D.
Lorri Lee M.D.
Mitchell Lee M.D.
Tat Leang Lee M.B., B.S.
Jonathan Leff M.D.
Lisa Leffert M.D.
Marc Leib M.D.
Mark Leibel M.D.
Andrew Leibowitz M.D.
Louis Lejarza
Joel Levey Ph.D
Michelle Levey M.A
Matthew Levin M.D.
Adam Levine M.D.
Wilton Levine M.D.
Jerrold Levy M.D.
Linda Le-Wendling M.D.
Galina Leyvi M.D.
Mei-Ying Liang M.D.
Yuan-Chi Lin M.D.
Steven Lisco M.D.
Ronald Litman D.O.
Linda Liu M.D.
Spencer Liu M.D.
Asa Lockhart M.D., M.B.A.
Andreas Loepke M.D., Ph.D.
Martin London M.D.
Lindsey Loveland-Baptist M.D.
Timothy Lubenow M.D.
Stephen Lucas M.D.
Tanya Lucas M.D.
Danielle Ludwin M.D.
Philip Lumb M.D.
Pastor Luna M.D.
Gerald Maccioli M.D.
David Mackey M.D.
Sean Mackey M.D., Ph.D.
David MacLeod M.D.
Aman Mahajan M.D., P.H.D.
Elizabeth Mahanna M.D.
Kamal Maheshwari M.D.
Mohamed Mahmoud M.B.,B.Ch.
David Maine M.D.
Anuj Malhotra M.D.
Khalid Malik M.D.
Tariq Malik M.D.
Shobha Malviya M.D.
Jeff Mandel M.D., M.S.
David Mann M.D.
Bruno Marciniak M.D.
Edward Mariano M.D.
Jonathan Mark M.D.
Scott Markowitz M.D., FAAP
Erich Marks M.D.
Mitchell Marshall M.D.
Christine Martin M.D.
Gavin Martin M.B.,Ch.B.
Susan Martinelli M.D.
Vicente Martinez-Pons M.D., Ph.D.
George Mashour M.D., Ph.D.
Chawla LaToya Mason M.D.
Eric Mason M.D.
Keira Mason M.D.
Linda Mason M.D.
Adrian Matioc M.D.
Maria Matuszczak M.D.
Robina Matyal M.D.
Walter Maurer M.D.
Timothy Maus M.D.
Lynne Maxwell M.D.
C. Mazer M.D.
John McAllister M.D.
Mary Ellen McCann M.D., M.P.H.
Patrick McCarty M.D.
Craig McClain M.D.
Maureen McCunn M.D., MIPP
David McDonagh M.D.
Timothy McDonald M.D.
Matthew McEvoy M.D.
Kathryn McGoldrick M.D.
Ali Mchaourab M.D.
Anne Marie McKenzie Brown M.D.
Duncan McLean M.D.
Jason McVicar M.D.
Nagy Mekhail M.D.,Ph.D.
Jannicke Mellin-Olsen M.D., Dr.PH
Estela Melman M.D.
Joseph Meltzer M.D.
Matthias Merkel M.D., Ph.D.
Sharon Merrick M.S., CCS-P
Alan Merry M.D.
Alonso Mesa M.D.
Amy Mesa-Jonassen M.D.
David Metro M.D.

183
Julia Metzner M.D.
Jill Mhyre M.D.
Rafael Miguel M.D.
Scott Miller M.D.
Steven Miller M.D.
Thomas Miller Ph.D., M.B.A.
Mohammed Minhaj M.D.
Leonid Minkovich M.D.
Alexander Mittnacht M.D.
Annette Mizuguchi M.D., Ph.D.
Daria Moaveni M.D.
James Modir M.D.
Vivek Moitra M.D.
Yue-Pang Mok M.D.
Candice Montzingo M.D.
James Moore M.D.
Laurel Moore M.D.
Tomonori Morita M.D
Debra Morrison M.D.
Loran Mounir M.D.
Loran Mounir Soliman M.D.
Danny Muehlschlegel M.D.
Jan Mulier M.D., Ph.D.
John Murkin M.D.
Glenn Murphy M.D.
Michael Murphy M.D.
David Murray M.D.
Michael Murray M.D., Ph.D.
Kimmo Murto M.D.
Paul Myles M.B., B.S.
Antoun Nader M.D.
Ryan Nagy M.D.
Samer Narouze M.D., Ph.D.
Robert Naruse M.D.
Muhaammed Nasir M.B.,B.S.
Joseph Neal M.D.
Nicholas Nedeff M.D.
Jacques Neelankavil M.D.
John Neeld M.D.
Vladimir Nekhendzy M.D.
Patrick Neligan M.B., B.Ch.
Eric Nelson D.O.
Kenneth Nelson M.D.
Edward Nemergut M.D.
Mark Neuman M.D., M.Sc.
Steven Neustein M.D.
Michael Nichols A.A.-C
Alina Nicoara M.D.
Adam Niesen M.D.
Dolores Njoku M.D.
James North M.D.
Mark Nunnally M.D., FCCM
Michael Nurok M.B.,Ch.B., Ph.D.
Nancy Nussmeier M.D.
Sydney Nykiel D.O.
Michael O’Connor M.D., FCCM
Colleen O’Leary M.D.
Susan O’Leary M.D., FRCPC
Michael Oleyar D.O.
Patrick Olomu M.D.
Olutoyin Olutoye M.D., M.Sc., F.A.A.P.
Vilma Ortiz M.D.
Irene Osborn M.D.
James Osorio M.D.
Kristie Osteen M.D.
Ellen O’Sullivan FCAI, FRCA, FCPSP
Einar Ottestad M.D.
Sheela Pai M.D.
Arvind Palanisamy M.D., FRCA
Jason Panchamia D.O.
Pratik Pandharipande M.D.
Oliver Panzer M.D.
Christine Park M.D.
Brian Parker M.D.
Vikram Patel M.D.
Bridget Pearce M.D.
Ronald Pearl M.D., Ph.D.
Paolo Pelosi M.D.
Philip Peng M.B.B.S.
Susan Penney J.D.
Anahi Perlas M.D.
Misha Perouansky M.D.
Albert Perrino M.D.
Gene Peterson M.D., Ph.D.
Cathleen Peterson-Layne M.D.,Ph.D.
Beverly Philip M.D.
Mark Phillips M.D.
May Pian-Smith M.D.
Paul Picton M.D.
Michael Pilla M.D.
Carlos Pino M.D.
Sergey Pisklakov M.D.
Jean-Francois Pittet M.D.
Jeffrey Plagenhoef M.D.
Stanford Plavin M.D.
Kelly Pollak M.D.
Julia Pollock M.D.
Wanda Popescu M.D.
Jovan Popovic M.D.
Y.s. Prakash M.D., Ph.D.
Jayant Pratap M.B.,B.Ch.
Paul Preston M.D.
David Provenzano M.D.
Rene Przkora M.D., Ph.D.
Erin Pukenas M.D.
Chunyuan Qiu M.D., M.S.
Joseph Quinlan M.D.
Govind Rajan M.D.
Niraja Rajan M.B.
Satya-Krishna Ramachandran M.D.
Chandra Ramamoorthy M.D.
Sally Rampersad M.B., FRCA
Davinder Ramsingh M.D.
Maunak Rana M.D.
Gail Randel M.D.
James Rathmell M.D.
Emily Ratner M.D.
Richard Rauck M.D.
Elizabeth Rebello M.D.
Amanda Redding M.D.
Scott Reeves M.D., M.B.A.
John Edward Reynolds M.D.
Paul Reynolds M.D.
Jalil Riazi M.D.
Elizabeth Rickerson M.D.
Matthias Riess M.D., Ph.D.
Richard Rivers M.D., Ph.D.
Christopher Robards M.D.
Russell Roberson M.D.
Amy Robertson M.D.
Steven Robicsek M.D., Ph.D.
Meghan Rodes M.D.
Doris Rohde Ph.D.
Daniel Roke M.D.
Mark Rollins M.D., Ph.D.
Ryan Romeo M.D.
Margot Roozekrans M.D.
Gregory Rose M.D.
Andrew Rosenberg M.D.
Meg Rosenblatt M.D.
William Rosenblatt M.D.
Richard Rosenquist M.D.
Vernon Ross M.D.
Andrew Roth M.D.
Patricia Roth M.D.
Brian Rothman M.D.
John Rowlingson M.D.
Colin Royse M.B.,B.S.
Marc Rozner M.D., Ph.D.
Stephen Rupp M.D.
Keith Ruskin M.D.
Deborah Rusy M.D.
Lynn Rusy M.D.
Haleh Saadat M.D.
Senthilkumar Sadhasivam M.D
Nicholas Sadovnikoff M.D., F.C.C.M.
Nahel Saied M.B., B. Ch.
Xavier Sala-Blanch M.D.
Francis Salinas M.D.
Kenneth Sapire M.D.
Todd Sarge M.D.
Mona Sarkiss M.D.
Atsushi Sawada M.D., Ph.D.
Amod Sawardekar M.D.
Barbara Scavone M.D.
John Schaefer III, M.D.
Scott Schartel D.O.
Gregory Schears M.D.
Randall Schell M.D., M.Ed.
Corey Scher M.D.
Michelle Schlunt M.D.
J. Michael Schmidt Ph.D., M.Sc.
Bettina Schmitz M.D., Ph.D., DEAA
Mark Schneider M.D.
Catherine Scholl M.D.
Kristopher Schroeder M.D.
Armin Schubert M.D., M.B.A.
Peter Schulman M.D.
Thomas Schulte M.D.
Roman Schuman M.D.
Roman Schumann M.D.
Joseph Schwab M.D., M.S.
Alan Jay Schwartz M.D., M.S.
Mike Schweitzer M.D., M.B.A.
Deborah Schwengel M.D.
Joshua Sebranek M.D.
John Seif M.D.
Catherine Seipel M.D.
Judith Semo J.D.
Judith Jurin Semo J.D., Esq.
Daniel Sessler M.D.
Donald Shaffner Jr., M.D.
Ravi Shah M.D.
Sajid Shahul M.D., MPH
Aryeh Shander M.D.
Jack Shanewise M.D.
Hariharan Shankar M.B.,B.S.
Sam Sharar M.D.
John Shepler M.D.
Stanton Shernan M.D., F.A.H.A., F.A.S.E.
Ketan Shevde M.D.
SPEAKER INDEX

184
Maria Shier M.D.
Sasha Shillcutt M.D.
Douglas Shook M.D.
Jeffrey Silverstein M.D.
Kenneth Silverstein M.D., M.B.A.
Alan Sim M.D.
William Simmons M.D.
Michael Simon M.D.
Allan Simpao M.D.
Mark Singleton M.D.
Ashish Sinha M.D., Ph.D.
Nikolaos Skubas M.D.
Nikolas Skubas M.D.
Robert Sladen M.B.,Ch.B., FCCM
Peter Slinger M.D.
Tod Sloan M.D., Ph.D., M.B.A.
Richard Smiley M.D., Ph.D.
Charles Smith M.D.
Kathleen Smith M.D.
Martin Smith M.B.,B.S.
Sarah Smith M.D.
Roman Sniecinski M.D.
Jose Soberon M.D.
Lisa Sohn M.D.
Ken Solt M.D.
Neilesh Soneji M.D.
Massimilano Sorbello M.D.
Sulpicio Soriano M.D.
Roy Soto M.D.
Michael Souter M.B., Ch.B., FRCA
Sven Staender M.D
Brian Starr M.D.
Creed Stary M.D., Ph.D.
Stanley Stead M.D. MBA
Randolph Steadman M.D., M.S.
Erica Stein M.D.
Francis Stellaccio M.D.
Marjorie Stiegler M.D.
Ljuba Stojiljkovic M.D., Ph.D.
Tracey Straker M.D., M.P.H.
Jacob Strand M.D.
Andrea Strathman M.D.
Scott Streckenbach M.D.
Gary Strichartz Ph.D.
Paul Stricker M.D.
Wyndam Strodtbeck M.D.
Kathirvel Subramaniam M.D.
John Sullivan M.D., M.B.A.
William Sumrall III, M.D.
Lena Sun M.D.
Sugantha Sundar M.D.
Yung-Fong Sung M.D.
Maya Suresh M.D.
Santhanam Suresh M.D.
Stephen Surgenor M.B.A., M.D.
Robert Suriani M.D.
Hans Sviggum M.D.
Madhav Swaminathan M.D.
BobbieJean Sweitzer M.D.
Margit Szabari M.D.
Peter Szmuk M.D.
Joseph Szokol M.D., J.D, M.B.A.
Pekka Talke M.D.
Daniel Talmor M.D., M.P.H.
Rosalie Tassone M.D., M.P.H.
Norman Taylor M.D., Ph.D.
Wendy Teoh M.B.,B.S., FANZCA
John Tetzlaff M.D.
Nelson Thaemert M.D.
Dilip Thakar M.D.
Ilka Theruvath M.D.
Stephan Thilen M.D., M.S.
Leslie Thomas M.D.
Mack Thomas M.D.
Annemarie Thompson M.D.
Jeff Thompson M.D.
Catherine Tobin M.D.
Joshua Tobin M.D.
Michael Todd M.D.
Paloma Toledo M.D., M.P.H.
Concezione Tommasino M.D.
Justin Traunero M.D.
Narendra Trivedi M.D.
Christopher Troianos M.D.
Lawrence Tsen M.D.
Avery Tung M.D., F.C.C.M.
Cynthia Tung M.D.
Mark Twite M.D.
Mercy Udoji M.D.
Joshua Uffman M.D.
Soban Umar M.D., Ph.D.
Kelly Ural M.D.
Felipe Urdaneta M.D.
Richard Urman M.D., M.B.A., C.P.E.
Sonia Vaida M.D.
Songyos Valairucha M.D
Manuel Vallejo M.D., D.M.D.
Gail Van Norman M.D.
Adriaan Van Rensburg M.D.
Mary Ann Vann M.D.
John Vargo M.D., M.P.H.
Albert Varon M.D.
Jeffery Vender M.D., FCCM
Lakshmikumar Venkat Raghavan M.B.,B.S.
Steven Venticinque M.D.
Chandy Verghese M.D.
Susan Verghese M.D
Marcos Vidal-Melo M.D., Ph.D.
Amy Vinson M.D.
Eugene Viscusi M.D.
Shane Volney M.D.
Kevin Vorenkamp M.D.
Melissa Vu M.D.
Trung Vu M.D.
Laszlo Vutskits M.D.
Amaresh Vydyanathan M.D.
Leonard Wade M.S.
Chad Wagner M.D.
Joyce Wahr M.D.
David Waisel M.D.
Gary Walco Ph.D.
Samuel Wald M.D.
Ashutosh Wali M.D.
Benjamin Walker M.D.
Michael Wall M.D.
John Walsh M.D.
Michael Walsh M.D.
Daniel Wambold M.D.
Jonathan Wanderer M.D.
Shu Ming Wang M.D.
Shu-Ming Wang M.D.
David Warner M.D.
Mark Warner M.D.
Daniel Warren M.D.
Lisa Warren M.D.
Marcin Wasowicz M.D.
Scott Watkins M.D.
Charles Watson M.D.
Guy Weinberg M.D.
Menachem Weiner M.D.
Matthew Weinger M.D.
Mark Weiss M.D.
Nathaen Weitzel M.D.
James West M.D., M.A.
Sivan Wexler M.D.
Michelle White M.D.
Elizabeth Whitlock M.D., M.Sc.
Jeanine Wiener-Kronish M.D.
Troy Wildes M.D.
David Wilkinson M.B.B.S.
Brian Williams M.D., M.B.A.
George Williams MD
Kayode Williams M.B., B.S.
Tamara Willis Ph.D., MPH
Karl Willmann M.D.
Sylvia Wilson M.D.
William Wilson M.D.
Thomas Witkowski M.D.
David Wlody M.D.
Richard Wolman M.D., M.A.
Cynthia Wong M.D.
David Wong M.D.
Patrick Wong M.D.
Michael Woo M.D.
Derek Woodrum M.D.
Lee Woodson M.D., Ph.D.
Glenn Woodworth M.D.
Crystal Wright M.D.
Hannah Wunsch M.D., M.Sc.
Yan Xu Ph.D.
Jacques Ya Deau M.D., Ph.D.
Myron Yaster M.D.
Meltem Yilmaz M.D.
David Young M.D., MBA
George Youssef M.D.
Francine Yudkowitz M.D.
Vivian Manying Yuen M.B.,B.S.
Luis Zabala M.D.
Zdravka Zarova M.D.
Ahmed Zaky M.D.
Laura Zeigler M.D.
Yun-Xia Zuo M.D.
Andrew Zura M.D.
David Zvara M.D.
SPEAKER INDEX
